Trends in Caesarean Section Rate According to Robson Group Classification among Pregnant Women with SARS-CoV-2 Infection: A Single-Center Large Cohort Study in Italy
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Coronavirus Disease (COVID-19) Dashboard|WHO Coronavirus Disease (COVID-19) Dashboard (n.d.). Available online: https://covid19.who.int/table (accessed on 29 December 2020).
- Muralidar, S.; Ambi, S.V.; Sekaran, S.; Krishnan, U.M. The emergence of COVID-19 as a global pandemic: Understanding the epidemiology, immune response, and potential therapeutic targets of SARSCoV-2. Biochimie 2020, 179, 85–100. [Google Scholar] [CrossRef] [PubMed]
- Parazzini, F.; Bortolus, R.; Mauri, P.A.; Favilli, A.; Gerli, S.; Ferrazzi, E. Delivery in pregnant women infected with SARS-CoV-2: A fast review. Int. J. Gynaecol. Obstet. 2020, 150, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Goyal, M.; Singh, P.; Melana, N. Review of care and management of pregnant women during COVID-19 pandemic. Taiwan J. Obstet. Gynecol. 2020, 59, 791–794. [Google Scholar] [CrossRef] [PubMed]
- Alhousseini, A.; Turkoglu, O.; Sajja, S.; Wharton, K.; Idler, J.; Bahado-Singh, R. Does Maternal SARS-CoV-2 Infection or SARS-CoV-2 Vaccination trigger an Inflammatory Response in The Fetus? A Prospective Cohort Study. Gynecol. Obstet. Investig. 2022, 87, 219–225. [Google Scholar] [CrossRef]
- Akhtar, H.; Patel, C.; Abuelgasim, E.; Harky, A. COVID-19 (SARS-CoV-2) Infection in Pregnancy: A Systematic Review. Gynecol. Obstet. Investig 2020, 85, 295–306. [Google Scholar] [CrossRef] [PubMed]
- Shen, W.B.; Turan, S.; Wang, B.; Cojocaru, L.; Harman, C.; Logue, J.; Reece, E.A.; Frieman, M.B.; Yang, P. A SARS-CoV-2 Delta Variant Case Manifesting as Extensive Placental Infection and Fetal Transmission. Gynecol. Obstet. Investig. 2022, 87, 165–172. [Google Scholar] [CrossRef] [PubMed]
- World Association of Perinatal Medicine (WAPM) Working Group on COVID-19. Maternal and perinatal outcomes of pregnant women with SARS-CoV-2 infection. Ultrasound Obstet Gynecol. 2021, 57, 232–241. [Google Scholar] [CrossRef] [PubMed]
- Di Mascio, D.; Sen, C.; Saccone, G.; Galindo, A.; Grünebaum, A.; Yoshimatsu, J.; Stanojevic, M.; Kurjak, A.; Chervenak, F.; Rodríguez Suárez, M.J.; et al. Risk factors associated with adverse fetal outcomes in pregnancies affected by Coronavirus disease 2019 (COVID-19): A secondary analysis of the WAPM study on COVID-19. J. Perinat. Med. 2020, 48, 950–958. [Google Scholar] [CrossRef]
