Predictive Value of Baseline [18F]FDG PET/CT for Response to Systemic Therapy in Patients with Advanced Melanoma
Abstract
:1. Introduction
2. Materials and Methods
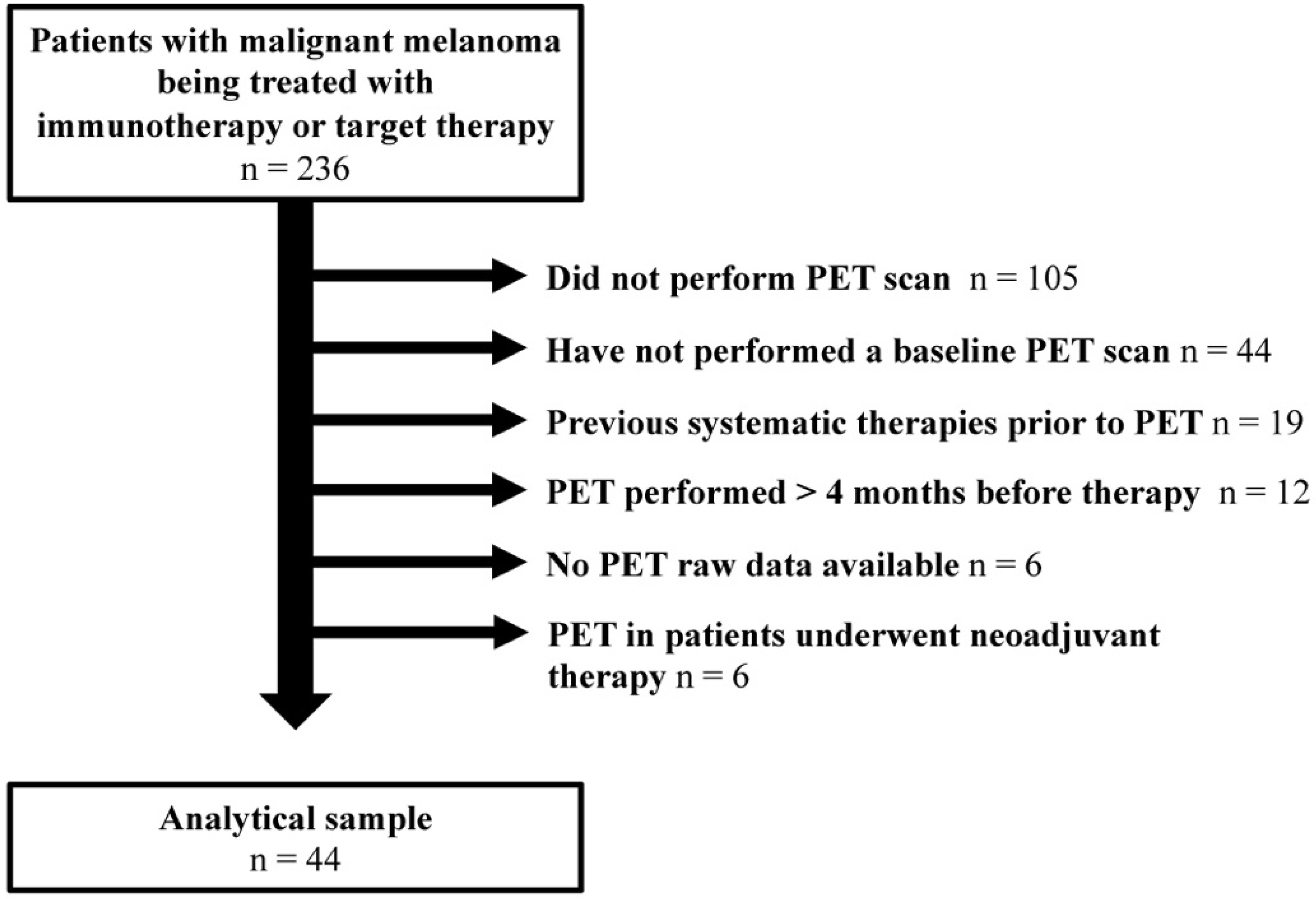
2.1. Patient Selection
2.2. Clinical Evaluation and Melanoma Classification
2.3. PET/CT Acquisition
2.4. Quantitative Imaging Analysis
2.5. Assessment of Therapy Response—Endpoints
2.6. Statistical Analysis
3. Results
3.1. Patient and Primary Tumor Characteristics
3.2. Semi-Quantitative PET Images Results—Metabolic Tumor Burden
3.3. Early and Late Response Assessment
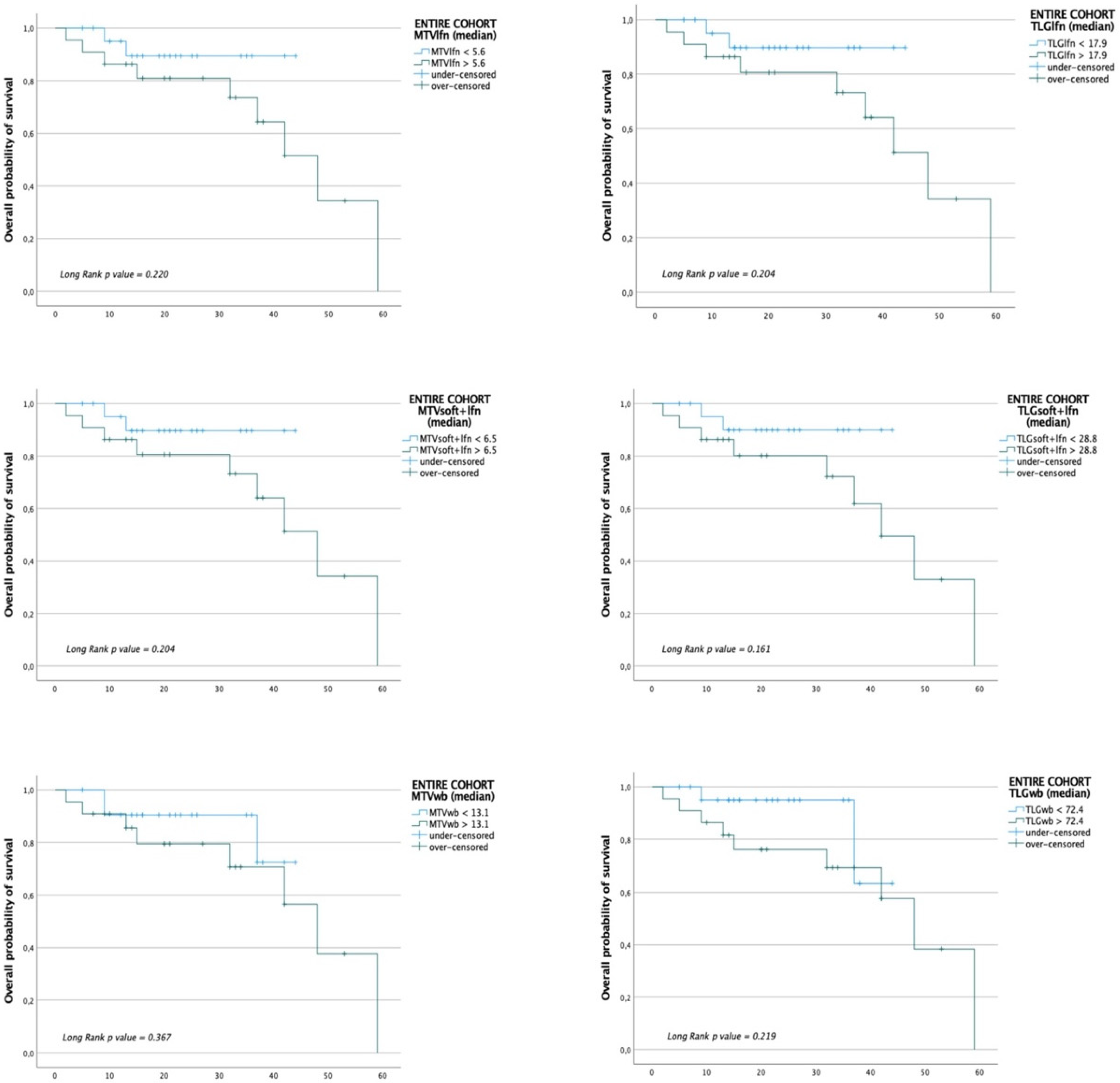
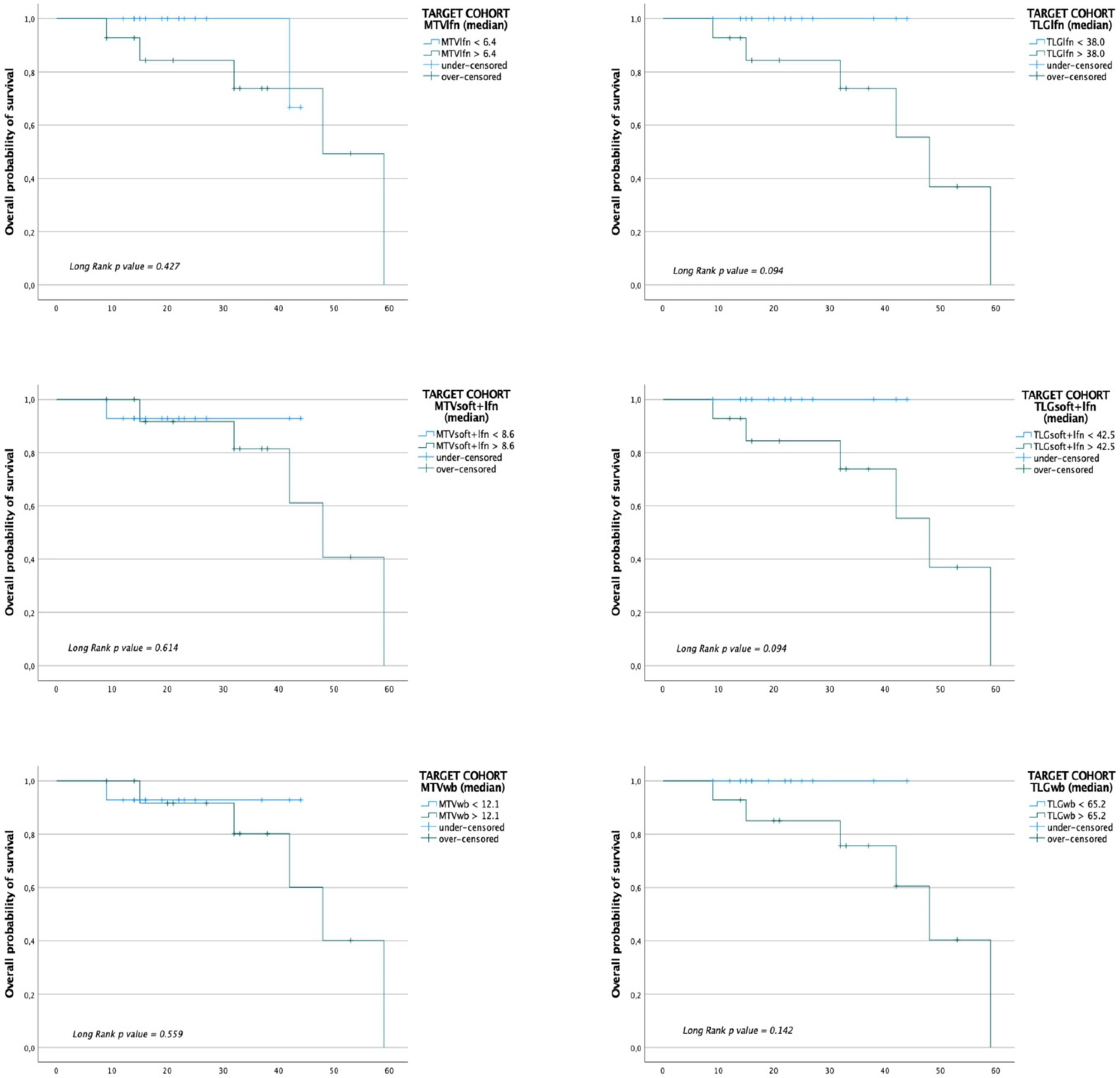
3.4. Patients’ Outcome Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Tripp, M.K.; Watson, M.; Balk, S.J.; Swetter, S.M.; Gershenwald, J.E. State of the science on prevention and screening to reduce melanoma incidence and mortality: The time is now. CA Cancer J. Clin. 2016, 66, 460–480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schadendorf, D.; Fisher, D.E.; Garbe, C.; Gershenwald, J.E.; Grob, J.J.; Halpern, A.; Herlyn, M.; Marchetti, M.A.; McArthur, G.; Ribas, A.; et al. Melanoma. Nat. Rev. Dis. Prim. 2015, 1, 15003. [Google Scholar] [CrossRef]
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Mathers, C.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int. J. Cancer 2019, 144, 1941–1953. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lombardo, N.; Della Corte, M.; Pelaia, C.; Piazzetta, G.; Lobello, N.; Del Duca, E.; Bennardo, L.; Nisticò, S.P. Primary mucosal melanoma presenting with a unilateral nasal obstruction of the left inferior turbinate. Medicina 2021, 57, 359. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bomar, L.; Senithilnathan, A.; Ahn, C. Systemic therapies for advanced melanoma. Dermatol. Clin. 2019, 37, 409–423. [Google Scholar] [CrossRef]
- Wong, D.J.L.; Ribas, A. Targeted therapy for melanoma. Cancer Treat. Res. 2016, 167, 251–262. [Google Scholar] [CrossRef] [Green Version]
