Digital Analysis Using 3D Intraoral Scanner on Gingival Contour Changes Following the Roll Flap Technique
Abstract
1. Introduction
2. Materials and Methods
2.1. Case Selection and Description
- Inclusion criteria
- -
- Patients with general good health;
- -
- Patients who received implant placement in posterior maxilla area;
- -
- Patients who received single implant placement.
- Exclusion criteria
- -
- Patients who received implant placement with guided bone regeneration.
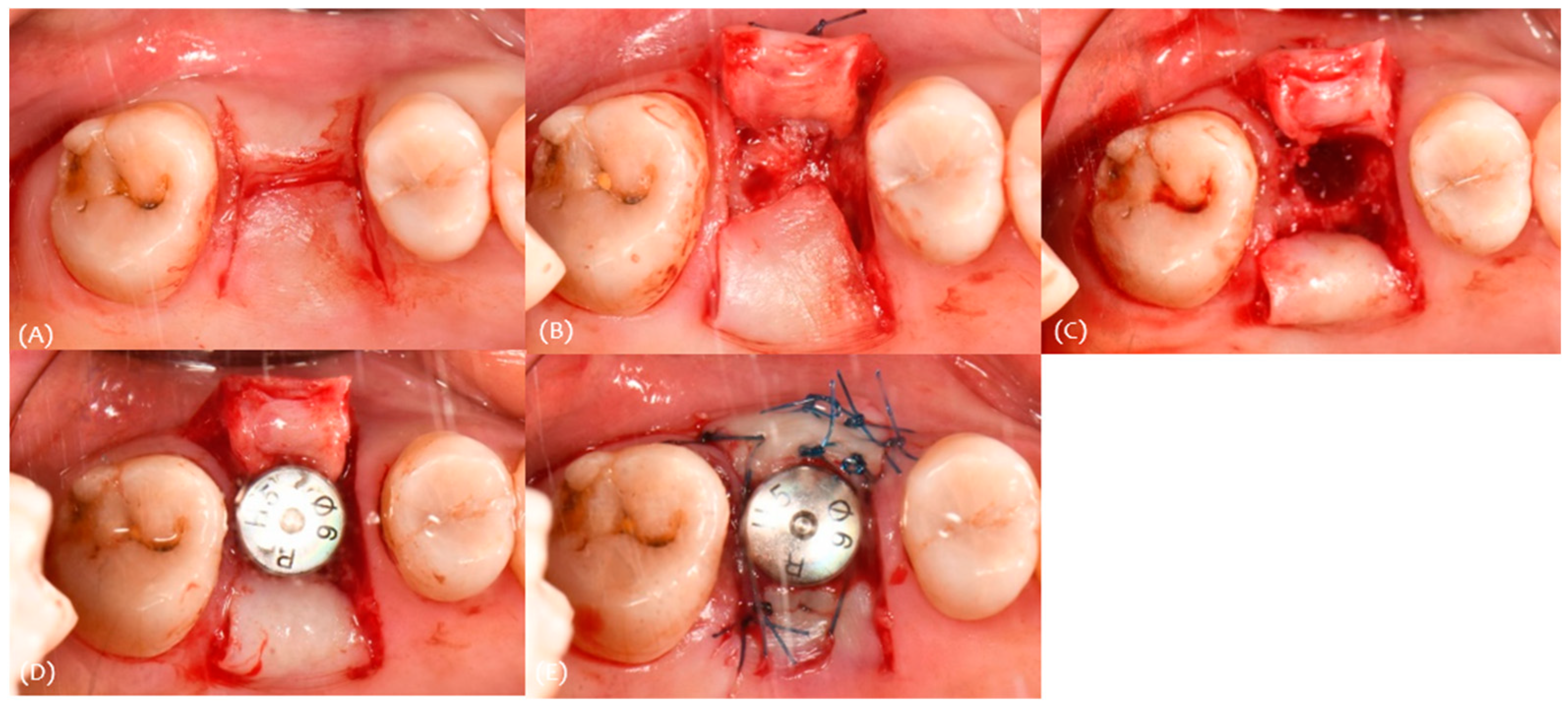
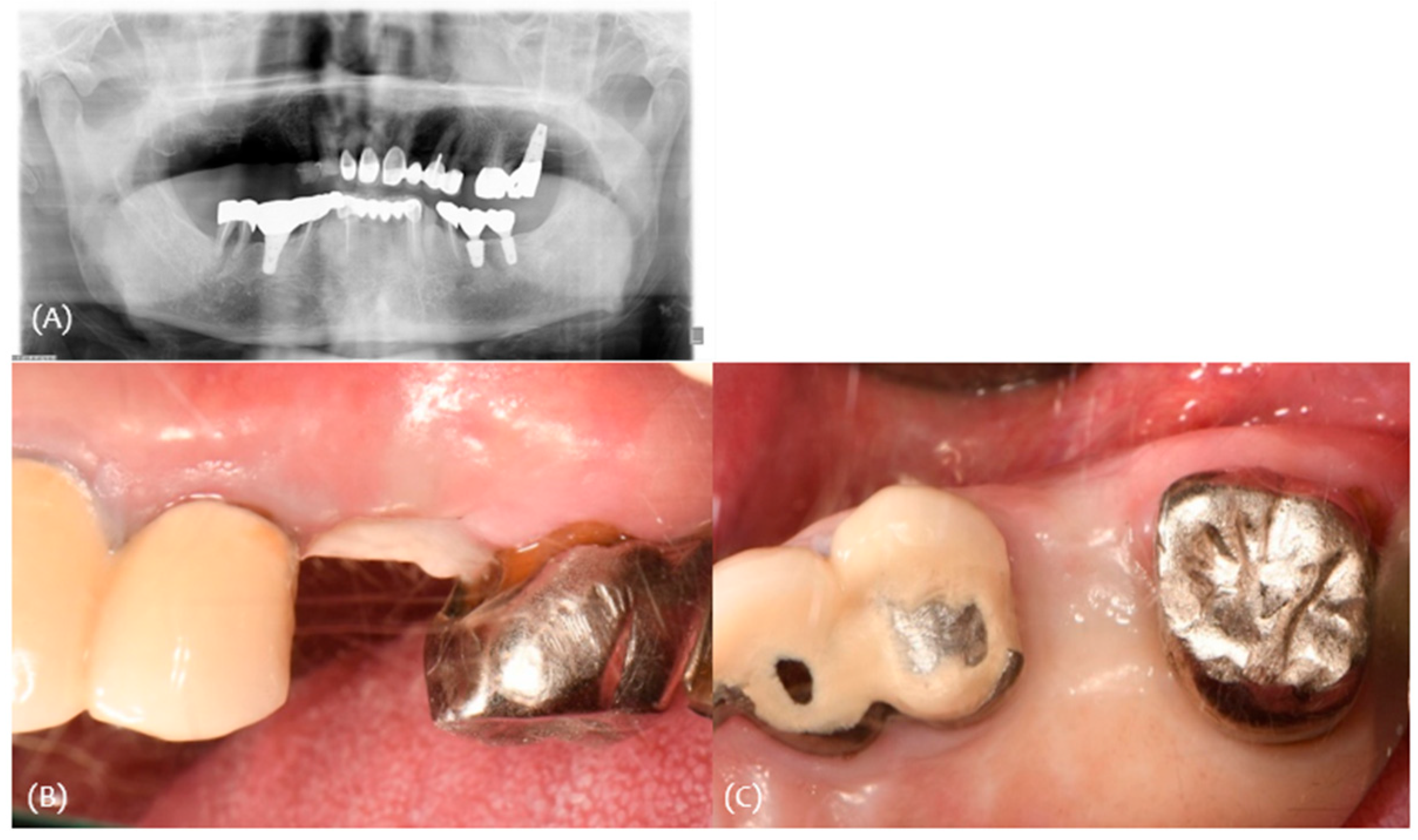
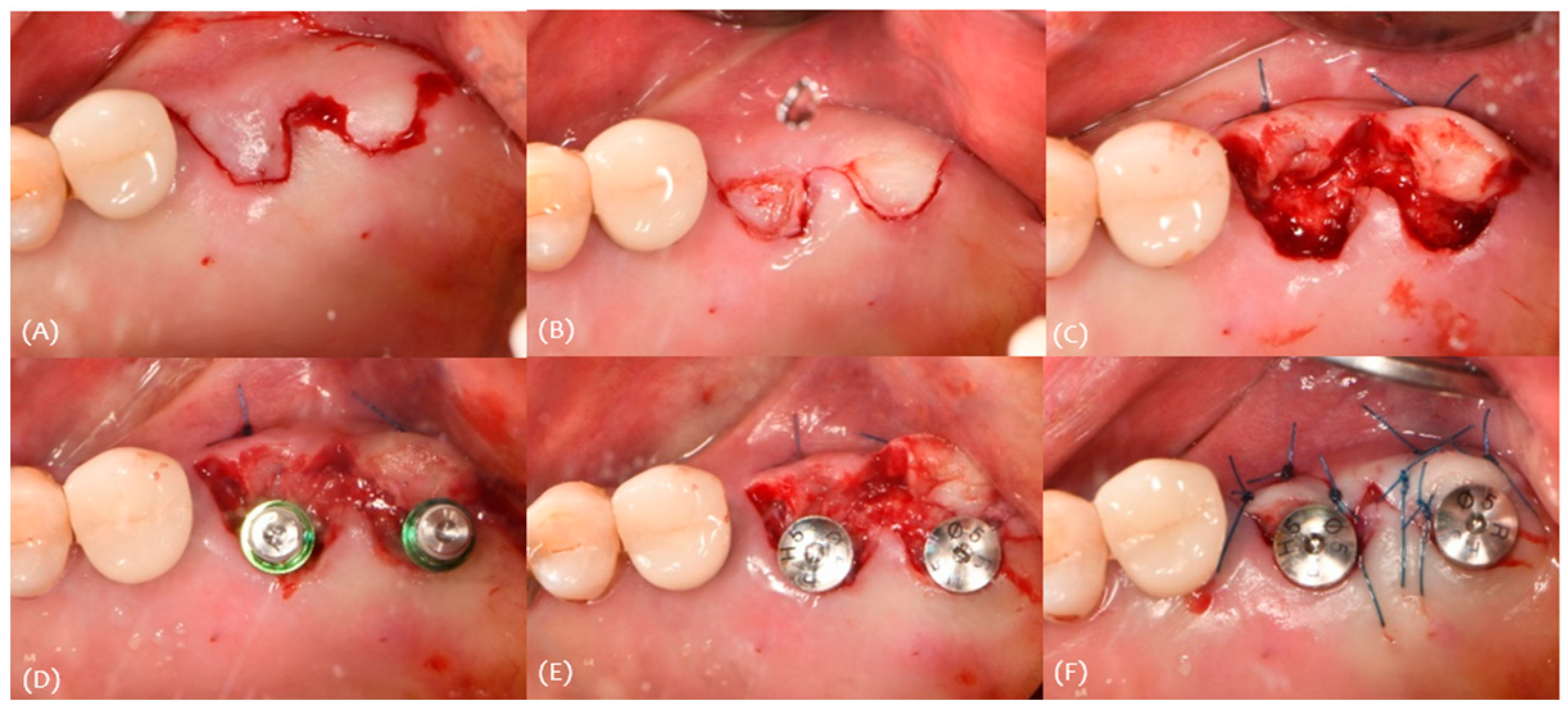
2.2. Surgical Protocol
