Positive Effects of Saliva on Oral Candidiasis: Basic Research on the Analysis of Salivary Properties
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Detection of C. albicans
2.3. Measurement Items
2.3.1. Salivary Flow Rate
2.3.2. Intraoral Symptoms
2.3.3. Bite Force Test
2.4. Statistical Analysis
3. Results
3.1. Participants
3.2. Changes in C. albicans
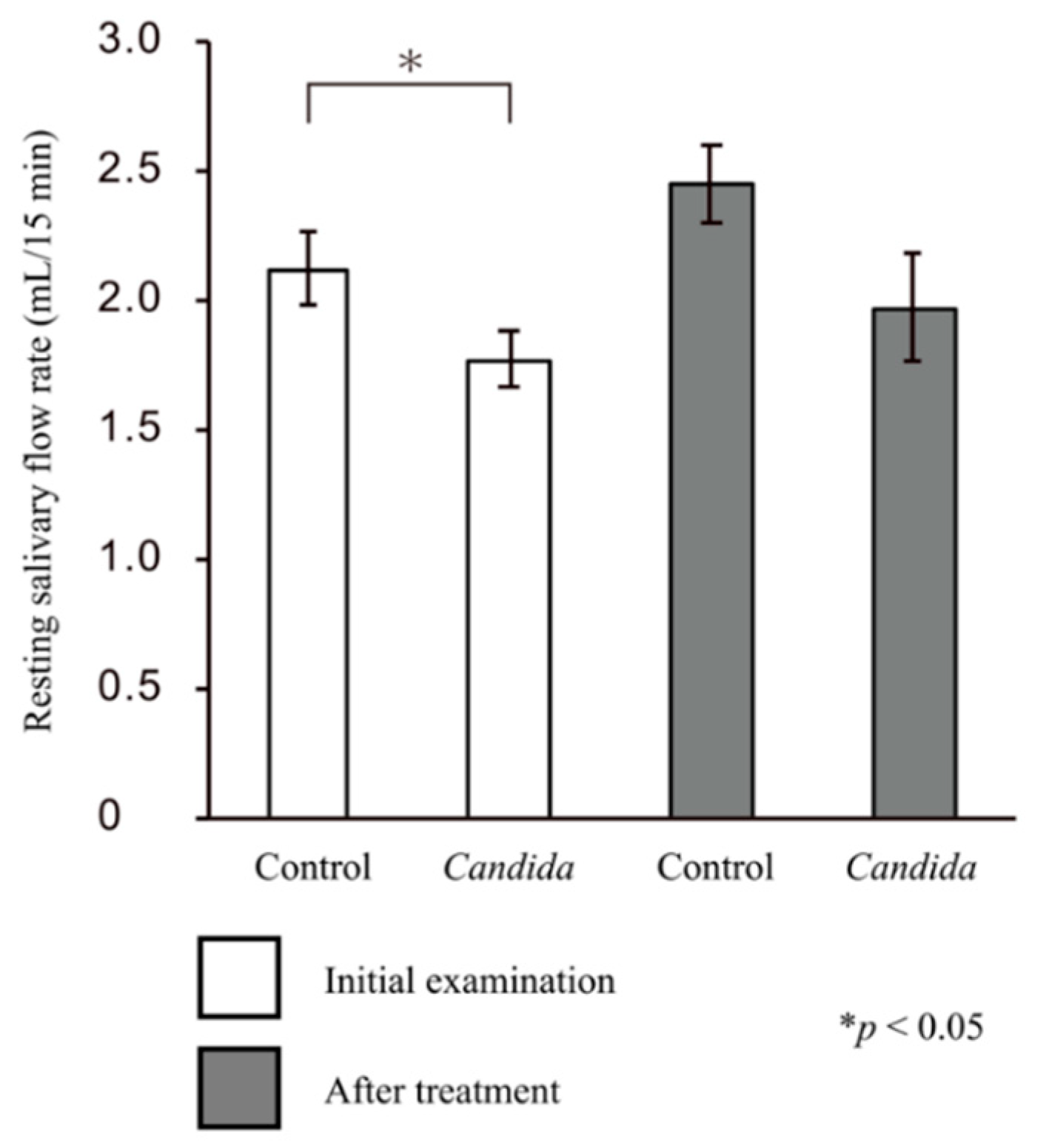
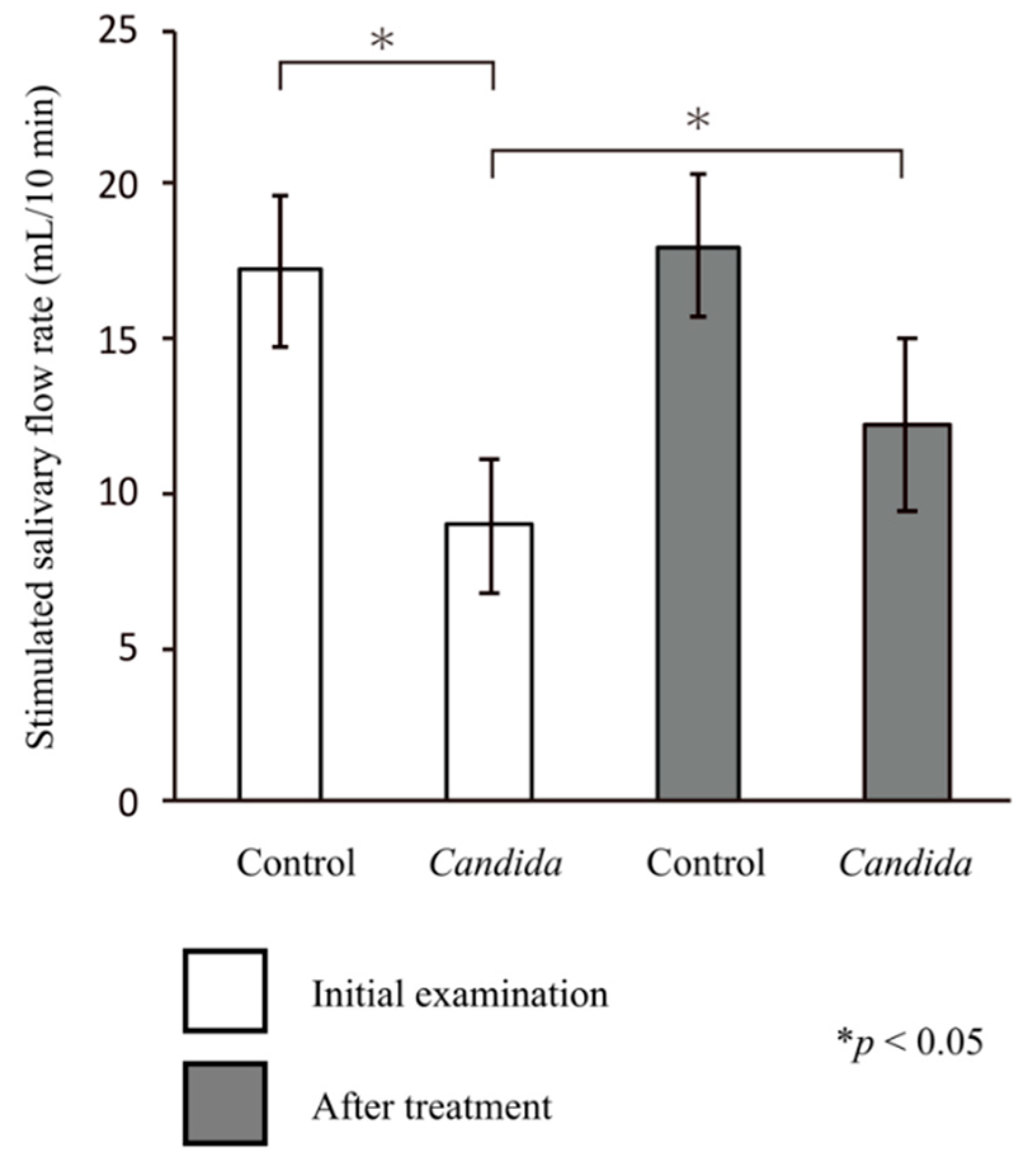
3.3. Salivary Flow Rate
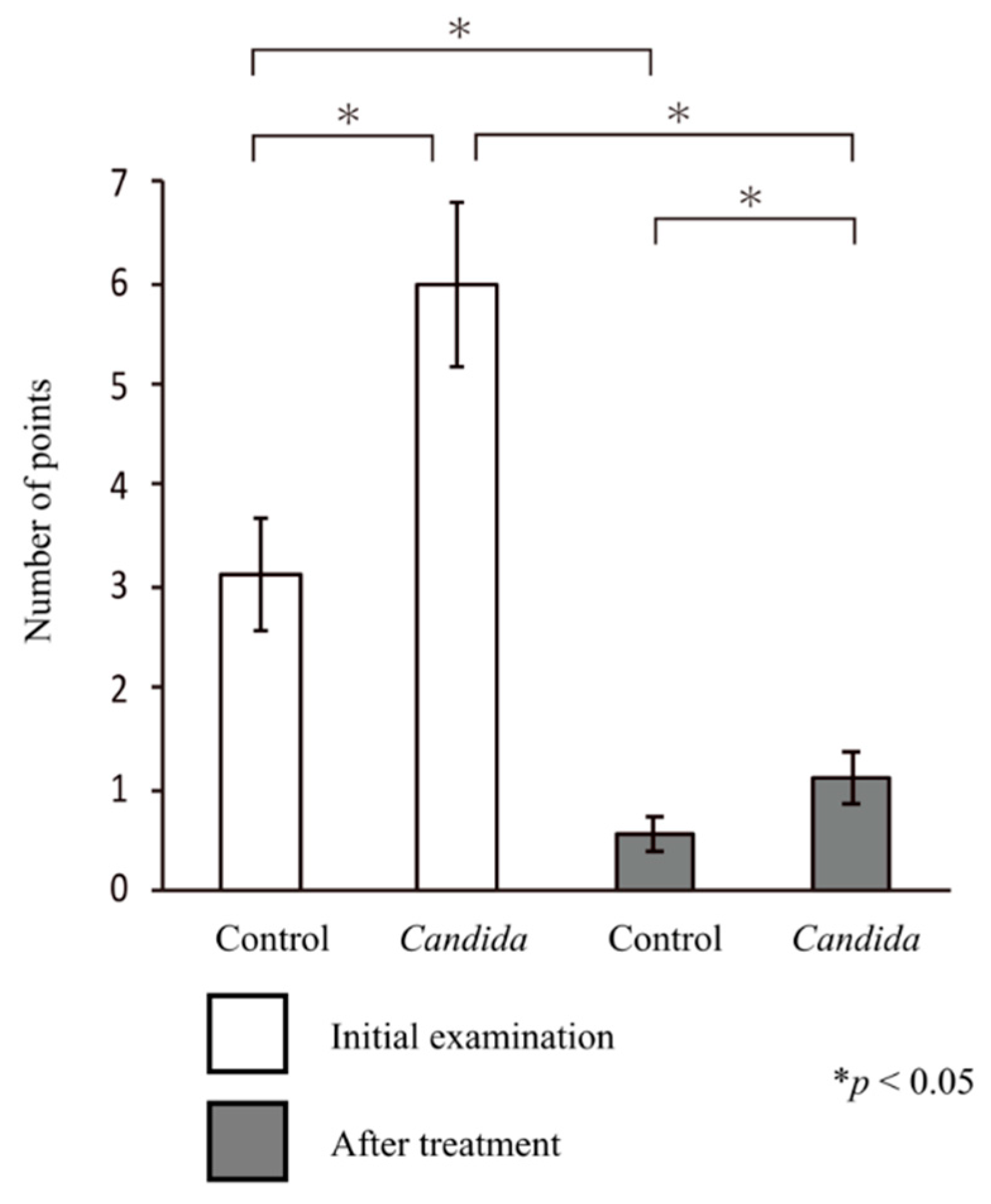
3.4. Intraoral Symptoms
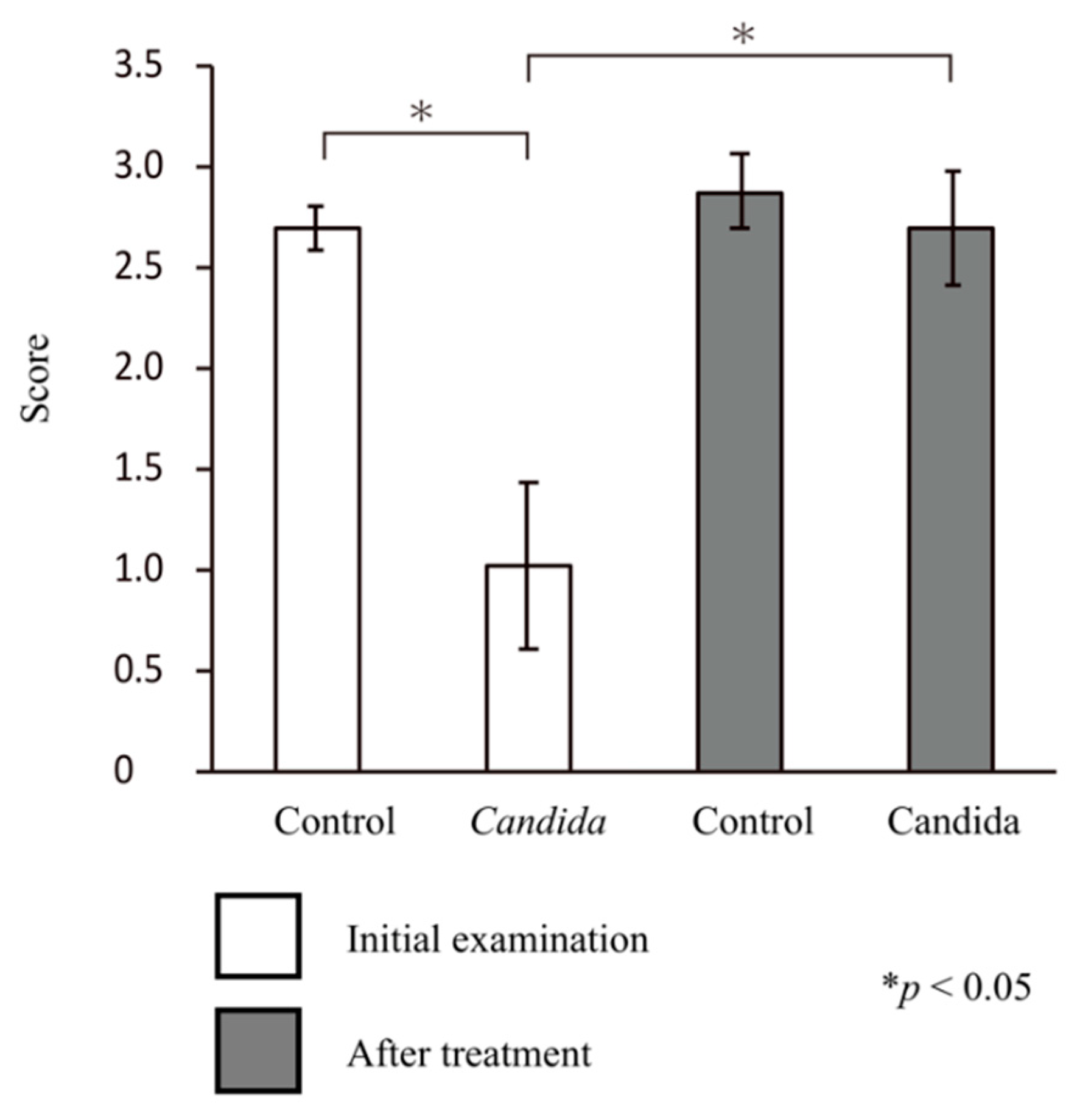
3.5. Bite Force
3.6. Multiple Regression Analysis of the Salivary Flow Rate, Intraoral Symptoms, and Bite Force
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liotti, F.M.; Posteraro, B.; Mannu, F.; Carta, F.; Pantaleo, A.; De Angelis, G.; Menchinelli, G.; Spanu, T.; Fiori, P.L.; Turrini, F.; et al. Development of a Multiplex PCR Platform for the Rapid Detection of Bacteria, Antibiotic Resistance, and Candida in Human Blood Samples. Front. Cell. Infect. Microbiol. 2019, 9, 389. [Google Scholar] [CrossRef] [PubMed]
- Hadadi-Fishani, M.; Shakerimoghaddam, A.; Khaledi, A. Candida coinfection among patients with pulmonary tuberculosis in Asia and Africa; A systematic review and meta-analysis of cross-sectional studies. Microb. Pathog. 2020, 139, 103898. [Google Scholar] [CrossRef]
- Aragón, F.; Zea-Sevilla, M.A.; Montero, J.; Sancho, P.; Corral, R.; Tejedor, C.; Frades-Payo, B.; Paredes-Gallardo, V.; Albaladejo, A. Oral health in Alzheimer’s disease: A multicenter case-control study. Clin. Oral Investig. 2018, 22, 3061–3070. [Google Scholar] [CrossRef] [PubMed]
- Naik, A.V.; Pai, R.C. A Study of Factors Contributing to Denture Stomatitis in a North Indian Community. Int. J. Dent. 2011, 2011, 1–4. [Google Scholar] [CrossRef]