- Long, G.V.; Stroyakovskiy, D.; Gogas, H.; Levchenko, E.; De Braud, F.; Larkin, J.; Garbe, C.; Jouary, T.; Hauschild, A.; Grob, J.J.; et al. Dabrafenib and trametinib versus dabrafenib and placebo for Val600 BRAF-mutant melanoma: A multicentre, double-blind, phase 3 randomised controlled trial. Lancet 2015, 386, 444–451. [Google Scholar] [CrossRef]
- Wong, A.N.M.; McArthur, G.A.; Hofman, M.S.; Hicks, R.J. The Advantages and challenges of using FDG PET/CT for response assessment in melanoma in the era of targeted agents and immunotherapy. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 67–77. [Google Scholar] [CrossRef]
- Wolchok, J.D.; Kluger, H.; Callahan, M.K.; Postow, M.A.; Rizvi, N.A.; Lesokhin, A.M.; Segal, N.H.; Ariyan, C.E.; Gordon, R.-A.; Reed, K.; et al. Nivolumab plus Ipilimumab in Advanced Melanoma. N. Engl. J. Med. 2013, 369, 122–133. [Google Scholar] [CrossRef] [Green Version]
- Liberini, V.; Laudicella, R.; Capozza, M.; Huellner, M.W.; Burger, I.A.; Baldari, S.; Terreno, E.; Deandreis, D. The future of cancer diagnosis, treatment and surveillance: A systemic review on immunotherapy and immuno-pet radiotracers. Molecules 2021, 26, 2201. [Google Scholar] [CrossRef]
- Luke, J.J.; Flaherty, K.T.; Ribas, A.; Long, G.V. Targeted agents and immunotherapies: Optimizing outcomes in melanoma. Nat. Rev. Clin. Oncol. 2017, 14, 463–482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamid, O.; Robert, C.; Daud, A.; Hodi, F.S.; Hwu, W.-J.; Kefford, R.; Wolchok, J.D.; Hersey, P.; Joseph, R.W.; Weber, J.S.; et al. Safety and tumor responses with lambrolizumab (Anti–PD-1) in melanoma. N. Engl. J. Med. 2013, 369, 134–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Topalian, S.L.; Hodi, F.S.; Brahmer, J.R.; Gettinger, S.N.; Smith, D.C.; McDermott, D.F.; Powderly, J.D.; Carvajal, R.D.; Sosman, J.A.; Atkins, M.B.; et al. Safety, activity, and immune correlates of Anti–PD-1 antibody in cancer. N. Engl. J. Med. 2012, 366, 2443–2454. [Google Scholar] [CrossRef]
- Tonella, L.; Pala, V.; Ponti, R.; Rubatto, M.; Gallo, G.; Mastorino, L.; Avallone, G.; Merli, M.; Agostini, A.; Fava, P.; et al. Prognostic and predictive biomarkers in stage iii melanoma: Current insights and clinical implications. Int. J. Mol. Sci. 2021, 22, 4561. [Google Scholar] [CrossRef] [PubMed]
