Preclinical Intracranial Aneurysm Models: A Systematic Review
Abstract
1. Introduction
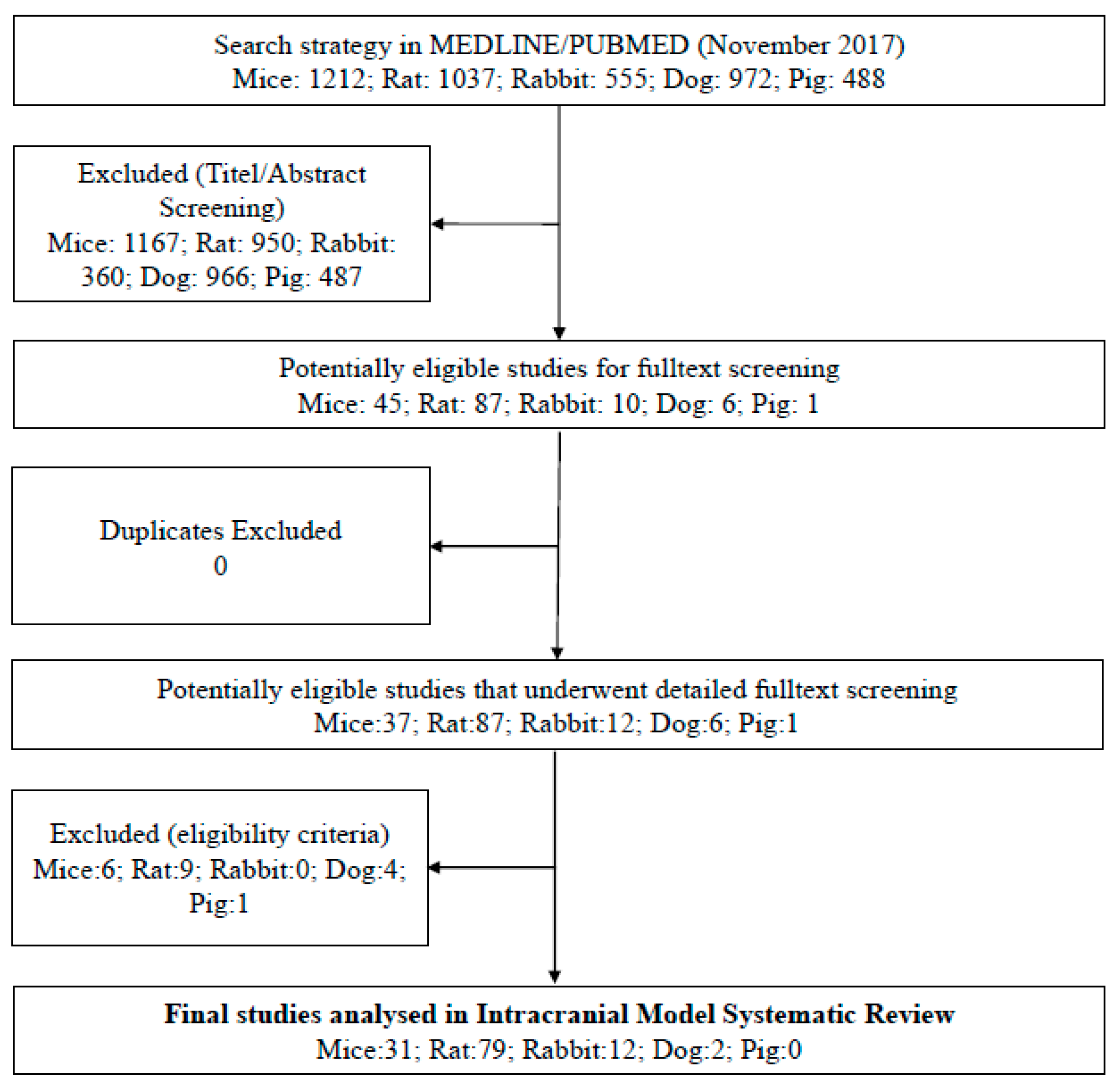
2. Materials and Methods
3. Results
4. Discussion
General Considerations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Etminan, N.; Rinkel, G.J. Unruptured intracranial aneurysms: Development, rupture and preventive management. Nat. Rev. Neurol. 2016, 12, 699–713. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, M.; Aoki, T. Molecular basis for intracranial aneurysm formation. Acta Neurochir. Suppl. 2015, 120, 13–15. [Google Scholar] [CrossRef] [PubMed]
- Vlak, M.H.; Algra, A.; Brandenburg, R.; Rinkel, G.J. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: A systematic review and meta-analysis. Lancet Neurol. 2011, 10, 626–636. [Google Scholar] [CrossRef]
- Brinjikji, W.; Pereira, V.M.; Khumtong, R.; Kostensky, A.; Tymianski, M.; Krings, T.; Radovanovich, I. PHASES and ELAPSS scores are associated with aneurysm growth: A study of 431 unruptured intracranial aneurysms. World Neurosurg. 2018, 114, e425–e432. [Google Scholar] [CrossRef] [PubMed]
- Diaz, O.; Rangel-Castilla, L. Endovascular treatment of intracranial aneurysms. Handb. Clin. Neurol. 2016, 136, 1303–1309. [Google Scholar] [CrossRef]
- Bouzeghrane, F.; Naggara, O.; Kallmes, D.F.; Berenstein, A.; Raymond, J.; International Consortium of Neuro Endovascular Centres. In vivo experimental intracranial aneurysm models: A systematic review. AJNR Am. J. Neuroradiol. 2010, 31, 418–423. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef]
- Alvarez, F.; Roda, J.M. Experimental model for induction of cerebral aneurysms in rats. J. Neurosurg. 1986, 65, 398–400. [Google Scholar] [CrossRef]
- Cai, J.; He, C.; Yuan, F.; Chen, L.; Ling, F. A novel haemodynamic cerebral aneurysm model of rats with normal blood pressure. J. Clin. Neurosci. 2012, 19, 135–138. [Google Scholar] [CrossRef]
- Coutard, M.; Huang, W.; Osborne-Pellegrin, M. Heritability of intracerebral hemorrhagic lesions and cerebral aneurysms in the rat. Stroke 2000, 31, 2678–2684. [Google Scholar] [CrossRef][Green Version]
- Hashimoto, N.; Handa, H.; Hazama, F. Experimentally induced cerebral aneurysms in rats. Surg. Neurol. 1978, 10, 3–8. [Google Scholar] [PubMed]
- Hashimoto, N.; Handa, H.; Hazama, F. Experimentally induced cerebral aneurysms in rats: Part II. Surg. Neurol. 1979, 11, 243–246. [Google Scholar] [PubMed]
- Hashimoto, N.; Handa, H.; Hazama, F. Experimentally induced cerebral aneurysms in rats: Part III. Pathology. Surg. Neurol. 1979, 11, 299–304. [Google Scholar] [PubMed]
- Hashimoto, N.; Handa, H.; Nagata, I.; Hazama, F. Experimentally induced cerebral aneurysms in rats: Part V. Relation of hemodynamics in the circle of Willis to formation of aneurysms. Surg. Neurol. 1980, 13, 41–45. [Google Scholar]
- Ishibashi, R.; Aoki, T.; Nishimura, M.; Miyamoto, S. Imidapril inhibits cerebral aneurysm formation in an angiotensin-converting enzyme-independent and matrix metalloproteinase-9-dependent manner. Neurosurgery 2012, 70, 722–730. [Google Scholar] [CrossRef]
- Kaufmann, T.J.; Marx, W.F.; Kallmes, D.F. A failure of matrix metalloproteinase inhibition in the prevention of rat intracranial aneurysm formation. Neuroradiology 2006, 48, 190–195. [Google Scholar] [CrossRef]
- Matsushita, N.; Kitazato, K.T.; Tada, Y.; Sumiyoshi, M.; Shimada, K.; Yagi, K.; Kanematsu, Y.; Satomi, J.; Nagahiro, S. Increase in body Na+/water ratio is associated with cerebral aneurysm formation in oophorectomized rats. Hypertension 2012, 60, 1309–1315. [Google Scholar] [CrossRef][Green Version]
- Suzuki, S.; Robertson, J.T.; White, R.P.; Stadlan, E.M.; Popoff, N. Experimental intracranial aneurysms in rats. A gross and microscopic study. J. Neurosurg. 1980, 52, 494–500. [Google Scholar] [CrossRef]
- Roda, J.M.; Alvarez, F.; Garcia-Villalon, A.L.; Ruiz, M.R.; Gutierrez, M.; Garcia Blazquez, M. An increment in unilateral carotid blood flow produces cerebral aneurysms in rats. Acta Neurochir. Suppl. (Wien) 1988, 43, 189–192. [Google Scholar]
- Xu, Y.; Tian, Y.; Wei, H.J.; Chen, J.; Dong, J.F.; Zacharek, A.; Zhang, J.N. Erythropoietin increases circulating endothelial progenitor cells and reduces the formation and progression of cerebral aneurysm in rats. Neuroscience 2011, 181, 292–299. [Google Scholar] [CrossRef]
