Occult Non-Small Cell Lung Cancer: An Underappreciated Disease
Abstract
:1. Background
2. Methods
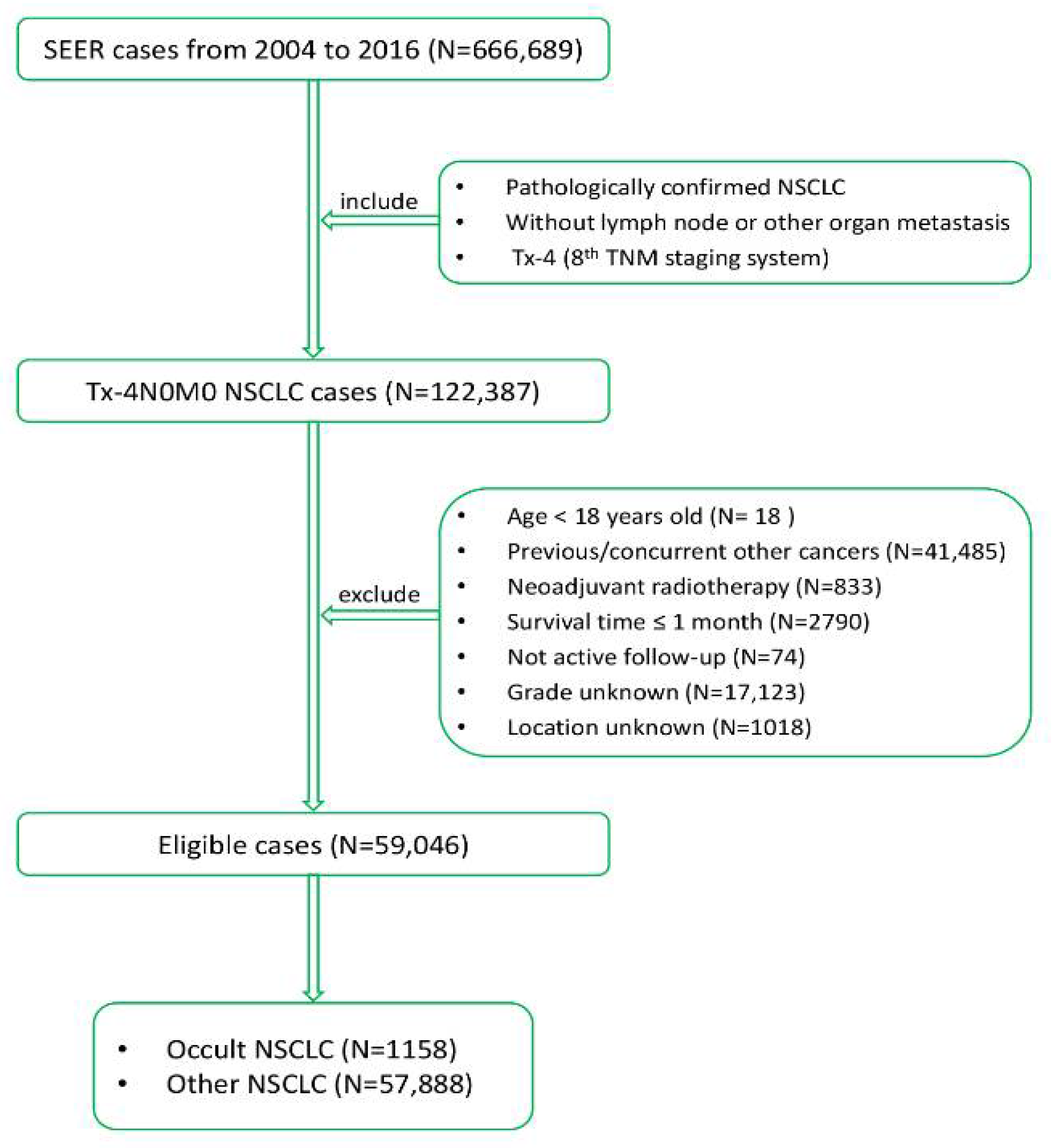
2.1. Patient Selection
2.2. Data Collection
2.3. Follow-Up
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. LASSO Penalized Multivariate Cox Regression Analysis
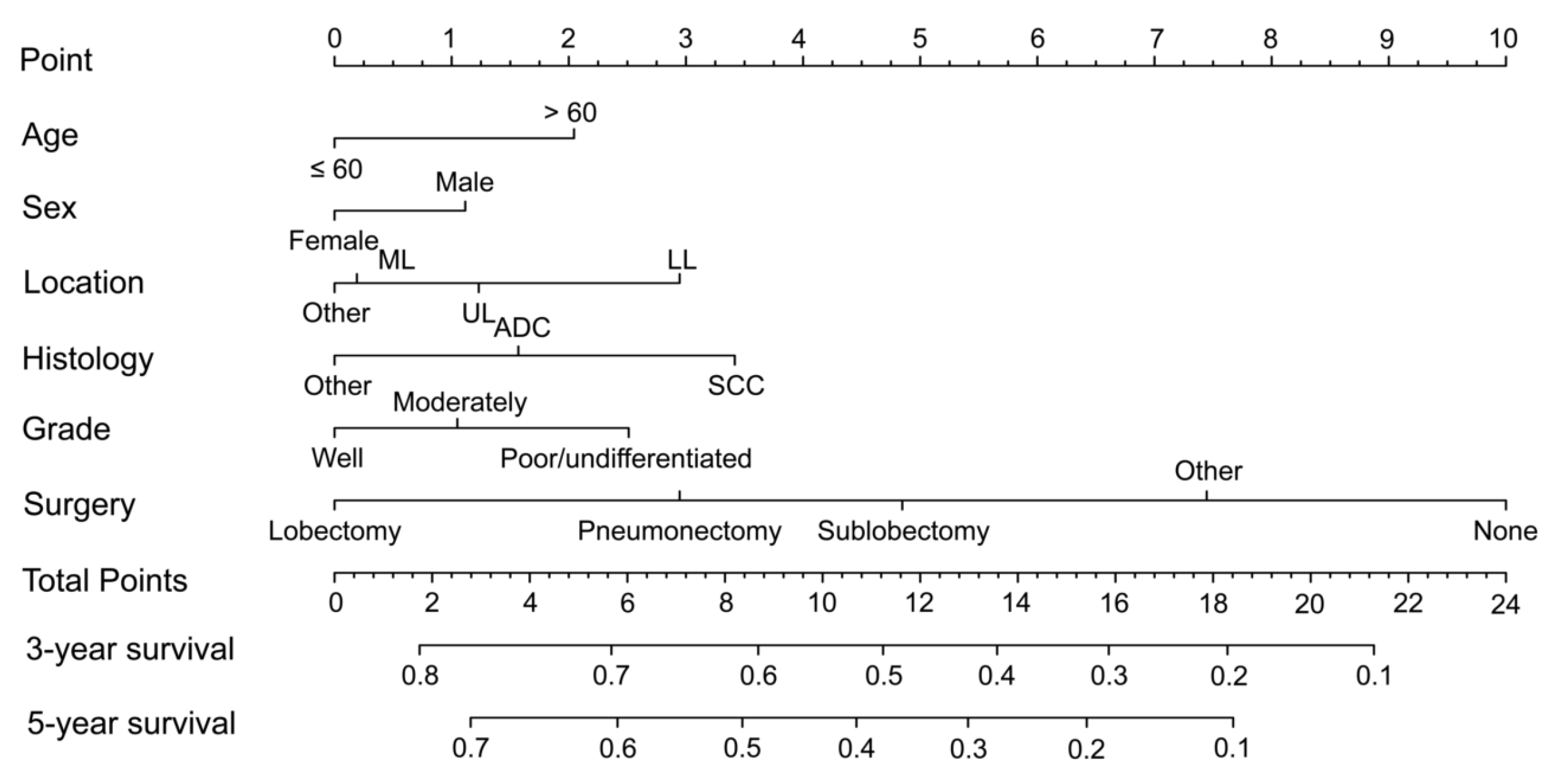
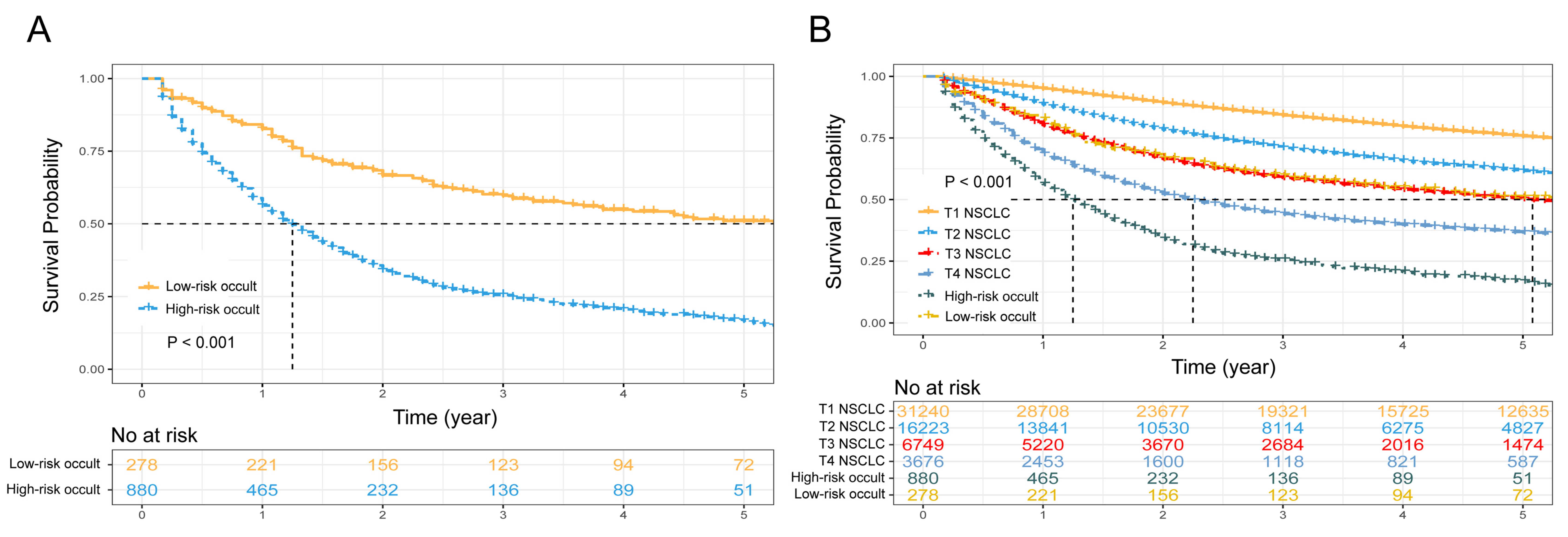
3.3. Nomogram and Risk-Classifying System
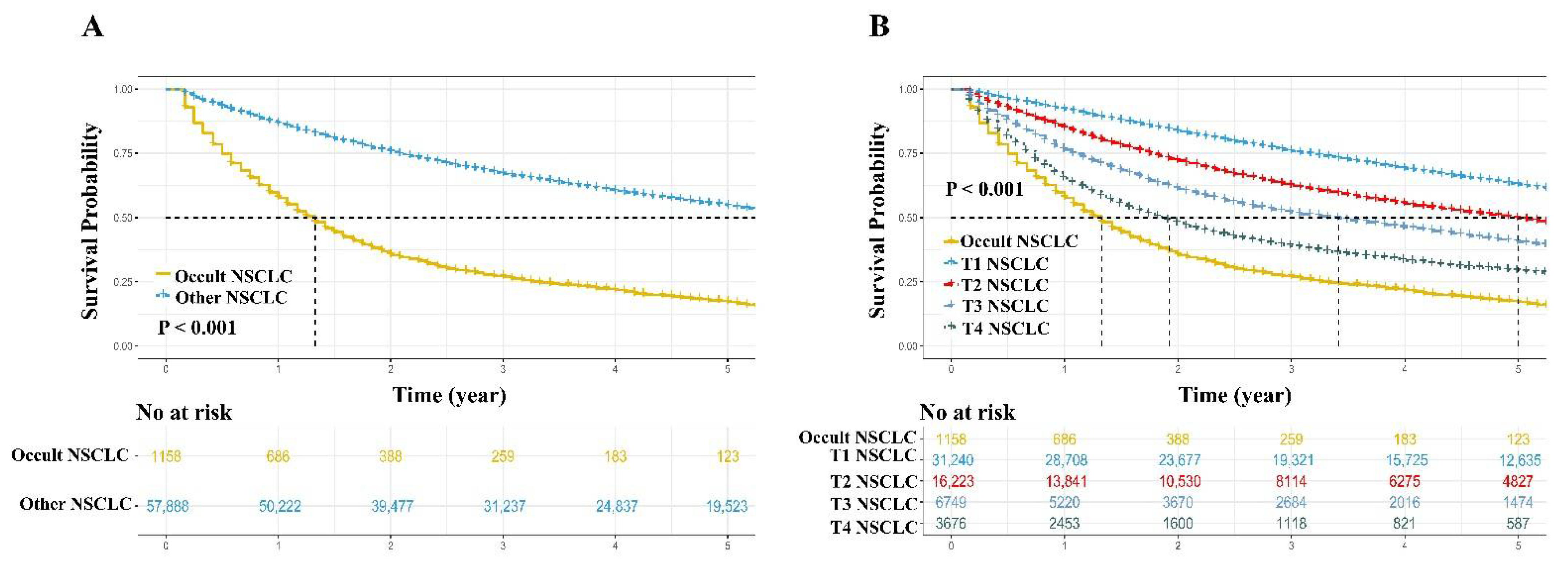
3.4. Survival Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| NSCLC | non-small cell lung cancer |
| LASSO | least absolute shrinkage and selection operator |
| OS | overall survival |
| TNM | tumor-node-metastasis |
| SEER | Surveillance |
| HR | hazard ratio |
| CI | confidential interval |
| SD | standard deviation |
| UL | upper lobe |
| ML | middle lobe |
| LL | low lobe |
| ADC | adenocarcinoma |
| SCC | squamous cell carcinoma |
References
- Petty, T.L.; Tockman, M.S.; Palcic, B. Diagnosis of roentgenographically occult lung cancer by sputum cytology. Clin. Chest Med. 2002, 23, 59–64. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network. Non-Small Cell Lung Cancer (Version 4.2021). 2021. Available online: https://www.nccn.org/professionals/physician__gls/pdf/nscl.pdf (accessed on 5 March 2021).
- Nivar, I.; Panico, L.C.; Yoo, C.; Parrish, W. Trapezial Acrometastasis as the First Presentation of Occult Lung Cancer: A Case Report. JBJS Case Connect. 2021, 11, e20. [Google Scholar] [CrossRef] [PubMed]