- Ugurel, S.; Schadendorf, D.; Horny, K.; Sucker, A.; Schramm, S.; Utikal, J.; Pföhler, C.; Herbst, R.; Schilling, B.; Blank, C.; et al. Elevated baseline serum PD-1 or PD-L1 predicts poor outcome of PD-1 inhibition therapy in metastatic melanoma. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2020, 31, 144–152. [Google Scholar] [CrossRef] [Green Version]
- Diazzi, S.; Tartare-Deckert, S.; Deckert, M. Bad neighborhood: Fibrotic stroma as a new player in melanoma resistance to targeted therapies. Cancers 2020, 12, 1364. [Google Scholar] [CrossRef]
- Falcone, I.; Conciatori, F.; Bazzichetto, C.; Ferretti, G.; Cognetti, F.; Ciuffreda, L.; Milella, M. Tumor microenvironment: Implications in melanoma resistance to targeted therapy and immunotherapy. Cancers 2020, 12, 2870. [Google Scholar] [CrossRef] [PubMed]
- Saadani, H.; Van der Hiel, B.; Aalbersberg, E.A.; Zavrakidis, I.; Haanen, J.B.A.G.; Hoekstra, O.S.; Boellaard, R.; Stokkel, M.P.M. Metabolic biomarker–based BRAFV600 mutation association and prediction in melanoma. J. Nucl. Med. 2019, 60, 1545–1552. [Google Scholar] [CrossRef] [PubMed]
- Burns, D.; George, J.; Aucoin, D.; Bower, J.; Burrell, S.; Gilbert, R.; Bower, N. The pathogenesis and clinical management of cutaneous melanoma: An evidence-based review. J. Med. Imaging Radiat. Sci. 2019, 50, 460–469.e1. [Google Scholar] [CrossRef] [Green Version]
- Franken, M.G.; Leeneman, B.; Gheorghe, M.; Uyl-de Groot, C.A.; Haanen, J.B.A.G.; van Baal, P.H.M. A systematic literature review and network meta-analysis of effectiveness and safety outcomes in advanced melanoma. Eur. J. Cancer 2019, 123, 58–71. [Google Scholar] [CrossRef] [PubMed]
- Wright, C.L.; Miller, E.D.; Contreras, C.; Knopp, M.V. Precision nuclear medicine: The evolving role of PET in melanoma. Radiol. Clin. N. Am. 2021, 59, 755–772. [Google Scholar] [CrossRef] [PubMed]
- Hindié, E. Metastatic melanoma: Can FDG-PET predict success of anti-PD-1 therapy and help determine when it can be discontinued? Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 2227–2232. [Google Scholar] [CrossRef] [Green Version]
