Modulation of Lipid Profile and Lipoprotein Subfractions in Overweight/Obese Women at Risk of Cardiovascular Diseases through the Consumption of Apple/Berry Juice
Abstract
1. Introduction
2. Materials and Methods
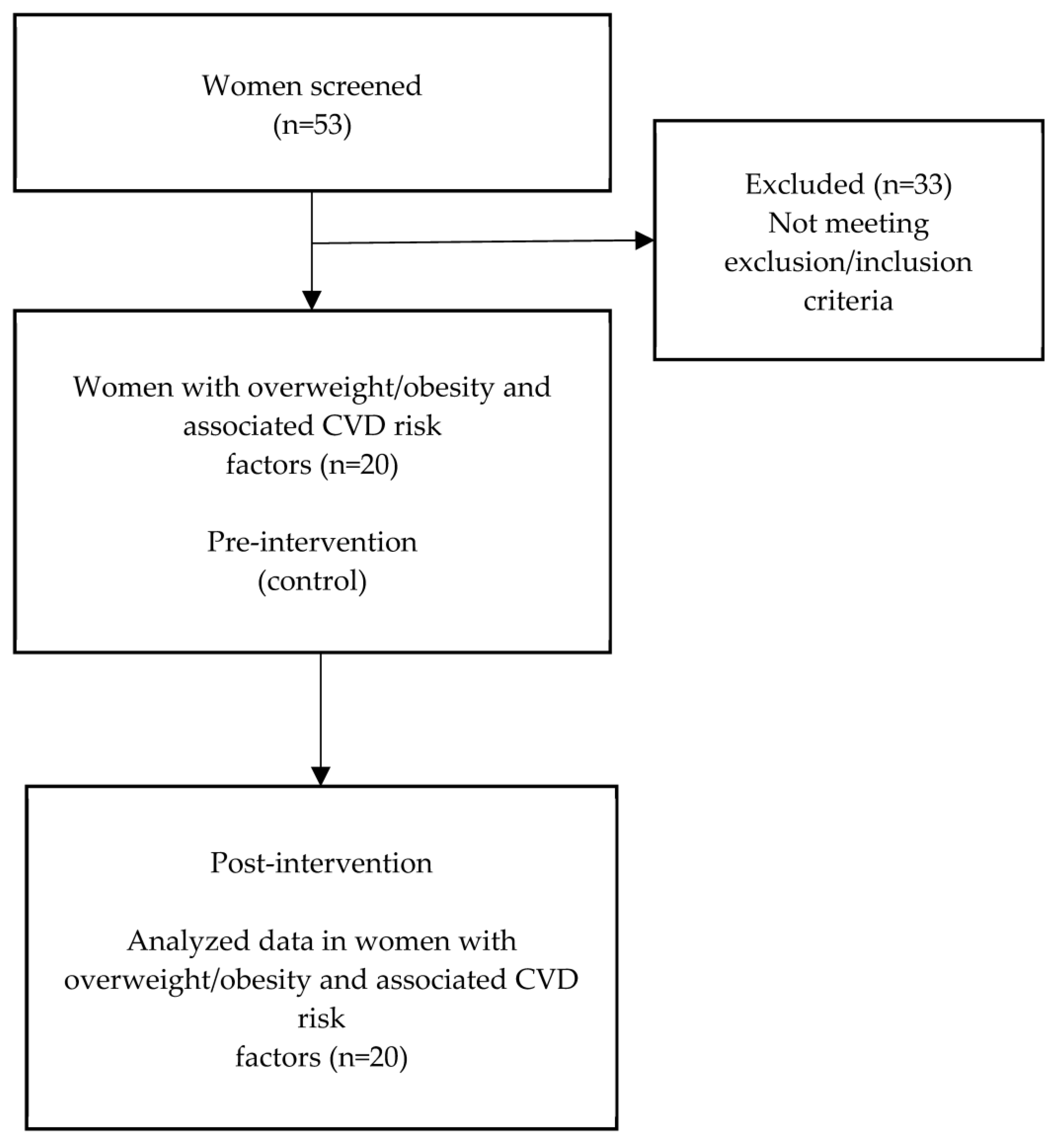
2.1. Participants and Study Design
2.2. Intervention
2.3. Anthropometric Measurements
2.4. Preparation of Blood Samples
2.5. Clinical Parameters
2.6. Statistical Analysis
3. Results
3.1. Characteristics of Study Participants
3.2. Phenolic Compounds in Apple/Berry Juice
3.3. Changes in Anthropometric Parameters, Blood Pressure, and Lipid Profile
3.4. Changes in Lipid Profile, hs-CRP, and TAS in Women with LDL Subclass Phenotype B
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Guo, F.; Garvey, T. Cardiometabolic disease Risk in Metabolically Healthy and Unhealthy Obesity: Stability of Metabolic Health Status in Adults. Obesity 2016, 24, 516–525. [Google Scholar] [CrossRef] [PubMed]
- Chung, Y.; Ding, C.; Magkos, F. The epidemiology of obesity. Metabolism 2019, 92, 6–10. [Google Scholar] [CrossRef]
- Battineni, G.; Sagaro, G.G.; Chintalapudi, N.; Amenta, F.; Tomassoni, D.; Tayebati, S.K. Impact of Obesity-Induced Inflammation on Cardiovascular Diseases (CVD). Int. J. Mol. Sci. 2021, 22, 4798. [Google Scholar] [CrossRef] [PubMed]
- Conte, M.; Petraglia, L.; Poggio, P.; Valerio, V.; Cabaro, S.; Campana, P.; Comentale, G.; Attena, E.; Russo, V.; Pilato, E.; et al. Inflammation and Cardiovascular Diseases in the Elderly: The Role of Epicardial Adipose Tissue. Front. Med. 2022, 9, 844266. [Google Scholar] [CrossRef] [PubMed]
- Alexandros Tsoupras, R.L.; Zabetakis, I. Inflammation, not Cholesterol, Is a Cause of Chronic Disease. Nutrients 2018, 10, 604. [Google Scholar] [CrossRef]
- Atapattu, P.M. Obesity at menopause: An expanding problem. J. Patient Care 2015, 1, 1000103. [Google Scholar] [CrossRef]
- Bakhtiyari, M.; Kazemian, E.; Kabir, K.; Hadaegh, F.; Aghajanian, S.; Mardi, P.; Ghahfarokhi, N.T.; Ghanbari, A.; Mansournia, M.A.; Azizi, F. Contribution of obesity and cardiometabolic risk factors in developing cardiovascular disease: A population-based cohort study. Sci. Rep. 2022, 12, 1544. [Google Scholar] [CrossRef]
- Faulkner, J.L. Obesity-associated cardiovascular risk in women: Hypertension and heart failure. Clin. Sci. 2021, 135, 1523–1544. [Google Scholar] [CrossRef]
- Kozakowski, J.; Gietka-czernel, M.; Leszczyńska, D.; Majos, A. Obesity in menopause–our negligence or an unfortunate inevitability? Menopause Rev. 2017, 16, 61–65. [Google Scholar] [CrossRef]
- Cífková, R.; Krajčoviechová, A. Dyslipidemia and Cardiovascular Disease in Women. Curr. Cardiol. Rep. 2015, 17, 52. [Google Scholar] [CrossRef]