- D'Antonio, F.; Sen, C.; Mascio, D.D.; Galindo, A.; Villalain, C.; Herraiz, I.; Arisoy, R.; Ovayolu, A.; Eroğlu, H.; Canales, M.G.; et al. Maternal and perinatal outcomes in high compared to low risk pregnancies complicated by severe acute respiratory syndrome coronavirus 2 infection (phase 2): The World Association of Perinatal Medicine working group on coronavirus disease 2019. Am. J. Obstet. Gynecol. MFM 2021, 3, 100329. [Google Scholar] [CrossRef]
- Carbone, L.; Esposito, R.; Raffone, A.; Verrazzo, P.; Carbone, I.F.; Saccone, G. Proposal for radiologic diagnosis and follow-up of COVID-19 in pregnant women. J. Matern Fetal Neonatal Med. 2020, 16, 1–2. [Google Scholar] [CrossRef]
- Carbone, L.; Raffone, A.; Sarno, L.; Travaglino, A.; Saccone, G.; Gabrielli, O.; Migliorini, S.; Sirico, A.; Genesio, R.; Castaldo, G.; et al. Invasive prenatal diagnosis during COVID-19 pandemic. Arch. Gynecol. Obstet. 2021, 305, 797–801. [Google Scholar] [CrossRef] [PubMed]
- Carbone, L.; Raffone, A.; Travaglino, A.; Sarno, L.; Conforti, A.; Gabrielli, O.; De Vivo, V.; De Rosa, M.; Migliorini, S.; Saccone, G.; et al. Obstetric A&E unit admission and hospitalization for obstetrical management during COVID-19 pandemic in a third-level hospital of southern Italy. Arch. Gynecol. Obstet. 2021, 29, 1–9. [Google Scholar] [CrossRef]
- Poon, L.C.; Yang, H.; Kapur, A.; Melamed, N.; Dao, B.; Divakar, H.; McIntyre, H.D.; Kihara, A.B.; Ayres-de-Campos, D.; Ferrazzi, E.M.; et al. Global interim guidance on coronavirus disease 2019 (COVID-19) during pregnancy and puerperium from FIGO and allied partners: Information for healthcare professionals. Int. J. Gynaecol. Obstet. 2020, 149, 273–286. [Google Scholar] [CrossRef] [PubMed]
- De Georgeo, M.R.; De Georgeo, J.M.; Egan, T.M.; Klee, K.P.; Schwemm, M.S.; Bye-Kollbaum, H.; Kinser, A.J. Containing SARS-CoV-2 in hospitals facing finite PPE, limited testing, and physical space variability: Navigating resource constrained enhanced traffic control bundling. J. Microbiol. Immunol. Infect. 2021, 54, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Sheil, O.; McAuliffe, F.M. Reorganisation of obstetric services during the COVID pandemic-Experience from National Maternity Hospital Dublin Ireland. Best Pract. Res. Clin. Obstet. Gynaecol. 2021, 73, 104–112. [Google Scholar] [CrossRef] [PubMed]
- López, M.; Gonce, A.; Meler, E.; Plaza, A.; Hernández, S.; Martinez-Portilla, R.J.; Cobo, T.; García, F.; Gómez Roig, M.D.; Gratacós, E.; et al. Coronavirus Disease 2019 in Pregnancy: A Clinical Management Protocol and Considerations for Practice. Fetal Diagn. Ther. 2020, 47, 519–528. [Google Scholar] [CrossRef]
