Outcomes of Endovascular Treatment versus Standard Medical Treatment for Acute Ischemic Stroke with Basilar Artery Occlusion: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy and Study Selection
2.2. Data Extraction and Outcome Measures
2.3. Risk-of-Bias Assessment
2.4. Statistical Analysis
3. Results
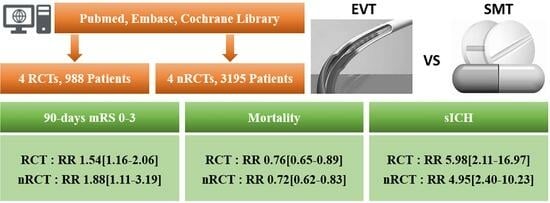
3.1. Literature Search Results and Study Selection
3.2. Risk of Bias
3.3. Effect of EVT on Functional Outcomes
3.4. Effect of EVT on Mortality and sICH
3.5. Factors Influencing the Functional Outcomes of EVT
4. Discussion
4.1. Evidence from RCTs
4.2. Evidence from Non-RCTs
4.3. Effect Modification of EVT Outcomes by Specific Factors
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mattle, H.P.; Arnold, M.; Lindsberg, P.J.; Schonewille, W.J.; Schroth, G. Basilar artery occlusion. Lancet Neurol. 2011, 10, 1002–1014. [Google Scholar] [CrossRef] [PubMed]
- Smith, W.S.; Lev, M.H.; English, J.D.; Camargo, E.C.; Chou, M.; Johnston, S.C.; Gonzalez, G.; Schaefer, P.W.; Dillon, W.P.; Koroshetz, W.J.; et al. Significance of Large Vessel Intracranial Occlusion Causing Acute Ischemic Stroke and TIA. Stroke 2009, 40, 3834–3840. [Google Scholar] [CrossRef] [PubMed]
- Hawkes, M.A.; Blaginykh, E.; Ruff, M.W.; Burrus, T.; Wijdicks, E.F.; Rabinstein, A.A. Long-term mortality, disability and stroke recurrence in patients with basilar artery occlusion. Eur. J. Neurol. 2020, 27, 579–585. [Google Scholar] [CrossRef]
- Ritvonen, J.; Sairanen, T.; Silvennoinen, H.; Virtanen, P.; Salonen, O.; Lindsberg, P.J.; Strbian, D. Outcomes and long-term mortality after basilar artery occlusion—A cohort with up to 20 years’ follow-up. Eur. J. Neurol. 2021, 28, 816–822. [Google Scholar] [CrossRef]
- Berkhemer, O.A.; Fransen, P.S.; Beumer, D.; Van Den Berg, L.A.; Lingsma, H.F.; Yoo, A.J.; Schonewille, W.J.; Vos, J.A.; Nederkoorn, P.J.; Wermer, M.J.H.; et al. A Randomized Trial of Intraarterial Treatment for Acute Ischemic Stroke. N. Engl. J. Med. 2015, 372, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Goyal, M.; Demchuk, A.M.; Menon, B.K.; Eesa, M.; Rempel, J.L.; Thornton, J.; Roy, D.; Jovin, T.G.; Willinsky, R.A.; Biggya, L.; et al. SapkotaRandomized Assessment of Rapid Endovascular Treatment of Ischemic Stroke. N. Engl. J. Med. 2015, 372, 1019–1030. [Google Scholar] [CrossRef]
- Saver, J.L.; Goyal, M.; Bonafe, A.; Diener, H.C.; Levy, E.I.; Pereira, V.M.; Albers, G.W.; Cognard, C.; Cohen, D.J.; Hacke, W.; et al. Stent-Retriever Thrombectomy after Intravenous t-PA vs. t-PA Alone in Stroke. N. Engl. J. Med. 2015, 372, 2285–2295. [Google Scholar] [CrossRef]
- Campbell, B.C.; Mitchell, P.J.; Kleinig, T.J.; Dewey, H.M.; Churilov, L.; Yassi, N.; Yan, B.; Dowling, R.J.; Parsons, M.W.; Oxley, T.J.; et al. Endovascular Therapy for Ischemic Stroke with Perfusion-Imaging Selection. N. Engl. J. Med. 2015, 372, 1009–1018. [Google Scholar] [CrossRef]