- Fonseca, I.M.H.; da Silva, I.T.; Ferreira, S.R.G. Impact of menopause and diabetes on atherogenic lipid profile: Is it worth to analyse lipoprotein subfractions to assess cardiovascular risk in women ? Diabetol. Metab. Syndr. 2017, 9, 22. [Google Scholar] [CrossRef] [PubMed]
- Cleeman, J.; Grundy, S.; Becker, D.; Clark, L.; Cooper, R.; Denke, M.; Howard, W.; Hunninghake, D.; Illingworth, D. Executive summary of the third report of the national cholesterol education program (NCEP). Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef]
- Khalil, R.M.A.Z.; Al-Azab, D.A.M.; Akl, O.A. Is sdLDL a valuable screening tool for cardiovascular disease in patients with metabolic syndrome? Alexandria J. Med. 2017, 53, 299–305. [Google Scholar] [CrossRef]
- Vekic, J.; Zeljkovic, A.; Cicero, A.F.G.; Sonmez, A.; Rizzo, M. Atherosclerosis Development and Progression: The Role of Atherogenic Small, Dense LDL. Medicina 2022, 58, 299. [Google Scholar] [CrossRef] [PubMed]
- Kanonidou, C. Small dense low-density lipoprotein: Analytical review. Clin. Chim. Acta 2021, 520, 172–178. [Google Scholar] [CrossRef]
- Thongtang, N.; Sukmawan, R.; Llanes, J.E.; Lee, Z.-V. Dyslipidemia management for primary prevention of cardiovascular events: Best in-clinic practices. Prev. Med. Rep. 2022, 27, 101819. [Google Scholar] [CrossRef]
- Panchal, S.K.; Brown, L. Cholesterol versus Inflammation as Cause of Chronic Diseases. Nutrients 2019, 11, 2332. [Google Scholar] [CrossRef]
- Sikand, G.; Severson, T. Top 10 dietary strategies for atherosclerotic cardiovascular risk reduction. Am. J. Prev. Cardiol. 2020, 4, 100106. [Google Scholar] [CrossRef]
- Zuraini, N.Z.A.; Sekar, M.; Wu, Y.S.; Gan, S.H.; Bonam, S.R.; Mat Rani, N.N.I.; Begum, M.Y.; Lum, P.T.; Subramaniyan, V.; Fuloria, N.K.; et al. Promising Nutritional Fruits Against Cardiovascular Diseases: An Overview of Experimental Evidence and Understanding Their Mechanisms of Action. Vasc. Health Risk Manag. 2021, 17, 739–769. [Google Scholar] [CrossRef]
- Pap, N.; Fidelis, M.; Azevedo, L.; Wang, D.; Arau, M.; Mocan, A.; Penha, E.; Pereira, R.; Xavier-Santos, D.; Ana, A.S.S.; et al. Berry polyphenols and human health: Evidence of antioxidant, anti-inflammatory, microbiota modulation, and cell-protecting effects. Curr. Opin. Food Sci. 2021, 42, 167–186. [Google Scholar] [CrossRef]
- Poli, A.; Barbagallo, C.M.; Cicero, A.F.G.; Corsini, A.; Manzato, E.; Trimarco, B.; Bernini, F.; Visioli, F.; Canzone, G.; Crescini, C.; et al. Nutraceuticals and functional foods for the control of plasma cholesterol levels. An intersociety position paper. Pharmacol. Res. 2018, 134, 51–60. [Google Scholar] [CrossRef]