- Roger-Leroi, V.; Mishellany-Dutour, A.; Woda, A.; Marchand, M.; Peyron, M.A. Substantiation of an artificial saliva formulated for use in a masticatory apparatus. Trop. Dent. J. 2012, 35, 5–14. [Google Scholar]
- Ishijima, T.; Koshino, H.; Hirai, T.; Takasaki, H. The relationship between salivary secretion rate and masticatory efficiency. J. Oral Rehabil. 2004, 31, 3–6. [Google Scholar] [CrossRef]
- Arinaga, Y.; Iwasaki, M.; Awano, S.; Ito, K.; Yoshida, A.; Kakuta, S.; Inho, S.; Ansai, T. The Association between Hyposalivation and Quality of Life in Dialysis Patients. J. Dent. Health 2017, 67, 64–69. [Google Scholar]
- Hirotomi, T.; Yoshihara, A.; Ogawa, H.; Ito, K.; Igarashi, A.; Miyazaki, H. A preliminary study on the relationship between stimulated saliva and periodontal conditions in community-dwelling elderly people. J. Dent. 2006, 34, 692–698. [Google Scholar] [CrossRef]
- Samnieng, P.; Ueno, M.; Shinada, K.; Zaitsu, T.; Wright, F.A.C.; Kawaguchi, Y. Association of hyposalivation with oral function, nutrition and oral health in community-dwelling elderly Thai. Community Dent. Health 2012, 29, 117–123. [Google Scholar]
- Nadig, S.D.; Ashwathappa, D.T.; Manjunath, M.; Krishna, S.; Annaji, A.G.; Shivaprakash, P.K. A relationship between salivary flow rates and Candida counts in patients with xerostomia. J. Oral Maxillofac. Pathol. 2017, 21, 316. [Google Scholar] [CrossRef] [PubMed]
- Navazesh, M.; Wood, G.J.; Brightman, V.J. Relationship between salivary flow rates and Candida albicans counts. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1995, 80, 284–288. [Google Scholar] [CrossRef]
- Kageyama, G.; Saegusa, J.; Irino, Y.; Tanaka, S.; Tsuda, K.; Takahashi, S.; Sendo, S.; Morinobu, A. Metabolomics analysis of saliva from patients with primary Sjögren’s syndrome. Clin. Exp. Immunol. 2015, 182, 149–153. [Google Scholar] [CrossRef]
- Spielmann, N.; Wong, D.T. Saliva: Diagnostics and therapeutic perspectives. Oral Dis. 2010, 17, 345–354. [Google Scholar] [CrossRef]
