Oral Health-Related Quality of Life in Patients after Stroke—A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. PICO Question
2.2. Eligibility Criteria
- -
- published before 30 November 2021;
- -
- inclusion of patients after stroke, irrespective of their time since stroke and form of therapy or rehabilitation;
- -
- reporting of a well-documented and valid OHRQoL measurement (especially questionnaire-based assessment);
- -
- full-text in English language.
2.3. Search Strategy
2.4. Data Extraction
- year of publication, number of participants, study type, age, gender, status, and time after stroke (time since stroke onset, form of current therapy, if applicable);
- inclusion of a healthy control group;
- information on oral health status, including tooth loss and dentures, dental as well as periodontal diseases, oral hygiene, and any further oral health parameters, if applicable;
- OHRQoL measurement and findings;
- associations between OHRQoL and quality of life, disease-related parameters, or oral health findings, if applicable;
- subscales of the OHRQoL, if applicable;
2.5. Quality Assessment
3. Results
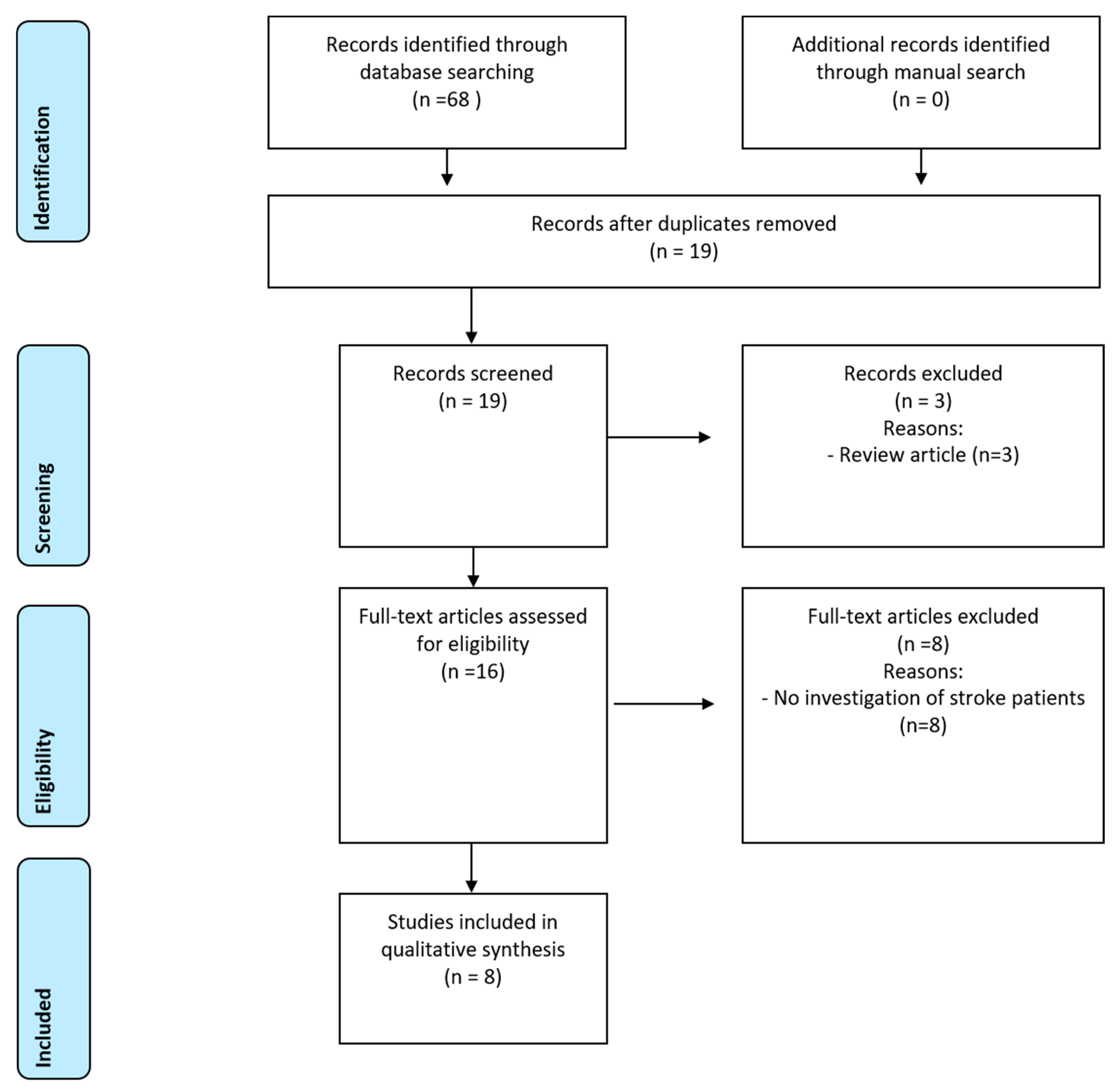
3.1. Search Findings
3.2. Characteristics of Included Studies
3.3. Quality Assessment
3.4. Oral Health Records and Findings
3.5. OHRQoL Measurements and Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| D-T | number of decayed teeth |
| DMF-T | decayed, missing, and filled teeth index |
| F-T | number of filled teeth |
| GOHAI | geriatric oral health assessment index |
| M-T | number of missing teeth |
| OHIP | oral health impact profile |
| OHRQoL | oral health-related quality of life |
| PICO | patient, intervention, control, outcome |
References
- Dichgans, M.; Pulit, S.L.; Rosand, J. Stroke genetics: Discovery, biology, and clinical applications. Lancet Neurol. 2019, 18, 587–599. [Google Scholar] [CrossRef]
- Hankey, G.J. Stroke. Lancet 2017, 389, 641–654. [Google Scholar] [CrossRef]
- Stinear, C.M.; Lang, C.E.; Zeiler, S.; Byblow, W.D. Advances and challenges in stroke rehabilitation. Lancet Neurol. 2020, 19, 348–360. [Google Scholar] [CrossRef]
- Opara, J.A.; Jaracz, K. Quality of life of post-stroke patients and their caregivers. J. Med. Life 2010, 3, 216–220. [Google Scholar] [PubMed]
- Love, M.F.; Sharrief, A.; Chaoul, A.; Savitz, S.; Beauchamp, J.E.S. Mind-Body Interventions, Psychological Stressors, and Quality of Life in Stroke Survivors. Stroke 2019, 50, 434–440. [Google Scholar] [CrossRef]
- Lo Buono, V.; Corallo, F.; Bramanti, P.; Marino, S. Coping strategies and health-related quality of life after stroke. J. Health Psychol. 2017, 22, 16–28. [Google Scholar] [CrossRef]
- Reissmann, D.R.; John, M.T.; Schierz, O.; Kriston, L.; Hinz, A. Association between perceived oral and general health. J. Dent. 2013, 41, 581–589. [Google Scholar] [CrossRef]
- Sischo, L.; Broder, H.L. Oral health-related quality of life: What, why, how, and future implications. J. Dent. Res. 2011, 90, 1264–1270. [Google Scholar] [CrossRef]