- Shukla, S.K.; Gupta, S.; Ojha, S.K.; Sharma, S.B. Cardiovascular friendly natural products: A promising approach in the management of CVD. Nat. Prod. Res. Res. 2010, 24, 873–898. [Google Scholar] [CrossRef]
- Ma, L.; Sun, Z.; Zeng, Y.; Luo, M.; Yang, J. Molecular Mechanism and Health Role of Functional Ingredients in Blueberry for Chronic Disease in Human Beings. Mol. Sci. 2018, 19, 2785. [Google Scholar] [CrossRef]
- Novotny, J.A.; Baer, D.J.; Khoo, C.; Gebauer, S.K.; Charron, C.S. Cranberry Juice Consumption Lowers Markers of Cardiometabolic Risk, Including Blood Pressure and Circulating C-Reactive Protein, Triglyceride, and Glucose Concentrations. J. Nutr. 2015, 145, 1185–1193. [Google Scholar] [CrossRef]
- Ruel, G.; Pomerleau, S.; Couture, P.; Lamarche, B.; Couillard, C. Changes in plasma antioxidant capacity and oxidized low-density lipoprotein levels in men after short-term cranberry juice consumption. Metabolism 2005, 54, 856–861. [Google Scholar] [CrossRef]
- Kim, B.; Ku, C.S.; Pham, T.X.; Park, Y.; Martin, D.A.; Xie, L.; Taheri, R.; Lee, J.; Bolling, B.W. Aronia melanocarpa (chokeberry) polyphenol–rich extract improves antioxidant function and reduces total plasma cholesterol in apolipoprotein E knockout mice. Nutr. Res. 2013, 33, 406–413. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhao, Y.; Liu, X.; Chen, X.; Ding, C.; Dong, L.; Zhang, J.; Sun, S.; Ding, Q.; Khatoom, S.; et al. Chokeberry (Aronia melanocarpa) as a new functional food relationship with health: An overview. J. Future Foods 2022, 1, 168–178. [Google Scholar] [CrossRef]
- Kwan, H.Y.; Chao, X.; Su, T.; Fu, X.; Wing, A.K.; Fong, W.; Yu, Z. The anticancer and antiobesity effects of Mediterranean diet. Crit. Rev. Food Sci. Nutr. 2017, 57, 82–94. [Google Scholar] [CrossRef]
- Skrovankova, S.; Sumczynski, D.; Mlcek, J.; Jurikova, T.; Sochor, J. Bioactive Compounds and Antioxidant Activity in Different Types of Berries. Int. J. Mol. Sci. 2015, 16, 24673–24706. [Google Scholar] [CrossRef]
- Thiese, M.S. Observational and interventional study design types; an overview. Lessons Biostat. 2014, 24, 199–210. [Google Scholar] [CrossRef]
- Harris, A.D.; McGregor, J.C.; Perencevich, E.N.; Furuno, J.P.; Zhu, J.; Peterso, D.E.; Finkelstein, J. The Use and Interpretation of Quasi-Experimental Studies in Medical Informatics. J. Am. Med. Inform. Assoc. 2006, 13, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Andrew, L. Waterhouse. Determination of total phenolics. Curr. Protoc. food Anal. Chem. 2002, I1-1. [Google Scholar] [CrossRef]