- Salvatori, O.; Puri, S.; Tati, S.; Edgerton, M. Innate Immunity and Saliva in Candida albicans–mediated Oral Diseases. J. Dent. Res. 2016, 95, 365–371. [Google Scholar] [CrossRef]
- Vila, T.; Rizk, A.M.; Sultan, A.S.; Jabra-Rizk, M.A. The power of saliva: Antimicrobial and beyond. PLoS Pathog. 2019, 15, e1008058. [Google Scholar] [CrossRef]
- Epstein, J.B.; Pearsall, N.N.; Truelove, E.L. Quantitative relationships between Candida albicans in saliva and the clinical status of human subjects. J. Clin. Microbiol. 1980, 12, 475–476. [Google Scholar] [CrossRef] [PubMed]
- Torres, S.R.; Peixoto, C.B.; Caldas, D.M.; Silva, E.B.; Akiti, T.; Nucci, M.; De Uzeda, M. Relationship between salivary flow rates and Candida counts in subjects with xerostomia. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2002, 93, 149–154. [Google Scholar] [CrossRef]
- Gendreau, L.; Loewy, Z.G. Epidemiology and Etiology of Denture Stomatitis. J. Prosthodont. 2011, 20, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Fouda, S.M.; Gad, M.M.; Ellakany, P.; Al-Thobity, A.M.; Al-Harbi, F.A.; Virtanen, J.I.; Raustia, A. The effect of nanodiamonds on candida albicans adhesion and surface characteristics of PMMA denture base material—An in vitro study. J. Appl. Oral Sci. 2019, 27, e20180779. [Google Scholar] [CrossRef] [PubMed]
- Morse, D.J.; Smith, A.; Wilson, M.J.; Marsh, L.; White, L.; Posso, R.; Bradshaw, D.J.; Wei, X.; Lewis, M.A.O.; Williams, D.W. Molecular community profiling of the bacterial microbiota associated with denture-related stomatitis. Sci. Rep. 2019, 9, 1–13. [Google Scholar] [CrossRef]
- Verhaeghe, T.V.; Wyatt, C.C.; Mostafa, N.Z. The effect of overnight storage conditions on complete denture colonization by Candida albicans and dimensional stability: A systematic review. J. Prosthet. Dent. 2020, 124, 176–182. [Google Scholar] [CrossRef]