- Reissmann, D.R. Methodological considerations when measuring oral health-related quality of life. J. Oral Rehabil. 2021, 48, 233–245. [Google Scholar] [CrossRef]
- Haag, D.G.; Peres, K.G.; Balasubramanian, M.; Brennan, D.S. Oral Conditions and Health-Related Quality of Life: A Systematic Review. J. Dent. Res. 2017, 96, 864–874. [Google Scholar] [CrossRef]
- Su, N.; van Wijk, A.; Visscher, C.M. Psychosocial oral health-related quality of life impact: A systematic review. J. Oral Rehabil. 2021, 48, 282–292. [Google Scholar] [CrossRef] [PubMed]
- Schierz, O.; Baba, K.; Fueki, K. Functional oral health-related quality of life impact: A systematic review in populations with tooth loss. J. Oral Rehabil. 2021, 48, 256–270. [Google Scholar] [CrossRef] [PubMed]
- Campbell, P.; Bain, B.; Furlanetto, D.L.; Brady, M.C. Interventions for improving oral health in people after stroke. Cochrane Database Syst. Rev. 2020, 12, CD003864. [Google Scholar] [CrossRef]
- Dai, R.; Lam, O.L.; Lo, E.C.; Li, L.S.; Wen, Y.; McGrath, C. A systematic review and meta-analysis of clinical, microbiological, and behavioural aspects of oral health among patients with stroke. J. Dent. 2015, 43, 171–180. [Google Scholar] [CrossRef]
- Fagundes, N.C.F.; Almeida, A.P.C.P.S.C.; Vilhena, K.F.B.; Magno, M.B.; Maia, L.C.; Lima, R.R. Periodontitis as a Risk Factor for Stroke: A Systematic Review and Meta-Analysis. Vasc. Health Risk Manag. 2019, 15, 519–532. [Google Scholar] [CrossRef] [PubMed]
- Schmalz, G.; Patschan, S.; Patschan, D.; Ziebolz, D. Oral-Health-Related Quality of Life in Adult Patients with Rheumatic Diseases-A Systematic Review. J. Clin. Med. 2020, 9, 1172. [Google Scholar] [CrossRef] [PubMed]
- Schmalz, G.; Garbade, J.; Kollmar, O.; Ziebolz, D. Does oral health-related quality of life of patients after solid organ transplantation indicate a response shift? Results of a systematic review. BMC Oral Health 2020, 20, 356. [Google Scholar] [CrossRef]
- Schmalz, G.; Patschan, S.; Patschan, D.; Ziebolz, D. Oral health-related quality of life in adult patients with end-stage kidney diseases undergoing renal replacement therapy—A systematic review. BMC Nephrol. 2020, 21, 154. [Google Scholar] [CrossRef]
- Ming, Y.; Hsu, S.W.; Yen, Y.Y.; Lan, S.J. Association of oral health-related quality of life and Alzheimer disease: A systematic review. J. Prosthet. Dent. 2020, 124, 168–175. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Rostom, A.; Dube, C.; Cranney, A.; Saloojee, N.; Sy, R.; Garritty, C.; Sampson, M.; Zhang, L.; Yazdi, F.; Mamaladze, V.; et al. Celiac Disease. In Evidence Reports/Technology Assessments, No. 104; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2004. Available online: https://www.ncbi.nlm.nih.gov/books/NBK35156/ (accessed on 10 December 2021).
- McMillan, A.S.; Leung, K.C.; Pow, E.H.; Wong, M.C.; Li, L.S.; Allen, P.F. Oral health-related quality of life of stroke survivors on discharge from hospital after rehabilitation. J. Oral Rehabil. 2005, 32, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Hunter, R.V.; Clarkson, J.E.; Fraser, H.W.; MacWalter, R.S. A preliminary investigation into tooth care, dental attendance and oral health related quality of life in adult stroke survivors in Tayside, Scotland. Gerodontology 2006, 23, 140–148. [Google Scholar] [CrossRef] [PubMed]