- Kumar, R.; Yeni, C.M.; Utami, N.A.; Masand, R.; Asrani, R.K.; Patel, S.K.; Kumar, A.; Yatoo, M.I.; Tiwari, R.; Natesan, S.; et al. SARS-CoV-2 infection during pregnancy and pregnancy-related conditions: Concerns, challenges, management, and mitigation strategies-a narrative review. J. Infect Public Health 2021, 14, 863–875. [Google Scholar] [CrossRef]
- Chen, L.; Li, Q.; Zheng, D.; Jiang, H.; Wei, Y.; Zou, L.; Feng, L.; Xiong, G.; Sun, G.; Wang, H.; et al. Clinical Characteristics of Pregnant Women with COVID-19 in Wuhan, China. N. Engl. J. Med. 2020, 382, e100. [Google Scholar] [CrossRef]
- Robson, M.S. Classification of caesarean sections. Fetal Matern. Med. Rev. 2001, 12, 23–39. [Google Scholar] [CrossRef]
- Triep, K.; Torbica, N.; Raio, L.; Surbek, D.; Endrich, O. The Robson classification for caesarean section—A proposed method based on routinely collected health data. PLoS ONE 2020, 15, e0242736. [Google Scholar] [CrossRef]
- Rudey, E.L.; Leal, M.D.C.; Rego, G. Cesarean section rates in Brazil: Trend analysis using the Robson classification system. Medicine 2020, 99, e19880. [Google Scholar] [CrossRef] [PubMed]
- Vogel, J.P.; Betrán, A.P.; Vindevoghel, N.; Souza, J.P.; Torloni, M.R.; Zhang, J.; Tunçalp, Ö.; Mori, R.; Morisaki, N.; Ortiz-Panozo, E.; et al. Use of the Robson classification to assess caesarean section trends in 21 countries: A secondary analysis of two WHO multicountry surveys. Lancet Glob. Health. 2015, 3, e260–e270. [Google Scholar] [CrossRef]
- Debrabandere, M.L.; Farabaugh, D.C.; Giordano, C. A Review on Mode of Delivery during COVID-19 between December 2019 and April 2020. Am. J. Perinatol. 2021, 38, 332–341. [Google Scholar] [CrossRef] [PubMed]
- Prabhu, M.; Cagino, K.; Matthews, K.C.; Friedlander, R.L.; Glynn, S.M.; Kubiak, J.M.; Yang, Y.J.; Zhao, Z.; Baergen, R.N.; DiPace, J.I.; et al. Pregnancy and postpartum outcomes in a universally tested population for SARS-CoV-2 in New York City: A prospective cohort study. BJOG Int. J. Obstet. Gynaecol. 2020, 127, 1548–1556. [Google Scholar] [CrossRef] [PubMed]
- Knight, M.; Bunch, K.; Vousden, N.; Morris, E.; Simpson, N.; Gale, C.; O’Brien, P.; Quigley, M.; Brocklehurst, P.; Kurinczuk, J.J. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: National population based cohort study. BMJ 2020, 369, m2107. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, A.M.; Ganatra, A.M.; Tank, P. Preliminary Results from the FOGSI's National Registry on Pregnancy with COVID-19. J. Obstet. Gynaecol. India 2021, 71, 1–8. [Google Scholar] [CrossRef]