- Shi, B.; Wu, T.; McLean, J.; Edlund, A.; Young, Y.; He, X.; Lv, H.; Zhou, X.; Shi, W.; Li, H.; et al. The Denture-Associated Oral Microbiome in Health and Stomatitis. mSphere 2016, 1, e00215-16. [Google Scholar] [CrossRef]
- Niedermeier, W.H.; Krämer, R. Salivary secretion and denture retention. J. Prosthet. Dent. 1992, 67, 211–216. [Google Scholar] [CrossRef]
- Márton, K.; Boros, I.; Fejérdy, P.; Madléna, M. Evaluation of unstimulated flow rates of whole and palatal saliva in healthy patients wearing complete dentures and in patients with Sjogren’s syndrome. J. Prosthet. Dent. 2004, 91, 577–581. [Google Scholar] [CrossRef] [PubMed]
- Yurdukoru, B.; Terzioglu, H.; Yilmaz, T. Assessment of whole saliva flow rate in denture wearing patients. J. Oral Rehabil. 2001, 28, 109–112. [Google Scholar] [CrossRef]
- Kawazoe, Y.; Hamada, T. The role of saliva in retention of maxillary complete dentures. J. Prosthet. Dent. 1978, 40, 131–136. [Google Scholar] [CrossRef]
- Mori, H.; Hoshi, N.; Taniguchi, M.; Banka, M.; Kimoto, K. Evaluation of xerostomia closely associated with systemic diseases using a dental approach. Open J. Stomatol. 2012, 2, 269–276. [Google Scholar] [CrossRef][Green Version]
- Banka, M.; Hoshi, N.; Saita, M.; Kuwabara, A.; Arai, Y.; Ohno, A.; Kumasaka, T.; Maruo, K.; Kimoto, S.; Kawai, Y.; et al. Denture Treatment Improves Oral Discomfort Accompanying Dry Sensation. Oral Health Dent. Manag. 2016, 65, 1–6. [Google Scholar] [CrossRef]
- Proctor, G.B. The physiology of salivary secretion. Periodontology 2000 2016, 70, 11–25. [Google Scholar] [CrossRef]
- Okuma, N.; Saita, M.; Hoshi, N.; Soga, T.; Tomita, M.; Sugimoto, M.; Kimoto, K. Effect of masticatory stimulation on the quantity and quality of saliva and the salivary metabolomic profile. PLoS ONE 2017, 12, e0183109. [Google Scholar] [CrossRef]