- Kaur, H.; Mishra, D.; Manchanda, S.; Bhutia, O. Mandibular tumour as the primary manifestation of an occult adenocarcinoma. BMJ Case Rep. 2021, 14, e239151. [Google Scholar] [CrossRef] [PubMed]
- Gilardi, R.; Della Rosa, N.; Pancaldi, G.; Landi, A. Acrometastasis showing an occult lung cancer. J. Plast. Surg. Hand Surg. 2013, 47, 550–552. [Google Scholar] [CrossRef]
- Tybjerg, A.J.; Babore, A.D.; Olsen, T.S.; Andersen, K.K. Types of occult cancer in stroke and the relation to smoking. Acta Neurol. Scand. 2020, 142, 486–492. [Google Scholar] [CrossRef]
- Scopelliti, G.; Bertora, P.; Bortolami, C.; Rosa, S.; Pantoni, L. Ischemic stroke caused by giant cell arteritis associated with pulmonary adenocarcinoma. J. Clin. Neurosci. 2019, 72, 485–486. [Google Scholar] [CrossRef]
- Babore, A.D.; Tybjerg, A.J.; Andersen, K.K.; Olsen, T.S. Occult lung cancer manifesting within the first year after stroke. J. Stroke Cerebrovasc. Dis. 2020, 29, 105023. [Google Scholar] [CrossRef]
- Navi, B.B.; DeAngelis, L.M.; Segal, A.Z. Multifocal strokes as the presentation of occult lung cancer. J. Neuro-Oncol. 2007, 85, 307–309. [Google Scholar] [CrossRef]
- Nose, T.; Imamura, Y.; Ohata, S.; Kimbara, S.; Miyata, Y.; Hyogo, Y.; Fujishima, Y.; Funakoshi, Y.; Toyoda, M.; Kiyota, N.; et al. Incidence of venous thromboembolism in patients with solid cancers in Japan: Retrospective study of 2735 patients. Int. J. Hematol. 2021, 114, 319–324. [Google Scholar] [CrossRef]
- Galarza Fortuna, G.M.; Singh, A.; Jacobs, A.; Ugalde, I. Lung Adenocarcinoma Presenting as Multiple Thromboembolic Events: A Case Report and Review of the Literature. J. Investig. Med. High Impact Case Rep. 2020, 8, 2324709620969482. [Google Scholar] [CrossRef]