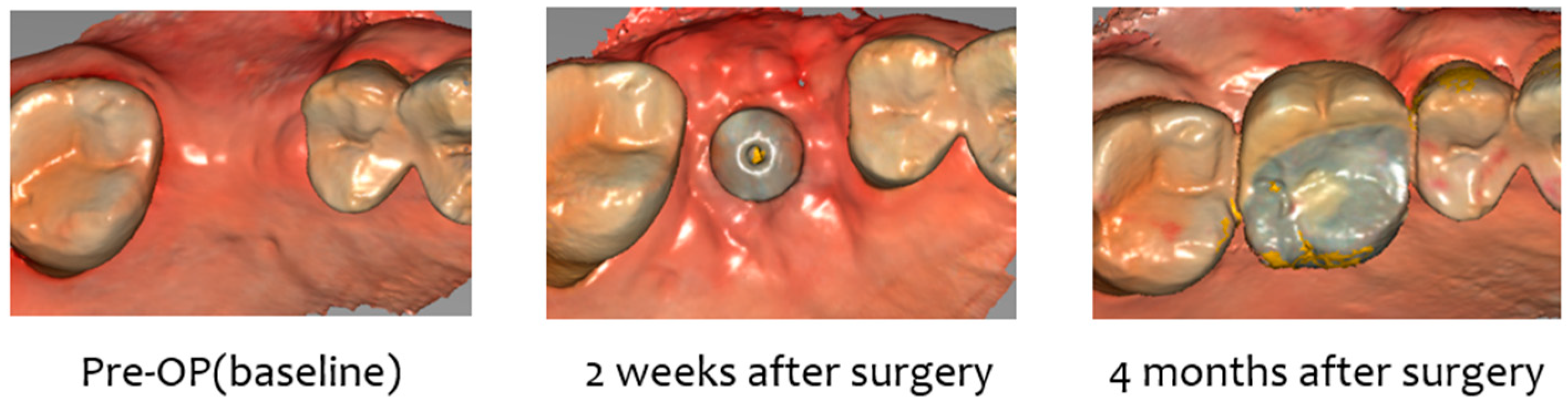
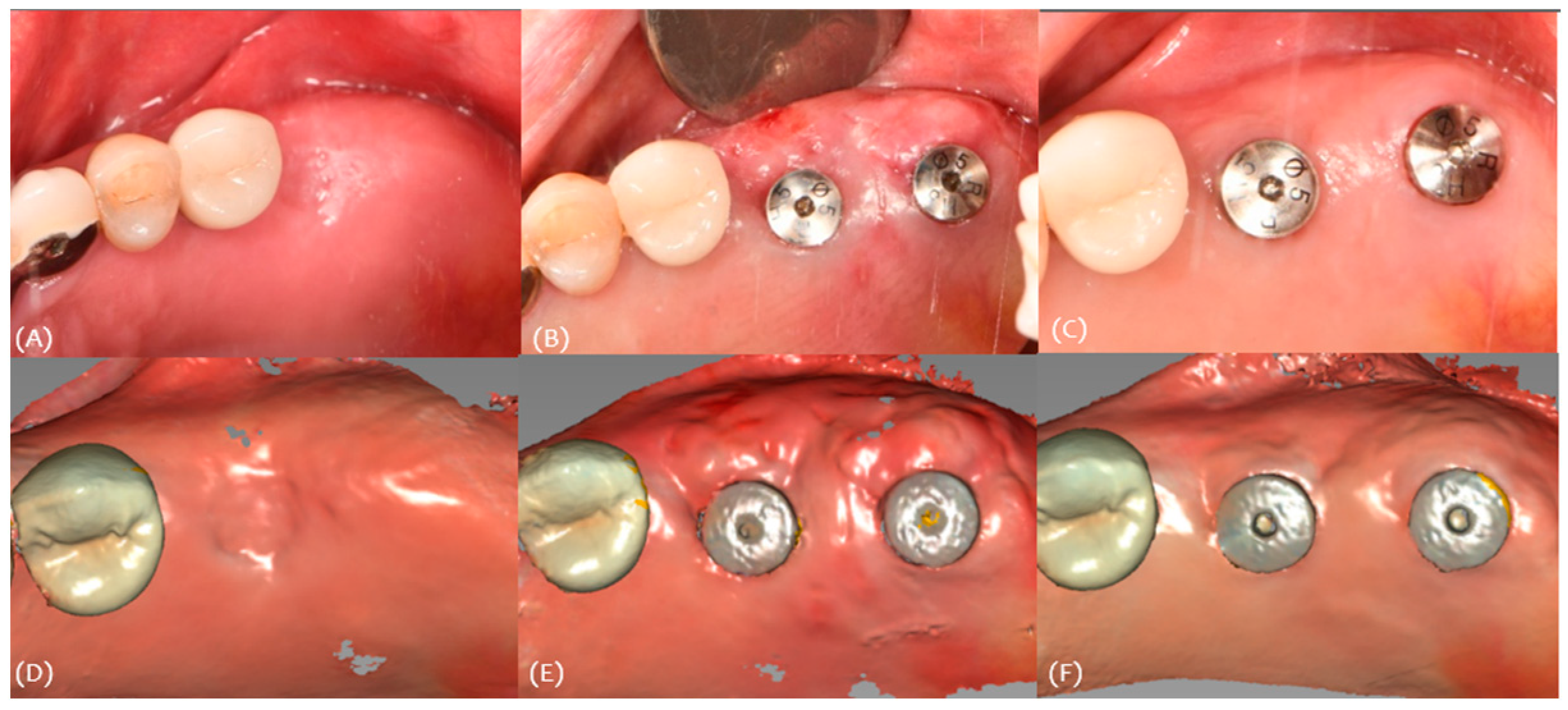
2.3. 3D Scan Protocol
- Pre-operation (pre-op) intraoral scan before surgery;
- Implant placement or second operation;
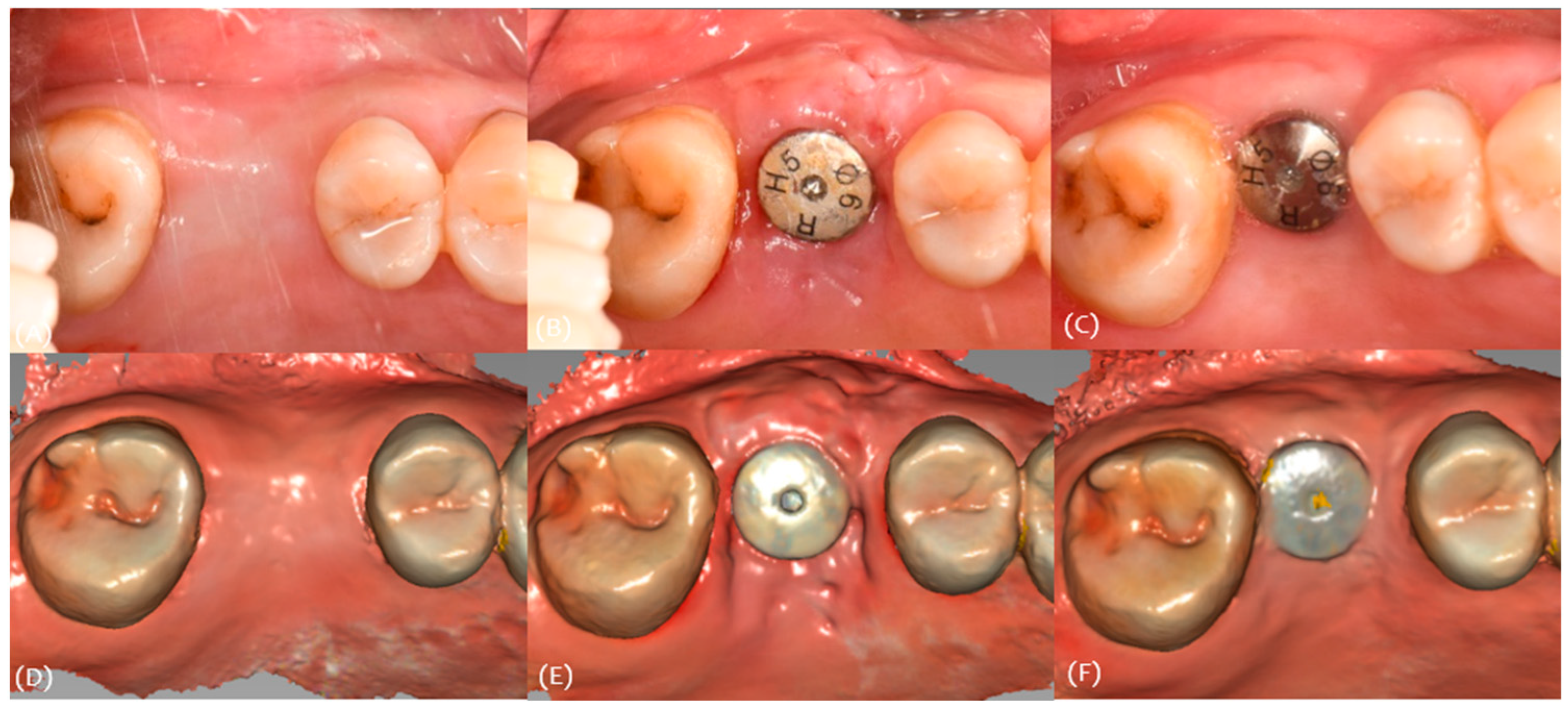
- 2-week, 4-week, and 4-month intraoral scan after the surgery (CS 