- Salaün, P.Y.; Abgral, R.; Malard, O.; Querellou-Lefranc, S.; Quere, G.; Wartski, M.; Coriat, R.; Hindie, E.; Taieb, D.; Tabarin, A.; et al. Good clinical practice recommendations for the use of PET/CT in oncology. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 28–50. [Google Scholar] [CrossRef]
- Basler, L.; Gabryś, H.S.; Hogan, S.A.; Pavic, M.; Bogowicz, M.; Vuong, D.; Tanadini-Lang, S.; Förster, R.; Kudura, K.; Huellner, M.W.; et al. Radiomics, tumor volume, and blood biomarkers for early prediction of pseudoprogression in patients with metastatic melanoma treated with immune checkpoint inhibition. Clin. Cancer Res. 2020, 26, 4414–4425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fridman, W.H.; Zitvogel, L.; Sautès-Fridman, C.; Kroemer, G. The immune contexture in cancer prognosis and treatment. Nat. Rev. Clin. Oncol. 2017, 14, 717–734. [Google Scholar] [CrossRef]
- Sarikaya, I.; Sarikaya, A. Assessing PET Parameters in Oncologic 18F-FDG Studies. J. Nucl. Med. Technol. 2020, 48, 278–282. [Google Scholar] [CrossRef]
- Gershenwald, J.E.; Scolyer, R.A. Melanoma staging: American Joint Committee on Cancer (AJCC) 8th edition and beyond. Ann. Surg. Oncol. 2018, 25, 2105–2110. [Google Scholar] [CrossRef]
- Boellaard, R.; Delgado-Bolton, R.; Oyen, W.J.G.; Giammarile, F.; Tatsch, K.; Eschner, W.; Verzijlbergen, F.J.; Barrington, S.F.; Pike, L.C.; Weber, W.A.; et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: Version 2.0. Eur. J. Nucl. Med. Mol. Imaging 2015, 42, 328–354. [Google Scholar] [CrossRef]
- Nioche, C.; Orlhac, F.; Boughdad, S.; Reuze, S.; Goya-Outi, J.; Robert, C.; Pellot-Barakat, C.; Soussan, M.; Frouin, F.; Buvat, I. Lifex: A freeware for radiomic feature calculation in multimodality imaging to accelerate advances in the characterization of tumor heterogeneity. Cancer Res. 2018, 78, 4786–4789. [Google Scholar] [CrossRef] [Green Version]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef] [PubMed]
- IBM Corp. Released 2017. IBM SPSS Statistics for Windows; Version 25.0; IBM Corp.: Armonk, NY, USA, 2017. [Google Scholar]