- Hoshi, N.; Arai, Y.; Kawanishi, N.; Kumasaka, T.; Tanaka, K.; Kimoto, K. The Effects of Prosthetic Treatment on Oral Candidiasis. Biol. Med. 2017, 9. [Google Scholar] [CrossRef]
- Dawes, C. Physiological Factors Affecting Salivary Flow Rate, Oral Sugar Clearance, and the Sensation of Dry Mouth in Man. J. Dent. Res. 1987, 66, 648–653. [Google Scholar] [CrossRef]
- Dawes, C.; Watanabe, S. The Effect of Taste Adaptation on Salivary Flow Rate and Salivary Sugar Clearance. J. Dent. Res. 1987, 66, 740–744. [Google Scholar] [CrossRef]
- Navazesh, M. Method for Collecting Saliva. Ann. N. Y. Acad. Sci. 1993, 694, 72–77. [Google Scholar] [CrossRef]
- Kawanishi, N.; Hoshi, N.; Masahiro, S.; Enomoto, A.; Ota, S.; Kaneko, M.; Soga, T.; Tomita, M.; Kimoto, K. Effects of inter-day and intra-day variation on salivary metabolomic profiles. Clin. Chim. Acta 2019, 489, 41–48. [Google Scholar] [CrossRef]
- Hama, Y.; Kanazawa, M.; Minakuchi, S.; Uchida, T.; Sasaki, Y. Properties of a color-changeable chewing gum used to evaluate masticatory performance. J. Prosthodont. Res. 2014, 58, 102–106. [Google Scholar] [CrossRef]
- Hama, Y.; Kanazawa, M.; Minakuchi, S.; Uchida, T.; Sasaki, Y. Reliability and validity of a quantitative color scale to evaluate masticatory performance using color-changeable chewing gum. J. Med. Dent. Sci. 2014, 61, 1–6. [Google Scholar]
- Komagamine, Y.; Kanazawa, M.; Minakuchi, S.; Uchida, T.; Sasaki, Y. Association between masticatory performance using a colour-changeable chewing gum and jaw movement. J. Oral Rehabil. 2011, 38, 555–563. [Google Scholar] [CrossRef]
- Horie, T.; Kanazawa, M.; Komagamine, Y.; Hama, Y.; Minakuchi, S. Association between near occlusal contact areas and mixing ability. J. Oral Rehabil. 2014, 41, 829–835. [Google Scholar] [CrossRef]
- Berdicevsky, I.; Ben-Aryeh, H.; Szargel, R.; Gutman, D. Oral Candida in asymptomatic denture wearers. Int. J. Oral Surg. 1980, 9, 113–115. [Google Scholar] [CrossRef]
