Ratio between Right Ventricular Longitudinal Strain and Pulmonary Arterial Systolic Pressure: Novel Prognostic Parameter in Patients Undergoing Cardiac Resynchronization Therapy
Abstract
1. Introduction
2. Methods
2.1. Study Patients
2.1.1. Left Ventricle Echocardiographic Evaluation
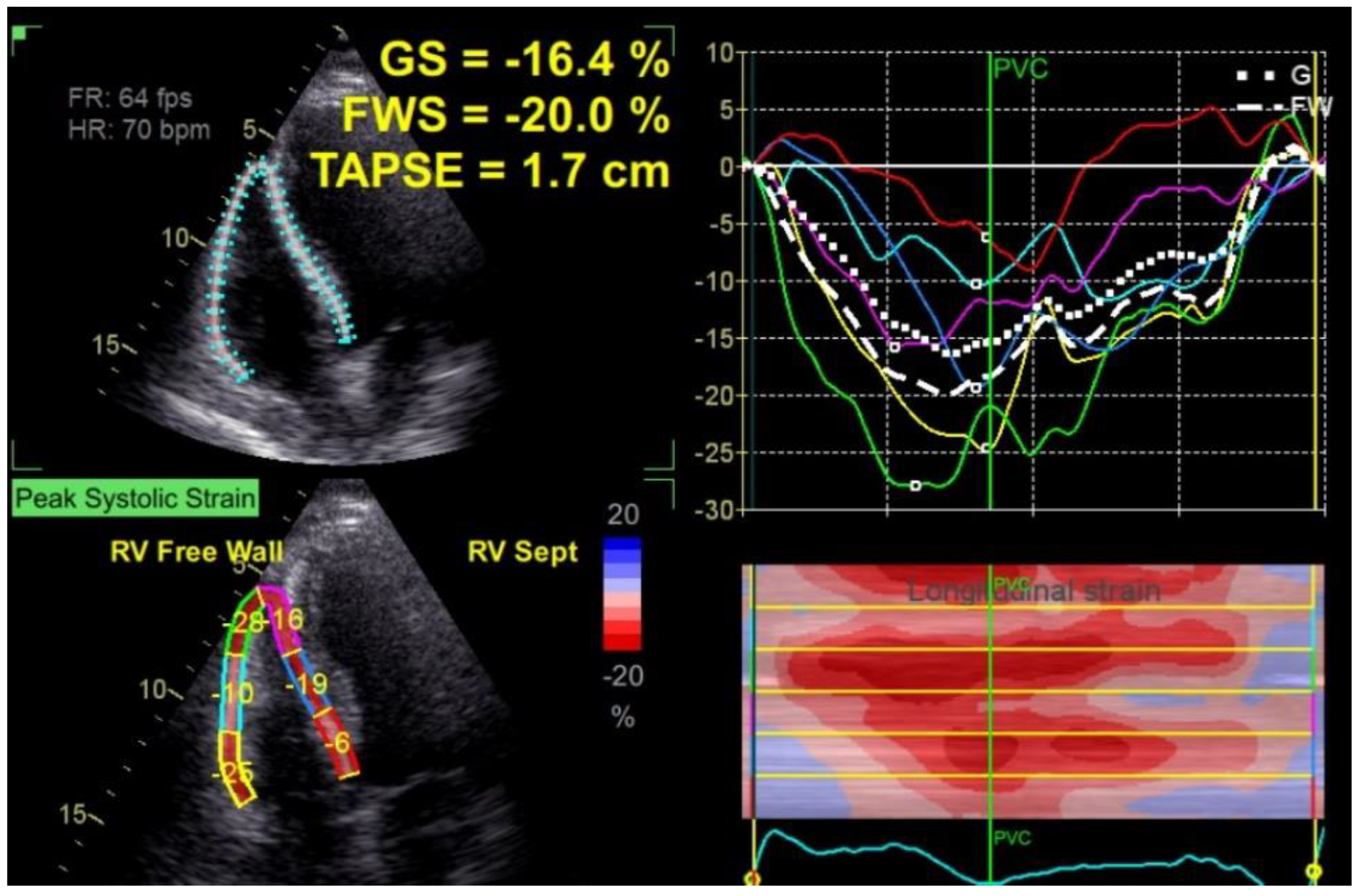
2.1.2. Right Ventricle Echocardiographic Evaluation
2.2. Follow-Up Period
2.3. Statistical Analysis
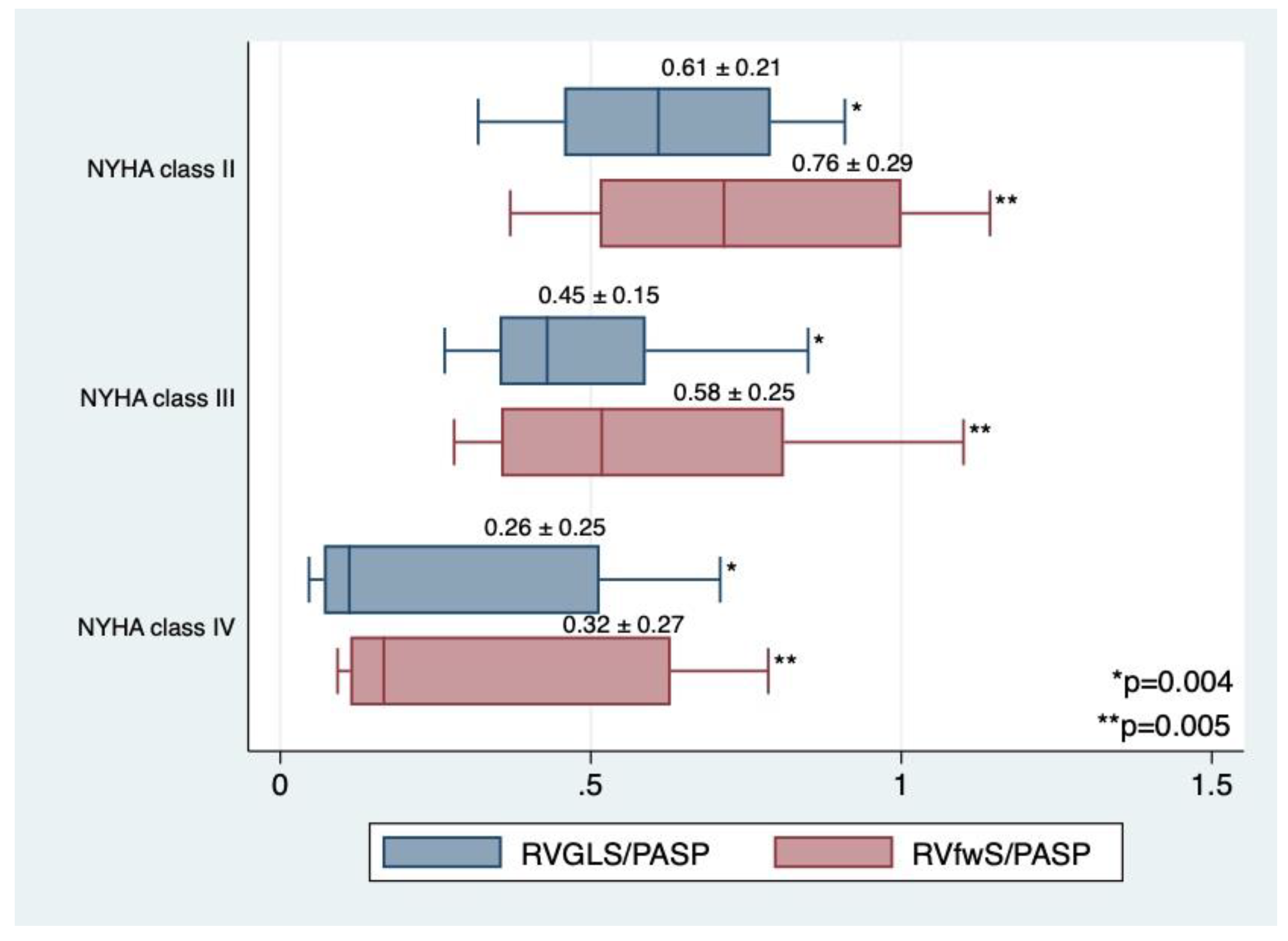
3. Results
3.1. Study Data
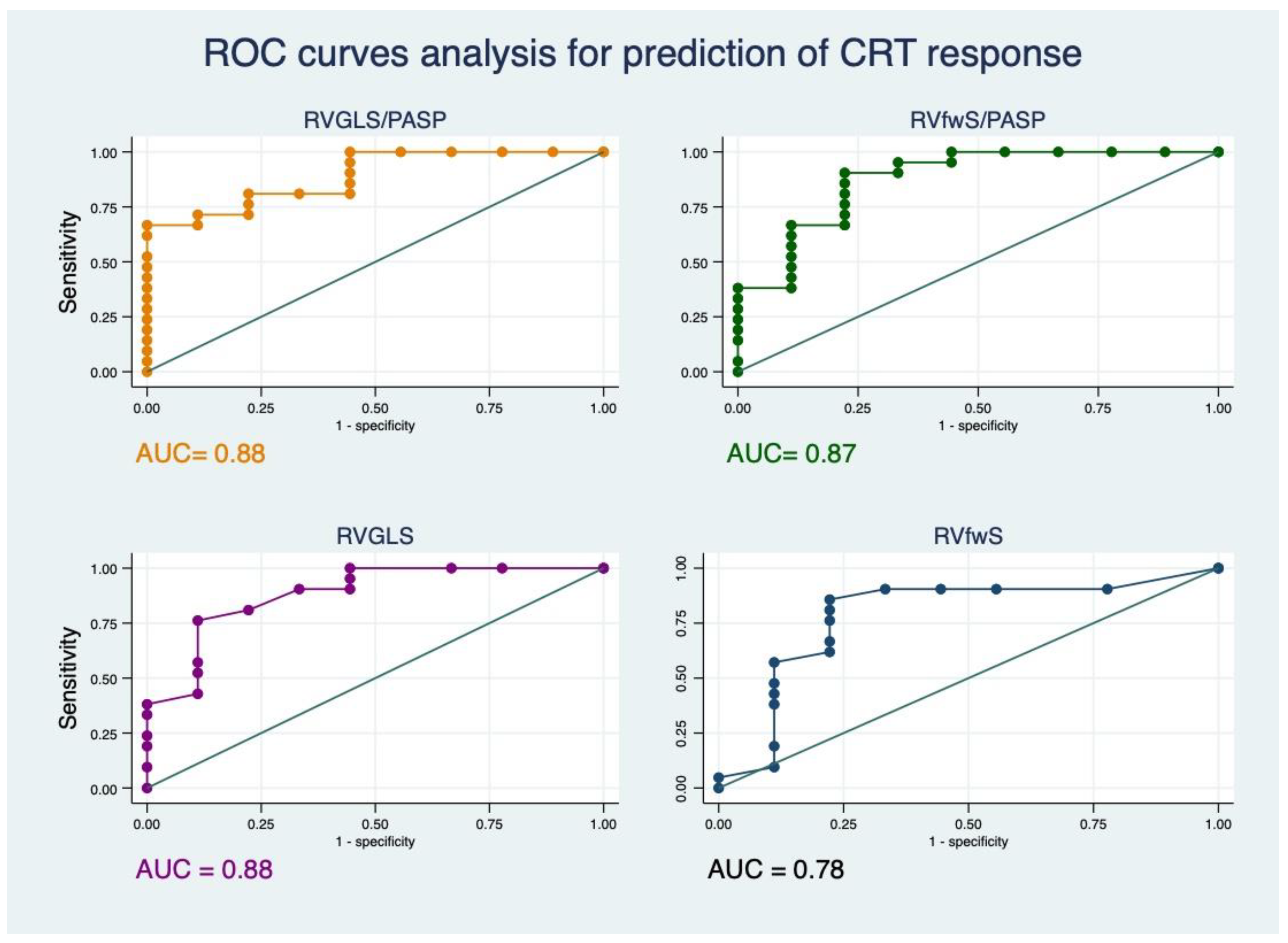
3.2. Evolution One Year after CRT
- RVGLS/PASP of 0.35 with sensibility of 80% and specificity of 77%.
- RVfwS/PASP of 0.41 with sensibility of 80% and specificity of 77%.
- RVGLS of −11% with sensibility of 80% and specificity of 77%.
- RVfwS of −13% with sensibility of 80% and specificity of 77%.