- Giusti, M.M.; Wrolstad, R.E. Characterization and measurement of anthocyanins by UV-visible spectroscopy. In Current Protocols in Food Analytical Chemistry; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2001; pp. F1.2.1–F1.2.13. [Google Scholar] [CrossRef]
- Justesen, U.; Knuthsen, P. Composition of flavonoids in fresh herbs and calculation of flavonoid intake by use of herbs in traditional Danish dishes. Food Chem. 2001, 73, 245–250. [Google Scholar] [CrossRef]
- Brand-Williams, W.; Cuvelier, M.E.; Berset, C. Use of a Free Radical Method to Evaluate Antioxidant Activity. LWT-Food Sci. Technol. 1995, 28, 25–30. [Google Scholar] [CrossRef]
- Sánchez-Moreno, C.; Larrauri, J.A.; Saura-Calixto, F. A procedure to measure the antiradical efficiency of polyphenols. J. Sci. Food Agric. 1998, 76270, 270–276. [Google Scholar] [CrossRef]
- Skrzypczak, M.; Szwed, A.; Pawli, R.; Skrzypulec, V. Assessment of the BMI, WHR and W/Ht in pre- and postmenopausal women. Anthropol. Rev. 2007, 70, 3–13. [Google Scholar] [CrossRef]
- Laposata, M. Laboratory Medicine Diagnosis of Disease in Clinical Laboratory 2/E, 3rd ed.; McGraw-Hill Education: New York, NY, USA, 2014. [Google Scholar]
- Muntner, P.; Shimbo, D.; Carey, R.M.; Charleston, J.B.; Gaillard, T.; Misra, S.; Myers, M.G.; Ogedegbe, G.; Schwartz, J.E.; Townsend, R.R.; et al. Measurement of Blood Pressure in Humans: A scientific statement from the American Heart Association. Hypertension 2019, 73, 35–66. [Google Scholar] [CrossRef]
- Millán, J.; Pintó, X.; Muñoz, A.; Zúñiga, M.; Rubiés-Prat, J.; Pallardo, L.F.; Masana, L.; Mangas, A.; Hernández-Mijares, A.; González-Santos, P.; et al. Lipoprotein ratios: Physiological significance and clinical usefulness in cardiovascular prevention. Vasc. Heal. Risk Manag. 2009, 5, 757–765. [Google Scholar]
- Ridker, M. High-Sensitivity C-Reactive Protein. J. Am. Coll. Cardiol. 2016, 67, 712–723. [Google Scholar] [CrossRef]
- Habauzit, V.; Verny, M.; Milenkovic, D.; Barber-chamoux, N.; Mazur, A.; Morand, C. Flavanones protect from arterial stiffness in postmenopausal women consuming grapefruit juice for 6 mo: A randomized, controlled, crossover trial. Am. J. Cinical Nutr. 2015, 102, 66–74. [Google Scholar] [CrossRef]
- Bondonno, N.P.; Bondonno, C.P.; Blekkenhorst, L.C.; Considine, M.J.; Maghzal, G.; Stocker, R.; Woodman, R.J.; Ward, N.C.; Hodgson, J.M.; Croft, K.D. Flavonoid-Rich Apple Improves Endothelial Function in Individuals at Risk for Cardiovascular Disease: A Randomized Controlled Clinical Trial. Mol. Nutr. Food Res. 2018, 62, 1700674. [Google Scholar] [CrossRef]