- Xu, Y.; Tian, Y.; Wei, H.J.; Dong, J.F.; Zhang, J.N. Methionine diet-induced hyperhomocysteinemia accelerates cerebral aneurysm formation in rats. Neurosci. Lett. 2011, 494, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Abruzzo, T.; Kendler, A.; Apkarian, R.; Workman, M.; Khoury, J.C.; Cloft, H.J. Cerebral aneurysm formation in nitric oxide synthase-3 knockout mice. Curr. Neurovasc. Res. 2007, 4, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Dai, D.; Ding, Y.H.; Kadirvel, R.; Rad, A.E.; Lewis, D.A.; Kallmes, D.F. Lack of aneurysm formation after carotid artery ligation in rabbits: A polymer MICROFIL(R) study. Neuroradiology 2013, 55, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Hoi, Y.; Swartz, D.D.; Kolega, J.; Siddiqui, A.; Meng, H. Nascent aneurysm formation at the basilar terminus induced by hemodynamics. Stroke 2008, 39, 2085–2090. [Google Scholar] [CrossRef]
- Tutino, V.M.; Liaw, N.; Spernyak, J.A.; Ionita, C.N.; Siddiqui, A.H.; Kolega, J.; Meng, H. Assessment of vascular geometry for bilateral carotid artery ligation to induce early basilar terminus aneurysmal remodeling in rats. Curr. Neurovasc. Res. 2016, 13, 82–92. [Google Scholar] [CrossRef] [PubMed]
- Dolan, J.M.; Meng, H.; Sim, F.J.; Kolega, J. Differential gene expression by endothelial cells under positive and negative streamwise gradients of high wall shear stress. Am. J. Physiol. Cell Physiol. 2013, 305, C854–C866. [Google Scholar] [CrossRef]
- Kolega, J.; Gao, L.; Mandelbaum, M.; Mocco, J.; Siddiqui, A.H.; Natarajan, S.K.; Meng, H. Cellular and molecular responses of the basilar terminus to hemodynamics during intracranial aneurysm initiation in a rabbit model. J. Vasc. Res. 2011, 48, 429–442. [Google Scholar] [CrossRef]
- Li, M.H.; Li, P.G.; Huang, Q.L.; Ling, J. Endothelial injury preceding intracranial aneurysm formation in rabbits. West Indian Med. J. 2014, 63, 167–171. [Google Scholar] [CrossRef]
- Liaw, N.; Fox, J.M.; Siddiqui, A.H.; Meng, H.; Kolega, J. Endothelial nitric oxide synthase and superoxide mediate hemodynamic initiation of intracranial aneurysms. PLoS ONE 2014, 9, e101721. [Google Scholar] [CrossRef]
- Mandelbaum, M.; Kolega, J.; Dolan, J.M.; Siddiqui, A.H.; Meng, H. A critical role for proinflammatory behavior of smooth muscle cells in hemodynamic initiation of intracranial aneurysm. PLoS ONE 2013, 8, e74357. [Google Scholar] [CrossRef]
- Metaxa, E.; Tremmel, M.; Natarajan, S.K.; Xiang, J.; Paluch, R.A.; Mandelbaum, M.; Siddiqui, A.H.; Kolega, J.; Mocco, J.; Meng, H. Characterization of critical hemodynamics contributing to aneurysmal remodeling at the basilar terminus in a rabbit model. Stroke 2010, 41, 1774–1782. [Google Scholar] [CrossRef] [PubMed]
- Tutino, V.M.; Mandelbaum, M.; Choi, H.; Pope, L.C.; Siddiqui, A.; Kolega, J.; Meng, H. Aneurysmal remodeling in the circle of Willis after carotid occlusion in an experimental model. J. Cereb. Blood Flow Metab. 2014, 34, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Tutino, V.M.; Mandelbaum, M.; Takahashi, A.; Pope, L.C.; Siddiqui, A.; Kolega, J.; Meng, H. Hypertension and estrogen deficiency augment aneurysmal remodeling in the rabbit circle of willis in response to carotid ligation. Anat. Rec. (Hoboken) 2015, 298, 1903–1910. [Google Scholar] [CrossRef]
- Aoki, T.; Kataoka, H.; Moriwaki, T.; Nozaki, K.; Hashimoto, N. Role of TIMP-1 and TIMP-2 in the progression of cerebral aneurysms. Stroke 2007, 38, 2337–2345. [Google Scholar] [CrossRef]
- Aoki, T.; Fukuda, M.; Nishimura, M.; Nozaki, K.; Narumiya, S. Critical role of TNF-alpha-TNFR1 signaling in intracranial aneurysm formation. Acta Neuropathol. Commun. 2014, 2, 34. [Google Scholar] [CrossRef]
- Coutard, M.; Osborne-Pellegrin, M. Genetic susceptibility to experimental cerebral aneurysm formation in the rat. Stroke 1997, 28, 1035–1041. [Google Scholar] [CrossRef]
- Fukuda, M.; Aoki, T.; Manabe, T.; Maekawa, A.; Shirakawa, T.; Kataoka, H.; Takagi, Y.; Miyamoto, S.; Narumiya, S. Exacerbation of intracranial aneurysm and aortic dissection in hypertensive rat treated with the prostaglandin F-receptor antagonist AS604872. J. Pharmacol. Sci. 2014, 126, 230–242. [Google Scholar] [CrossRef]
- Ikedo, T.; Minami, M.; Kataoka, H.; Hayashi, K.; Nagata, M.; Fujikawa, R.; Higuchi, S.; Yasui, M.; Aoki, T.; Fukuda, M.; et al. Dipeptidyl peptidase-4 inhibitor anagliptin prevents intracranial aneurysm growth by suppressing macrophage infiltration and activation. J. Am. Heart Assoc. 2017, 6. [Google Scholar] [CrossRef]
- Miyata, H.; Koseki, H.; Takizawa, K.; Kasuya, H.; Nozaki, K.; Narumiya, S.; Aoki, T. T cell function is dispensable for intracranial aneurysm formation and progression. PLoS ONE 2017, 12, e0175421. [Google Scholar] [CrossRef]