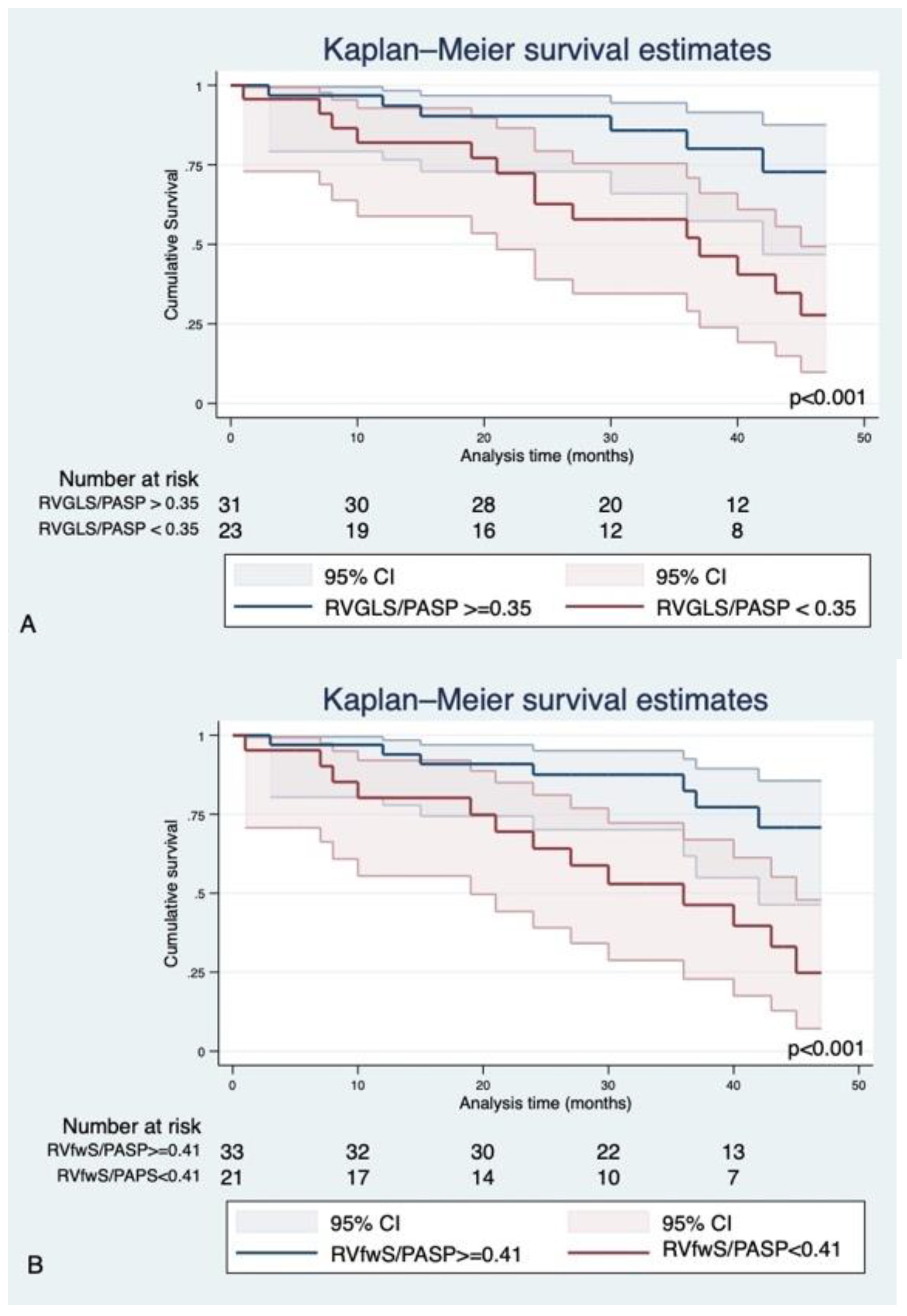
3.3. Survival Analysis
4. Discussion
- Low values of RVGLS/PASP and RVfwS/PASP are independently associated with a high risk of cardiovascular events (when corrected for gender, ischemic etiology, QRS morphology and duration).
- Low values of RVGLS/PASP and RVfwS/PASP predict non-response to CRT.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.-P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef] [PubMed]
- de Groote, P.; Millaire, A.; Foucher-Hossein, C.; Nugue, O.; Marchandise, X.; Ducloux, G.; Lablanche, J.M. Right Ventricular Ejection Fraction Is an Independent Predictor of Survival in Patients with Moderate Heart Failure. JACC. 1998. Available online: http://content.onlinejacc.org/ (accessed on 24 December 2014).