- Grosso, G.; Godos, J.; Currenti, W.; Micek, A.; Falzone, L.; Libra, M.; Giampieri, F.; Forbes-hern, T.Y.; Quiles, J.L.; Battino, M.; et al. The Effect of Dietary Polyphenols on Vascular Health and Hypertension: Current Evidence and Mechanisms of Action. Nutrients 2022, 14, 545. [Google Scholar] [CrossRef]
- Szajdek, A.; Borowska, E.J. Bioactive Compounds and Health-Promoting Properties of Berry Fruits: A Review. Plant Foods Hum. Nutr. 2008, 63, 147–156. [Google Scholar] [CrossRef]
- Gralec, M.; Wawer, I.; Zawada, K. Aronia melanocarpa berries: Phenolics composition and antioxidant properties changes during fruit development and ripening. Emir. J. Food Agric. 2019, 31, 214–221. [Google Scholar] [CrossRef]
- Mckay, D.L.; Blumberg, J.B. Cranberries (Vaccinium macrocarpon) and cardiovascular disease risk factors. Nutr. Rev. 2007, 65, 490–502. [Google Scholar] [CrossRef]
- Olas, B. Berry Phenolic Antioxidants—Implications for Human Health? Front. Pharmacol. 2018, 9, 78. [Google Scholar] [CrossRef]
- Sirtori, C.R.; Fumagalli, R. LDL-cholesterol lowering or HDL-cholesterol raising for cardiovascular prevention A lesson from cholesterol turnover studies and others. Atherosclerosis 2006, 186, 1–11. [Google Scholar] [CrossRef]
- Huang, H.; Chen, G.; Liao, D.; Zhu, Y.; Xue, X. Effects of Berries Consumption on Cardiovascular Risk Factors: A Meta-analysis with Trial Sequential Analysis of Randomized Controlled Trials. Sci. Rep. 2016, 23, 23625. [Google Scholar] [CrossRef]
- Grohmann, T.; Litts, C.; Horgan, G.; Zhang, X.; Hoggard, N.; Russell, W.; Roos, B. Efficacy of Bilberry and Grape Seed Extract Supplement Interventions to Improve Glucose and Cholesterol Metabolism and Blood Pressure in Different Populations—A Systematic Review of the Literature. Nutrients 2021, 13, 1692. [Google Scholar] [CrossRef]
- Koutsos, A.; Riccadonna, S.; Ulaszewska, M.M.; Franceschi, P.; Trošt, K.; Galvin, A.; Braune, T.; Fava, F.; Perenzoni, D.; Mattivi, F.; et al. Two apples a day lower serum cholesterol and improve cardiometabolic biomarkers in mildly hypercholesterolemic adults: A randomized, controlled, crossover trial. Am. J. Cinical Nutr. 2020, 111, 307–318. [Google Scholar] [CrossRef]
- Kunutsor, S.K.; Zaccardi, F.; Karppi, J.; Kurl, S.; Laukkanen, J.A. Is High Serum LDL/HDL Cholesterol Ratio an Emerging Risk Factor for Sudden Cardiac Death ? Findings from the KIHD Study. J. Atheroscler. Thromb. 2017, 24, 600–608. [Google Scholar] [CrossRef] [PubMed]
- Hsu, S.H.; Jang, M.; Torng, P.; Su, T. Positive Association Between Small Dense Low-Density Lipoprotein Cholesterol Concentration and Biomarkers of Inflammation, Thrombosis, and Prediabetes in Non-Diabetic Adults. J. Atheroscler. Thromb. 2019, 26, 624–635. [Google Scholar] [CrossRef] [PubMed]