- Yamamoto, R.; Aoki, T.; Koseki, H.; Fukuda, M.; Hirose, J.; Tsuji, K.; Takizawa, K.; Nakamura, S.; Miyata, H.; Hamakawa, N.; et al. A sphingosine-1-phosphate receptor type 1 agonist, ASP4058, suppresses intracranial aneurysm through promoting endothelial integrity and blocking macrophage transmigration. Br. J. Pharmacol. 2017, 174, 2085–2101. [Google Scholar] [CrossRef]
- Moriwaki, T.; Takagi, Y.; Sadamasa, N.; Aoki, T.; Nozaki, K.; Hashimoto, N. Impaired progression of cerebral aneurysms in interleukin-1beta-deficient mice. Stroke 2006, 37, 900–905. [Google Scholar] [CrossRef] [PubMed]
- Aoki, T.; Kataoka, H.; Morimoto, M.; Nozaki, K.; Hashimoto, N. Macrophage-derived matrix metalloproteinase-2 and -9 promote the progression of cerebral aneurysms in rats. Stroke 2007, 38, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Aoki, T.; Kataoka, H.; Shimamura, M.; Nakagami, H.; Wakayama, K.; Moriwaki, T.; Ishibashi, R.; Nozaki, K.; Morishita, R.; Hashimoto, N. NF-kappaB is a key mediator of cerebral aneurysm formation. Circulation 2007, 116, 2830–2840. [Google Scholar] [CrossRef]
- Aoki, T.; Kataoka, H.; Ishibashi, R.; Nozaki, K.; Hashimoto, N. Simvastatin suppresses the progression of experimentally induced cerebral aneurysms in rats. Stroke 2008, 39, 1276–1285. [Google Scholar] [CrossRef]
- Aoki, T.; Kataoka, H.; Ishibashi, R.; Nozaki, K.; Hashimoto, N. Gene expression profile of the intima and media of experimentally induced cerebral aneurysms in rats by laser-microdissection and microarray techniques. Int. J. Mol. Med. 2008, 22, 595–603. [Google Scholar]
- Aoki, T.; Kataoka, H.; Ishibashi, R.; Nozaki, K.; Hashimoto, N. Cathepsin B, K, and S are expressed in cerebral aneurysms and promote the progression of cerebral aneurysms. Stroke 2008, 39, 2603–2610. [Google Scholar] [CrossRef]
- Aoki, T.; Moriwaki, T.; Takagi, Y.; Kataoka, H.; Yang, J.; Nozaki, K.; Hashimoto, N. The efficacy of apolipoprotein E deficiency in cerebral aneurysm formation. Int. J. Mol. Med. 2008, 21, 453–459. [Google Scholar] [CrossRef][Green Version]
- Aoki, T.; Kataoka, H.; Ishibashi, R.; Nakagami, H.; Nozaki, K.; Morishita, R.; Hashimoto, N. Pitavastatin suppresses formation and progression of cerebral aneurysms through inhibition of the nuclear factor kappaB pathway. Neurosurgery 2009, 64, 357–365. [Google Scholar] [CrossRef]
- Aoki, T.; Kataoka, H.; Nishimura, M.; Ishibashi, R.; Morishita, R.; Miyamoto, S. Ets-1 promotes the progression of cerebral aneurysm by inducing the expression of MCP-1 in vascular smooth muscle cells. Gene Ther. 2010, 17, 1117–1123. [Google Scholar] [CrossRef]
- Aoki, T.; Nishimura, M.; Ishibashi, R.; Kataoka, H.; Takagi, Y.; Hashimoto, N. Toll-like receptor 4 expression during cerebral aneurysm formation. Laboratory investigation. J. Neurosurg. 2010, 113, 851–858. [Google Scholar] [CrossRef]
- Aoki, T.; Nishimura, M.; Kataoka, H.; Ishibashi, R.; Nozaki, K.; Miyamoto, S. Complementary inhibition of cerebral aneurysm formation by eNOS and nNOS. Lab. Investig. 2011, 91, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Aoki, T.; Kataoka, H.; Nishimura, M.; Ishibashi, R.; Morishita, R.; Miyamoto, S. Regression of intracranial aneurysms by simultaneous inhibition of nuclear factor-kappaB and Ets with chimeric decoy oligodeoxynucleotide treatment. Neurosurgery 2012, 70, 1534–1543. [Google Scholar] [CrossRef] [PubMed]
- Aoki, T.; Frosen, J.; Fukuda, M.; Bando, K.; Shioi, G.; Tsuji, K.; Ollikainen, E.; Nozaki, K.; Laakkonen, J.; Narumiya, S. Prostaglandin E2-EP2-NF-kappaB signaling in macrophages as a potential therapeutic target for intracranial aneurysms. Sci. Signal. 2017, 10. [Google Scholar] [CrossRef]
- Aoki, T.; Saito, M.; Koseki, H.; Tsuji, K.; Tsuji, A.; Murata, K.; Kasuya, H.; Morita, A.; Narumiya, S.; Nozaki, K.; et al. Macrophage imaging of cerebral aneurysms with ferumoxytol: An exploratory study in an animal model and in patients. J. Stroke Cerebrovasc. Dis. 2017, 26, 2055–2064. [Google Scholar] [CrossRef] [PubMed]
- Eldawoody, H.; Shimizu, H.; Kimura, N.; Saito, A.; Nakayama, T.; Takahashi, A.; Tominaga, T. Simplified experimental cerebral aneurysm model in rats: Comprehensive evaluation of induced aneurysms and arterial changes in the circle of Willis. Brain Res. 2009, 1300, 159–168. [Google Scholar] [CrossRef]
- Futami, K.; Yamashita, J.; Tachibana, O.; Higashi, S.; Ikeda, K.; Yamashima, T. Immunohistochemical alterations of fibronectin during the formation and proliferative repair of experimental cerebral aneurysms in rats. Stroke 1995, 26, 1659–1664. [Google Scholar] [CrossRef] [PubMed]