- Jovin, T.G.; Chamorro, A.; Cobo, E.; de Miquel, M.A.; Molina, C.A.; Rovira, A.; Román, L.S.; Serena, J.; Abilleira, S.; Ribó, M.; et al. Thrombectomy within 8 Hours after Symptom Onset in Ischemic Stroke. N. Engl. J. Med. 2015, 372, 2296–2306. [Google Scholar] [CrossRef]
- Schonewille, W.J.; Wijman, C.A.; Michel, P.; Rueckert, C.M.; Weimar, C.; Mattle, H.P.; Engelter, S.T.; Tanne, D.; Muir, K.W.; Molina, C.A.; et al. Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): A prospective registry study. Lancet Neurol. 2009, 8, 724–730. [Google Scholar] [CrossRef]
- Writing Group for the BASILAR Group; Zi, W.; Qiu, Z.; Wu, D.; Li, F.; Liu, H.; Liu, W.; Huang, W.; Shi, Z.; Bai, Y.; et al. Assessment of Endovascular Treatment for Acute Basilar Artery Occlusion via a Nationwide Prospective Registry. JAMA Neurol. 2020, 77, 561. [Google Scholar] [PubMed]
- Tao, C.; Qureshi, A.I.; Yin, Y.; Li, J.; Li, R.; Xu, P.; Sun, J.; Liao, G.; Yue, X.; Shi, H.; et al. Endovascular Treatment Versus Best Medical Management in Acute Basilar Artery Occlusion Strokes: Results From the ATTENTION Multicenter Registry. Circulation 2022, 146, 6–17. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Dai, Q.; Ye, R.; Zi, W.; Liu, Y.; Wang, H.; Zhu, W.; Ma, M.; Yin, Q.; Li, M.; et al. Endovascular treatment versus standard medical treatment for vertebrobasilar artery occlusion (BEST): An open-label, randomised controlled trial. Lancet Neurol. 2020, 19, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Langezaal, L.C.; van der Hoeven, E.J.; Mont’Alverne, F.J.; de Carvalho, J.J.; Lima, F.O.; Dippel, D.W.; van der Lugt, A.; Lo, R.T.; Boiten, J.; Nijeholt, G.J.L. À; et al. Endovascular Therapy for Stroke Due to Basilar-Artery Occlusion. N. Engl. J. Med. 2021, 384, 1910–1920. [Google Scholar] [CrossRef] [PubMed]
- Jovin, T.G.; Li, C.; Wu, L.; Wu, C.; Chen, J.; Jiang, C.; Shi, Z.; Gao, Z.; Song, C.; Chen, W.; et al. Trial of Thrombectomy 6 to 24 Hours after Stroke Due to Basilar-Artery Occlusion. N. Engl. J. Med. 2022, 387, 1373–1384. [Google Scholar] [CrossRef] [PubMed]
- Tao, C.; Nogueira, R.G.; Zhu, Y.; Sun, J.; Han, H.; Yuan, G.; Wen, C.; Zhou, P.; Chen, W.; Zeng, G.; et al. Trial of Endovascular Treatment of Acute Basilar-Artery Occlusion. N. Engl. J. Med. 2022, 387, 1361–1372. [Google Scholar] [CrossRef]
- Broussalis, E.; Hitzl, W.; McCoy, M.; Trinka, E.; Killer, M. Comparison of Endovascular Treatment Versus Conservative Medical Treatment in Patients With Acute Basilar Artery Occlusion. Vasc. Endovasc. Surg. 2013, 47, 429–437. [Google Scholar] [CrossRef]
- Yoshimoto, T.; Tanaka, K.; Yamagami, H.; Uchida, K.; Inoue, M.; Koge, J.; Ihara, M.; Toyoda, K.; Imamura, H.; Ohara, N.; et al. Treatment Outcomes by Initial Neurological Deficits in Acute Stroke Patients with Basilar Artery Occlusion: The RESCUE Japan Registry 2. J. Stroke Cerebrovasc. Dis. 2020, 29, 105256. [Google Scholar] [CrossRef]