- Izumida, T.; Nakamura, Y.; Hino, Y.; Ishikawa, S. Combined Effect of Small Dense Low-Density Lipoprotein Cholesterol (sdLDL-C) and Remnant-Like Particle Cholesterol (RLP-C) on Low-Grade. J. Atheroscler. Thromb. 2020, 24, 319–330. [Google Scholar] [CrossRef] [PubMed]
- Jin, X.; Yang, S.; Lu, J.; Wu, M. Small, Dense Low-Density Lipoprotein-Cholesterol and Atherosclerosis: Relationship and Therapeutic Strategies. Front. Cardiovasc. Med. 2022, 8, 804214. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Liu, Y.; Yin, S.; Chen, N.; Bai, X.; Ke, Q.; Shen, J.; Xia, M. Small dense LDL cholesterol is associated with metabolic syndrome traits independently of obesity and inflammation. Nutr. Metab. 2019, 16, 7. [Google Scholar] [CrossRef]
- Nafari, A.; Mohammadifard, N.; Haghighatdoost, F.; Nasirian, S.; Najafian, J.; Sadeghi, M.; Roohafza, H.; Sarrafzadegan, N. High-sensitivity C-reactive protein and low-density lipoprotein cholesterol association with incident of cardiovascular events: Isfahan cohort study. BMC Cardiovasc. Disord. 2022, 22, 241. [Google Scholar] [CrossRef]
- Zitnanova, I.; Oravec, S.; Janubova, M.; Konarikova, K.; Dvorakova, M.; Laubertova, L.; Kralova, M.; Simko, M.; Muchova, J. Gender differences in LDL and HDL subfractions in atherogenic and nonatherogenic phenotypes. Clin. Biochem. 2020, 79, 9–13. [Google Scholar] [CrossRef]
- Nikawa, T.; Ulla, A.; Sakakibara, I. Polyphenols and Their Effects on Muscle Atrophy and Muscle Health. Molecules 2021, 26, 4887. [Google Scholar] [CrossRef]
- Hwang, S.J.; Yoon, W.B.; Lee, O.-H.; Cha, S.J.; Kim, J.D. Radical-scavenging-linked antioxidant activities of extracts from black chokeberry and blueberry cultivated in Korea. Food Chem. 2014, 146, 71–77. [Google Scholar] [CrossRef]
- Pedersen, C.B.; Kyle, J.; Jenkinson, A.; Gardner, P.T.; Mcphail, D.B.; Duthie, G.G. Effects of blueberry and cranberry juice consumption on the plasma antioxidant capacity of healthy female volunteers. Eur. J. Clin. Nutr. 2000, 54, 405–408. [Google Scholar] [CrossRef]

| Parameters | Standard/Optimal Range | Women (n = 20) Baseline | ||
|---|---|---|---|---|
| Mean ± SD | Max | Min | ||
| Age (years) | 52.95 ± 5.80 | 60 | 41 | |
| Bodyweight (kg) | 75.25 ± 8.34 | 100.40 | 57.20 | |
| BMI (kg/m2) | 18.5–24.9 | 28.01 ± 2.88 | 37.33 | 25.05 |
| PBF (%) | 18–28 | 38.35 ± 5.05 | 48.81 | 28.60 |
| WHR | 0.75–0.85 | 0.97 ± 0.05 | 1.08 | 0.90 |
| SMM (kg) | 31.7–38.7 | 25.52± 2.81 | 30.06 | 20.84 |
| Systolic blood pressure (mm Hg) | ˂120 | 137.40 ± 16.75 | 169 | 115 |
| Diastolic blood pressure (mm Hg) | ˂80 | 81.95 ± 9.90 | 99 | 60 |