- Gleiznys, A.; Zdanavičienė, E.; Žilinskas, J. Candida albicans Importance to Denture Wearers. A Literature Review. Stomatologija 2015, 17, 54–66. [Google Scholar]
- de Vasconcellos, A.A.; Gonçalves, L.M.; Cury, A.A.D.B.; da Silva, W.J. Candida-associated denture stomatitis: Clinical relevant aspects. In Oral Candidosis; Springer: Berlin/Heidelberg, Germany, 2015; pp. 53–57. [Google Scholar]
- Chandrasekaran, A.P.; Sonthalia, A.; Mhaske, S.P.; Lau, M.; Joshy, V.R.; Attokaran, G. Comparative evaluation of effect of complete denture wears on the flow rate of saliva in both medicated and apparently healthy patients. J. Int. Soc. Prev. Community Dent. 2016, 6, 219–223. [Google Scholar] [CrossRef]
- Torres, S.R.; Peixoto, C.B.; Caldas, D.M.; Silva, E.B.; Magalhães, F.A.C.; Uzeda, M.; Nucci, M. Clinical aspects of Candida species carriage in saliva of xerotomic subjects. Med. Mycol. 2003, 41, 411–415. [Google Scholar] [CrossRef][Green Version]
- Torres, S.R.; Peixoto, C.B.; Caldas, D.M.; Akiti, T.; Barreiros, M.G.C.; De Uzeda, M.; Nucci, M. A prospective randomized trial to reduce oral Candida spp. colonization in patients with hyposalivation. Braz. Oral Res. 2007, 21, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, A.; Singh, A.; Verma, R.; Murari, A. Oral candidiasis: An overview. J. Oral Maxillofac. Pathol. 2014, 18, 81–85. [Google Scholar] [CrossRef]
- Williamson, J.J. Diurnal variation of Candida albicans counts in saliva. Aust. Dent. J. 1972, 17, 54–60. [Google Scholar] [CrossRef]
- Khiyani, M.; Ahmadi, M.; Barbeau, J.; Feine, J.; De Souza, R.; Siqueira, W.; Emami, E. Salivary Biomarkers in Denture Stomatitis: A Systematic Review. JDR Clin. Transl. Res. 2019, 4, 312–322. [Google Scholar] [CrossRef]
- Bertram, H.C.; Eggers, N.; Eller, N. Potential of Human Saliva for Nuclear Magnetic Resonance-Based Metabolomics and for Health-Related Biomarker Identification. Anal. Chem. 2009, 81, 9188–9193. [Google Scholar] [CrossRef]