- Li, X.; Tan, H. Value of (18)F-FDG PET/CT in the detection of occult malignancy in patients with dermatomyositis. Heliyon 2020, 6, e03707. [Google Scholar] [CrossRef]
- Goldstraw, P.; Chansky, K.; Crowley, J.; Rami-Porta, R.; Asamura, H.; Eberhardt, W.E.; Nicholson, A.G.; Groome, P.; Mitchell, A.; Bolejack, V.; et al. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J. Thorac. Oncol. 2016, 11, 39–51. [Google Scholar] [CrossRef] [Green Version]
- Iasonos, A.; Schrag, D.; Raj, G.V.; Panageas, K.S. How to Build and Interpret a Nomogram for Cancer Prognosis. J. Clin. Oncol. 2008, 26, 1364–1370. [Google Scholar] [CrossRef]
- Balachandran, V.P.; Gonen, M.; Smith, J.J.; DeMatteo, R.P. Nomograms in oncology: More than meets the eye. Lancet Oncol. 2015, 16, e173–e180. [Google Scholar] [CrossRef] [Green Version]
- Harrell, F.E.; Califf, R.M.; Pryor, D.B.; Lee, K.L.; A Rosati, R. Evaluating the yield of medical tests. JAMA 1982, 247, 2543–2546. [Google Scholar] [CrossRef] [PubMed]
- Camp, R.L.; Dolled-Filhart, M.; Rimm, D.L. X-tile: A new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin. Cancer Res. 2004, 10, 7252–7259. [Google Scholar] [CrossRef] [Green Version]
- Dai, D.; Jin, H.; Wang, X. Nomogram for predicting survival in triple-negative breast cancer patients with histology of infiltrating duct carcinoma: A population-based study. Am. J. Cancer Res. 2018, 8, 1576–1585. [Google Scholar]