- Ghio, S.; Gavazzi, A.; Campana, C. Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. ACC Curr. J. Rev. 2001, 37, 183–188. [Google Scholar]
- Chatterjee, N.A.; Upadhyay, G.A.; Singal, G.; Parks, K.A.; Dec, G.W.; Singh, J.P.; Lewis, G.D. Pre-Capillary Pulmonary Hypertension and Right Ventricular Dilation Predict Clinical Outcome in Cardiac Resynchronization Therapy. JACC Heart Fail. 2014, 2, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Guazzi, M.; Dixon, D.; Labate, V.; Beussink-Nelson, L.; Bandera, F.; Cuttica, M.J.; Shah, S.J. RV Contractile Function and its Coupling to Pulmonary Circulation in Heart Failure with Preserved Ejection Fraction: Stratification of Clinical Phenotypes and Outcomes. JACC Cardiovasc. Imaging 2017, 10, 1211–1221. [Google Scholar] [CrossRef] [PubMed]
- Tello, K.; Wan, J.; Dalmer, A.; Vanderpool, R.; Ghofrani, H.A.; Naeije, R.; Roller, F.; Mohajerani, E.; Seeger, W.; Herberg, U.; et al. Validation of the Tricuspid Annular Plane Systolic Excursion/Systolic Pulmonary Artery Pressure Ratio for the Assessment of Right Ventricular-Arterial Coupling in Severe Pulmonary Hypertension. Circ. Cardiovasc. Imaging 2019, 12, e009047. [Google Scholar] [CrossRef] [PubMed]
- Guazzi, M.; Bandera, F.; Pelissero, G.; Castelvecchio, S.; Menicanti, L.; Ghio, S.; Temporelli, P.L.; Arena, R. Tricuspid annular plane systolic excursion and pulmonary arterial systolic pressure relationship in heart failure: An index of right ventricular contractile function and prognosis. Am. J. Physiol. Circ. Physiol. 2013, 305, H1373–H1381. [Google Scholar] [CrossRef] [PubMed]
- Iacoviello, M.; Monitillo, F.; Citarelli, G.; Leone, M.; Grande, D.; Antoncecchi, V.; Rizzo, C.; Terlizzese, P.; Romito, R.; Caldarola, P.; et al. Right ventriculo-arterial coupling assessed by two-dimensional strain: A new parameter of right ventricular function independently associated with prognosis in chronic heart failure patients. Int. J. Cardiol. 2017, 241, 318–321. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American society of echocardiography and the European association of cardiovascular imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 233–271. [Google Scholar] [CrossRef] [PubMed]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F.; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: An update from the American society of echocardiography and the European association of cardiovascular imaging. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 1321–1360. [Google Scholar] [CrossRef]
- Kossaify, A.; Nasr, M. Diastolic Dysfunction and the New Recommendations for Echocardiographic Assessment of Left Ventricular Diastolic Function: Summary of Guidelines and Novelties in Diagnosis and Grading. J. Diagn. Med. Sonogr. 2019, 35, 317–325. [Google Scholar] [CrossRef]
