Abstract
(1) Background: Advancements in dental imaging technologies have significantly transformed diagnostic and surgical practices. The integration of cone beam computed tomography (CBCT), artificial intelligence (AI), augmented reality (AR), and virtual reality (VR) is enhancing clinical precision, streamlining workflows, and redefining dental education. This review examines the evolution, applications, and future potential of these technologies in modern dental practice. (2) Methods: A narrative literature review was conducted, synthesizing findings from recent studies on digital radiography, CBCT, AI-assisted diagnostics, 3D imaging, and involving simulation tools (AR/VR). Peer-reviewed journal articles, systematic reviews, and clinical studies were analyzed to explore their impact on diagnosis, treatment planning, surgical execution, and training. (3) Results: Digital and 3D imaging modalities have improved diagnostic accuracy and reduced radiation exposure. AI applications enhance image interpretation, automate clinical tasks, and support treatment simulations. AR and VR technologies provide involved, competency-based surgical training and real-time intraoperative guidance. Integrating 3D printing and portable imaging expands accessibility and personalization in care delivery. (4) Conclusions: The integration of CBCT, AI, AR, and VR represents a paradigm shift in dentistry, elevating precision, efficiency, and patient outcomes. Continued research, standardization, and ethical practice will be essential for widespread adoption and maximizing clinical benefits.