- Kim, J.S.; Bonovich, D. Research on Intracranial Atherosclerosis from the East and West: Why Are the Results Different? J. Stroke 2014, 16, 105. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, X.; Liu, L.; Soo, Y.O.; Pu, Y.; Pan, Y.; Wang, Y.; Zou, X.; Leung, T.W.H.; Cai, Y.; et al. Prevalence and Outcomes of Symptomatic Intracranial Large Artery Stenoses and Occlusions in China: The Chinese Intracranial Atherosclerosis (CICAS) Study. Stroke 2014, 45, 663–669. [Google Scholar] [CrossRef]
- Goyal, M.; Menon, B.K.; Van Zwam, W.H.; Dippel, D.W.J.; Mitchell, P.J.; Demchuk, A.M.; Dávalos, A.; Majoie, C.B.L.M.; Van Der Lugt, A.; De Miquel, M.A.; et al. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet 2016, 387, 1723–1731. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Kong, W.; Qiu, Z.; Liu, D.; Li, H.; Zhou, P.; Yan, Z.; Wang, Y.; Dai, W.; Zheng, C.; et al. Outcome of endovascular treatment in acute basilar artery occlusion with National Institutes of Health Stroke Scale score 10–19. J. Neurosurg. 2022, 137, 1081–1087. [Google Scholar] [CrossRef] [PubMed]
- Kong, W.; Yuan, J.; Huang, J.; Song, J.; Zhao, C.; Sang, H.; Luo, W.; Xie, D.; Gao, F.; Li, H.; et al. Outcomes of Endovascular Therapy in Acute Basilar Artery Occlusion With Severe Symptoms. JAMA Netw. Open 2021, 4, e2139550. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, P.J.; Yan, B.; Churilov, L.; Dowling, R.J.; Bush, S.J.; Bivard, A.; Huo, X.C.; Wang, G.; Zhang, S.Y.; Ton, M.D.; et al. Endovascular thrombectomy versus standard bridging thrombolytic with endovascular thrombectomy within 4·5 h of stroke onset: An open-label, blinded-endpoint, randomised non-inferiority trial. Lancet 2022, 400, 116–125. [Google Scholar] [CrossRef]
- Fischer, U.; Kaesmacher, J.; Strbian, D.; Eker, O.; Cognard, C.; Plattner, P.S.; Bütikofer, L.; Mordasini, P.; Deppeler, S.; Pereira, V.M.; et al. Thrombectomy alone versus intravenous alteplase plus thrombectomy in patients with stroke: An open-label, blinded-outcome, randomised non-inferiority trial. Lancet 2022, 400, 104–115. [Google Scholar] [CrossRef]
- Liebeskind, D.S. Collateral Circulation. Stroke 2003, 34, 2279–2284. [Google Scholar] [CrossRef]
- Tei, H.; Uchiyama, S.; Usui, T.; Ohara, K. Posterior circulation ASPECTS on diffusion-weighted MRI can be a powerful marker for predicting functional outcome. J. Neurol. 2010, 257, 767–773. [Google Scholar] [CrossRef]
- Sang, H.; Li, F.; Yuan, J.; Liu, S.; Luo, W.; Wen, C.; Zhu, Q.; Chen, W.; Lin, M.; Qi, L.; et al. Values of Baseline Posterior Circulation Acute Stroke Prognosis Early Computed Tomography Score for Treatment Decision of Acute Basilar Artery Occlusion. Stroke 2021, 52, 811–820. [Google Scholar] [CrossRef]
- Adusumilli, G.; Kobeissi, H.; Ghozy, S.; Hardy, N.; Kallmes, K.M.; Hutchison, K.; Kallmes, D.F.; Brinjikji, W.; Albers, G.W.; Heit, J.J. Endovascular thrombectomy after acute ischemic stroke of the basilar artery: A meta-analysis of four randomized controlled trials. J. Neurointerv. Surg. 2022, jnis-2022-019776. [Google Scholar] [CrossRef]