- Futami, K.; Yamashita, J.; Tachibana, O.; Kida, S.; Higashi, S.; Ikeda, K.; Yamashima, T. Basic fibroblast growth factor may repair experimental cerebral aneurysms in rats. Stroke 1995, 26, 1649–1654. [Google Scholar] [CrossRef]
- Futami, K.; Yamashita, J.; Higashi, S. Do cerebral aneurysms originate at the site of medial defects? Microscopic examinations of experimental aneurysms at the fenestration of the anterior cerebral artery in rats. Surg. Neurol. 1998, 50, 141–146. [Google Scholar] [CrossRef]
- Guo, D.; Wang, Y.W.; Ma, J.; Yan, L.; Li, T.F.; Han, X.W.; Shui, S.F. Study on the role of Cathepsin B and JNK signaling pathway in the development of cerebral aneurysm. Asian Pac. J. Trop. Med. 2016, 9, 499–502. [Google Scholar] [CrossRef]
- Hazama, F.; Kataoka, H.; Yamada, E.; Kayembe, K.; Hashimoto, N.; Kojima, M.; Kim, C. Early changes of experimentally induced cerebral aneurysms in rats. Light-microscopic study. Am. J. Pathol. 1986, 124, 399–404. [Google Scholar]
- Ishibashi, R.; Aoki, T.; Nishimura, M.; Hashimoto, N.; Miyamoto, S. Contribution of mast cells to cerebral aneurysm formation. Curr. Neurovasc. Res. 2010, 7, 113–124. [Google Scholar] [CrossRef] [PubMed]
- Jamous, M.A.; Nagahiro, S.; Kitazato, K.T.; Satoh, K.; Satomi, J. Vascular corrosion casts mirroring early morphological changes that lead to the formation of saccular cerebral aneurysm: An experimental study in rats. J. Neurosurg. 2005, 102, 532–535. [Google Scholar] [CrossRef] [PubMed]
- Jamous, M.A.; Nagahiro, S.; Kitazato, K.T.; Satomi, J.; Satoh, K. Role of estrogen deficiency in the formation and progression of cerebral aneurysms. Part I: Experimental study of the effect of oophorectomy in rats. J. Neurosurg. 2005, 103, 1046–1051. [Google Scholar] [CrossRef]
- Jamous, M.A.; Nagahiro, S.; Kitazato, K.T.; Tamura, T.; Kuwayama, K.; Satoh, K. Role of estrogen deficiency in the formation and progression of cerebral aneurysms. Part II: Experimental study of the effects of hormone replacement therapy in rats. J. Neurosurg. 2005, 103, 1052–1057. [Google Scholar] [CrossRef]
- Jamous, M.A.; Nagahiro, S.; Kitazato, K.T.; Tamura, T.; Aziz, H.A.; Shono, M.; Satoh, K. Endothelial injury and inflammatory response induced by hemodynamic changes preceding intracranial aneurysm formation: Experimental study in rats. J. Neurosurg. 2007, 107, 405–411. [Google Scholar] [CrossRef]
- Kang, Y.; Hashimoto, N.; Kikuchi, H.; Yamazoe, N.; Hazama, F. Effects of blood coagulation factor XIII on the development of experimental cerebral aneurysms in rats. J. Neurosurg. 1990, 73, 242–247. [Google Scholar] [CrossRef]
- Kim, C.; Kikuchi, H.; Hashimoto, N.; Kojima, M.; Kang, Y.; Hazama, F. Involvement of internal elastic lamina in development of induced cerebral aneurysms in rats. Stroke 1988, 19, 507–511. [Google Scholar] [CrossRef]
- Kim, C.; Cervos-Navarro, J.; Kikuchi, H.; Hashimoto, N.; Hazama, F. Degenerative changes in the internal elastic lamina relating to the development of saccular cerebral aneurysms in rats. Acta Neurochir. (Wien) 1993, 121, 76–81. [Google Scholar] [CrossRef]
- Kimura, N.; Shimizu, H.; Eldawoody, H.; Nakayama, T.; Saito, A.; Tominaga, T.; Takahashi, A. Effect of olmesartan and pravastatin on experimental cerebral aneurysms in rats. Brain Res. 2010, 1322, 144–152. [Google Scholar] [CrossRef]
- Kojima, M.; Handa, H.; Hashimoto, N.; Kim, C.; Hazama, F. Early changes of experimentally induced cerebral aneurysms in rats: Scanning electron microscopic study. Stroke 1986, 17, 835–841. [Google Scholar] [CrossRef]
- Kondo, S.; Hashimoto, N.; Kikuchi, H.; Hazama, F.; Nagata, I.; Kataoka, H. Cerebral aneurysms arising at nonbranching sites. An experimental Study. Stroke 1997, 28, 398–403. [Google Scholar] [CrossRef] [PubMed]
- Kondo, S.; Hashimoto, N.; Kikuchi, H.; Hazama, F.; Nagata, I.; Kataoka, H. Apoptosis of medial smooth muscle cells in the development of saccular cerebral aneurysms in rats. Stroke 1998, 29, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Korai, M.; Kitazato, K.T.; Tada, Y.; Miyamoto, T.; Shimada, K.; Matsushita, N.; Kanematsu, Y.; Satomi, J.; Hashimoto, T.; Nagahiro, S. Hyperhomocysteinemia induced by excessive methionine intake promotes rupture of cerebral aneurysms in ovariectomized rats. J. Neuroinflamm. 2016, 13, 165. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Tian, Y.; Huang, X.; Zhang, Y.; Wang, D.; Wei, H.; Dong, J.; Jiang, R.; Zhang, J. Intravenous transfusion of endothelial colony-forming cells attenuates vascular degeneration after cerebral aneurysm induction. Brain Res. 2014, 1593, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Wang, D.; Tian, Y.; Wei, H.; Zhou, Z.; Liu, L.; Wang, D.; Dong, J.F.; Jiang, R.; Zhang, J. Aspirin inhibits degenerative changes of aneurysmal wall in a rat model. Neurochem. Res. 2015, 40, 1537–1545. [Google Scholar] [CrossRef]