- Rudski, L.G.; Lai, W.W.; Afilalo, J.; Hua, L.; Handschumacher, M.D.; Chandrasekaran, K.; Solomon, S.D.; Louie, E.K.; Schiller, N.B. Guidelines for the Echocardiographic Assessment of the Right Heart in Adults: A Report from the American Society of Echocardiography. Endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J. Am. Soc. Echocardiogr. 2010, 23, 685–713. [Google Scholar]
- Borgdorff, M.A.J.; Dickinson, M.G.; Berger, R.M.F.; Bartelds, B. Right ventricular failure due to chronic pressure load: What have we learned in animal models since the NIH working group statement? Heart Fail. Rev. 2015, 20, 475–491. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mertens, L.L.; Friedberg, M.K. Imaging the right ventricle—Current state of the art. Nat. Rev. Cardiol. 2010, 7, 551–563. [Google Scholar] [CrossRef] [PubMed]
- Bragança, B.; Trêpa, M.; Santos, R.; Silveira, I.; Fontes-Oliveira, M.; Sousa, M.J.; Reis, H.; Torres, S.; Santos, M. Echocardiographic Assessment of Right Ventriculo-arterial Coupling: Clinical Correlates and Prognostic Impact in Heart Failure Patients Undergoing Cardiac Resynchronization Therapy. J. Cardiovasc. Imaging 2020, 28, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Kawata, T.; Daimon, M.; Kimura, K.; Nakao, T.; Lee, S.L.; Hirokawa, M.; Kato, T.S.; Watanabe, M.; Yatomi, Y.; Komuro, I. Echocardiographic assessment of right ventricular function in routine practice: Which parameters are useful to predict one-year outcome in advanced heart failure patients with dilated cardiomyopathy? J. Cardiol. 2017, 70, 316–322. [Google Scholar] [CrossRef] [PubMed]
- Storsten, P.; Aalen, J.M.; Boe, E.; Remme, E.W.; Gjesdal, O.; Larsen, C.K.; Andersen, Ø.S.; Eriksen, M.; Kongsgaard, E.; Duchenne, J.; et al. Mechanical Effects on Right Ventricular Function from Left Bundle Branch Block and Cardiac Resynchronization Therapy. JACC Cardiovasc. Imaging 2020, 13, 1475–1484. [Google Scholar] [CrossRef] [PubMed]
- Lumens, J.; Willemen, E.; Prinzen, F.W. Does the Right Go Wrong during Cardiac Resynchronization Therapy? JACC Cardiovasc. Imaging 2020, 13, 1485–1488. [Google Scholar] [CrossRef]
- Damy, T.; Ghio, S.; Rigby, A.S.; Hittinger, L.; Jacobs, S.; Leyva, F.; Delgado, J.F.; Daubert, J.C.; Gras, D.; Tavazzi, L.; et al. Interplay between right ventricular function and cardiac resynchronization therapy: An analysis of the care-HF trial (Cardiac resynchronization-heart Failure). J. Am. Coll. Cardiol. 2013, 61, 2153–2160. [Google Scholar] [CrossRef] [PubMed]
- Abdelhamid, M.A.; Ghanem, M.T.; Abdelmotaleb, A.M. Assessment of right ventriclular systolic function prior to cardiac resynchronization therapy: Does it make any difference? Indian Heart J. 2017, 69, 731–735. [Google Scholar] [CrossRef] [PubMed]
| Variables | Overall (n = 54) | Events (n = 18) | Without Events (n = 36) | p Value |
|---|---|---|---|---|
| Age (years) | 64.0 ± 13.8 | 59.5 ± 13 | 66 ± 12.19 | 0.09 |
| Male gender (%) | 58 | 64.2 | 53.9 | 0.5 |
| LBBB (%) | 70.7 | 66.6 | 70.0 | 0.8 |
| Ischemic etiology (%) | 28.8 | 50 | 19.2 | 0.04 |
| NYHA class (%) | 0.03 | |||
| II | 26.32 | 15 | 32 | |