- Abdalkader, M.; Finitsis, S.; Li, C.; Hu, W.; Liu, X.; Ji, X.; Huo, X.; Alemseged, F.; Qiu, Z.; Strbian, D.; et al. Endovascular versus Medical Management of Acute Basilar Artery Occlusion: A Systematic Review and Meta-Analysis of the Randomized Controlled Trials. J. Stroke 2023, 25, 81–91. [Google Scholar] [CrossRef]
- Yu, Y.; Lou, Y.; Cui, R.; Miao, Z.; Lou, X.; Ma, N. Endovascular treatment versus standard medical treatment for basilar artery occlusion: A meta-analysis of randomized controlled trials. J. Neurosurg. 2023, 1, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-H.; Liebeskind, D.S.; Ovbiagele, B.; Lee, M.; Saver, J.L. Efficacy of endovascular therapy for basilar and vertebral artery occlusion: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Intern. Med. 2023, 110, 22–28. [Google Scholar] [CrossRef] [PubMed]





| Type | Author, Year (Trial) | Country | Study Design | Population | Characteristics | |||
|---|---|---|---|---|---|---|---|---|
| N | EVT | N | SMT | |||||
| RCT | Liu et al., 2020 (BEST) [13] | China | Multicenter, prospective, open-label trial with blinded endpoint assessment | Age ≥ 18 years, pre-mRS score of 0–2, CTA/MRA/DSA-confirmed BAO, and onset within 8 h | 66 | Age: 62 (50–74) years * NIHSS score: 32 (18–38) * pc-ASPECTS: 8 (7–9) * IVT: 18 (27%) Onset-to-randomization time: 246 (139–360) min * | 65 | Age: 68 (57–74) years * NIHSS score: 26 (13–37) * pc-ASPECTS: 8 (7–9) * IVT: 21 (32%) Onset-to-randomization time: 278 (191–387) min * |
| RCT | Langezaal et al., 2021 (BASICS) [14] | International | Multicenter, open-label trial with blinded outcome assessment | Age < 85 years, NIHSS score ≥ 10, CTA/MRA-confirmed BAO, and onset within 6 h (expanded to age ≥ 85 and NIHSS score < 10 due to slow recruitment) | 154 | Age: 66.8 ± 13.1 years £ NIHSS score: 21.9 £ pc-ASPECTS: NA IVT: 121 (78.6%) Onset-to-randomization time: NA | 146 | Age: 67.2 ± 11.9 years £ NIHSS score: 22.1 £ pc-ASPECTS: NA IVT: 116 (79.5%) Onset-to-randomization time: NA |
| RCT | Jovin et al., 2022 (BAOCHE) [15] | China | Investigator-initiated, multicenter, open-label trial with blinded outcome evaluation | Age 18–80 years, pre-mRS score of 0–1, NIHSS score ≥ 10, BAO, onset within 6–24 h (expanded to NIHSS score ≥ 6 due to slow recruitment) | 110 | Age: 64.2 ± 9.6 years £ NIHSS score: 20 (15–29) * pc-ASPECTS: 8 (7–10) * IVT: 15 (14%) Onset-to-randomization time: 664 (512–861) min * | 107 | Age: 63.7 ± 9.8 £ NIHSS score: 19 (12–30) * pc-ASPECTS: 8 (7–10) * IVT: 23 (21%) Onset-to-randomization time: 662 (492–838) min * |
| RCT | Tao et al., 2022 (ATTENTION) [16] | China | Investigator-initiated, multicenter, prospective trial | Age ≥ 18 years, NIHSS score ≥ 10, CTA/MRA/DSA-confirmed BAO, and onset within 12 h | 226 | Age: 66.0 ± 11.1 years £ NIHSS score: 24 (15–35) * pc-ASPECTS: 9 (8–10) * IVT: 60 (27%) Onset-to-randomization time: 306 (216–432) min * | 114 | Age: 67.3 ± 10.2 £ NIHSS score: 24 (14–35) * pc-ASPECTS: 10 (8–10) * IVT: 35 (31%) Onset-to-randomization time: 294 (210–420) min * |