- Seban, R.D.; Nemer, J.S.; Marabelle, A.; Yeh, R.; Deutsch, E.; Ammari, S.; Moya-Plana, A.; Mokrane, F.Z.; Gartrell, R.D.; Finkel, G.; et al. Prognostic and theranostic 18F-FDG PET biomarkers for anti-PD1 immunotherapy in metastatic melanoma: Association with outcome and transcriptomics. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 2298–2310. [Google Scholar] [CrossRef] [PubMed]
- Ito, K.; Teng, R.; Schöder, H.; Humm, J.L.; Ni, A.; Michaud, L.; Nakajima, R.; Yamashita, R.; Wolchok, J.D.; Weber, W.A. 18 F-FDG PET/CT for monitoring of ipilimumab therapy in patients with metastatic melanoma. J. Nucl. Med. 2019, 60, 335–341. [Google Scholar] [CrossRef] [Green Version]
- Mannavola, F.; Mandala, M.; Todisco, A.; Sileni, V.C.; Palla, M.; Minisini, A.M.; Pala, L.; Morgese, F.; Di Guardo, L.; Stucci, L.S.; et al. An Italian retrospective survey on bone metastasis in melanoma: Impact of immunotherapy and radiotherapy on survival. Front. Oncol. 2020, 10, 1652. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Rahman, O. Clinical correlates and prognostic value of different metastatic sites in patients with malignant melanoma of the skin: A SEER database analysis. J. Dermatolog. Treat. 2018, 29, 176–181. [Google Scholar] [CrossRef]
- Bisschop, C.; de Heer, E.C.; Brouwers, A.H.; Hospers, G.A.P.; Jalving, M. Rational use of 18F-FDG PET/CT in patients with advanced cutaneous melanoma: A systematic review. Crit. Rev. Oncol. Hematol. 2020, 153, 103044. [Google Scholar] [CrossRef]
- Ito, K.; Schöder, H.; Teng, R.; Humm, J.L.; Ni, A.; Wolchok, J.D.; Weber, W.A. Prognostic value of baseline metabolic tumor volume measured on 18 F-fluorodeoxyglucose positron emission tomography/computed tomography in melanoma patients treated with ipilimumab therapy. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 930–939. [Google Scholar] [CrossRef] [PubMed]
- Beasley, G.; Tyler, D. In-transit melanoma metastases: Incidence, prognosis, and the role of lymphadenectomy. Ann. Surg. Oncol. 2014, 22, 358–360. [Google Scholar] [CrossRef] [Green Version]