| T-C (mmol/L) | ˂5.19 | 6.29 ± 0.99 | 8.51 | 4.94 |
| TG (mmol/L) | ˂1.7 | 1.47 ± 0.66 | 2.42 | 0.44 |
| HDL-C (mmol/L) | ≥1.55 | 1.30 ± 0.29 | 1.83 | 0.86 |
| LDL-C (mmol/L) | ˂2.6 | 4.19 ± 0.83 | 6.03 | 3.12 |
| LDL/HDL (mmol/L) | ˂2.5 | 3.40 ± 0.99 | 5.15 | 2.04 |
| hs-CRP (mg/L) | ˂1 | 1.90 ± 2.35 | 10.78 | 0.36 |
| Glucose (mmol/L) | 4.0–5.5 | 5.50 ± 0.72 | 7.35 | 4.51 |
| Parameter | Units | Results |
|---|---|---|
| TPC | µg/mL | 286.25 ± 8.41 |
| TA | µg/mL | 7.82 ± 0.93 |
| Rutin | µg/mL | 64.64 ±7.12 |
| Quercetin | µg/mL | 20.77 ± 0.80 |
| Kaempferol | µg/mL | 0.41 ± 0.03 |
| Chlorogenic acid | µg/mL | 27.47 ± 2.29 |
| Gallic acid | µg/mL | 6.80 ± 0.62 |
| Rosmarinic acid | µg/mL | 1.24 ± 0.11 |
| Caffeic acid | µg/mL | 1.31 ± 0.12 |
| Antioxidant activity (AA), inhibition of DPPH | % | 73.24 ± 1.85 |
| Parameters | Overweight/Obese Women with Associated CVD Risk Factors (n = 20) | ||
|---|---|---|---|
| Pre | Post | p-Value | |
| Anthropometric parameters | |||
| Body weight (kg) | 74.30 (69.35–79.65) | 75.55 (69.68–81.23) | NS |
| BMI (kg/m2) | 27.79 (25.86–28.91) | 27.61 (25.87–28.97) | NS |
| WHR | 0.96 (0.92–0.99) | 0.97 (0.92–0.99) | NS |
| PBF (%) | 38.16 (34.80–42.47) | 37.47 (33.59–41.01) | NS |
| SMM (kg) | 25.74 (23.22–27.65) | 25.89(23.24–27.93) | 0.025 |
| Blood pressure | |||
| Systolic blood pressure (mm Hg) | 135 (124–150) | 131 (116–142) | NS |
| Diastolic blood pressure (mm Hg) | 82 (75–90) | 79 (74–85) | NS |
| Blood lipids | |||
| T-C (mmol/L) | 6.15 (5.59–6.82) | 6.01 (5.39–6.34) | 0.015 |
| LDL-C (mmol/L) | 4.00 (3.55–4.77) | 3.83 (3.48–4.26) | NS |
| HDL-C (mmol/L) | 1.27 (1.12–1.59) | 1.51 (1.35–1.75) | <0.001 |
| LDL/HDL (mmol/L) | 3.56 (2.41–4.26) | 2.67 (2.28–3.11) | <0.001 |
| TG (mmol/L) | 1.60 (0.87–2.05) | 1.46 (0.95–1.81) | NS |
| Other biochemical parameters | |||
| Mg (mmol/L) | 0.85 (0.82–0.87) | 0.91 (0.88–0.93) | 0.001 |
| TAS (mmol/L) | 1.68 (1.62–1.73) | 1.79 (1.75–1.85) | <0.001 |
| Glucose (mmol/L) | 5.29 (5.08–5.82) | 5.21(4.84–5.59) | <0.041 |
| hs-CRP (mg/L) | 1.13 (0.62–2.11) | 1.14 (0.70–1.85) | NS |
| Reference Values of NCEP ATP III | Participants (%) | ||
|---|---|---|---|
| Overweight/Obese Women with CVD Risk Factors (n = 20) | |||
| Pre | Post | ||
| T-C | |||
| Desirable | <5.19 mmol/L | 10 | 20 |
| Higher borderline | 5.2–6.19 mmol/L | 45 | 50 |
| High | ≥6.2 mmol/L | 45 | 30 |
| LDL-C | |||
| Optimal | <2.6 mmol/L | 0 | 0 |
| Near or above optimal | 2.6–3.3 mmol/L | 10 | 10 |
| Higher borderline | 3.4–4.1 mmol/L | 50 | 60 |
| High | 4.2–4.9 mmol/L | 15 | 25 |
| Very high | >4.9 mmol/L | 25 | 5 |
| HDL-C | |||
| High | ≥1.55 mmol/L | 30 | 50 |
