Model Calibration of Pharmacokinetic-Pharmacodynamic Lung Tumour Dynamics for Anticancer Therapies
Abstract
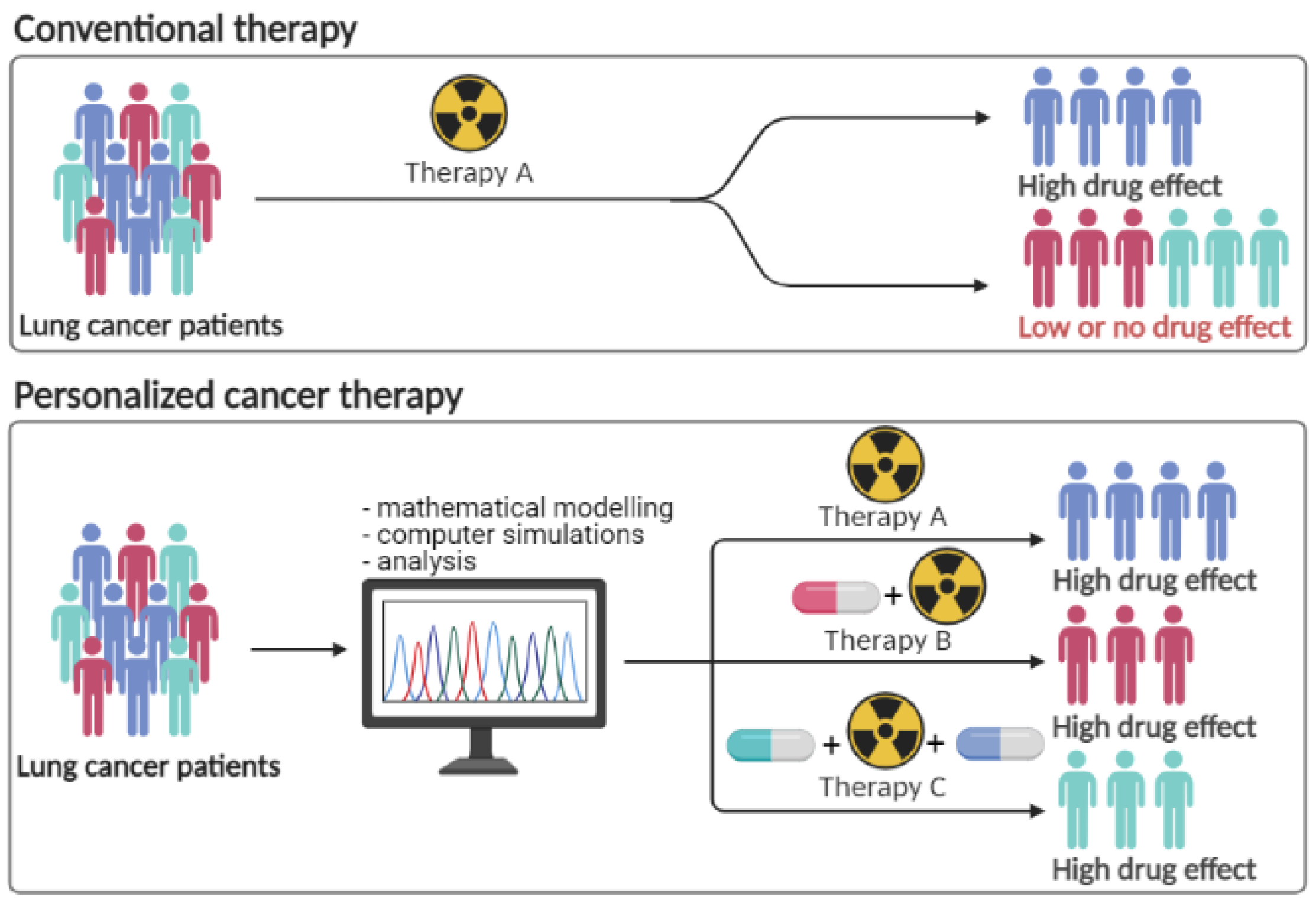
:1. Introduction
- dynamic carrying capacity models [12],
2. Materials and Methods
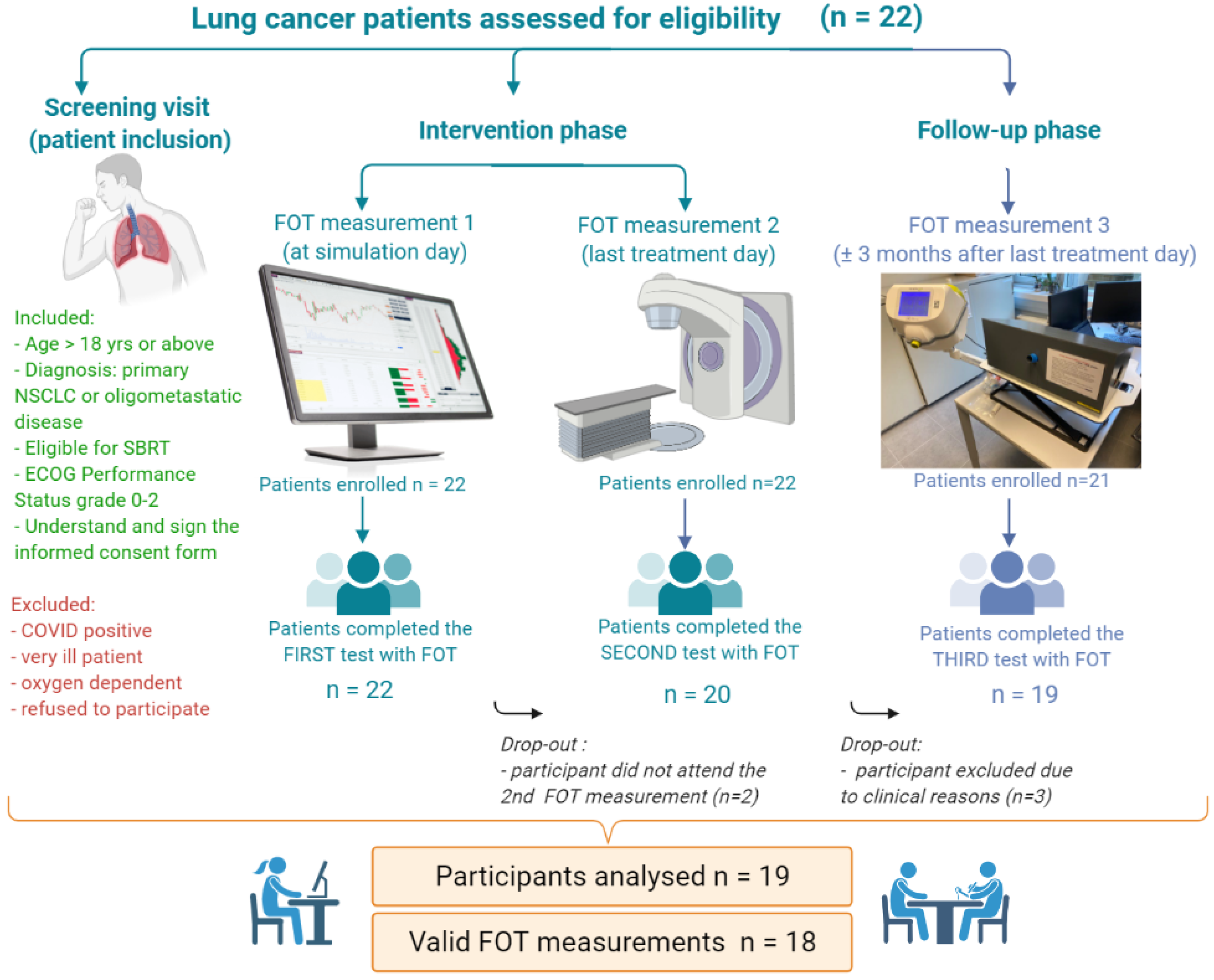
2.1. Clinical Study Design
- 1.
- Screening visit (patient inclusion). Eligibility of the patient is determined according to the inclusion/exclusion criteria and screening assessments are recorded, as shown in Table 1 (i.e., anthropometric data, diagnosis, the extent of cancer, tumor characteristics and localization, medical history, concomitant medication, spirometric and plethysmographic data (if available)).
- 2.
- Intervention phase. Once enrolled, fully eligible patients will start with the intended SBRT treatment and specific clinical information about the scheme of treatment is provided (dose fractionation, dose distribution details, duration of administration, and concomitant therapies.) The tumor volume was measured by the radiation oncologist using CT scans done for RT treatment simulation.
- 3.
- Follow-up phase (usually 3 months after last treatment day). The tumor volume was measured by the radiation oncologist using CT scans done after RT administration, during the follow-up visit.
| Characteristic | Value (n = 19 Patients) | % |
|---|---|---|
| Age (y) | ||
| Median | 67.84 | (46–80) |
| Sex | ||
| Men | 12 | 63.2% |
| Women | 7 | 36.8% |
| Site of original primary tumor | ||
| Lung | 10 | 52.6% |
| Colon | 4 | 21% |
| Rectum | 2 | 10.5% |
| Other sites 1 | 3 | 15.8% |
| Primary tumor histology | ||
| Adenocarcinoma | 9 | 47.4% |
| Spinocellular carcinoma | 4 | 21% |
| Mucinous carcinoma | 1 | 5.3% |
| Clear cell carcinoma | 1 | 5.3% |
| Unknown/NA | 4 | 21% |
| Primary or metastatic lung lesion | ||
| Primary | 9 | 47.4% |
| Metastatic | 10 | 52.6% |
| TNM Classification of Malignant tumors 2 | ||
| T0N0M1 | 10 | 52.6% |
| T1N0M0 | 7 | 36.8% |
| T2N0M0 | 2 | 10.5% |
| Tumor localization (by lobe side) | ||
| Right side | 12 | 63.2% |
| Left side | 5 | 26.3% |