3600; Carestream Dental, Stuttgart, Germany) (Figure 2);
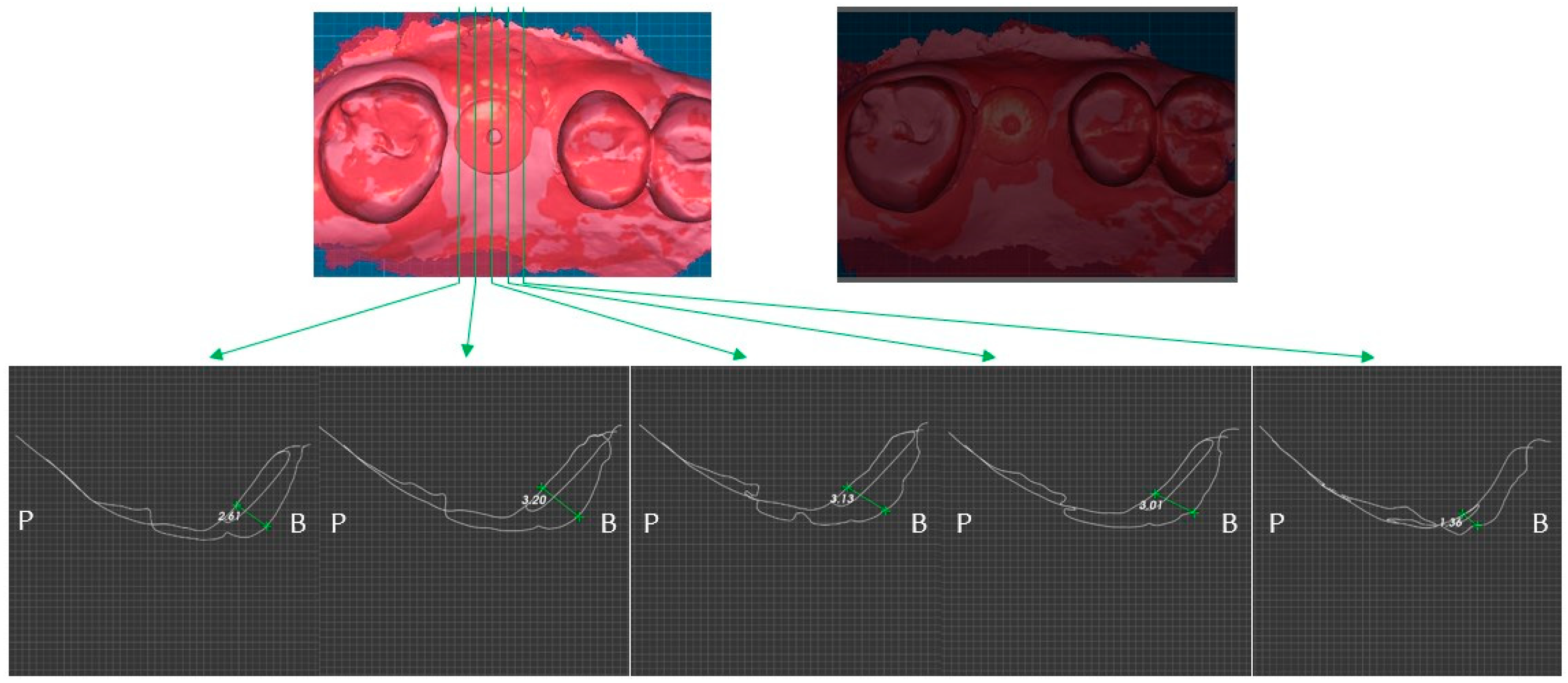
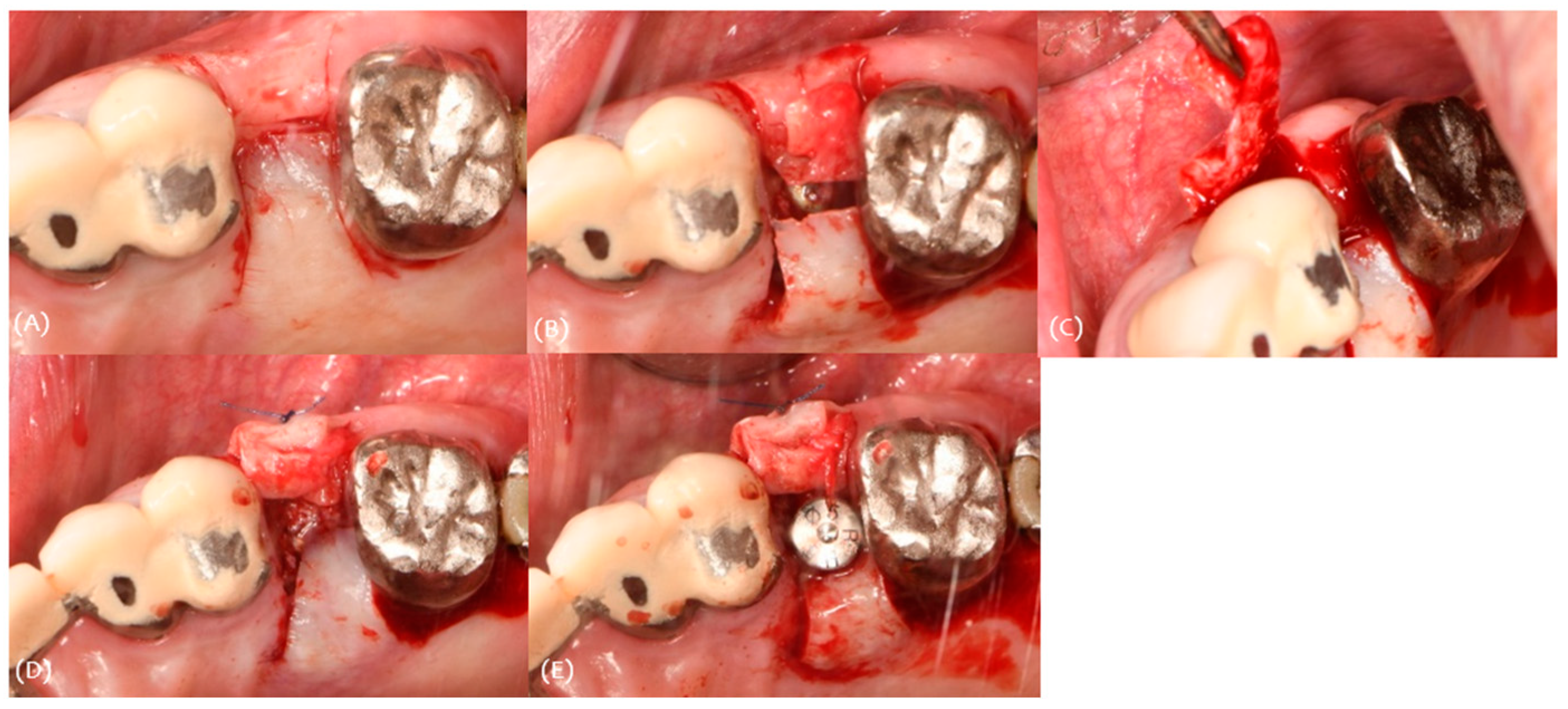
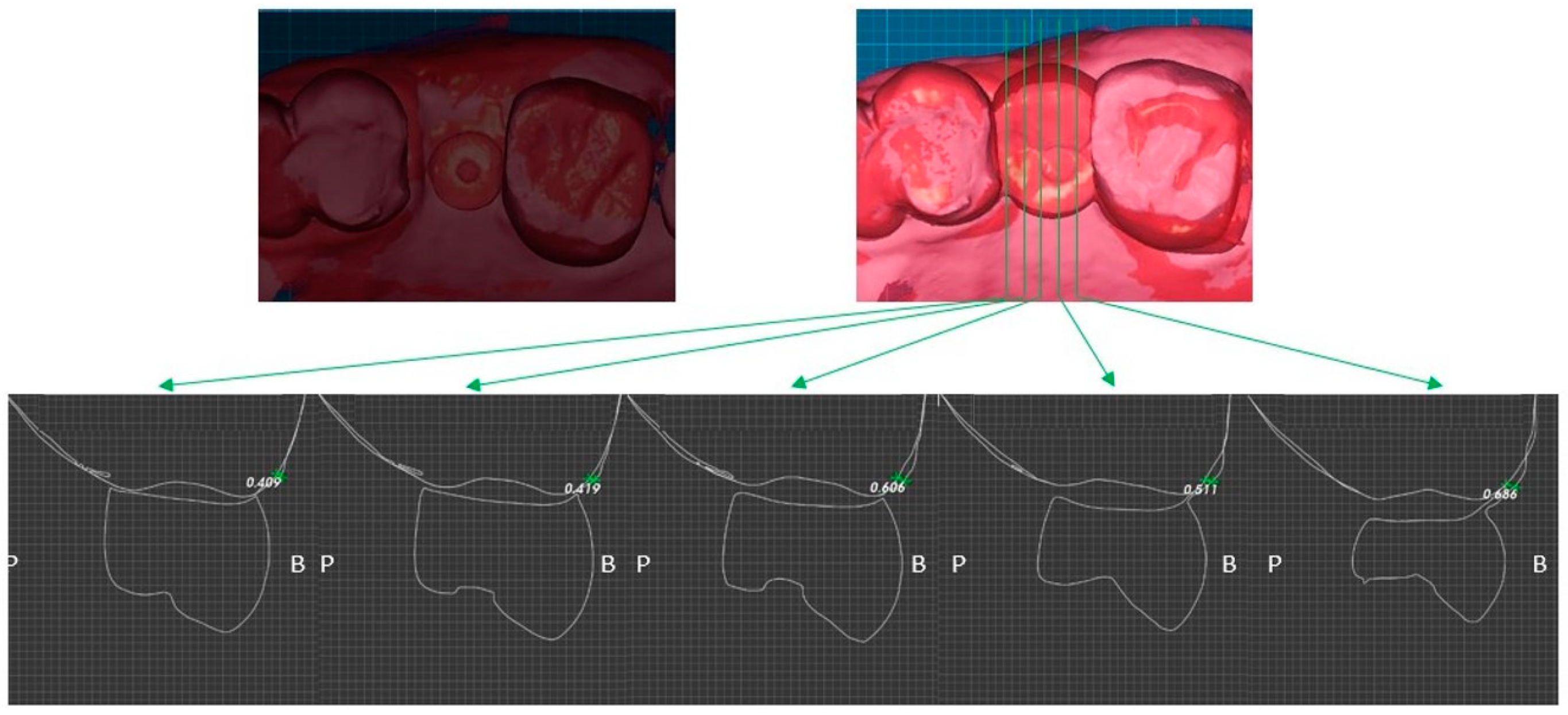
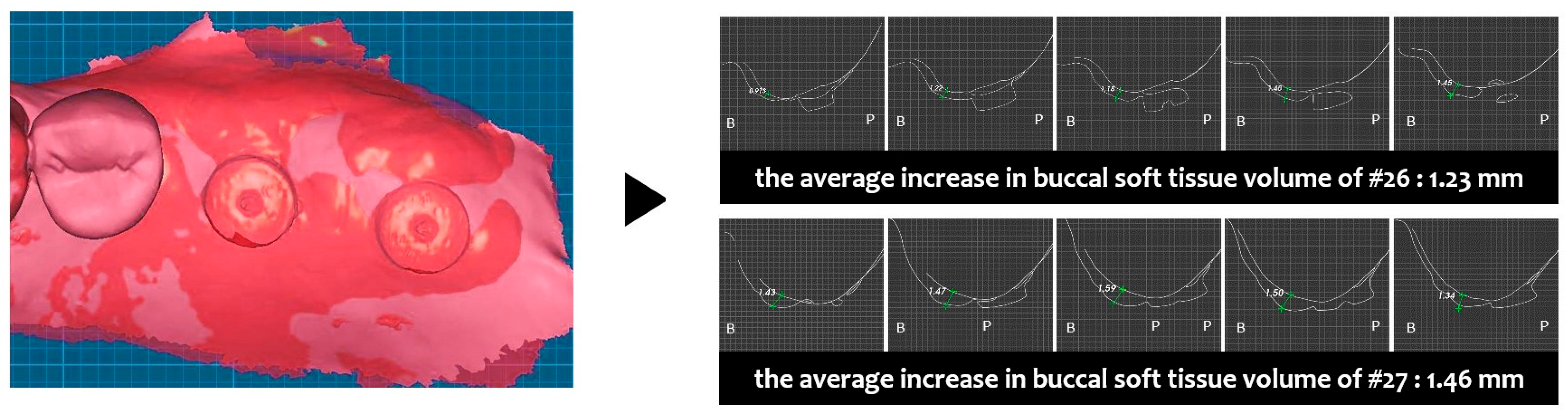
- In Exocad Software (exocad GmbH, DentalCAD 3.0 Galway, Darmstadt, Germany, 2021), a mesh file was added and superimposed using the adjacent teeth as a reference. By overlapping the recorded scan data using Exocad Software, cross-sections were set, and the increase in buccal soft tissue at fixture level was measured at five sites (mesial, mesio-middle, mid, disto-middle, and distal) and averaged.