- Maekawa, H.; Tada, Y.; Yagi, K.; Miyamoto, T.; Kitazato, K.T.; Korai, M.; Satomi, J.; Hashimoto, T.; Nagahiro, S. Bazedoxifene, a selective estrogen receptor modulator, reduces cerebral aneurysm rupture in Ovariectomized rats. J. Neuroinflamm. 2017, 14, 197. [Google Scholar] [CrossRef]
- Miyamoto, T.; Kung, D.K.; Kitazato, K.T.; Yagi, K.; Shimada, K.; Tada, Y.; Korai, M.; Kurashiki, Y.; Kinouchi, T.; Kanematsu, Y.; et al. Site-specific elevation of interleukin-1beta and matrix metalloproteinase-9 in the Willis circle by hemodynamic changes is associated with rupture in a novel rat cerebral aneurysm model. J. Cereb. Blood Flow Metab. 2017, 37, 2795–2805. [Google Scholar] [CrossRef]
- Nagata, I.; Handa, H.; Hashimoto, N. Experimentally induced cerebral aneurysms in rats: Part IV—Cerebral angiography. Surg. Neurol. 1979, 12, 419–424. [Google Scholar]
- Nagata, I.; Handa, H.; Hashimoto, N.; Hazama, F. Experimentally induced cerebral aneurysms in rats: Part VI. Hypertension. Surg. Neurol. 1980, 14, 477–479. [Google Scholar]
- Nagata, I.; Handa, H.; Hasimoto, N.; Hazama, F. Experimentally induced cerebral aneurysms in rats: VII. Scanning electron microscope study. Surg. Neurol. 1981, 16, 291–296. [Google Scholar] [CrossRef]
- Nakatani, H.; Hashimoto, N.; Kikuchi, H.; Yamaguchi, S.; Niimi, H. In vivo flow visualization of induced saccular cerebral aneurysms in rats. Acta Neurochir. (Wien) 1993, 122, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Sadamasa, N.; Nozaki, K.; Takagi, Y.; Moriwaki, T.; Kawanabe, Y.; Ishikawa, M.; Hashimoto, N. Cerebral aneurysm progression suppressed by blockage of endothelin B receptor. J. Neurosurg. 2007, 106, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Sadamasa, N.; Nozaki, K.; Kita-Matsuo, H.; Saito, S.; Moriwaki, T.; Aoki, T.; Kawarazaki, S.; Kataoka, H.; Takagi, Y.; Ishikawa, M.; et al. Gene expression during the development of experimentally induced cerebral aneurysms. J. Vasc. Res. 2008, 45, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Tada, Y.; Yagi, K.; Kitazato, K.T.; Tamura, T.; Kinouchi, T.; Shimada, K.; Matsushita, N.; Nakajima, N.; Satomi, J.; Kageji, T.; et al. Reduction of endothelial tight junction proteins is related to cerebral aneurysm formation in rats. J. Hypertens. 2010, 28, 1883–1891. [Google Scholar] [CrossRef]
- Tada, Y.; Kitazato, K.T.; Yagi, K.; Shimada, K.; Matsushita, N.; Kinouchi, T.; Kanematsu, Y.; Satomi, J.; Kageji, T.; Nagahiro, S. Statins promote the growth of experimentally induced cerebral aneurysms in estrogen-deficient rats. Stroke 2011, 42, 2286–2293. [Google Scholar] [CrossRef]
- Tamura, T.; Jamous, M.A.; Kitazato, K.T.; Yagi, K.; Tada, Y.; Uno, M.; Nagahiro, S. Endothelial damage due to impaired nitric oxide bioavailability triggers cerebral aneurysm formation in female rats. J. Hypertens. 2009, 27, 1284–1292. [Google Scholar] [CrossRef]
- Yagi, K.; Tada, Y.; Kitazato, K.T.; Tamura, T.; Satomi, J.; Nagahiro, S. Ibudilast inhibits cerebral aneurysms by down-regulating inflammation-related molecules in the vascular wall of rats. Neurosurgery 2010, 66, 551–559. [Google Scholar] [CrossRef]
- Yamazoe, N.; Hashimoto, N.; Kikuchi, H.; Hazama, F. Elastic skeleton of intracranial cerebral aneurysms in rats. Stroke 1990, 21, 1722–1726. [Google Scholar] [CrossRef]
- Yokoi, T.; Isono, T.; Saitoh, M.; Yoshimura, Y.; Nozaki, K. Suppression of cerebral aneurysm formation in rats by a tumor necrosis factor-alpha inhibitor. J. Neurosurg. 2014, 120, 1193–1200. [Google Scholar] [CrossRef]
- Wu, C.; Liu, Y.; He, M.; Zhu, L.; You, C. Single operation with simplified incisions to build an experimental cerebral aneurysm model by induced hemodynamic stress and estrogen deficiency in rats. Turk. Neurosurg. 2016, 26, 62–68. [Google Scholar] [CrossRef][Green Version]
- Zhou, D.; Bao, Y.D.; Du, Z.W.; Takeda, F.; Kanno, T. Experimental cerebral aneurysms in rats. Experimental method and effect of estradiol. Chin. Med. J. (Engl.) 1985, 98, 421–426. [Google Scholar] [PubMed]