- Kim, S.Y.; Yoon, M.J.; Park, Y.I.; Kim, M.J.; Nam, B.-H.; Park, S.R. Nomograms predicting survival of patients with unresectable or metastatic gastric cancer who receive combination cytotoxic chemotherapy as first-line treatment. Gastric Cancer 2017, 21, 453–463. [Google Scholar] [CrossRef] [Green Version]
- Dou, X.-M.; Zhang, N.; Fang, Y.-Y.; Zhang, B.-H.; Liao, J.-J.; Cai, J.-S.; Li, J.-B. Prognostic nomograms and risk-stratifying systems for predicting survival in patients with resected pT2-4aN0M0 esophageal carcinoma. J. Thorac. Dis. 2021, 13, 2363–2377. [Google Scholar] [CrossRef]
- Wu, L.-L.; Chen, W.-T.; Liu, X.; Jiang, W.-M.; Huang, Y.-Y.; Lin, P.; Long, H.; Zhang, L.-J.; Ma, G.-W. A Nomogram to Predict Long-Term Survival Outcomes of Patients Who Undergo Pneumonectomy for Non-small Cell Lung Cancer with Stage I-IIIB. Front. Surg. 2021, 8, 604880. [Google Scholar] [CrossRef]
- Cai, J.-S.; Dou, X.-M.; Li, J.-B.; Yang, M.-Z.; Xie, C.-L.; Hou, X.; Yang, H.-X. Nomogram to Predict Cancer Specific Survival in Patients with Pathological Stage IA Non-small Cell Lung Cancer. Semin. Thorac. Cardiovasc. Surg. 2021. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Liu, X.; Jiang, W.-M.; Huang, W.; Lin, P.; Long, H.; Zhang, L.-J.; Ma, G.-W. Stratification of Patients with Stage IB NSCLC Based on the 8th Edition of the American Joint Committee on Cancer (AJCC) Staging Manual. Front. Oncol. 2020, 10, 571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, L.-L.; Li, C.-W.; Lin, W.-K.; Qiu, L.-H.; Xie, D. Incidence and survival analyses for occult lung cancer between 2004 and 2015: A population-based study. BMC Cancer 2021, 21, 1009. [Google Scholar] [CrossRef] [PubMed]