3. Case Description and Results
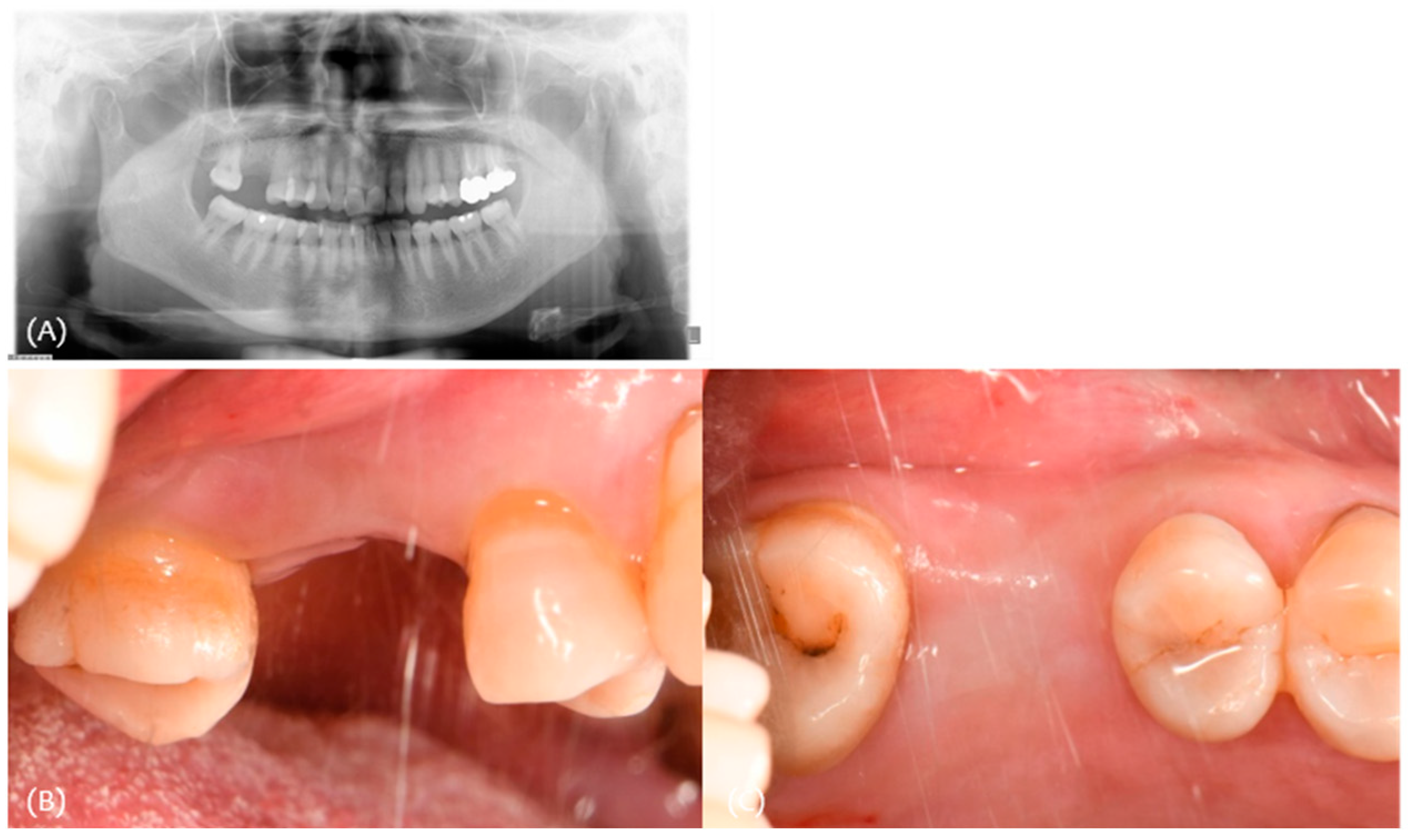
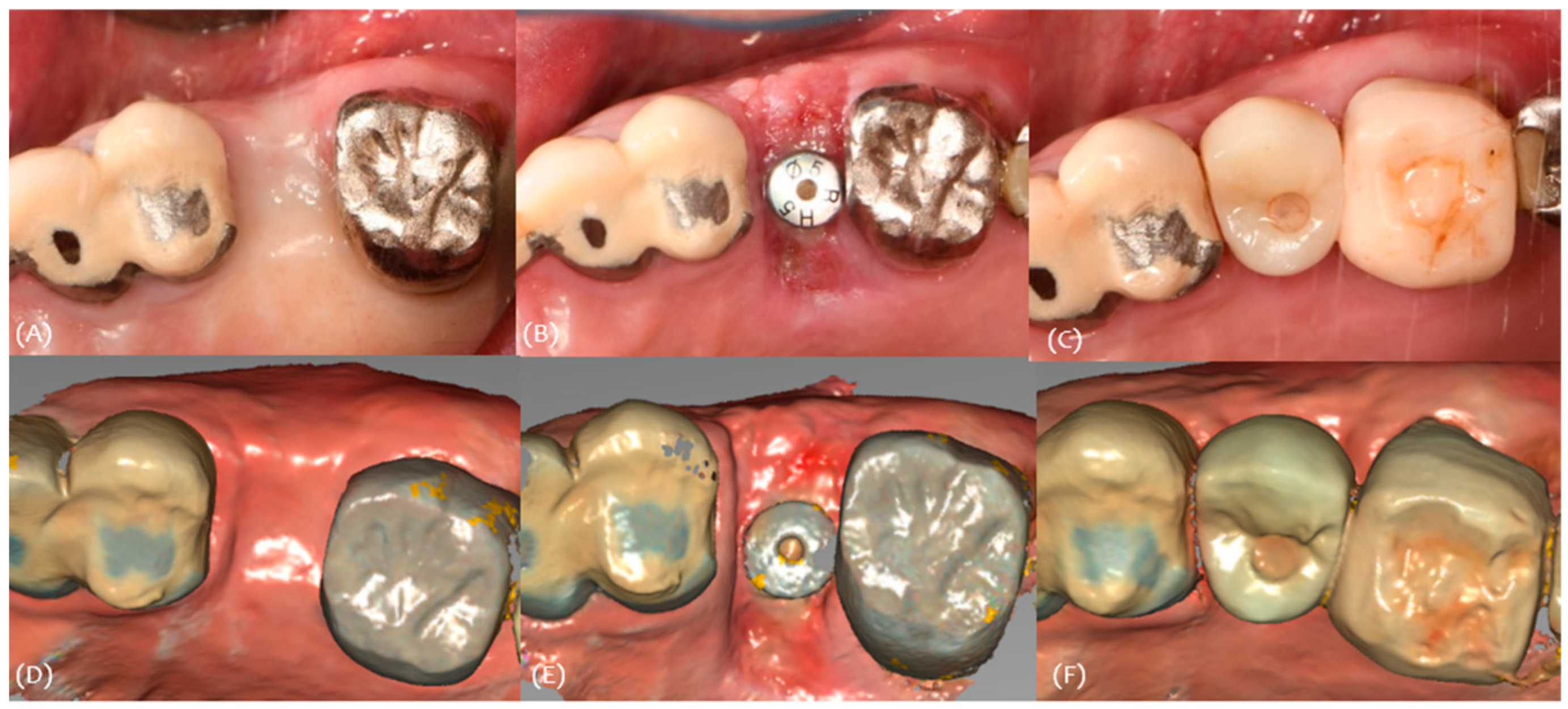
3.1. Case 1
3.2. Case 2
3.3. Case 3
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tan, W.L.; Wong, T.L.; Wong, M.C.; Lang, N.P. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin. Oral Implants Res. 2012, 23 (Suppl. S5), 1–21. [Google Scholar] [CrossRef] [PubMed]
- Js, S. Reconstruction of deformed, partially edentulous ridges, using full thickness onlay grafts. Part I. Technique and wound healing. Compend. Contin. Educ. Dent. 1983, 4, 437. [Google Scholar]
- Allen, E.P.; Gainza, C.S.; Farthing, G.G.; Newbold, D.A. Improved technique for localized ridge augmentation. A report of 21 cases. J. Periodontol. 1985, 56, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Marzadori, M.; Stefanini, M.; Sangiorgi, M.; Mounssif, I.; Monaco, C.; Zucchelli, G. Crown lengthening and restorative procedures in the esthetic zone. Periodontology 2000 2018, 77, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Abrams, L. Augmentation of the deformed residual edentulous ridge for fixed prosthesis. Compend. Contin. Educ. Gen. Dent. 1980, 1, 205–213. [Google Scholar] [PubMed]
- Scharf, D.R.; Tarnow, D.P. Modified roll technique for localized alveolar ridge augmentation. Int. J. Periodontics Restor. Dent. 1992, 12, 415–425. [Google Scholar]
- Langer, B.; Calagna, L. The subepithelial connective tissue graft. J. Prosthet. Dent. 1980, 44, 363–367. [Google Scholar] [CrossRef] [PubMed]
- Garber, D.A.; Rosenberg, E.S. The edentulous ridge in fixed prosthodontics. Compend. Contin. Educ. Dent. 1981, 2, 212–223. [Google Scholar] [PubMed]
- Seibert, J.; Nyman, S. Localized ridge augmentation in dogs: A pilot study using membranes and hydroxyapatite. J. Periodontol. 1990, 61, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Shakibaie, B.; Sabri, H.; Blatz, M.B.; Barootchi, S. Comparison of the minimally-invasive roll-in envelope flap technique to the holding suture technique in implant surgery: A prospective case series. J. Esthet. Restor. Dent. 2023, 35, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Abrahamsson, I.; Berglundh, T.; Wennström, J.; Lindhe, J. The peri-implant hard and soft tissues at different implant systems. A comparative study in the dog. Clin. Oral Implants Res. 1996, 7, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Linkevicius, T.; Apse, P.; Grybauskas, S.; Puisys, A. The influence of soft tissue thickness on crestal bone changes around implants: A 1-year prospective controlled clinical trial. Int. J. Oral Maxillofac. Implants 2009, 24, 712–719. [Google Scholar] [PubMed]