| non-RCT | Broussalis, 2013 [17] | Austria | Prospective, nationwide registry study | Posterior circulation stroke caused by BAO | 77 | Age: 68 (range 32–89) years NIHSS score: 22 (range 4–28) pc-ASPECTS: NA IVT: 30 (38.9%) Duration of treatment: 259 (range 60–1080) min | 22 | Age: 72 (range 31–94) years NIHSS score: 23 (range 12–28) pc-ASPECTS: NA IVT: 5/22 (22.7%) Duration of treatment: 314 (range 90–720) min |
| non-RCT | Zi et al., 2020 (BASILAR) [11] | China | Prospective, nationwide registry study | Age ≥ 18 years and acute symptomatic and radiologically confirmed BAO | 647 | Age: 64 (56–73) years § NIHSS score: 27 (17–33) § pc-ASPECTS: 8 (7–9) § IVT: 119 (18.4%) Duration of treatment: 246 (132–390) min § | 182 | Age: 67 (59–76) years § NIHSS score: 26.5 (16–33) § pc-ASPECTS: 7 (6–8) § IVT: 47/182 (25.8%) Duration of treatment: 221.5 (116.25–407) min § |
| non-RCT | Yoshimoto et al., 2020 (RESCUE) [18] | Japan | Prospective, multicenter registry study | MRA, CTA, or DSA-confirmed acute BAO | 135 | Mild group Age: 77 (67–79) § NIHSS score: 7 (5–9) § pc-ASPECTS: 8 (7–9) § Duration of treatment: 313 (155–405) min § Severe group Age: 75 (66–81) years § NIHSS score: 28 (21–33) § pc-ASPECTS: 7 (6–8) § Duration of treatment: 225 (150–455) min § | 42 | Mild group Age: 69 (62–80) years § NIHSS score: 4 (3–5) § pc-ASPECTS: 9 (7–9) § Duration of treatment: NA Severe group Age: 80 (73–84) years § NIHSS score: 25 (19–30) § pc-ASPECTS: 6 (4–10) § Duration of treatment: NA |
| non-RCT | Tao et al., 2022 (ATTENTION) [12] | China | Prospective, nationwide registry study | CTA/MRA/DSA-confirmed BAO, admission within 24 h of estimated onset, and pre-mRS score of ≤ 2 | 1672 | Age: 66 (56–73) years § NIHSS score: 20.5 (13–29) § pc-ASPECTS: NA IVT: 404 (24.2%) Duration of treatment: NA | 462 | Age: 64 (54–72) years § NIHSS score: 21 (14–28) § pc-ASPECTS: NA IVT: 86 (18.6%) Duration of treatment: NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, J.-H.; Lin, S.-C.; Hong, C.-T.; Chan, L. Outcomes of Endovascular Treatment versus Standard Medical Treatment for Acute Ischemic Stroke with Basilar Artery Occlusion: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 6444. https://doi.org/10.3390/jcm12206444
Chen J-H, Lin S-C, Hong C-T, Chan L. Outcomes of Endovascular Treatment versus Standard Medical Treatment for Acute Ischemic Stroke with Basilar Artery Occlusion: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(20):6444. https://doi.org/10.3390/jcm12206444
Chicago/Turabian StyleChen, Jia-Hung, Sheng-Chieh Lin, Chien-Tai Hong, and Lung Chan. 2023. "Outcomes of Endovascular Treatment versus Standard Medical Treatment for Acute Ischemic Stroke with Basilar Artery Occlusion: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 12, no. 20: 6444. https://doi.org/10.3390/jcm12206444
APA StyleChen, J.-H., Lin, S.-C., Hong, C.-T., & Chan, L. (2023). Outcomes of Endovascular Treatment versus Standard Medical Treatment for Acute Ischemic Stroke with Basilar Artery Occlusion: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 12(20), 6444. https://doi.org/10.3390/jcm12206444