- Schimmel, M.; Leemann, B.; Christou, P.; Kiliaridis, S.; Schnider, A.; Herrmann, F.R.; Müller, F. Oral health-related quality of life in hospitalised stroke patients. Gerodontology 2011, 28, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Jang, E.J.; Kim, E.K.; Lee, K.S.; Lee, H.K.; Choi, Y.H.; Hwang, T.Y.; Kim, S.K.; Jo, M.W. Oral health related qual-ity of life and it’s related factors of stroke patients at home in Korea. Arch. Gerontol. Geriatr. 2015, 61, 523–528. [Google Scholar] [CrossRef]
- Lawal, I.U.; Ibrahim, R.; Ramphoma, K.J. Oral hygiene in stroke survivors undergoing rehabilitation: Does upper extremity motor function matters? Top. Stroke Rehabil. 2021, 28, 531–536. [Google Scholar] [CrossRef]
- McGrath, C.; McMillan, A.S.; Zhu, H.W.; Li, L.S. Agreement between patient and proxy assessments of oral health-related quality of life after stroke: An observational longitudinal study. J. Oral Rehabil. 2009, 36, 264–270. [Google Scholar] [CrossRef]
- Lam, O.L.; McMillan, A.S.; Li, L.S.; McGrath, C. Predictors of oral health-related quality of life in patients following stroke. J. Rehabil. Med. 2014, 46, 520–526. [Google Scholar] [CrossRef][Green Version]
- Dai, R.; Lam, O.L.T.; Lo, E.C.M.; Li, L.S.W.; McGrath, C. Oral health-related quality of life in patients with stroke: A randomized clinical trial of oral hygiene care during outpatient rehabilitation. Sci. Rep. 2017, 7, 7632. [Google Scholar] [CrossRef]
- Slade, G.D.; Spencer, A.J. Development and evaluation of the oral health impact profile. Community Dent. Health 1994, 11, 3–11. [Google Scholar]
- Slade, G.D. Derivation and validation of a short-form oral health impact profile. Community Dent. Oral Epidemiol. 1997, 25, 284–290. [Google Scholar] [CrossRef]
- John, M.T.; Rener-Sitar, K.; Baba, K.; Čelebić, A.; Larsson, P.; Szabo, G.; Norton, W.E.; Reissmann, D.R. Patterns of impaired oral health-related quality of life dimensions. J. Oral Rehabil. 2016, 43, 519–527. [Google Scholar] [CrossRef] [PubMed]
- John, M.T.; Micheelis, W.; Biffar, R. Reference values in oral health-related quality of life for the abbreviated version of the Oral Health Impact Profile. Schweiz. Monatschr. Zahnmed. 2004, 114, 784–791. (In German) [Google Scholar]
- Atchison, K.A.; Dolan, T.A. Development of the Geriatric Oral Health Assessment Index. J. Dent. Educ. 1990, 54, 680–687. [Google Scholar] [CrossRef] [PubMed]
- De Carvalho, B.M.D.F.; Parente, R.C.; Franco, J.M.P.L.; Silva, P.G.B. GOHAI and OHIP-EDENT Evaluation in Removable Dental Prostheses Users: Factorial Analysis and Influence of Clinical and Prosthetic Variables. J. Prosthodont. 2021, 30, 581–589. [Google Scholar] [CrossRef]
- Azami-Aghdash, S.; Pournaghi-Azar, F.; Moosavi, A.; Mohseni, M.; Derakhshani, N.; Kalajahi, R.A. Oral Health and Related Quality of Life in Older People: A Systematic Review and Meta-Analysis. Iran. J. Public Health 2021, 50, 689–700. [Google Scholar] [CrossRef]