- Bigler, L.R.; Streckfus, C.F.; Dubinsky, W.P. Salivary Biomarkers for the Detection of Malignant Tumors That are Remote from the Oral Cavity. Clin. Lab. Med. 2009, 29, 71–85. [Google Scholar] [CrossRef]
- Miller, C.S.; Foley, J.D.; Bailey, A.L.; Campell, C.L.; Humphries, R.L.; Christodoulides, N.; Floriano, P.N.; Simmons, G.; Bhagwandin, B.; Jacobson, J.W.; et al. Current developments in salivary diagnostics. Biomark. Med. 2010, 4, 171–189. [Google Scholar] [CrossRef]
- Zhang, A.; Sun, H.; Wang, X. Saliva Metabolomics Opens Door to Biomarker Discovery, Disease Diagnosis, and Treatment. Appl. Biochem. Biotechnol. 2012, 168, 1718–1727. [Google Scholar] [CrossRef]
- Sugimoto, M.; Ota, S.; Kaneko, M.; Enomoto, A.; Soga, T. Quantification of Salivary Charged Metabolites using Capillary Electrophoresis Time-of-flight-mass Spectrometry. Bio-Protocol 2020, 10, e3797. [Google Scholar] [CrossRef]
- Sugimoto, M. Salivary metabolomics for cancer detection. Expert Rev. Proteom. 2020, 17, 1–10. [Google Scholar] [CrossRef]
| Control Group (n = 25) | Candida Group (n = 37) | |
|---|---|---|
| Age (years) | 71.1 ± 2.4 | 74.5 ± 2.8 * |
| Sex | ||
| Male | 10 (40) | 13 (35) |
| Female | 15 (60) | 24 (65) |
| Prosthetic | ||
| Partial denture | 22 | 33 |
| Full denture | 13 | 29 |
| Prosthetic treatment (%) | 100 | 100 |
| Dependent Variable | Independent Variable | Non-Standardization Factor | p-Value |
|---|---|---|---|
| Candida | Sex (male/female) | 1.511 | 0.029 * |
| Type of denture (PD/FD) | −0.428 | 0.012 * | |
| Existing denture treatment (new/old) | −2.481 | 0.01 * | |
| Masticatory ability | 1.922 | 0.025 * | |
| Unstimulated salivary | 0.399 | 0.701 | |
| Stimulated salivary | −0.459 | 0.011 * | |
| Oral symptoms | Sex (male/female) | 0.819 | 0.059 |
| Type of denture (PD/FD) | −0.924 | 0.072 * | |