- Bechtel, J.J.; Petty, T.L.; Saccomanno, G. Five year survival and later outcome of patients with X-ray occult lung cancer detected by sputum cytology. Lung Cancer 2000, 30, 1–7. [Google Scholar] [CrossRef]
- A Cortese, D.; Pairolero, P.C.; Bergstralh, E.J.; Woolner, L.B.; A Uhlenhopp, M.; Piehler, J.M.; Sanderson, D.R.; E Bernatz, P.; E Williams, D.; Taylor, W.F.; et al. Roentgenographically occult lung cancer. A ten-year experience. J. Thorac. Cardiovasc. Surg. 1983, 86, 373–380. [Google Scholar] [CrossRef]


| Characteristics | Occult NSCLC (N = 1158) | Other NSCLC (N = 57,888) | p |
|---|---|---|---|
| No. of Patients (%) | No. of Patients (%) | ||
| Age, year | |||
| Mean ± SD | 71.9 ± 10.5 | 68.7 ± 10.1 | <0.001 a |
| Median (range) | 73 (33–95) | 69 (18–98) | |
| ≤60 | 181 (15.6) | 11,852 (20.5) | <0.001 |
| >60 | 977 (84.8) | 46,036 (79.5) | |
| Sex | <0.001 | ||
| Male | 627 (54.1) | 28,108 (48.6) | |
| Female | 531 (45.9) | 29,780 (51.4) | |
| Ethnicity | <0.001 | ||
| Caucasian | 934 (80.7) | 48,700 (84.1) | |
| African | 151 (13.0) | 5271 (9.1) | |
| Other b | 73 (6.3) | 3917 (6.8) | |
| Marital status | <0.001 | ||
| Married | 553 (47.8) | 31,431 (54.3) | |
| Other | 605 (52.2) | 26,457 (45.7) | |
| Location | <0.001 | ||
| UL | 642 (55.4) | 35,138 (60.7) | |
| ML | 65 (5.6) | 2985 (5.2) | |
| LL | 401 (34.6) | 18,520 (32.0) | |
| Other | 50 (4.3) | 1245 (2.2) | |
| Surgery type | <0.001 | ||