- Gershenwald, J.E.; Scolyer, R.A.; Hess, K.R.; Sondak, V.K.; Long, G.V.; Ross, M.I.; Lazar, A.J.; Faries, M.B.; Kirkwood, J.M.; McArthur, G.A.; et al. Melanoma staging: Evidence-based changes in the American joint committee on cancer eighth edition cancer staging manual. CA Cancer J. Clin. 2017, 67, 472–492. [Google Scholar] [CrossRef] [Green Version]
- Liberini, V.; Messerli, M.; Husmann, L.; Kudura, K.; Grünig, H.; Maurer, A.; Skawran, S.; Orita, E.; Pizzuto, D.A.; Deandreis, D.; et al. Improved detection of in-transit metastases of malignant melanoma with BSREM reconstruction in digital [18F]FDG PET/CT. Eur. Radiol. 2021, 31, 8011–8020. [Google Scholar] [CrossRef]
- Pararajasingam, A.; Goodwin, R. In-transit metastases: The migration of melanoma. Br. J. Hosp. Med. 2020, 81, 1. [Google Scholar] [CrossRef]
- Clemente-Ruiz de Almiron, A.; Serrano-Ortega, S. Factores de riesgo de metástasis en tránsito en pacientes con melanoma cutáneo. Actas Dermosifiliogr. 2012, 103, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Marcoval, J.; Ferreres, J.R.; Penín, R.M.; Piulats, J.M.; Caminal, J.M.; Fabra, À. Análisis descriptivo de los patrones de recidiva cutánea en los pacientes con melanoma. Actas Dermosifiliogr. 2011, 102, 791–796. [Google Scholar] [CrossRef]
- Rao, U.N.M.; Ibrahim, J.; Flaherty, L.E.; Richards, J.; Kirkwood, J.M. Implications of microscopic satellites of the primary and extracapsular lymph node spread in patients with high-risk melanoma: Pathologic corollary of eastern cooperative oncology group trial E1690. J. Clin. Oncol. 2002, 20, 2053–2057. [Google Scholar] [CrossRef] [PubMed]
- León, P.; Daly, J.M.; Synnestvedt, M.; Schultz, D.J.; Elder, D.E.; Clark, W.H. The prognostic implications of microscopic satellites in patients with clinical stage I melanoma. Arch. Surg. 1991, 126, 1461–1468. [Google Scholar] [CrossRef] [PubMed]
- Read, R.L.; Haydu, L.; Saw, R.P.M.; Quinn, M.J.; Shannon, K.; Spillane, A.J.; Stretch, J.R.; Scolyer, R.A.; Thompson, J.F. In-transit melanoma metastases: Incidence, prognosis, and the role of lymphadenectomy. Ann. Surg. Oncol. 2015, 22, 475–481. [Google Scholar] [CrossRef]