| Higher borderline | 1.04–1.54 mmol/L | 50 | 45 |
| Low | <1.03 mmol/L | 20 | 5 |
| TG | |||
| Optimal | <1.7 mmol/L | 60 | 65 |
| Higher borderline | 1.70–2.25 mmol/L | 30 | 25 |
| High | 2.26–5.64 mmol/L | 10 | 10 |
| Very high | ≥5.65 mmol/L | 0 | 0 |
| Parameters | Overweight/Obese Women with Phenotype B (n = 6) | ||
|---|---|---|---|
| Pre | Post | p-Value | |
| T-C (mmol/L) | 6.41 ± 1.35 | 5.89 ± 0.56 | NS |
| LDL-C (mmol/L) | 4.32 ± 1.10 | 3.94 ± 0.43 | NS |
| HDL-C (mmol/L) | 1.24 ± 0.26 | 1.54 ± 0.26 | 0.002 |
| LDL/HDL (mmol/L) | 3.61 ± 1.14 | 2.61 ± 0.52 | 0.032 |
| TG (mmol/L) | 1.51 ± 0.83 | 1.31 ± 0.57 | NS |
| VLDL (mmol/L) | 1.45 ± 0.49 | 1.18 ± 0.15 | NS |
| IDL1 (mmol/L) | 0.74 ± 0.22 | 0.55 ± 0.08 | NS |
| IDL2 (mmol/L) | 0.60 ± 0.21 | 0.59 ± 0.21 | NS |
| IDL3 (mmol/L) | 0.59 ± 0.23 | 0.75 ± 0.18 | 0.029 |
| LDL1 (mmol/L) | 0.95 ± 0.23 | 1.06 ± 0.27 | NS |
| LDL2 (mmol/L) | 1.00 ± 0.32 | 0.72 ± 0.18 | 0.012 |
| LDL3-7 (mmol/L) | 0.45 ± 0.19 | 0.09 ± 0.07 | 0.003 |
| hs-CRP (mg/L) | 1.21 ± 1.23 | 1.26 ± 1.01 | NS |
| TAS (mmol/L) | 1.72 ± 0.10 | 1.88 ± 0.13 | 0.005 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Habanova, M.; Holovicova, M.; Scepankova, H.; Lorkova, M.; Gazo, J.; Gazarova, M.; Pinto, C.A.; Saraiva, J.A.; Estevinho, L.M. Modulation of Lipid Profile and Lipoprotein Subfractions in Overweight/Obese Women at Risk of Cardiovascular Diseases through the Consumption of Apple/Berry Juice. Antioxidants 2022, 11, 2239. https://doi.org/10.3390/antiox11112239
Habanova M, Holovicova M, Scepankova H, Lorkova M, Gazo J, Gazarova M, Pinto CA, Saraiva JA, Estevinho LM. Modulation of Lipid Profile and Lipoprotein Subfractions in Overweight/Obese Women at Risk of Cardiovascular Diseases through the Consumption of Apple/Berry Juice. Antioxidants. 2022; 11(11):2239. https://doi.org/10.3390/antiox11112239
Chicago/Turabian StyleHabanova, Marta, Maria Holovicova, Hana Scepankova, Marta Lorkova, Jan Gazo, Martina Gazarova, Carlos A. Pinto, Jorge A. Saraiva, and Leticia M. Estevinho. 2022. "Modulation of Lipid Profile and Lipoprotein Subfractions in Overweight/Obese Women at Risk of Cardiovascular Diseases through the Consumption of Apple/Berry Juice" Antioxidants 11, no. 11: 2239. https://doi.org/10.3390/antiox11112239
APA StyleHabanova, M., Holovicova, M., Scepankova, H., Lorkova, M., Gazo, J., Gazarova, M., Pinto, C. A., Saraiva, J. A., & Estevinho, L. M. (2022). Modulation of Lipid Profile and Lipoprotein Subfractions in Overweight/Obese Women at Risk of Cardiovascular Diseases through the Consumption of Apple/Berry Juice. Antioxidants, 11(11), 2239. https://doi.org/10.3390/antiox11112239