- El Osta, N.; Tubert-Jeannin, S.; Hennequin, M.; Bou Abboud Naaman, N.; El Osta, L.; Geahchan, N. Comparison of the OHIP-14 and GOHAI as measures of oral health among elderly in Lebanon. Health Qual. Life Outcomes 2012, 10, 131. [Google Scholar] [CrossRef]
- Gerritsen, A.E.; Allen, P.F.; Witter, D.J.; Bronkhorst, E.M.; Creugers, N.H. Tooth loss and oral health-related quality of life: A systematic review and meta-analysis. Health Qual. Life Outcomes 2010, 8, 126. [Google Scholar] [CrossRef]
- Ferreira, M.C.; Dias-Pereira, A.C.; Branco-de-Almeida, L.S.; Martins, C.C.; Paiva, S.M. Impact of periodontal disease on quality of life: A systematic review. J. Periodontal Res. 2017, 52, 651–665. [Google Scholar] [CrossRef]
- Fagundes, N.C.F.; Couto, R.S.D.; Brandão, A.P.T.; Lima, L.A.O.; Bittencourt, L.O.; Souza-Rodrigues, R.D.; Freire, M.A.M.; Maia, L.C.; Lima, R.R. Association between Tooth Loss and Stroke: A Systematic Review. J. Stroke Cerebrovasc. Dis. 2020, 29, 104873. [Google Scholar] [CrossRef]
- Belfiore, P.; Miele, A.; Gallè, F.; Liguori, G. Adapted physical activity and stroke: A systematic review. J. Sports Med. Phys. Fit. 2018, 58, 1867–1875. [Google Scholar] [CrossRef]
- Thilarajah, S.; Mentiplay, B.F.; Bower, K.J.; Tan, D.; Pua, Y.H.; Williams, G.; Koh, G.; Clark, R.A. Factors Associated with Post-Stroke Physical Activity: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2018, 99, 1876–1889. [Google Scholar] [CrossRef] [PubMed]
- Kassebaum, N.J.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.; Marcenes, W. Global Burden of Severe Tooth Loss: A Systematic Review and Meta-analysis. J. Dent. Res. 2014, 93 (Suppl. S7), 20S–28S. [Google Scholar] [CrossRef] [PubMed]
- Riva, F.; Seoane, M.; Reichenheim, M.E.; Tsakos, G.; Celeste, R.K. Adult oral health-related quality of life instruments: A systematic review. Community Dent. Oral Epidemiol. 2021, in press. [CrossRef] [PubMed]
- Schmalz, G.; Ziebolz, D. Changing the Focus to the Whole Patient instead of One Oral Disease: The Concept of Individualized Prevention. Adv. Prev. Med. 2020, 2020, 6752342. [Google Scholar] [CrossRef]
- Zhu, H.W.; McGrath, C.; McMillan, A.S.; Li, L.S. Can caregivers be used in assessing oral health-related quality of life among patients hospitalized for acute medical conditions? Community Dent. Oral Epidemiol. 2008, 36, 27–33. [Google Scholar] [CrossRef]
- Molania, T.; Malekzadeh Shafaroudi, A.; Taghavi, M.; Ehsani, H.; Moosazadeh, M.; Haddadi, A.; Gholizadeh, N.; Salehi, M. Oral health-related quality of life (OHRQoL) in cardiovascular patients referring to Fatima Zahra Hospital in Sari, Iran. BMC Oral Health 2021, 21, 391. [Google Scholar] [CrossRef]
- Pengpid, S.; Peltzer, K. Prevalence and Associated Factors of Self-rated Oral Health among a National Population-based Sample of Adults in Sudan: Results of the 2016 STEPS Survey. Oral Health Prev. Dent. 2021, 19, 391–397. [Google Scholar] [CrossRef]