| Both sides | 2 | 10.5% |
| Tumor localization (by tumor position within the lobe) | ||
| Upper lobe | 7 | 36.8% |
| Lower lobe | 9 | 47.4% |
| Upper and lower lobe | 2 | 10.5% |
| Mid lobe | 1 | 5.3% |
| Number of lesions | ||
| 1 lesion | 16 | 84.2% |
| 2 lesions | 2 | 10.5% |
| 3 lesions | 1 | 5.3% |
| ECOG Performance Status 3 | ||
| ECOG 0 | 7 | 36.8% |
| ECOG 1 | 11 | 57.9% |
| ECOG 2 | 1 | 5.3% |
| Smoking history | ||
| Active | 9 | 47.4% |
| Ex-smoker | 5 | 26.3% |
| Never | 5 | 26.3% |
| Respiratory disorders | ||
| COPD 4 | 8 | 42.1% |
| Other respiratory disorders 5 | 2 | 10.5% |
| NA | 9 | 47.4% |
| Medical history | ||
| Previous surgeries 6 | 8 | 42.1% |
| Previous RT 7 | 4 | 21% |
| No previous interventions | 9 | 47.4% |
| Fractionation schemes | ||
| 1 × 34 Gy | 2/22 | 9% |
| 3 × 18 Gy | 9/22 | 40.9% |
| 4 × 12 Gy | 10/22 | 45.5% |
| 8 × 7.5 Gy | 1/22 | 4.5% |
| Concomitant cancer therapy | ||
| Chemotherapy—Xeloda (Capecitabine) | 1 | 5.3% |
2.2. Participants Data
2.3. Treatment Strategy—Clinical Protocol
2.4. Mathematical Formulation
| Parameter | Name | Value | Units | Source |
|---|---|---|---|---|
| a | tumor growth rate | 0.693 | 1/day | [34,49] |
| n | necrosis rate | 0.10 | 1/day | [34,49] |
| clearance rate RT | 3/treatment days | 1/day | [34] | |
| half-effect concentration RT | 20 | Gy/day | [34] | |
| half-effect tumor growth | 50 | % mm3 | [34,51] | |
| max effect RT | 50 | % | [34,51] | |
| patient response | varies (0.043-0.25) | (-) | [52] | |
| drug reaction (synergic) | 8 | (-) | [52] | |
| E | combined effects (all) | calculated | 1/day | NA |
| radiotherapy dose rate | varies | mg/(mL·day) | Table 2 |
2.5. Analysis
3. Results
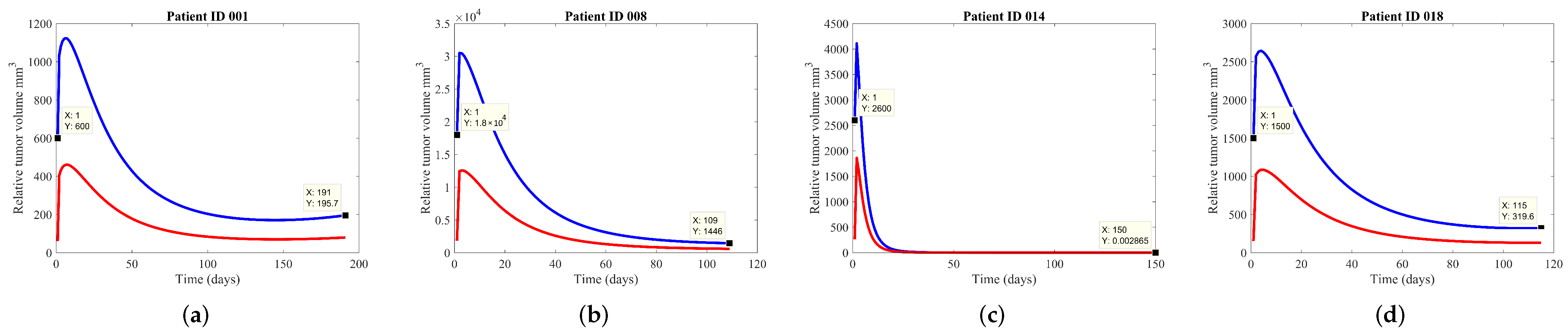
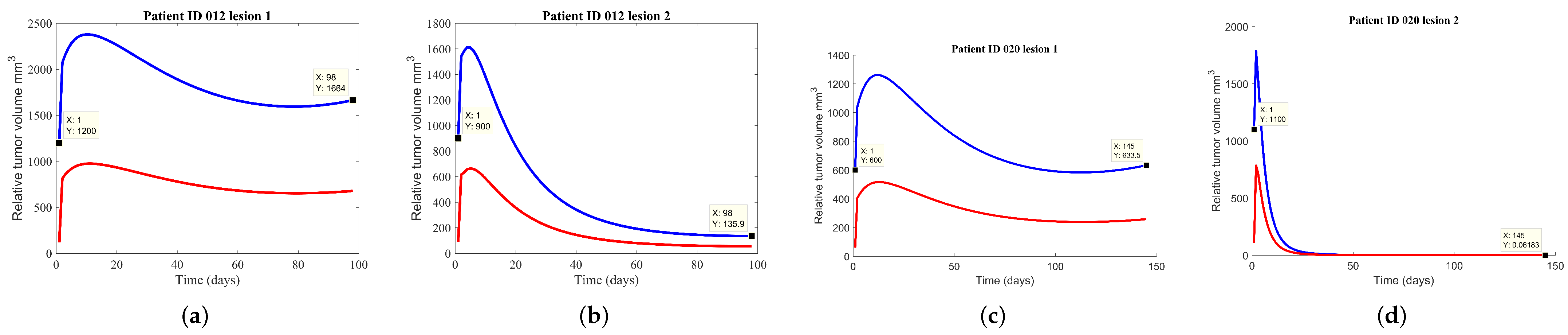
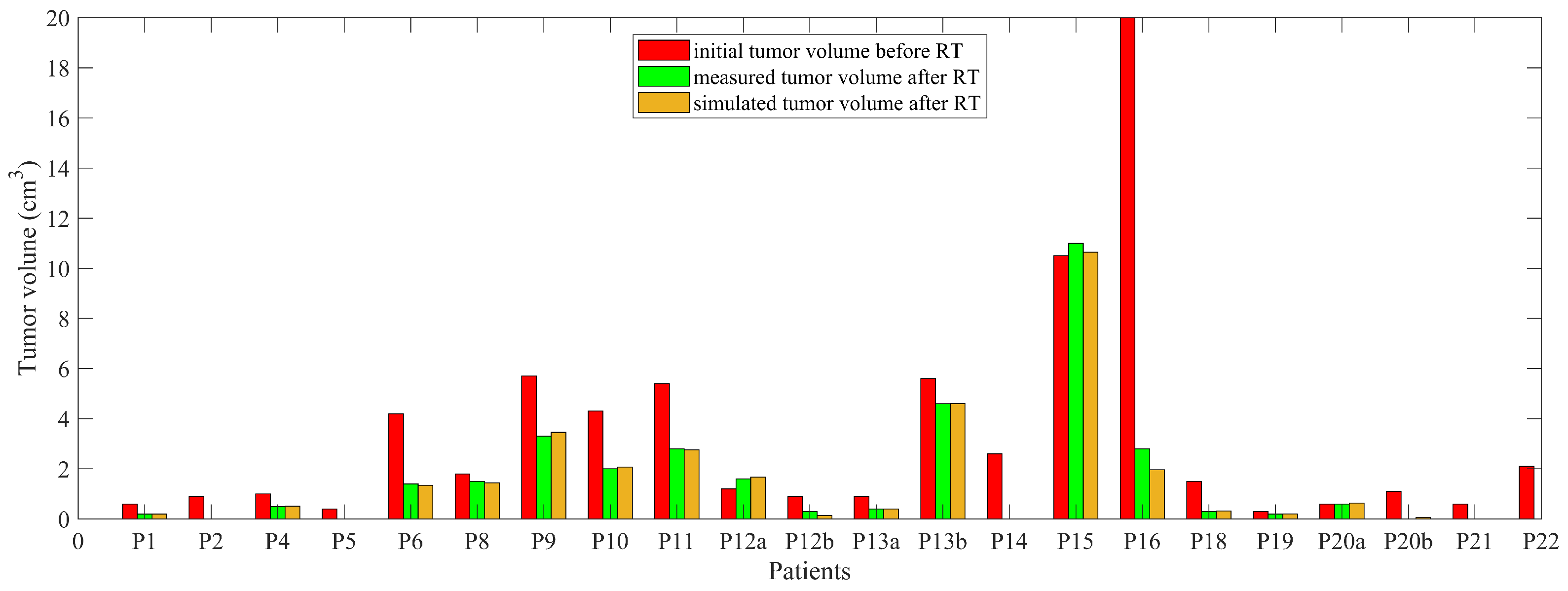
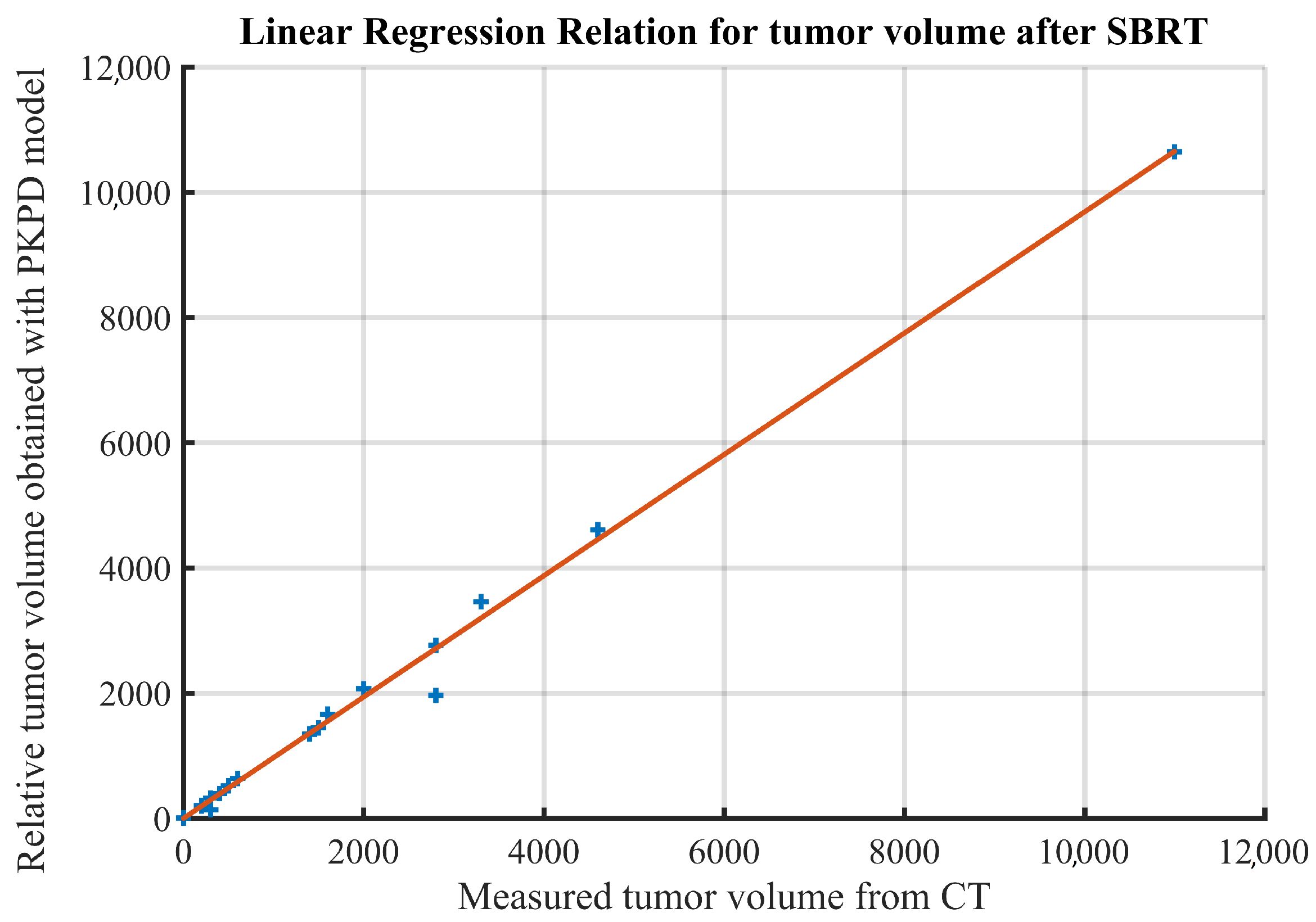
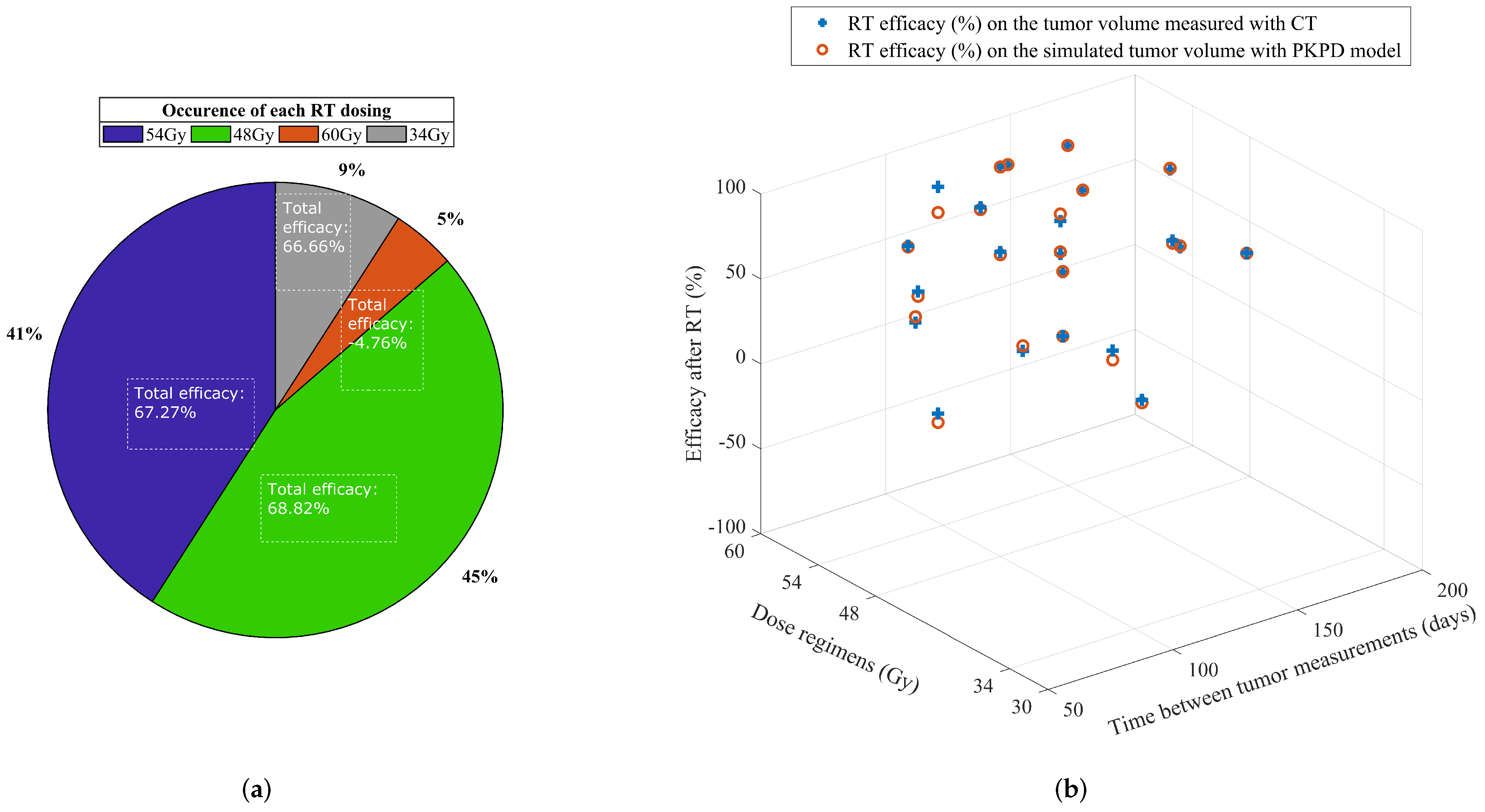
3.1. Prediction of Tumor Volume
3.2. Tumor Growth for Multiple Lesions
3.3. Uncertainty Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BED | Biological Effective Dose |
| COPD | Chronic Obstructive Pulmonary Disease |