- Sadamasa, N.; Nozaki, K.; Hashimoto, N. Disruption of gene for inducible nitric oxide synthase reduces progression of cerebral aneurysms. Stroke 2003, 34, 2980–2984. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Lin, X.; He, C.; Yang, G.Y.; Ling, F. Study of cerebral aneurysms in a modified rat model: From real-time imaging to histological analysis. J. Clin. Neurosci. 2015, 22, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Chalouhi, N.; Starke, R.M.; Correa, T.; Jabbour, P.M.; Zanaty, M.; Brown, R.D., Jr.; Torner, J.C.; Hasan, D.M. Differential sex response to aspirin in decreasing aneurysm rupture in humans and mice. Hypertension 2016, 68, 411–417. [Google Scholar] [CrossRef]
- Chu, Y.; Wilson, K.; Gu, H.; Wegman-Points, L.; Dooley, S.A.; Pierce, G.L.; Cheng, G.; Pena Silva, R.A.; Heistad, D.D.; Hasan, D. Myeloperoxidase is increased in human cerebral aneurysms and increases formation and rupture of cerebral aneurysms in mice. Stroke 2015, 46, 1651–1656. [Google Scholar] [CrossRef]
- Hasan, D.M.; Starke, R.M.; Gu, H.; Wilson, K.; Chu, Y.; Chalouhi, N.; Heistad, D.D.; Faraci, F.M.; Sigmund, C.D. Smooth muscle peroxisome proliferator-activated receptor gamma plays a critical role in formation and rupture of cerebral aneurysms in mice in vivo. Hypertension 2015, 66, 211–220. [Google Scholar] [CrossRef]
- Kanematsu, Y.; Kanematsu, M.; Kurihara, C.; Tada, Y.; Tsou, T.L.; van Rooijen, N.; Lawton, M.T.; Young, W.L.; Liang, E.I.; Nuki, Y.; et al. Critical roles of macrophages in the formation of intracranial aneurysm. Stroke 2011, 42, 173–178. [Google Scholar] [CrossRef]
- Kuwabara, A.; Liu, J.; Kamio, Y.; Liu, A.; Lawton, M.T.; Lee, J.W.; Hashimoto, T. Protective effect of mesenchymal stem cells against the development of intracranial aneurysm rupture in mice. Neurosurgery 2017, 81, 1021–1028. [Google Scholar] [CrossRef]
- Labeyrie, P.E.; Goulay, R.; Martinez de Lizarrondo, S.; Hebert, M.; Gauberti, M.; Maubert, E.; Delaunay, B.; Gory, B.; Signorelli, F.; Turjman, F.; et al. Vascular tissue-type plasminogen activator promotes intracranial aneurysm formation. Stroke 2017, 48, 2574–2582. [Google Scholar] [CrossRef]
- Lee, J.A.; Marshman, L.A.; Moran, C.S.; Kuma, L.; Guazzo, E.P.; Anderson, D.S.; Golledge, J. A small animal model for early cerebral aneurysm pathology. J. Clin. Neurosci. 2016, 34, 259–263. [Google Scholar] [CrossRef]
- Liu, J.; Kuwabara, A.; Kamio, Y.; Hu, S.; Park, J.; Hashimoto, T.; Lee, J.W. Human mesenchymal stem cell-derived microvesicles prevent the rupture of intracranial aneurysm in part by suppression of mast cell activation via a pge2-dependent mechanism. Stem Cells 2016, 34, 2943–2955. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Zhao, J.; Zhou, Q.; Peng, Y.; Zhou, Y.; Jiang, Y. Primary cilia deficiency induces intracranial aneurysm. Shock 2018, 49, 604–611. [Google Scholar] [CrossRef] [PubMed]
- Makino, H.; Tada, Y.; Wada, K.; Liang, E.I.; Chang, M.; Mobashery, S.; Kanematsu, Y.; Kurihara, C.; Palova, E.; Kanematsu, M.; et al. Pharmacological stabilization of intracranial aneurysms in mice: A feasibility study. Stroke 2012, 43, 2450–2456. [Google Scholar] [CrossRef]
- Makino, H.; Hokamura, K.; Natsume, T.; Kimura, T.; Kamio, Y.; Magata, Y.; Namba, H.; Katoh, T.; Sato, S.; Hashimoto, T.; et al. Successful serial imaging of the mouse cerebral arteries using conventional 3-T magnetic resonance imaging. J. Cereb. Blood Flow Metab. 2015, 35, 1523–1527. [Google Scholar] [CrossRef]
- Nuki, Y.; Tsou, T.L.; Kurihara, C.; Kanematsu, M.; Kanematsu, Y.; Hashimoto, T. Elastase-induced intracranial aneurysms in hypertensive mice. Hypertension 2009, 54, 1337–1344. [Google Scholar] [CrossRef] [PubMed]
- Pena Silva, R.A.; Kung, D.K.; Mitchell, I.J.; Alenina, N.; Bader, M.; Santos, R.A.; Faraci, F.M.; Heistad, D.D.; Hasan, D.M. Angiotensin 1–7 reduces mortality and rupture of intracranial aneurysms in mice. Hypertension 2014, 64, 362–368. [Google Scholar] [CrossRef] [PubMed]
- Pena-Silva, R.A.; Chalouhi, N.; Wegman-Points, L.; Ali, M.; Mitchell, I.; Pierce, G.L.; Chu, Y.; Ballas, Z.K.; Heistad, D.; Hasan, D. Novel role for endogenous hepatocyte growth factor in the pathogenesis of intracranial aneurysms. Hypertension 2015, 65, 587–593. [Google Scholar] [CrossRef]
- Shimada, K.; Furukawa, H.; Wada, K.; Korai, M.; Wei, Y.; Tada, Y.; Kuwabara, A.; Shikata, F.; Kitazato, K.T.; Nagahiro, S.; et al. Protective role of peroxisome proliferator-activated receptor-gamma in the development of intracranial aneurysm rupture. Stroke 2015, 46, 1664–1672. [Google Scholar] [CrossRef]
- Shimada, K.; Furukawa, H.; Wada, K.; Wei, Y.; Tada, Y.; Kuwabara, A.; Shikata, F.; Kanematsu, Y.; Lawton, M.T.; Kitazato, K.T.; et al. Angiotensin-(1-7) protects against the development of aneurysmal subarachnoid hemorrhage in mice. J. Cereb. Blood Flow Metab. 2015, 35, 1163–1168. [Google Scholar] [CrossRef]