- Parat, K.; Radić, M.; Perković, D.; Lukenda, D.B.; Kaliterna, D.M. Reduced salivary flow and caries status are correlated with disease activity and severity in patients with diffuse cutaneous systemic sclerosis. J. Int. Med. Res. 2020, 48, 300060520941375. [Google Scholar] [CrossRef]
- de Bataille, C.; Castellan, M.; Massabeau, C.; Jouve, E.; Lacaze, J.L.; Sibaud, V.; Vigarios, E. Oral mucosal changes induced by adjuvant endocrine therapies in breast cancer patients: Clinical aspects and proposal for management. Support. Care Cancer 2021, 29, 1719–1722. [Google Scholar] [CrossRef]
- Montero, J.; Dib, A.; Guadilla, Y.; Flores, J.; Pardal-Peláez, B.; Quispe-López, N.; Gómez-Polo, C. Functional and Patient-Centered Treatment Outcomes with Mandibular Overdentures Retained by Two Immediate or Conventionally Loaded Implants: A Randomized Clinical Trial. J. Clin. Med. 2021, 10, 3477. [Google Scholar] [CrossRef]
- Vasiliu, M.P.; Sachelarie, L.; Popovici, D.; Farcas, D.M. Oral Health-Related Quality of Life in the Case of Elderly People from Romania Before and After the Prosthetic Treatment. Int. J. Med. Res. Health Sci. 2019, 8, 33–39. [Google Scholar]
- Fan, W.Y.; Tiang, N.; Broadbent, J.M.; Thomson, W.M. Occurrence, Associations, and Impacts of Nocturnal Parafunction, Daytime Parafunction, and Temporomandibular Symptoms in 38-Year-Old Individuals. J. Oral Facial Pain Headache 2019, 33, 254–259. [Google Scholar] [CrossRef] [PubMed]
| Author, Year | Country | No. of Patients | Status/Time after Stroke | Study Type | Subjects Mean Age in Years | Male (%) | Healthy Control Group for OHRQoL |
|---|---|---|---|---|---|---|---|
| McMillan et al., 2005 [22] | China | 43 | rehabilitation after stroke | monocentric cross-sectional | 73.9 ± 6.1 | 60% | yes, n = 43, 44% male, age: 73.7 ± 6.1 years |
| Hunter et al., 2006 [23] | Scotland | 41 | 1 year after stroke | monocentric cross-sectional | 69 ± 9.8 | 49% | no |
| McGrath et al., 2009 [27] | China | acute stroke: 121, after 6 months: 65 | acute stroke and 6 months later | monocentric observational with 6 months follow-up | acute stroke: 67.7 ± 11.1; after 6 months: 68.3 ± 11.3 | acute stroke: 69%, after 6 months: 72% | no |
| Schimmel et al., 2011 [24] | Switzerland | 31 | hospitalized after stroke | monocentric cross-sectional | 69.0 ± 12.7 | 58% | yes, n = 2 4, 54% male, age: 68.8 ± 10.8 years |
| Lam et al., 2014 [28] | China | 81 | rehabilitation after stroke (time since stroke onset 13 ± 6.8 days) | randomized clinical trial | 69.9 ± 10.9 | 63% | no |
| Jang et al., 2015 [25] | Korea | 549 | care at home after stroke (0–10 years after stroke) | monocentric cross-sectional | <60 years: 13.8%, 60–69 years: 35.3%, 70–79 years: 40.5%, ≥80 years: 10.4% | 60% | no |
| Dai et al., 2017 [29] | China | baseline: 94, after 3 months: 74 | rehabilitation after stroke | randomized clinical trial | n/a | n/a | no |
| Lawal et al., 2020 [26] | Nigeria | 60 | onset less than 3 months: 10%, 3–6 months: 23.3%, >6 months: 66.7% | monocentric cross-sectional | 55.7 ± 12.9 | 53.3% | no |
| Item | McMillan et al., 2005 [22] | Hunter et al., 2006 [23] | McGrath et al., 2009 [27] | Schimmel et al., 2011 [24] | Lam et al., 2014 [28] | Jang et al., 2015 [25] | Dai et al., 2017 [29] | Lawal et al., 2020 [26] |