| CT | Computed Tomography |
| CTCAE | Common Terminology Criteria for Adverse Events |
| DVH | Dose-volume histogram |
| ECOG | Eastern Cooperative Oncology Group |
| FOT | Forced Oscillation Technique |
| GCP | Good Clinical Practice |
| GOLD | Global Initiative for COPD |
| GTV | Gross tumor volume |
| GZA | GasthuisZusters Antwerpen |
| ICF | Informed consent form |
| MLD | Mean lung dose |
| NA | Not applicable |
| NSCLC | Non-small cell lung cancer |
| PKPD | Pharmacokinetic-Pharmacodynamic |
| RP | Radiation pneumonitis |
| RT | Radiotherapy |
| SBRT | Stereotactic Body Radiation Therapy |
| TLV | Total lung volume |
| TNM | Classification of Malignant tumors |
References
- Osarogiagbon, R.U.; Veronesi, G.; Fang, W.; Ekman, S.; Suda, K.; Aerts, J.G.; Donington, J. Early-stage NSCLC: Advances in thoracic oncology 2018. J. Thorac. Oncol. 2019, 14, 968–978. [Google Scholar] [CrossRef] [PubMed]
- Varlatto, J.M.; Veronesi, G. Editorial: Controversies in the local management of lung cancer. Front. Oncol. 2018, 8, 233. [Google Scholar] [CrossRef] [PubMed]
- Poels, K.; Depuydt, T.; Verellen, D.; Gevaert, T.; Dhont, J.; Duchateau, M.; Burghelea, M.; Boussaer, M.; Steenbeke, F.; Collen, C.; et al. Improving the intra-fraction update efficiency of a correlation model used for internal motion estimation during real-time tumor tracking for SBRT patients: Fast update or no update? Radiother. Oncol. 2014, 112, 352–359. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Liu, A.; Chan, J.; Boldt, R.G.; Munoz-Schuffenegger, P.; Louie, A.W. What is the optimal radiotherapy utilization rate for lung cancer?—A systematic review. Transl. Lung Cancer Res. 2019, 8 (Suppl. S2), S163–S171. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.A.; Plummer, R.; Stock, J.K.; Greenhalgh, T.A.; Ataman, O.; Kelly, S.; Clay, R.; Adams, R.A.; Baird, R.D.; Billingham, L.; et al. Clinical development of new drug–radiotherapy combinations. Nat. Rev. Clin. Oncol. 2016, 13, 627–642. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benzekry, S.; Lamont, C.; Beheshti, A.; Tracz, A.; Ebos, J.M.L.; Hlatky, L.; Hahnfeldt, P. Classical mathematical models for description and prediction of experimental tumor growth. PLoS Comput. Biol. 2014, 10, e1003800. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altrock, P.M.; Liu, L.L.; Michor, F. The mathematics of cancer: Integrating quantitative models. Nat. Rev. Cancer 2015, 15, 730–745. [Google Scholar] [CrossRef]
- Murphy, H.M.D.; Jaafari, H.; Dobrovolny, H.M. Differences in predictions of ODE models of tumor growth: A cautionary example. BMC Cancer 2016, 16, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Sápi, J.; Drexler, D.A.; Kovács, L. Comparison of mathematical tumor growth models. In Proceedings of the 13th International Symposium on Intelligent Systems and Informatics (SISY), Subotica, Serbia, 17–19 September 2015; pp. 323–328. [Google Scholar]
- Hong, W.-S.; Zhang, G.-Q. Simulation analysis for tumor radiotherapy based on three component mathematical model. J. Appl. Clin. Med. Phys. 2019, 20, 22–26. [Google Scholar] [CrossRef]
- Akanuma, A. Parameter analysis of Gompertzian function growth model in clinical tumors. Eur. J. Cancer 1978, 14, 681–688. [Google Scholar] [CrossRef]
- Ribba, B.; Watkin, E.; Tod, M.; Girard, P.; Grenier, E.; You, B.; Giraudo, E.; Freyer, G. A model of vascular tumor growth in mice combining longitudinal tumor size data with histological biomarkers. Eur. J. Cancer 2011, 47, 479–490. [Google Scholar] [CrossRef] [PubMed]
- Von Bertalanffy, L. Quantitative laws in metabolism and growth. Q. Rev. Biol. 1957, 32, 217–231. [Google Scholar] [CrossRef] [PubMed]
- West, G.B.; Brown, J.H.; Enquist, B.J. A general model for ontogenetic growth. Nature 2001, 413, 628–631. [Google Scholar] [CrossRef] [PubMed]
- Gerlee, P. The model muddle: In search of tumor growth laws. Cancer Res. 2013, 73, 2407–2411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghita, M.; Copot, D.; Ghita, M.; Derom, E.; Ionescu, C. Low frequency forced oscillation lung function test can distinguish dynamic tissue non-linearity in COPD patients. Front. Physiol. 2019, 10, 1390. [Google Scholar] [CrossRef] [PubMed]