| III | 39.47 | 23.08 | 48 | |
| IV | 34.21 | 61.65 | 20 | |
| QRS (ms) | 170.27 ± 21.4 | 176 ± 31.07 | 169 ± 17.7 | 0.44 |
| LV EDD (mm) | 65 ± 10.1 | 72 ± 12 | 61 ± 6.6 | 0.009 |
| LVEF (%) | 28.4 ± 1.3 | 26.69 ± 18.8 | 29.5 ± 6.18 | 0.2 |
| LVEDV (mL) | 212.7 ± 17 | 251 ± 150.37 | 183 ± 75.7 | 0.04 |
| LVESV (mL) | 156 ± 94 | 198 ± 139.74 | 131 ± 64.69 | 0.03 |
| E/e ratio baseline | 14 ± 11.4 | 21.028 ± 17.9 | 10.67 ± 4.54 | 0.02 |
| Tei index | 0.57 ± 0.22 | 0.66 ± 0.22 | 0.54 ± 0.21 | 0.18 |
| S wave (cm/sec) | 0.11 ± 0.029 | 0.09 ± 0.028 | 0.11 ± 0.029 | 0.04 |
| TAPSE/PASP (mm/mmHg) | 0.7 ± 0.2 | 0.5 ± 0.27 | 0.80± 0.22 | <0.001 |
| TAPSE (mm) | 21 ± 3.8 | 18.6 ± 3.62 | 22.3 ± 3.37 | <0.001 |
| PASP (mmHg) | 34 ± 13.6 | 44.42 ± 17.14 | 29.73 ± 9.8 | 0.001 |
| FAC RV (%) | 41.5 ± 18.3 | 31 ± 20.5 | 47.83 ± 15.47 | 0.01 |
| RVGLS (%) | 12 ± 5.2 | 9.3 ± 5.67 | 13.9 ± 4.5 | 0.009 |
| RVGLS/PASP | 0.43 ± 0.23 | 0.27 ± 0.25 | 0.50 ± 0.21 | 0.005 |
| RVfwS (%) | 16 ± 7.45 | 11.8 ± 5.49 | 18 ± 7.54 | 0.01 |
| RVfwS/PASP | 0.54 ± 0.29 | 0.32 ± 0.21 | 0.65 ± 0.29 | 0.003 |
| CRT Responders (n = 33) | CRT Non-Responders (n = 21) | |||||
|---|---|---|---|---|---|---|
| Variable | Baseline | One Year | p Value | Baseline | One Year | p Value |
| QRS (ms) | 173 ± 16.8 | 136 ± 12.7 | <0.001 | 177 ± 34.9 | 138.57 ± 16.7 | 0.005 |
| LV EF (%) | 30.06 ± 6.47 | 43.33 ± 7.90 | <0.001 | 22.2 ± 6.98 | 21.9 ± 7.88 | 0.75 |
| LAESV (mL) | 72.43 ± 29.2 | 61.18 ± 20.2 | 0.02 | 127 ± 45.6 | 110 ± 41.7 | 0.9 |
| RAESV (mL) | 39 ± 13.17 | 41.33 ± 12.11 | 0.46 | 74.62 ± 30 | 72 ± 42.3 | 0.5 |
| TAPSE (mm) | 22.5 ± 3.03 | 24 ± 2.9 | 0.057 | 18.02 ± 3.9 | 19.2 ± 2.7 | 0.14 |
| PASP (mmHg) | 28 ± 5.57 | 29.63 ± 5.12 | 0.3 | 46 ± 20.2 | 41 ± 14.7 | 0.27 |
| TAPSE/PASP (mm/mmHg) | 0.8 ± 0.22 | 0.8 ± 0.17 | 0.5 | 0.50 ± 0.33 | 0.54 ± 0.26 | 0.7 |
| RVGLS (%) | 14.4 ± 3.7 | 16.3 ± 3.08 | 0.03 | 7.4 ± 4.5 | 8.6 ± 5.07 | 0.053 |
| RVGLS/PASP | 0.53 ± 0.19 | 0.56 ± 0.15 | 0.36 | 0.21 ± 0.17 | 0.28 ± 0.10 | 0.06 |
| RVfwS (%) | 17.2 ± 6.01 | 18.04 ± 5.14 | 0.52 | 10.44 ± 6.26 | 10.84 ± 6.18 | 0.69 |
| RVfwS/PASP | 0.61 ± 0.23 | 0.63 ± 0.23 | 0.15 | 0.28 ± 0.22 | 0.32 ± 0.24 | 0.15 |
| Variables | HR | C-Index | p Value | 95% CI |
|---|---|---|---|---|
| Univarate analysis | ||||
| Gender (female) | 0.69 | 0.50 | 0.55 | 0.20–2.32 |
| Etiology (ischemic) | 2.60 | 0.69 | 0.09 | 0.83–8.11 |
| NYHA class | 2.57 | 0.67 | 0.04 | 1.02–6.48 |
| QRS duration | 1.02 | 0.59 | 0.12 | 0.99–1.04 |
| LBBB | 1.10 | 0.49 | 0.88 | 0.28–4.21 |
| TAPSE | 0.82 | 0.69 | 0.02 | 0.69–0.96 |
| RVGLS | 0.88 | 0.61 | 0.06 | 0.78–1.00 |
| RVfwS | 0.91 | 0.63 | 0.09 | 0.82–1.01 |
| PASP | 1.03 | 0.78 | 0.02 | 1–1.07 |
| TAPSE/PASP | 0.046 | 0.73 | 0.009 | 0.004–0.45 |
| RVGLS/PASP | 0.039 | 0.65 | 0.03 | 0.001–0.8 |
| RVfwS/PASP | 0.049 | 0.70 | 0.02 | 0.003–0.72 |
| Multivariate analysis | ||||
| Gender (female) | 1.48 | 0.6 | 0.28–7.79 | |
| Etiology | 4.63 | 0.05 | 0.94–22.7 | |