| None | 976 (84.3) | 11,760 (20.3) | |
| Lobectomy | 109 (9.4) | 36,250 (62.6) | |
| Pneumonectomy | 2 (0.2) | 1073 (1.9) | |
| Sublobectomy | 32 (2.8) | 8206 (14.2) | |
| Other | 39 (3.4) | 599 (1.0) | |
| Histology | <0.001 | ||
| ADC | 548 (47.3) | 33,583 (58.5) | |
| SCC | 551 (47.6) | 19,414 (33.5) | |
| Other | 59 (5.1) | 4621 (8.0) | |
| Grade | 0.001 | ||
| Well | 225 (19.4) | 10,481 (18.1) | |
| Moderate | 446 (38.5) | 25,565 (44.2) | |
| Poor/undifferentiated | 487 (42.1) | 21,842 (37.7) | |
| Radiotherapy | <0.001 | ||
| No | 1130 (97.6) | 55,051 (95.1) | |
| Yes | 28 (2.4) | 2837 (4.9) | |
| Chemotherapy | <0.001 | ||
| No | 862 (74.4) | 47,861 (82.7) | |
| Yes | 296 (25.6) | 10,027 (17.3) |
| Characteristics | Multivariate Analysis | ||
|---|---|---|---|
| HR | 95% CI | p | |
| Age, year | 0.011 | ||
| ≤60 | 1 | ||
| >60 | 1.277 | 1.057–1.544 | |
| Sex | 0.020 | ||
| Male | 1 | ||
| Female | 0.849 | 0.739–0.975 | |
| Ethnicity | 0.112 | ||
| Caucasian | 1 | ||
| African | 0.876 | 0.723–1.061 | |
| Other b | 0.784 | 0.592–1.038 | |
| Marital status | 0.215 | ||
| Married | 1 | ||
| Other | 1.091 | 0.951–1.253 | |
| Location | 0.013 | ||
| UL | 1 | ||
| ML | 0.893 | 0.655–1.217 | |
| LL | 1.219 | 1.062–1.399 | |
| Other | 0.880 | 0.633–1.224 | |
| Surgery type | <0.001 | ||
| None | 1 | ||
| Lobectomy | 0.310 | 0.235–0.408 | |
| Pneumonectomy | 0.440 | 0.109–1.774 | |
| Sublobectomy | 0.545 | 0.355–0.836 | |
| Other | 0.737 | 0.512–1.061 | |
| Histology | 0.006 | ||
| ADC | 1 | ||
| SCC | 1.220 | ||
| Other | 0.822 | 0.586 | |