- Ionescu, C.; Lopes, A.; Copot, D.; Machado, J.A.T.; Bates, J.H.T. The role of fractional calculus in modeling biological phenomena: A review. Commun. Nonlinear Sci. Numer. Simul. 2017, 51, 141–159. [Google Scholar] [CrossRef]
- Ionescu, C.; Kelly, J.F. Fractional calculus for respiratory mechanics: Power law impedance, viscoelasticity and tissue heterogeneity. Chaos Solitons Fractals 2017, 102, 433–440. [Google Scholar] [CrossRef]
- Ghita, M.; Copot, D.; Ionescu, C.M. Lung cancer dynamics using fractional order impedance modeling on a mimicked lung tumor setup. J. Adv. Res. 2021, 32, 61–71. [Google Scholar] [CrossRef]
- Assadi, I.; Charef, A.; Copot, D.; De Keyser, R.; Bensouici, T.; Ionescu, C. Evaluation of respiratory properties by means of fractional order models. Biomed. Signal. Process Control 2017, 34, 206–213. [Google Scholar] [CrossRef]
- West, B.J. Colloquium: Fractional calculus view of complexity: A tutorial. Rev. Mod. Phys. 2014, 86, 1169–1184. [Google Scholar] [CrossRef]
- Valentim, C.A.; Oliveira, N.A.; Rabi, J.A.; David, S.A. Can fractional calculus help improve tumor growth models? J. Comput. Appl. Math. 2020, 379, 112964. [Google Scholar] [CrossRef]
- Valentim, C.A.; Rabi, J.A.; David, S.A.; Tenreiro Machado, J.A. On multistep tumor growth models of fractional variable-order. BioSystems 2021, 199, 104294. [Google Scholar] [CrossRef] [PubMed]
- Enderling, H.; Chaplain, M.A.J.; Hahnfeldt, P. Quantitative modeling of tumor dynamics and radiotherapy. Acta Biotheor. 2010, 58, 341–353. [Google Scholar] [CrossRef] [PubMed]
- Drexler, D.A.; Ferenci, T.; Furedi, A.; Szakacs, G.; Kovacs, L. Experimental data-driven tumor modeling for chemotherapy. IFACPapersOnline 2020, 53, 16245–16250. [Google Scholar] [CrossRef]
- Drexler, D.A.; Sápi, J.; Kovács, L. Modeling of tumor growth incorporating the effects of necrosis and the effect of bevacizumab. Complexity 2017, 2017, 5985031. [Google Scholar] [CrossRef] [Green Version]