- Malhotra, Y.; Miller, R.; Bajaj, K.; Sloma, A.; Wieland, D.; Wilcox, W. No change in cesarean section rate during COVID-19 pandemic in New York City. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 253, 328–329. [Google Scholar] [CrossRef]
- Gurol-Urganci, I.; Jardine, J.E.; Carroll, F.; Draycott, T.; Dunn, G.; Fremeaux, A.; Harris, T.; Hawdon, J.; Morris, E.; Muller, P.; et al. Maternal and perinatal outcomes of pregnant women with SARS-CoV-2 infection at the time of birth in England: National cohort study. Am. J. Obstet. Gynecol. 2021, 225, 522.e1–522.e11. [Google Scholar] [CrossRef]
- Adhikari, E.H.; SoRelle, J.A.; McIntire, D.D.; Spong, C.Y. Increasing severity of COVID-19 in pregnancy with Delta (B.1.617.2) variant surge. Am. J. Obstet. Gynecol. 2021, 226, 149–151. [Google Scholar] [CrossRef]
- Seasely, A.R.; Blanchard, C.T.; Arora, N.; Battarbee, A.N.; Casey, B.M.; Dionne-Odom, J.; Leal SMJr Moates, D.B.; Sinkey, R.G.; Szychowski, J.M.; Tita, A.T.; et al. Maternal and Perinatal Outcomes Associated With the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Delta (B.1.617.2) Variant. Obstet. Gynecol. 2021, 138, 842–844. [Google Scholar] [CrossRef]
- Carbone, L.; Mappa, I.; Sirico, A.; Di Girolamo, R.; Saccone, G.; Di Mascio, D.; Donadono, V.; Cuomo, L.; Gabrielli, O.; Migliorini, S.; et al. Pregnant women’s perspectives on severe acute respiratory syndrome coronavirus 2 vaccine. Am. J. Obstet. Gynecol. MFM 2021, 3, 100352. [Google Scholar] [CrossRef] [PubMed]
- Mappa, I.; Luviso, M.; Distefano, F.A.; Carbone, L.; Maruotti, G.M.; Rizzo, G. Women perception of SARS-CoV-2 vaccination during pregnancy and subsequent maternal anxiety: A prospective observational study. J. Matern Fetal Neonatal Med. 2021, 11, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Carbone, L.; Di Girolamo, R.; Mappa, I.; Saccone, G.; Raffone, A.; Di Mascio, D.; De Vivo, V.; D’Antonio, F.; Guida, M.; Rizzo, G.; et al. Worldwide beliefs among pregnant women on SARS-CoV-2 vaccine: A systematic review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 268, 144–164. [Google Scholar] [CrossRef] [PubMed]
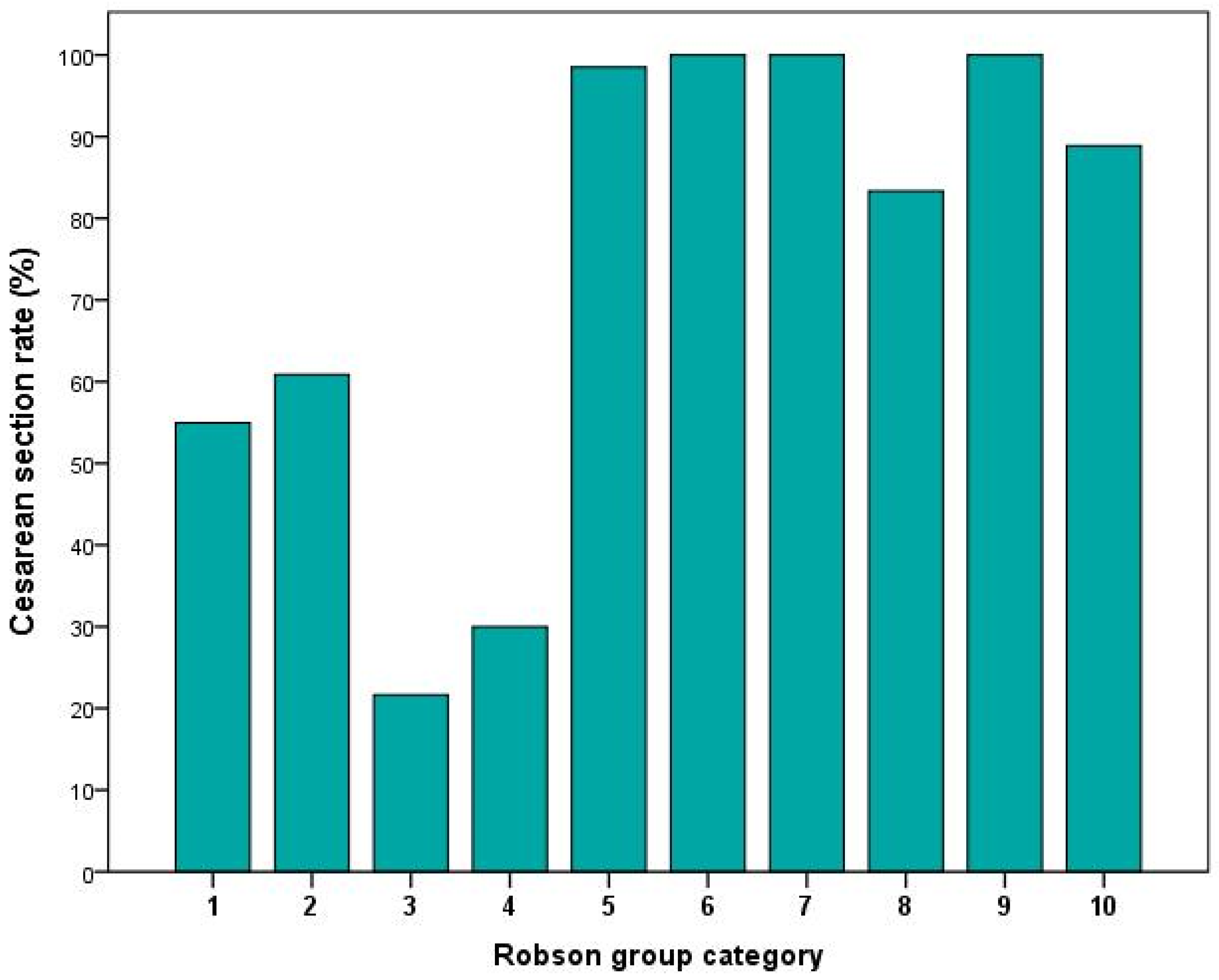

| Robson Group | Description |
|---|---|
| Group 1 | Nulliparous, single cephalic, ≥37 weeks, in spontaneous labor. |
| Group 2 | Nulliparous, single cephalic, ≥37 weeks, induced or CS before labor. |
| Group 3 | Multiparous (excluding previous caesarean section), singleton, cephalic, ≥37 weeks’ gestation, in spontaneous labor. |