- Weide, B.; Faller, C.; Büttner, P.; Pflugfelder, A.; Leiter, U.; Eigentler, T.K.; Bauer, J.; Forschner, A.; Meier, F.; Garbe, C. Prognostic factors of melanoma patients with satellite or in-transit metastasis at the time of stage III diagnosis. PLoS ONE 2013, 8, e63137. [Google Scholar] [CrossRef] [PubMed]

| Patient Characteristics | |
|---|---|
| Gender, n (%) | |
| Male | 28.0 (63.6) |
| Female | 16.0 (36.4) |
| Age (years), median (IQR) | 62.0 (49.7–75.0) |
| Primary melanoma characteristics | |
| Type, n (%) | |
| Superficial spreading melanoma (SSM) | 12 (27.3) |
| Lentigo malignant melanoma (LMM) | 2 (4.5) |
| Acral lentiginous melanoma (ALM) | 0 (0.0) |
| Nodular melanoma (NM) | 16 (36.4) |
| Unknown | 8 (18.2) |
| Location, n (%) | |
| Head and neck | 9 (20.4) |
| Torso | 19 (43.3) |
| Limbs | 10 (22.7) |
| Unknown | 6 (13.6) |
| PET stage, n (%) | |
| III | 11 (25.0) |
| IV | 33 (75.0) |
| Breslow (mm), median (IQR) | 4.5 (2.0–5.0) |
| Ulceration, n (%) | |
| Yes | 8 (18.2) |
| No | 11 (25.0) |
| Unknown | 25 (56.8) |
| BRAF mutation, n (%) | |
| Yes | 29 (65.9) |
| No | 15 (34.1) |
| Parameters at 12 Months | Optimal Cut-Off | Sensitivity | Specificity | AUC | p-Value |
|---|---|---|---|---|---|
| Entire cohort | |||||
| Bone MTV (mL) | 6.1 | 36% | 97% | 0.713 | 0.037 |
| Bone TLG | 18.8 | 45% | 97% | 0.716 | 0.034 |
| Bone SUVmax | 4.1 | 36% | 97% | 0.716 | 0.034 |
| Target therapy cohort | |||||
| Bone MTV (mL) | 13.1 | 42% | 100% | 0.786 | 0.027 |
| Bone TLG | 18.8 | 57% | 100% | 0.786 | 0.027 |
| Bone SUVmax | 5.7 | 42% | 100% | 0.786 | 0.027 |
| Target therapy cohort | |||||
| Whole-body MTV (mL) | 24.6 | 71% | 85% | 0.814 | 0.015 |
| Whole-body TLG | 208.4 | 71% | 85% | 0.793 | 0.023 |
| Parameters for OS | Optimal Cut-Off | Sensitivity | Specificity | AUC | p-Value |
|---|---|---|---|---|---|
| Entire cohort | |||||
| Lymph nodes MTV (mL) | 10.6 | 63% | 76% | 0.755 | 0.012 |
| Lymph nodes TLG | 55.1 | 63% | 76% | 0.777 | 0.006 |
| Lymph nodes SUVmax | 9.7 | 72% | 64% | 0.713 | 0.036 |
| Entire cohort | |||||
| Soft tissue + LFN MTV (mL) | 10.6 | 72% | 67% | 0.713 | 0.036 |
| Soft tissue + LFN TLG | 66.1 | 63% | 70% | 0.738 | 0.019 |