- van Brakel, R.; Noordmans, H.J.; Frenken, J.; de Roode, R.; de Wit, G.C.; Cune, M.S. The effect of zirconia and titanium implant abutments on light reflection of the supporting soft tissues. Clin. Oral Implants Res. 2011, 22, 1172–1178. [Google Scholar] [CrossRef] [PubMed]
- Lops, D.; Stellini, E.; Sbricoli, L.; Cea, N.; Romeo, E.; Bressan, E. Influence of abutment material on peri-implant soft tissues in anterior areas with thin gingival biotype: A multicentric prospective study. Clin. Oral Implants Res. 2017, 28, 1263–1268. [Google Scholar] [CrossRef] [PubMed]
- Avila-Ortiz, G.; Gonzalez-Martin, O.; Couso-Queiruga, E.; Wang, H.L. The peri-implant phenotype. J. Periodontol. 2020, 91, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-S.; Jeon, Y.-S.; Strauss, F.-J.; Jung, H.-I.; Gruber, R. Digital scanning is more accurate than using a periodontal probe to measure the keratinized tissue width. Sci. Rep. 2020, 10, 3665. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Gandolfi, A.; Luongo, G.; Logozzo, S. Intraoral scanners in dentistry: A review of the current literature. BMC Oral Health 2017, 17, 149. [Google Scholar] [CrossRef]

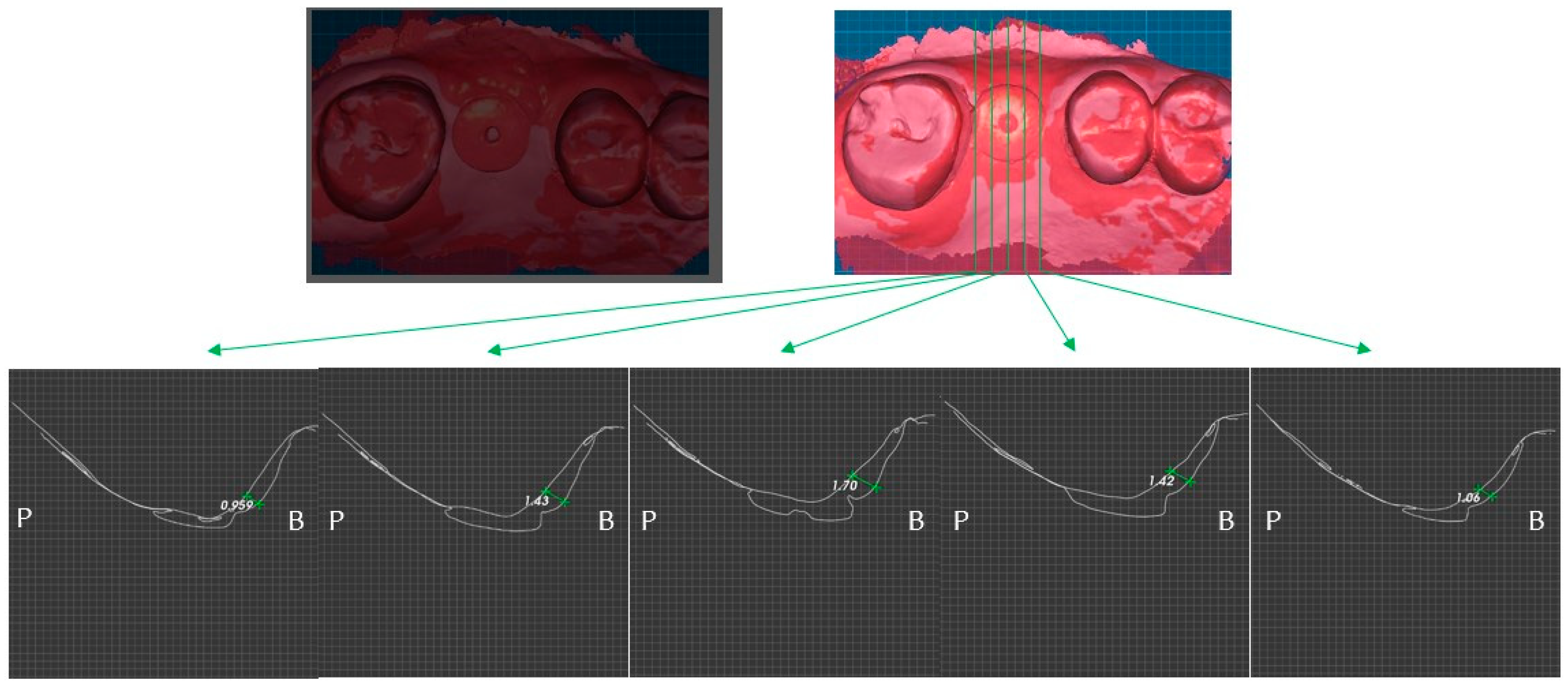



| #17 | #16 | #15 | |
|---|---|---|---|
| Classification (Seibert) | Class I | ||
| Amount of maximum concavity (mm) | 3.5 | ||
| Buccal pocket depth (mm) | 433 | 332 | |
| Palatal pocket depth (mm) | 443 | 333 | |
| Bleeding on probing | - | - | |
| gingival recession (mm) | 000 | 010 | |
| Keratinized tissue Width (mm) | 4 | 5 | 5 |
| Site | Pre-Op Concavity (mm) | Increased Buccal Soft Tissue Volume 2 Weeks After Op (mm) | Increased Buccal Soft Tissue Volume 4 Months After Op (mm) |
|---|---|---|---|
| Distal | 1.3 | Δ 2.61 | Δ 0.959 |
| Disto-middle | 2.9 | Δ 3.2 | Δ 1.43 |
| Middle | 3.5 | Δ 3.13 | Δ 1.7 |
| Mesio-middle | 3.2 | Δ 3.01 | Δ 1.42 |
| Msesial | 2 | Δ 1.36 | Δ 1.06 |
| Average | 2.58 | Δ 2.662 | Δ 1.3138 |
| #24 | #25 | #26 | |
|---|---|---|---|
| Classification (Seibert) | Class I | ||
| Amount of maximum concavity (mm) | 1.8 | ||
| Buccal pocket depth (mm) | 333 | 446 | |
| Palatal pocket depth (mm) | 223 | 346 | |
| Bleeding on probing | - | - | |
| gingival recession (mm) | 000 | 002 | |