- Leszczyński, M.; Ledzewicz, U.; Schättler, H. Optimal control for a mathematical model for chemotherapy with pharmacometrics. Math. Model. Nat. Phenom. 2020, 15, 69. [Google Scholar] [CrossRef] [Green Version]
- Ghita, M.; Drexler, D.A.; Kovacs, L.; Copot, D.; Muresan, C.I.; Ionescu, C.M. Model-based management of lung cancer radiation therapy. IFACPapersOnline 2020, 53, 15928–15933. [Google Scholar] [CrossRef]
- Ionescu, C.M.; Ghita, M.; Copot, D.; Derom, E.; Verellen, D. A minimal PKPD Interaction model for evaluating synergy effects of combined NSCLC therapies. J. Clin. Med. 2020, 9, 1832. [Google Scholar] [CrossRef]
- Simeoni, M.; Magni, P.; Cammia, C.; De Nicolao, G.; Croci, V.; Pesenti, E.; Germani, M.; Poggesi, I.; Rocchetti, M. Predictive pharmacokinetic-pharmacodynamic modeling of tumor growth kinetics in xenograft models after administration of anticancer agents. Cancer Res. 2004, 64, 1094–1101. [Google Scholar] [CrossRef] [Green Version]
- Bonate, P.L. Pharmacokinetic-Pharmacodynamic Moodeling and Simulation, 2nd ed.; Springer: London, UK, 2011. [Google Scholar]
- Olarte, O.; De Keyser, R.; Ionescu, C.M. Fan-based device for non-invasive measurement of respiratory impedance. Identification, calibration and analysis. Biomed. Signal. Process Control 2016, 30, 127–133. [Google Scholar] [CrossRef]
- King, G.G.; Bates, J.; Berger, K.I.; Calverley, P.; de Melo, P.L.; Dellacà, R.L.; Farré, R.; Hall, G.L.; Ioan, I.; Irvin, C.G.; et al. Technical standards for respiratory oscillometry. Eur. Respir. J. 2020, 55, 1900753. [Google Scholar] [CrossRef] [PubMed]
- Joiner, M.; van der Kogel, A. (Eds.) Basic Clinical Radiobiology, 4th ed.; Hodder Arnold: London, UK, 2009. [Google Scholar]
- Ionescu, C.M.; Copot, C.; Verellen, D. Motion compensation for robotic lung tumour radiotherapy in remote locations: A personalised medicine approach. Acta Astronaut. 2017, 132, 59–66. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network (NCCN). Clinical Practice Guidelines in Oncology—Non-Small Cell Lung Cancer, Version 7.2021. 29 October 2021. Available online: http://www.nccn.org/patients/guidelines/nscl/index.html (accessed on 19 December 2021).