| Existing denture treatment (new/old) | 1.192 | 0.104 | |
| Masticatory ability | 0.725 | 0.042 * | |
| Unstimulated salivary | 1.291 | 0.079 | |
| Stimulated salivary | −0.255 | 0.037 * | |
| Masticatory ability | Sex (male/female) | 1.102 | 0.318 |
| Type of denture (PD/FD) | 0.982 | 0.092 | |
| Existing denture treatment (new/old) | 1.587 | 0.048 * | |
| Unstimulated salivary | 0.911 | 0.441 | |
| Stimulated salivary | 1.745 | 0.031 * | |
| Unstimulated salivary flow rate | Sex (male/female) | 0.009 | 0.329 |
| Type of denture (PD/FD) | 0.155 | 0.11 | |
| Existing denture treatment (new/old) | 0.75 | 0.041 * | |
| Stimulated salivary flow rate | Sex (male/female) | −0.075 | 0.212 |
| Type of denture (PD/FD) | 1.102 | 0.059 | |
| Existing denture treatment (new/old) | 1.029 | 0.008 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kawanishi, N.; Hoshi, N.; Adachi, T.; Ichigaya, N.; Kimoto, K. Positive Effects of Saliva on Oral Candidiasis: Basic Research on the Analysis of Salivary Properties. J. Clin. Med. 2021, 10, 812. https://doi.org/10.3390/jcm10040812
Kawanishi N, Hoshi N, Adachi T, Ichigaya N, Kimoto K. Positive Effects of Saliva on Oral Candidiasis: Basic Research on the Analysis of Salivary Properties. Journal of Clinical Medicine. 2021; 10(4):812. https://doi.org/10.3390/jcm10040812
Chicago/Turabian StyleKawanishi, Norishige, Noriyuki Hoshi, Takuya Adachi, Narumi Ichigaya, and Katsuhiko Kimoto. 2021. "Positive Effects of Saliva on Oral Candidiasis: Basic Research on the Analysis of Salivary Properties" Journal of Clinical Medicine 10, no. 4: 812. https://doi.org/10.3390/jcm10040812
APA StyleKawanishi, N., Hoshi, N., Adachi, T., Ichigaya, N., & Kimoto, K. (2021). Positive Effects of Saliva on Oral Candidiasis: Basic Research on the Analysis of Salivary Properties. Journal of Clinical Medicine, 10(4), 812. https://doi.org/10.3390/jcm10040812