| Grade | 0.002 | ||
| Well | 1 | ||
| Moderate | 1.147 | 0.940–1.396 | |
| Poor/undifferentiated | 1.376 | 1.129–1.677 | |
| Radiotherapy | 0.506 | ||
| No | 1 | ||
| Yes | 0.861 | 0.555–1.337 | |
| Chemotherapy a | |||
| No | |||
| Yes | |||
| Characteristics | Category | Score |
|---|---|---|
| Age | ≤60 | 0 |
| >60 | 2 | |
| Sex | Male | 1 |
| Female | 0 | |
| Location | UL | 1 |
| ML | 0 | |
| LL | 3 | |
| Other | 0 | |
| Surgery | None | 10 |
| Lobectomy | 0 | |
| Pneumonectomy | 3 | |
| Sublobectomy | 5 | |
| Other | 7 | |
| Grade | Well | 0 |
| Moderate | 1 | |
| Poor/undifferentiated | 3 | |
| Histology | ADC | 2 |
| SCC | 3 | |
| Other | 0 | |
| Risk-classifying system (cutoff value = 15) | ||
| Low-risk | ≤15 | |
| High-risk | >15 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cai, J.; Yang, F.; Wang, X. Occult Non-Small Cell Lung Cancer: An Underappreciated Disease. J. Clin. Med. 2022, 11, 1399. https://doi.org/10.3390/jcm11051399
Cai J, Yang F, Wang X. Occult Non-Small Cell Lung Cancer: An Underappreciated Disease. Journal of Clinical Medicine. 2022; 11(5):1399. https://doi.org/10.3390/jcm11051399
Chicago/Turabian StyleCai, Jingsheng, Fan Yang, and Xun Wang. 2022. "Occult Non-Small Cell Lung Cancer: An Underappreciated Disease" Journal of Clinical Medicine 11, no. 5: 1399. https://doi.org/10.3390/jcm11051399
APA StyleCai, J., Yang, F., & Wang, X. (2022). Occult Non-Small Cell Lung Cancer: An Underappreciated Disease. Journal of Clinical Medicine, 11(5), 1399. https://doi.org/10.3390/jcm11051399