| QRS duration | 1.01 | 0.18 | 0.99–1.03 | |
| LBBB | 2.2 | 0.35 | 0.39–13.40 | |
| TAPSE/PASP | 0.045 | 0.76 | 0.053 | 0.001–1.02 |
| Gender (female) | 2.82 | 0.2 | 0.40–19.86 | |
| Etiology | 15.6 | 0.01 | 1.62–149 | |
| QRS duration | 1.01 | 0.36 | 0.98–1.03 | |
| LBBB | 4.93 | 0.13 | 0.61–39.39 | |
| RVGLS | 0.83 | 0.78 | 0.04 | 0.70–0.99 |
| Gender (female) | 2.20 | 0.44 | 0.28–17.19 | |
| Etiology | 15.32 | 0.02 | 1.33–175 | |
| QRS duration | 1.01 | 0.21 | 0.99–1.03 | |
| LBBB | 4.44 | 0.16 | 0.55–35.5 | |
| RVfwS | 0.86 | 0.72 | 0.059 | 0.74–1.00 |
| Gender (female) | 1.35 | 0.7 | 0.24–7.48 | |
| Etiology | 6.29 | 0.03 | 1.12–35.52 | |
| QRS duration | 1.01 | 0.23 | 0.99–1.03 | |
| LBBB | 3.24 | 0.23 | 0.45–23.13 | |
| PASP | 1.05 | 0.75 | 0.03 | 1.00–1.10 |
| Gender (female) | 2.62 | 0.32 | 0.39–17.62 | |
| Etiology | 15.3 | 0.01 | 1.85–127.56 | |
| QRS duration | 1.01 | 0.20 | 0.99–1.03 | |
| LBBB | 4.44 | 0.11 | 0.68–28.9 | |
| RVGLS/PASP | 0.018 | 0.80 | 0.02 | 0.0005–0.64 |
| Gender (female) | 2.37 | 0.39 | 0.31–17.68 | |
| Etiology | 20.5 | 0.01 | 1.98–212.62 | |
| QRS duration | 1.01 | 0.99 | 0.99–1.04 | |
| LBBB | 6.19 | 0.07 | 0.80–47.33 | |
| RVfwS/PASP | 0.015 | 0.82 | 0.01 | 0.0004–0.52 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deaconu, S.; Deaconu, A.; Scarlatescu, A.; Petre, I.; Onciul, S.; Vijiiac, A.; Zamfir, D.; Marascu, G.; Iorgulescu, C.; Radu, A.D.; et al. Ratio between Right Ventricular Longitudinal Strain and Pulmonary Arterial Systolic Pressure: Novel Prognostic Parameter in Patients Undergoing Cardiac Resynchronization Therapy. J. Clin. Med. 2021, 10, 2442. https://doi.org/10.3390/jcm10112442
Deaconu S, Deaconu A, Scarlatescu A, Petre I, Onciul S, Vijiiac A, Zamfir D, Marascu G, Iorgulescu C, Radu AD, et al. Ratio between Right Ventricular Longitudinal Strain and Pulmonary Arterial Systolic Pressure: Novel Prognostic Parameter in Patients Undergoing Cardiac Resynchronization Therapy. Journal of Clinical Medicine. 2021; 10(11):2442. https://doi.org/10.3390/jcm10112442
Chicago/Turabian StyleDeaconu, Silvia, Alexandru Deaconu, Alina Scarlatescu, Ioana Petre, Sebastian Onciul, Aura Vijiiac, Diana Zamfir, Gabriela Marascu, Corneliu Iorgulescu, Andrei Dan Radu, and et al. 2021. "Ratio between Right Ventricular Longitudinal Strain and Pulmonary Arterial Systolic Pressure: Novel Prognostic Parameter in Patients Undergoing Cardiac Resynchronization Therapy" Journal of Clinical Medicine 10, no. 11: 2442. https://doi.org/10.3390/jcm10112442
APA StyleDeaconu, S., Deaconu, A., Scarlatescu, A., Petre, I., Onciul, S., Vijiiac, A., Zamfir, D., Marascu, G., Iorgulescu, C., Radu, A. D., Bogdan, S., & Vatasescu, R. (2021). Ratio between Right Ventricular Longitudinal Strain and Pulmonary Arterial Systolic Pressure: Novel Prognostic Parameter in Patients Undergoing Cardiac Resynchronization Therapy. Journal of Clinical Medicine, 10(11), 2442. https://doi.org/10.3390/jcm10112442