- Guckenberger, M.; Andratschke, N.; Dieckmann, K.; Hoogeman, M.S.; Hoyer, M.; Hurkmans, C.; Tanadini-Lang, S.; Lartigau, E.; Méndez Romero, A.; Senan, S.; et al. ESTRO ACROP consensus guideline on implementation and practice of stereotactic body radiotherapy for peripherally located early stage, non-small cell lung cancer. Radiother. Oncol. 2017, 124, 11–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Postmus, P.E.; Kerr, K.M.; Oudkerk, M.; Senan, S.; Waller, D.A.; Vansteenkiste, J.; Escriu, C.; Peters, S. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2017, 28, iv1–iv21. [Google Scholar] [CrossRef] [PubMed]
- Remon, J.; Soria, J.C.; Peters, S. Early and locally advanced non-small-cell lung cancer: An update of the ESMO Clinical Practice Guidelines focusing on diagnosis, staging, systemic and local therapy. Ann. Oncol. 2021, 32, 1637–1642. [Google Scholar] [CrossRef] [PubMed]
- Planchard, D.; Popat, S.; Kerr, K.; Novello, S.; Smit, E.F.; Faivre-Finn, C.; Mok, T.S.; Reck, M.; Van Schil, P.E.; Hellmann, M.D.; et al. Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2018, 29, iv192–iv237. [Google Scholar] [CrossRef]
- Billiet, C.; Joye, I.; Mercier, C.; Depuydt, L.; De Kerf, G.; Vermeulen, P.; Van Laere, S.; Van de Kelft, E.; Meijnders, P.; Verellen, D.; et al. Outcome and toxicity of hypofractionated image-guided SABR for spinal oligometastases. Clin. Transl. Radiat.Oncol. 2020, 24, 65–70. [Google Scholar] [CrossRef]
- Saez, J.; Hernandez, V.; Goossens, J.; De Kerf, G.; Verellen, D. A novel procedure for determining the optimal: MLC. configuration parameters in treatment planning systems based on measurements with a Farmer chamber. Phys. Med. Biol. 2020, 65, 155006. [Google Scholar] [CrossRef]
- Benedict, S.H.; Yenice, K.M.; Followill, D.; Galvin, J.M.; Hinson, W.; Kavanagh, B.; Keall, P.; Lovelock, M.; Meeks, S.; Papiez, L.; et al. Stereotactic body radiation therapy: The report of AAPM Task Group 101. Med. Phys. 2010, 37, 4078–4101. [Google Scholar] [CrossRef] [Green Version]
- Wilke, L.; Andratschke, N.; Blanck, O.; Brunner, T.B.; Combs, S.E.; Grosu, A.-L.; Moustakis, C.; Schmitt, D.; Baus, W.W.; Guckenberger, M. ICRU report 91 on prescribing, recording, and reporting of stereotactic treatments with small photon beams: Statement from the DEGRO/DGMP working group stereotactic radiotherapy and radiosurgery. Strahlenther Onkol. 2019, 195, 193–198. [Google Scholar] [CrossRef]
- Ollivier, L.; Padhani, A.R.; Leclere, J. International criteria for measurement of tumor response. Cancer Imaging 2001, 2, 31–32. [Google Scholar]
- Wang, W.; Xu, Y.; Schipper, M.; Matuszak, M.M.; Ritter, T.; Cao, Y.; Ten Haken, R.K.; Kong, F.-M. Effect of normal lung definition on lung dosimetry and lung toxicity prediction in radiation therapy treatment planning. Int. J. Radiat. Oncol. Biol. Phys. 2013, 86, 956–963. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Billiet, C.; Peeters, S.; De Ruysscher, D. Focus on treatment complications and optimal management: Radiation oncology. Transl. Lung Cancer Res. 2014, 3, 187–191. [Google Scholar] [PubMed]
- Yom, S.S.; Liao, Z.; Liu, H.H.; Tucker, S.L.; Hu, C.; Wei, X.; Wang, X.; Wang, S.; Mohan, R.; Cox, J.D.; et al. Initial evaluation of treatment-related pneumonitis in advanced-stage non-small-cell lung cancer patients treated with concurrent chemotherapy and intensity-modulated radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2007, 68, 94–102. [Google Scholar] [CrossRef]
- Jin, S.Z.; Pan, X.N.; Wu, N.; Jin, G.H.; Liu, S.Z. Whole-body low dose irradiation promotes the efficacy of conventional radiotherapy for cancer and possible mechanisms. Dose-Response 2007, 5, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.; Chen, H. Mathematical rules for synergistic, additive, and antagonistic effects of multi-drug combinations and their application in research and development of combinatorial drugs and special medical food combinations. Food Sci. Hum. Wellness 2019, 8, 136–141. [Google Scholar] [CrossRef]
- Capasso, A.; Lang, J.; Pitts, T.M.; Jordan, K.R.; Lieu, C.H.; Davis, S.L.; Diamond, J.R.; Kopetz, S.; Barbee, J.; Peterson, J.; et al. Characterization of immune responses to anti-PD-1 mono- and combination therapy in hematopoietic humanized mice implanted with tumor xenographs. J. Immunother. Cancer 2019, 7, 37. [Google Scholar] [CrossRef]
- Ionescu, C.M. A computationally efficient Hill curve adaptation strategy during continuous monitoring of dose-effect relation in anesthesia. Nonlinear Dyn. 2018, 92, 843–852. [Google Scholar] [CrossRef]
- Injerd, R.; Turian, E. Mathematical Modeling of Non-Small Cell Lung Cancer Response to Therapy; Technical Report No. 17-0922. 2017. Available online: https://www.neiu.edu/sites/neiu.edu/files/migrated-arts-body/documents/ncwrinkl/Russell_TechnicalReport_Apr2018.pdf (accessed on 11 February 2021).