- Tada, Y.; Makino, H.; Furukawa, H.; Shimada, K.; Wada, K.; Liang, E.I.; Murakami, S.; Kudo, M.; Kung, D.K.; Hasan, D.M.; et al. Roles of estrogen in the formation of intracranial aneurysms in ovariectomized female mice. Neurosurgery 2014, 75, 690–695. [Google Scholar] [CrossRef]
- Tada, Y.; Wada, K.; Shimada, K.; Makino, H.; Liang, E.I.; Murakami, S.; Kudo, M.; Kitazato, K.T.; Nagahiro, S.; Hashimoto, T. Roles of hypertension in the rupture of intracranial aneurysms. Stroke 2014, 45, 579–586. [Google Scholar] [CrossRef] [PubMed]
- Tada, Y.; Wada, K.; Shimada, K.; Makino, H.; Liang, E.I.; Murakami, S.; Kudo, M.; Shikata, F.; Pena Silva, R.A.; Kitazato, K.T.; et al. Estrogen protects against intracranial aneurysm rupture in ovariectomized mice. Hypertension 2014, 63, 1339–1344. [Google Scholar] [CrossRef]
- Wada, K.; Makino, H.; Shimada, K.; Shikata, F.; Kuwabara, A.; Hashimoto, T. Translational research using a mouse model of intracranial aneurysm. Transl. Stroke Res. 2014, 5, 248–251. [Google Scholar] [CrossRef]
- Zhang, M.; Ren, Y.; Wang, Y.; Wang, R.; Zhou, Q.; Peng, Y.; Li, Q.; Yu, M.; Jiang, Y. Regulation of smooth muscle contractility by competing endogenous mRNAs in intracranial aneurysms. J. Neuropathol. Exp. Neurol. 2015, 74, 411–424. [Google Scholar] [CrossRef][Green Version]
- Dai, D.; Ding, Y.H.; Kadirvel, R.; Lewis, D.A.; Kallmes, D.F. Experience with microaneurysm formation at the basilar terminus in the rabbit elastase aneurysm model. AJNR Am. J. Neuroradiol. 2010, 31, 300–303. [Google Scholar] [CrossRef]
- Yasuda, H.; Kuroda, S.; Nanba, R.; Ishikawa, T.; Shinya, N.; Terasaka, S.; Iwasaki, Y.; Nagashima, K. A novel coating biomaterial for intracranial aneurysms: Effects and safety in extra- and intracranial carotid artery. Neuropathology 2005, 25, 66–76. [Google Scholar] [CrossRef]
- Hoh, B.L.; Hosaka, K.; Downes, D.P.; Nowicki, K.W.; Wilmer, E.N.; Velat, G.J.; Scott, E.W. Stromal cell-derived factor-1 promoted angiogenesis and inflammatory cell infiltration in aneurysm walls. J. Neurosurg. 2014, 120, 73–86. [Google Scholar] [CrossRef]
- Hosaka, K.; Downes, D.P.; Nowicki, K.W.; Hoh, B.L. Modified murine intracranial aneurysm model: Aneurysm formation and rupture by elastase and hypertension. J. Neurointerv. Surg. 2014, 6, 474–479. [Google Scholar] [CrossRef]
- Hosaka, K.; Rojas, K.; Fazal, H.Z.; Schneider, M.B.; Shores, J.; Federico, V.; McCord, M.; Lin, L.; Hoh, B. Monocyte chemotactic protein-1-interleukin-6-osteopontin pathway of intra-aneurysmal tissue healing. Stroke 2017, 48, 1052–1060. [Google Scholar] [CrossRef]
- Nowicki, K.W.; Hosaka, K.; Walch, F.J.; Scott, E.W.; Hoh, B.L. M1 macrophages are required for murine cerebral aneurysm formation. J. Neurointerv. Surg. 2018, 10, 93–97. [Google Scholar] [CrossRef]
- Lee, J.; Berry, C.L. Cerebral micro-aneurysm formation in the hypertensive rat. J. Pathol. 1978, 124, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Tada, Y.; Kitazato, K.T.; Tamura, T.; Yagi, K.; Shimada, K.; Kinouchi, T.; Satomi, J.; Nagahiro, S. Role of mineralocorticoid receptor on experimental cerebral aneurysms in rats. Hypertension 2009, 54, 552–557. [Google Scholar] [CrossRef] [PubMed]
- Jung, K.H.; Chu, K.; Lee, S.T.; Shin, Y.W.; Lee, K.J.; Park, D.K.; Yoo, J.S.; Kim, S.; Kim, M.; Lee, S.K.; et al. Experimental induction of cerebral aneurysms by developmental low copper diet. J. Neuropathol. Exp. Neurol. 2016, 75, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Bo, L.J.; Miao, Z.; Wang, Z.F.; Zhang, K.Z.; Gao, Z. A study on effect of curcumin on anticerebral aneurysm in the male albino rats. Brain Behav. 2017, 7, e00729. [Google Scholar] [CrossRef]
- Ebina, K.; Iwabuchi, T.; Suzuki, S. A clinico-experimental study on various wrapping materials of cerebral aneurysms. Acta Neurochir. (Wien) 1984, 72, 61–71. [Google Scholar] [CrossRef]
- Nishikawa, M.; Smith, R.D.; Yonekawa, Y. Experimental intracranial aneurysms. Surg. Neurol. 1977, 7, 241–244. [Google Scholar]
- Gopal, K.; Nagarajan, P.; Raj, T.A.; Jahan, P.; Ganapathy, H.S.; Mahesh Kumar, M.J. Effect of dietary beta carotene on cerebral aneurysm and subarachnoid haemorrhage in the brain apo E−/− mice. J. Thromb. Thrombolysis 2011, 32, 343–355. [Google Scholar] [CrossRef]
- CAMARADES. Collaborative Approach to Meta-Analysis and Review of Animal Data from Experimental Studies. Available online: http://www.dcn.ed.ac.uk/camarades/ (accessed on 1 August 2019).