| Soft tissue + LFN SUVmax | 9.2 | 81% | 61% | 0.702 | 0.046 |
| Entire cohort | |||||
| Whole-body MTV (mL) | 14.8 | 72% | 61% | 0.705 | 0.043 |
| Whole-body TLG | 86.4 | 72% | 64% | 0.76 | 0.01 |
| Whole-body SUVmax | 11.6 | 72% | 61% | 0.72 | 0.03 |
| Target therapy cohort | |||||
| Lymph nodes MTV (mL) | 10.9 | 66% | 73% | 0.811 | 0.022 |
| Lymph nodes TLG | 137.4 | 66% | 82% | 0.864 | 0.007 |
| Target therapy cohort | |||||
| Soft tissue + LFN MTV (mL) | 14.6 | 66% | 82% | 0.841 | 0.012 |
| Soft tissue + LFN TLG | 132.1 | 66% | 78% | 0.871 | 0.006 |
| Target therapy cohort | |||||
| Whole-body MTV (mL) | 17.6 | 66% | 69% | 0.773 | 0.044 |
| Whole-body TLG | 158.1 | 66% | 78% | 0.848 | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liberini, V.; Rubatto, M.; Mimmo, R.; Passera, R.; Ceci, F.; Fava, P.; Tonella, L.; Polverari, G.; Lesca, A.; Bellò, M.; et al. Predictive Value of Baseline [18F]FDG PET/CT for Response to Systemic Therapy in Patients with Advanced Melanoma. J. Clin. Med. 2021, 10, 4994. https://doi.org/10.3390/jcm10214994
Liberini V, Rubatto M, Mimmo R, Passera R, Ceci F, Fava P, Tonella L, Polverari G, Lesca A, Bellò M, et al. Predictive Value of Baseline [18F]FDG PET/CT for Response to Systemic Therapy in Patients with Advanced Melanoma. Journal of Clinical Medicine. 2021; 10(21):4994. https://doi.org/10.3390/jcm10214994
Chicago/Turabian StyleLiberini, Virginia, Marco Rubatto, Riccardo Mimmo, Roberto Passera, Francesco Ceci, Paolo Fava, Luca Tonella, Giulia Polverari, Adriana Lesca, Marilena Bellò, and et al. 2021. "Predictive Value of Baseline [18F]FDG PET/CT for Response to Systemic Therapy in Patients with Advanced Melanoma" Journal of Clinical Medicine 10, no. 21: 4994. https://doi.org/10.3390/jcm10214994
APA StyleLiberini, V., Rubatto, M., Mimmo, R., Passera, R., Ceci, F., Fava, P., Tonella, L., Polverari, G., Lesca, A., Bellò, M., Arena, V., Ribero, S., Quaglino, P., & Deandreis, D. (2021). Predictive Value of Baseline [18F]FDG PET/CT for Response to Systemic Therapy in Patients with Advanced Melanoma. Journal of Clinical Medicine, 10(21), 4994. https://doi.org/10.3390/jcm10214994