- Kwon, O.-B.; Yeo, C.-D.; Lee, H.-Y.; Kang, H.-S.; Kim, S.-K.; Kim, J.-S.; Park, C.-K.; Lee, S.-H.; Kim, S.-J.; Kim, J.-W. The value of residual volume/total lung capacity as an indicator for predicting postoperative lung function in non-small lung cancer. J. Clin. Med. 2021, 10, 4159. [Google Scholar] [CrossRef]

| Patients ID | Time between Tumor Measurements (Days ≈ Months) | Total Dose (Gy) | No. of Fractions | Total Duration of RT Treatment (Days) | Days of Treatment | Tumor Colume GTV before RT (cm) | Tumor Volume GTV after RT (cm) | Mean Lung Dose (Gy) | Total Lung Volume (cm) | V5 Lungs (%) | V20 Lungs (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 001 | 191 d ≈ 7 m | 54 | 3 | 6 | 1-3-6 | 0.6 | 0.2 | 1.2 | 4870.8 | 6.1 | 0.9 |
| 002 | 63 d ≈ 2 m | 48 | 4 | 8 | 1-3-5-8 | 0.9 | 0 | 2.7 | 2653.7 | 13 | 2.8 |
| 003 | 123 d ≈ 4 m | 54 | 3 | 6 | 1-3-6 | 1 | 0.5 | 2.4 | 3758.1 | 12 | 1.7 |
| 005 | 126 d ≈ 5 m | 54 | 3 | 6 | 1-3-6 | 0.4 | 0 * | 1.1 | 5031.4 | 5 | 0.9 |
| 006 | 124 d ≈ 4 m | 48 | 4 | 8 | 1-3-5-8 | 4.2 | 1.4 | 2.1 | 5263.3 | 1.6 | 2.1 |
| 008 | 109 d ≈ 4 m | 48 | 4 | 8 | 1-3-6-8 | 18 | 1.5 | 3.4 | 3598.8 | 13.9 | 4.5 |
| 009 | 90 d ≈ 3 m | 54 | 3 | 6 | 1-3-6 | 5.7 | 3.3 | 2.5 | 5485.3 | 12.4 | 3 |
| 010 | 169 d ≈ 6 m | 48 | 4 | 9 | 1-3-6-9 | 4.3 | 2 | 1.9 | 3932.6 | 8.6 | 2 |
| 011 | 172 d ≈ 6 m | 48 | 4 | 8 | 1-3-6-8 | 5.4 | 2.8 | 5.3 | 3340.5 | 34.3 | 4.3 |
| 012 | 98 d ≈ 4 m | 7 | 7.3 | 2335 | 31.5 | 13 | |||||
| les. | 1 | 54 | 3 | 1-4-6 | 1.2 | 1.6 | |||||
| les. | 2 | 54 | 3 | 3-5-7 | 0.9 | 0 | |||||
| les. | 3 | 54 | 3 | 3-5-7 | 0.9 | 0.3 | |||||
| 013 | 125 d ≈ 4 m | 10 | 5 | 2886.4 | 28 | 4.8 | |||||
| les. | 1 | 48 | 4 | 2-6-8-10 | 0.9 | 0.4 | |||||
| les. | 2 | 48 | 4 | 1-3-7-9 | 5.6 | 4.6 | |||||
| 014 | 150 d ≈ 5 m | 54 | 3 | 6 | 1-3-6 | 2.6 | 0 * | 3.7 | 2229 | 15.1 | 6 |
| 015 | 112 d ≈ 4 m | 60 | 8 | 17 | 1-3-6-8-10-13-15-17 | 10.5 | 11 | 4.5 | 3307.4 | 17 | 6.3 |
| 016 | 124 d ≈ 4 m | 48 | 4 | 10 | 1-3-7-10 | 20 | 2.8 | 3.7 | 4477 | 17.5 | 4 |
| 018 | 115 d ≈ 4 m | 54 | 3 | 7 | 1-3-7 | 1.5 | 0.3 | 1 | 4463.8 | 4.5 | 1.3 |
| 019 | 103 d ≈ 4 m | 34 | 1 | 1 | 1 | 0.3 | 0.2 | 1.2 | 3336.3 | 5.9 | 0.7 |
| 020 | 145 d ≈ 5 m | 9 | 1.7 | 2602.2 | 7.6 | 1.7 | |||||
| les. | 1 | 48 | 4 | 1 | 0.6 | 0.6 | |||||
| les. | 2 | 34 | 1 | 2-4-7-9 | 1.1 | 0 | |||||
| 021 | 133 d ≈ 5 m | 48 | 4 | 11 | 1-3-8-11 | 0.6 | 0 * | 1.9 | 2392.4 | 9.6 | 1.6 |
| 022 | 123 d ≈ 4 m | 54 | 3 | 6 | 1-2-6 | 2.1 | 0 * | 3.2 | 2830 | 16.5 | 3.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghita, M.; Billiet, C.; Copot, D.; Verellen, D.; Ionescu, C.M. Model Calibration of Pharmacokinetic-Pharmacodynamic Lung Tumour Dynamics for Anticancer Therapies. J. Clin. Med. 2022, 11, 1006. https://doi.org/10.3390/jcm11041006
Ghita M, Billiet C, Copot D, Verellen D, Ionescu CM. Model Calibration of Pharmacokinetic-Pharmacodynamic Lung Tumour Dynamics for Anticancer Therapies. Journal of Clinical Medicine. 2022; 11(4):1006. https://doi.org/10.3390/jcm11041006
Chicago/Turabian StyleGhita, Maria, Charlotte Billiet, Dana Copot, Dirk Verellen, and Clara Mihaela Ionescu. 2022. "Model Calibration of Pharmacokinetic-Pharmacodynamic Lung Tumour Dynamics for Anticancer Therapies" Journal of Clinical Medicine 11, no. 4: 1006. https://doi.org/10.3390/jcm11041006
APA StyleGhita, M., Billiet, C., Copot, D., Verellen, D., & Ionescu, C. M. (2022). Model Calibration of Pharmacokinetic-Pharmacodynamic Lung Tumour Dynamics for Anticancer Therapies. Journal of Clinical Medicine, 11(4), 1006. https://doi.org/10.3390/jcm11041006