|---|---|---|---|---|---|---|---|---|
| (1) Define the source of information (survey, record review) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| (2) List inclusion and exclusion criteria for exposed and unexposed subjects (cases and controls) or refer to previous publications | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes |
| (3) Indicate time period used for identifying patients | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| (4) Indicate whether or not subjects were consecutive if not population-based | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| (5) Indicate if evaluators of subjective components of study were masked to other aspects of the status of the participants | No | No | No | No | Yes | No | Yes | No |
| (6) Describe any assessments undertaken for quality assurance purposes (e.g., test/retest of primary outcome measurements) | Yes | No | Yes | Yes | Yes | Yes | Yes | No |
| (7) Explain any patient exclusions from analysis | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| (8) Describe how confounding was assessed and/or controlled. | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes |
| (9) If applicable, explain how missing data were handled in the analysis | NA | NA | NA | NA | NA | NA | Yes | NA |
| (10) Summarize patient response rates and completeness of data collection | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| (11) Clarify what follow-up, if any, was expected and the percentage of patients for which incomplete data or follow-up was obtained | NA | NA | Yes | NA | Yes | NA | Yes | NA |
| Total Score | 8 | 5 | 9 | 8 | 10 | 9 | 10 | 7 |
| Author, Year | Tooth Loss, Remaining Teeth, Dentures | Dental Diseases, Caries, Dental Treatment Need | Oral Hygiene Indices | Periodontal Parameters, Periodontal Treatment Need | Further Oral Health Parameters |
|---|---|---|---|---|---|
| McMillan et al., 2005 [22] | number of teeth: 14.6 ± 10.8, M-T: 18.0 ± 10.7, removable denture: 40.5%, complete denture: 20.9 (maxilla), 23.3 (mandible) | D-T: 2.7 ± 3.7, F-T: 0.9 ± 2.1, DMF-T: 21.6 ± 9.7 | n/a | n/a | n/a |
| Hunter et al., 2006 [23] | 44% edentolous and wore full dentures, mean number of teeth in dentate: 17 teeth, 52% of dentate wear dentures | n/a | n/a | 80% of dentate patients had CPI 1 or 2 | n/a |
| McGrath et al., 2009 [27] | n/a | n/a | n/a | n/a | n/a |
| Schimmel et al., 2011 [24] | number of teeth: 18.8 ± 8.9, number of occlusal units: 4.3 ± 4.0, removable partial denture: 19.4% | n/a | n/a | n/a | colour mixing test (masticatory efficiency) 0.0901 ± 0.0488, maximum lip force: small: 5.29 ± 1.92 N, medium: 6.70 ± 2.88 N, large: 8.68 ± 4.13 N |
| Lam et al., 2014 [28] | n/a | n/a | n/a | n/a | n/a |
| Jang et al., 2015 [25] | number of missing teeth: 9.1%, 1–8 missing teeth: 24.5%, more than 9 missing teeth: 70.6%, denture use: 46.9%, denture not use: 19.5% | n/a | n/a | n/a | n/a |
| Dai et al., 2017 [29] | n/a | n/a | n/a | n/a | n/a |