| Group 4 | Multiparous without a previous uterine scar, with singleton, cephalic pregnancy, ≥37 weeks’ gestation, induced or caesarean section before labor. |
| Group 5 | Previous caesarean section, singleton, cephalic, ≥37 weeks’ gestation. |
| Group 6 | All nulliparous with a single breech. |
| Group 7 | All multiparous with a single breech (including previous caesarean section). |
| Group 8 | All multiple pregnancies (including previous caesarean section). |
| Group 9 | All women with a single pregnancy in transverse or oblique lie (including those with previous caesarean section). |
| Group 10 | All singleton, cephalic, <37 weeks’ gestation pregnancies (including previous caesarean section). |
| N = 457 | p * | |
|---|---|---|
| Maternal age | 30 [8] | 0.004 |
| Maternal pregestational BMI | 30.1 [6.7] | <0.001 |
| Maternal GWG | 11.25 [6] | <0.001 |
| FGR | 24 (5.2%) | |
| Maternal hyperglycemia | 36 (7.9%) | |
| Maternal hypertension | 30 (6.6%) | |
| pPROM | 9 (2%) | |
| Induction of labor | 31 (6.8%) | |
| GA at delivery | 39 [2] | <0.001 |
| Preterm birth | 65 (14.3%) | |
| Neonatal weight < 2500 | 48 (10.5%) | |
| Neonatal weight < 1500 | 14 (3.1%) | |
| CS delivery | 291 (63.7%) | |
| Urgent CS for respiratory distress | 22 (4.8%) | |
| Robson category 1 | 151 (33%) | |
| Robson category 2 | 23 (5%) | |
| Robson category 3 | 97 (21.2%) | |
| Robson category 4 | 10 (2.2%) | |
| Robson category 5 | 133 (29.1) | |
| Robson category 6 | 8 (1.8%) | |
| Robson category 7 | 1 (0.2%) | |
| Robson category 8 | 6 (1.3%) | |
| Robson category 9 | 1 (0.2%) | |
| Robson category 10 | 27 (5.9%) |
| Mar–Dec 2020 (n = 222) | Jan–April 2021 (n = 134) | May–Nov 2021 (n = 101) | p * | |
|---|---|---|---|---|
| Maternal age (years) | 30 [7] | 30 [9] | 31 [8] | 0.890 |
| Maternal pregestational BMI (m2/kg) | 30.2 [5.1] | 30.3 [7.6] | 29.9 [7.1] | 0.999 |
| Maternal GWG (kg) | 12 [5] | 12 [7] | 10 [6] | 0.330 |
| FGR | 9 (4.1%) | 10 (7.5%) | 5 (5%) | 0.373 |
| Maternal hyperglycemia | 16 (7.2%) | 12 (9%) | 8 (7.9%) | 0.839 |
| Maternal hypertension | 12 (5.9%) | 11 (8.2%) | 7 (6.9) | 0.577 |
| pPROM | 3 (1.4%) | 4 (4%) | 2 (2%) | 0.560 |
| Induction of labor | 8 (3.6%) | 12 (9%) | 11 (10.9%) | 0.027 |
| GA at delivery (weeks) | 39 [1.71] | 38.6 [2.29] | 38.9 [2.29] | 0.021 |
| Preterm birth | 24 (10.9%) | 20 (15.3%) | 21 (20.8%) | 0.017 |
| Neonatal weight < 2500 g | 28 (12.6%) | 9/134 (6.7%) | 11/101 (10.9%) | 0.412 |
| Neonatal weight < 1500 g | 4 (1.8%) | 3 (2.2%) | 6 (5.9%) | 0.057 |
| Delivery by CS | 152 (68.5%) | 81 (60.4%) | 58 (57.4%) | 0.039 |