| Keratinized tissue Width (mm) | 5 | 4 | 5 |
| Site | Pre-Op Concavity (mm) | Increased Buccal Soft Tissue Volume 2 Weeks After Op (mm) | Increased Buccal Soft Tissue Volume 4 Months After Op (mm) |
|---|---|---|---|
| Distal | 1.2 | Δ 0.963 | Δ 0.409 |
| Disto-middle | 1.5 | Δ 1.52 | Δ 0.419 |
| Middle | 1.8 | Δ 1.39 | Δ 0.606 |
| Mesio-middle | 1.6 | Δ 1.13 | Δ 0.511 |
| Msesial | 1.1 | Δ 0.351 | Δ 0.686 |
| Average | 1.44 | Δ 1.0708 | Δ 0.5262 |
| #25i | #26 | #27 | |
|---|---|---|---|
| Classification (Seibert) | Class I | Class I | |
| Amount of maximum concavity (mm) | 1.2 | 0.8 | |
| Buccal pocket depth (mm) | 222 | ||
| Palatal pocket depth (mm) | 222 | ||
| Bleeding on probing | - | ||
| Gingival recession (mm) | 001 | ||
| Keratinized tissue Width (mm) | 5 | 5 | 6 |
| Site | Pre-Op Concavity (mm) | Increased Buccal Soft Tissue Volume 2 Weeks After Op (mm) | Increased Buccal Soft Tissue Volume 4 Months After Op (mm) | |||
|---|---|---|---|---|---|---|
| #26i | #27i | #26i | #27i | #26i | #27i | |
| Distal | 0.8 | 0.4 | Δ 0.913 | Δ 1.43 | Δ 0.983 | Δ 0.52 |
| Disto-middle | 0.9 | 0.6 | Δ 1.22 | Δ 1.47 | Δ 0.695 | Δ 0.54 |
| Middle | 1.2 | 0.8 | Δ 1.18 | Δ 1.59 | Δ 1.01 | Δ 0.606 |
| Mesio-middle | 1 | 0.7 | Δ 1.4 | Δ 1.5 | Δ 1.03 | Δ 0.226 |
| Msesial | 0.8 | 0.5 | Δ 1.45 | Δ 1.34 | Δ 0.358 | Δ 0.467 |
| Average | 0.94 | 0.6 | Δ 1.2326 | Δ 1.466 | Δ 0.8152 | Δ 0.4718 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, Y.-J.; Do, W.-S.; Hwang, S.-M.; Kim, Y.-G.; Lee, J.-M. Digital Analysis Using 3D Intraoral Scanner on Gingival Contour Changes Following the Roll Flap Technique. Appl. Sci. 2025, 15, 3578. https://doi.org/10.3390/app15073578
Shin Y-J, Do W-S, Hwang S-M, Kim Y-G, Lee J-M. Digital Analysis Using 3D Intraoral Scanner on Gingival Contour Changes Following the Roll Flap Technique. Applied Sciences. 2025; 15(7):3578. https://doi.org/10.3390/app15073578
Chicago/Turabian StyleShin, Ye-Jin, Woo-Seok Do, Sung-Min Hwang, Yong-Gun Kim, and Jae-Mok Lee. 2025. "Digital Analysis Using 3D Intraoral Scanner on Gingival Contour Changes Following the Roll Flap Technique" Applied Sciences 15, no. 7: 3578. https://doi.org/10.3390/app15073578
APA StyleShin, Y.-J., Do, W.-S., Hwang, S.-M., Kim, Y.-G., & Lee, J.-M. (2025). Digital Analysis Using 3D Intraoral Scanner on Gingival Contour Changes Following the Roll Flap Technique. Applied Sciences, 15(7), 3578. https://doi.org/10.3390/app15073578