| Category | Subcategory | References | |
|---|---|---|---|
| CCA ligation | Unilateral CCA ligation | Rat: Alvarez et al. 1986 [8], Cai et al. 2012 [9], Coutard et al. 2000 [10], Hahimoto et al. 1978 [11], 1979a [12], 1979b [13], 1980 [14], Ishibashi et al. 2012 [15], Kaufmann et al. 2006 [16], Matsushita et al. 2012 [17], Suzuki et al. 1980 [18], Roda et al. 1988 [19], Xu et al. 2011a [20], 2011b [21] | |
| Mouse: Abruzzo et al. 2007 [22] | |||
| Rabbit: Dai et al. 2013 [23], Gao et al. 2008 [24] | |||
| Bilateral CCA ligation | Rat: Tutino et al. 2016 [25] | ||
| Rabbit: Dolan et al. 2013 [26], Kolega et al. 2011 [27], Li et al. 2014 [28], Liaw et al. 2014 [29], Mandelbaum et al. 2013 [30], Metaxa et al. 2010 [31], Tutino et al. 2014 [32], 2015 [33] | |||
| CCA ligation and RA ligation | Unilateral CCA ligation | Unilateral RA ligation | Rat: Aoki 2007 [34], 2014 [35], Coutard et al. 1997 [36], Fukuda et al. 2014 [37], Ikedo et al. 2017 [38], Miyata et al. 2017 [39], Yamamoto et al. 2017 [40] |
| Mouse: Aoki et al. 2007 [34], 2017, Moriwaki et al. 2006 [41] | |||
| Rabbit: Gao et al. 2008 [24] | |||
| Bilateral RA ligation | Rat: Alvarez and Roda 1986 [8], Aoki et al. 2007a [42], 2007b [43], 2008a [44], 2008b [45], 2008c [46], 2008d [47], 2009 [48], 2010a [49], 2010b [50], 2011 [51], 2012 [52], 2017a [53], 2017b [54], Eldawoody et al. 2009 [55], Futami et al. 1995a [56], 1995b [57], 1998 [58], Guo et al. 2016 [59], Hazama et al. 1986 [60], Ishibashi et al. 2010 [61], Jamous et al. 2005a [62], 2005b [63], 2005c [64], 2007 [65], Kang et al. 1990 [66], Kim et al. 1988 [67], Kim et al. 1993 [68], Kimura et al. 2010 [69], Kojima et al. 1986 [70], Kondo et al. 1997 [71], 1998 [72], Korai et al. 2016 [73], Li et al. 2014 [74], 2015 [75], Maekawa et al. 2017 [76], Miyamoto et al. 2017 [77], Nagata et al. 1979 [78], 1980 [79], 1981 [80], Nakatani et al. 1993 [81], Sadamasa et al. 2007 [82], 2008 [83], Tada et al. 2010 [84], 2011 [85], Tamura et al. 2009 [86], Yagi et al. 2010 [87], Yamazoe et al. 1990 [88], Yokoi et al. 2014 [89], Wu et al. 2016 [90], Zhou et al. 1985 [91] | ||
| Mouse: Sadamasa et al. 2003 [92] | |||
| Elastase injection | Rat: Zhao et al. 2015 [93] | ||
| Mouse: Chalouhi et al. 2016 [94], Chu et al. 2015 [95], Hasan et al. 2015 [96], Kanematsu et al. 2011 [97], Kuwabara et al. 2017 [98], Labeyrie et al. 2017 [99], Lee et al. 2016 [100], Liu et al. 2016 [101], 2017 [102], Makino et al. 2012 [103], 2015 [104], Nuki et al. 2009 [105], Pena Silva et al. 2014 [106], 2015 [107], Shimada et al. 2015a [108], 2015b [109], Tada et al. 2014a [110], 2014b [111], 2014c [112], Wada et al. 2014 [113], Zhang et al. 2015 [114] | |||
| Rabbit: Dai et al. 2010 [115], Yasuda et al. 2005 [116] | |||
| Elastase injection and CCA ligation | Mouse: Hoh et al. 2014 [117], Hosaka et al. 2014 [118], 2017 [119], Nowicki et al. 2017 [120] | ||
| Other | Deoxycorticosterone/hypertension | Lee et al. 1978 [121] (rat) | |
| Eplerenone | Tada et al. 2009 [122] (rat) | ||
| Copper deficiency | Jung et al. 2016 [123] (rat) | ||
| CaCl2 | Bo et al. 2017 [124] (rat) | ||
| Coating of internal carotid artery | Ebina et al. 1984 [125] (dog) | ||
| Venous pouch or venous patch | Nishikawa et al. 1977 [126] (dog) | ||
| Species | Total No. of Studies Analyzed | CCA Ligation and RA Ligation | CCA Ligation Only | Elastase Only | Elastase and CCA Ligation | Other |
|---|---|---|---|---|---|---|
| Mice | 31 | 4 | 1 | 21 | 4 | - |
| Rats | 79 | 60 | 13 | 1 | - | 5 |
| Rabbits | 21 | - | 10 | 1 | 1 | - |
| Dogs | 2 | - | - | - | - | 2 |
| Overall | 133 | 64 | 24 | 22 | 5 | 6 |
| Species | CCA Ligation and RA Ligation | CCA Ligation Only | Elastase Only | Elastase and CCA Ligation | Other |
|---|---|---|---|---|---|
| Mice (31) | 3,4 (0,5–5) | 13 (0) | 0,53 (0,17–1) | 0,43 (0,1–0,75) | - |
| Rats (79) | 2,28 (0,17–12) | 2,49 (0,25–12) | 1,25 (0) | - | 1,83 (1–2,5) |
| Rabbits (12) | 3,0 | 2,59 (0,17–6) | 1,5 (1–2) | - | |
| Dogs (2) | - | - | - | - | 0,68 (0,35–1) |
| Overall | 2,38 (0,17–12) | 2,53 (0,17–13) | 0,65 (0,17–2) | 0,43 (0,1–0,75) | 1,37 (0,35–2,5) |
| Technique | Purpose | Number of Studies | Number of Species |
|---|---|---|---|
| RA ligation, unilateral | Hypertension | 12 | 3 |
| RA ligation, bilateral | Hypertension | 52 | 2 |
| High NaCl diet (1% or 8%) | Hypertension | 68 | 3 |
| Deoxycorticosterone administration | Hypertension | 15 | 3 |
| Angiotensin II | Hypertension | 13 | 1 |
| β-aminopropionitrile administration (0.12%) | Weakening of vessel walls | 36 | 2 |
| Estrogen depletion/oophorectomy | Weakening of vessel walls | 12 | 3 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strange, F.; Grüter, B.E.; Fandino, J.; Marbacher, S. Preclinical Intracranial Aneurysm Models: A Systematic Review. Brain Sci. 2020, 10, 134. https://doi.org/10.3390/brainsci10030134
Strange F, Grüter BE, Fandino J, Marbacher S. Preclinical Intracranial Aneurysm Models: A Systematic Review. Brain Sciences. 2020; 10(3):134. https://doi.org/10.3390/brainsci10030134
Chicago/Turabian StyleStrange, Fabio, Basil E Grüter, Javier Fandino, and Serge Marbacher. 2020. "Preclinical Intracranial Aneurysm Models: A Systematic Review" Brain Sciences 10, no. 3: 134. https://doi.org/10.3390/brainsci10030134
APA StyleStrange, F., Grüter, B. E., Fandino, J., & Marbacher, S. (2020). Preclinical Intracranial Aneurysm Models: A Systematic Review. Brain Sciences, 10(3), 134. https://doi.org/10.3390/brainsci10030134