| Urgent CS for respiratory distress | 8 (3.6%) | 4 (3%) | 10 (9.9%) | 0.032 |
| CS Robson category 1 | 48/80 (60%) | 27/47 (57.4%) | 8/24 (33.3%) | 0.043 |
| CS Robson category 2 | 5/8 (62.5%) | 4/7 (57.1%) | 5/8 (62.5%) | 0.971 |
| CS Robson category 3 | 13/42 (31%) | 6/33 (18.2%) | 2/22 (9.1%) | 0.037 |
| CS Robson category 4 | 2/3 (66.7%) | 0/2 (0%) | 1/5 (20%) | 0.230 |
| CS Robson category 5 | 71/73 (97.3%) | 34/34 (100%) | 26/26 (100%) | 0.244 |
| CS Robson category 6 | 2/2 (100%) | 2/2 (100%) | 4/4 (100%) | N.A. |
| CS Robson category 7 | 1/1 (100%) | / | / | N.A. |
| CS Robson category 8 | 3/3 (100%) | 0/1 (0%) | 2/2 (100%) | 0.853 |
| CS Robson category 9 | / | / | 1/1 (100%) | N.A. |
| CS Robson category 10 | 7/10 (70%) | 8/8 (100%) | 9/9 (100%) | 0.038 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sirico, A.; Carbone, L.; Avino, L.; Buonfantino, C.; De Angelis, M.C.; Cresce, M.D.; Fabozzi, A.; Improda, F.P.; Legnante, A.; Riccardi, C.; et al. Trends in Caesarean Section Rate According to Robson Group Classification among Pregnant Women with SARS-CoV-2 Infection: A Single-Center Large Cohort Study in Italy. J. Clin. Med. 2022, 11, 6503. https://doi.org/10.3390/jcm11216503
Sirico A, Carbone L, Avino L, Buonfantino C, De Angelis MC, Cresce MD, Fabozzi A, Improda FP, Legnante A, Riccardi C, et al. Trends in Caesarean Section Rate According to Robson Group Classification among Pregnant Women with SARS-CoV-2 Infection: A Single-Center Large Cohort Study in Italy. Journal of Clinical Medicine. 2022; 11(21):6503. https://doi.org/10.3390/jcm11216503
Chicago/Turabian StyleSirico, Angelo, Luigi Carbone, Luisa Avino, Cira Buonfantino, Maria Chiara De Angelis, Marco Di Cresce, Annamaria Fabozzi, Francesco Paolo Improda, Antonietta Legnante, Carla Riccardi, and et al. 2022. "Trends in Caesarean Section Rate According to Robson Group Classification among Pregnant Women with SARS-CoV-2 Infection: A Single-Center Large Cohort Study in Italy" Journal of Clinical Medicine 11, no. 21: 6503. https://doi.org/10.3390/jcm11216503
APA StyleSirico, A., Carbone, L., Avino, L., Buonfantino, C., De Angelis, M. C., Cresce, M. D., Fabozzi, A., Improda, F. P., Legnante, A., Riccardi, C., Santoro, R., Vallone, R., Zizolfi, B., Buonomo, A. R., Gentile, I., Salomè, S., Raimondi, F., Bifulco, G., & Guida, M. (2022). Trends in Caesarean Section Rate According to Robson Group Classification among Pregnant Women with SARS-CoV-2 Infection: A Single-Center Large Cohort Study in Italy. Journal of Clinical Medicine, 11(21), 6503. https://doi.org/10.3390/jcm11216503