| Lawal et al., 2020 [26] | n/a | n/a | OHI-S: male 2.42 ± 1.34, female: 2.22 ± 0.91 | n/a | n/a |
| Author, Year | Assessment of OHRQoL | OHRQoL Worse than Healthy Control (HC) | Association/Correlation between OHRQoL and General HRQoL | Association/Correlation between OHRQoL and Oral Health | Association and/or Correlation between OHRQoL and Disease-Related Parameters |
|---|---|---|---|---|---|
| McMillan et al., 2005 [22] | GOHAI: 52.0 (48.0–57.0) | no, 54.0 (49.0–57.0) | n/a | n/a | no association |
| Hunter et al., 2006 [23] | OHIP 14, no sum score or mean reported | n/a | n/a | no association | n/a |
| McGrath et al., 2009 [27] | GOHAI: acute: 45.6 ± 8.5; after 6 months: 48.9 ± 6.9 | n/a | n/a | n/a | n/a |
| Schimmel et al., 2011 [24] | OHIP-EDENT: 18.8 ± 15.5 | yes, 12.3 ± 17.7 | n/a | OHIP-EDENT associated with masticatory efficiency | no association |
| Lam et al., 2014 [28] | OHIP 14: baseline: 7.0 (2.0–14.0), after 3 weeks: 4.0 (1.0–9.0) | n/a | OHIP 14 associated to SF-12 | no association | no association |
| Jang et al., 2015 [25] | OHIP 14: male: 33.0 ± 9.0, female: 33.1 ± 9.4 | n/a | n/a | OHIP 14 associated with number of missing teeth | OHIP 14 associated with degree of disability and Barthel Index |
| Dai et al., 2017 [29] | GOHAI: baseline: 54.0 (49.0–56.0), follow-up: 55.0 (50.8–58.0), OHIP 14 baseline: 4.0 (2.0–12.0), follow-up: 3.5 (1.0-8.3) | n/a | GOHAI and OHIP 14 associated with PCS score of SF-12 | GOHAI associated with plaque accumulation | n/a |
| Lawal et al., 2020 [26] | OHIP 14: 2.87 ± 0.78 | n/a | n/a | n/a | n/a |
| OHIP 14 | |||||||
|---|---|---|---|---|---|---|---|
| Author, Year, Disease | Functional Limitation | Physical Pain | Psycho-Social Discomfort | Physical Disability | Psychological Disability | Social Disability | Handicap |
| Jang et al., 2015 (male/female) [25] | 5.7 ± 2.0/5.9 ± 2.1 | 5.2 ± 1.8/5.4 ± 1.9 | 4.7 ± 1.5/4.6 ± 1.5 | 5.2 ± 1.8/5.1 ± 1.9 | 3.8 ± 1.4/3.7 ± 1.4 | 3.8 ± 0.4/3.6 ± 1.4 | 4.7 ± 1.8/4.7 ± 1.9 |
| Lawal et al., 2020 [26] | 0.65 ± 0.18 | 1.12 ± 0.27 | 0.63 ± 0.18 | 0.70 ± 0.19 | 0.27 ± 0.09 | 0.03 ± 0.02 | 0 |
| OHIP-EDENT | |||||||
| Schimmel et al., 2011 [24] | 4.2 ± 3.7 * | 4.2 ± 3.6 * | 3.0 ± 2.8 | 3.1 ± 3.8 | 1.9 ± 2.1 | 0.8 ± 1.6 | 1.6 ± 2.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schmalz, G.; Li, S.; Ziebolz, D. Oral Health-Related Quality of Life in Patients after Stroke—A Systematic Review. J. Clin. Med. 2022, 11, 1415. https://doi.org/10.3390/jcm11051415
Schmalz G, Li S, Ziebolz D. Oral Health-Related Quality of Life in Patients after Stroke—A Systematic Review. Journal of Clinical Medicine. 2022; 11(5):1415. https://doi.org/10.3390/jcm11051415
Chicago/Turabian StyleSchmalz, Gerhard, Simin Li, and Dirk Ziebolz. 2022. "Oral Health-Related Quality of Life in Patients after Stroke—A Systematic Review" Journal of Clinical Medicine 11, no. 5: 1415. https://doi.org/10.3390/jcm11051415
APA StyleSchmalz, G., Li, S., & Ziebolz, D. (2022). Oral Health-Related Quality of Life in Patients after Stroke—A Systematic Review. Journal of Clinical Medicine, 11(5), 1415. https://doi.org/10.3390/jcm11051415