1. Introduction
Dental imaging has undergone a major transformation, moving from traditional film-based X-rays to advanced, data-driven systems enabled by artificial intelligence (AI), augmented reality (AR), and virtual reality (VR). This evolution reflects broader trends in digital health, where new technologies are being integrated into clinical workflows to enhance diagnostic accuracy, surgical precision, and patient care (Scheme 1). Tools such as Cone Beam Computed Tomography (CBCT), deep learning algorithms, and comprehensive simulation platforms now enable clinicians to visualize, plan, and perform procedures with greater detail and control. These advances represent not only technological advancements but also a fundamental change in the way dentistry is taught, practiced, and experienced [1,2].
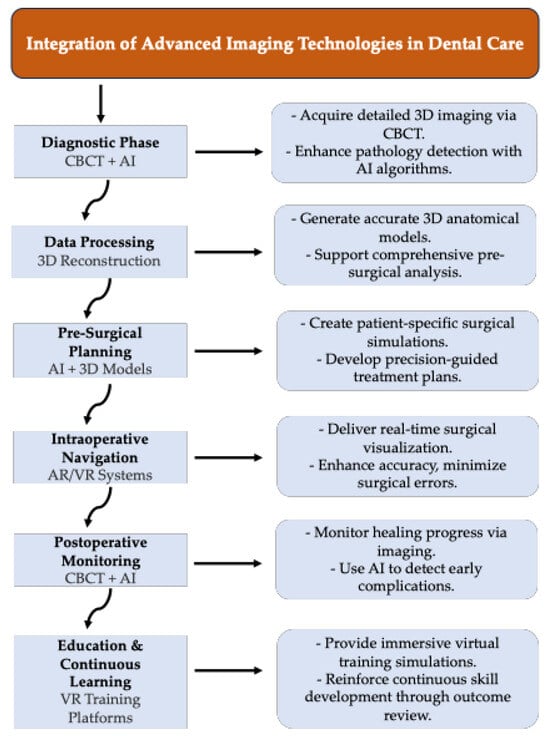
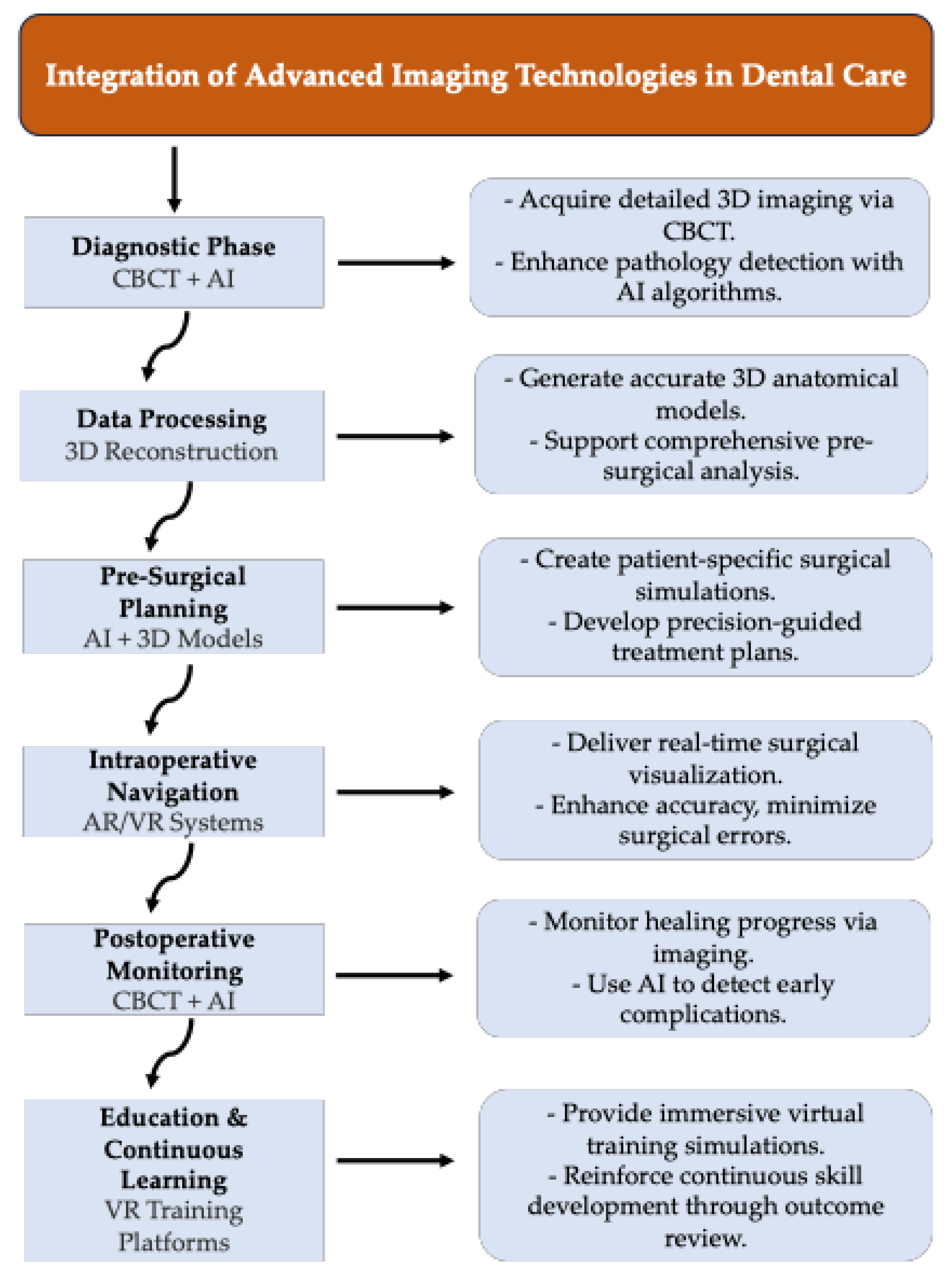
Scheme 1.
This scheme illustrates how advanced technologies, CBCT, AI, AR/VR, and 3D printing, are integrated into various phases of dental care. It starts with diagnosis, where CBCT scans are enhanced by AI for accurate pathology detection. The data supports 3D reconstruction, enabling precise pre-surgical planning. During treatment, AR/VR tools assist with real-time intraoperative navigation to improve accuracy and reduce complications. Postoperative imaging, combined with AI monitoring, helps in assessing recovery. Finally, immersive VR platforms provide educational feedback and virtual training, promoting continuous learning for dental professionals.
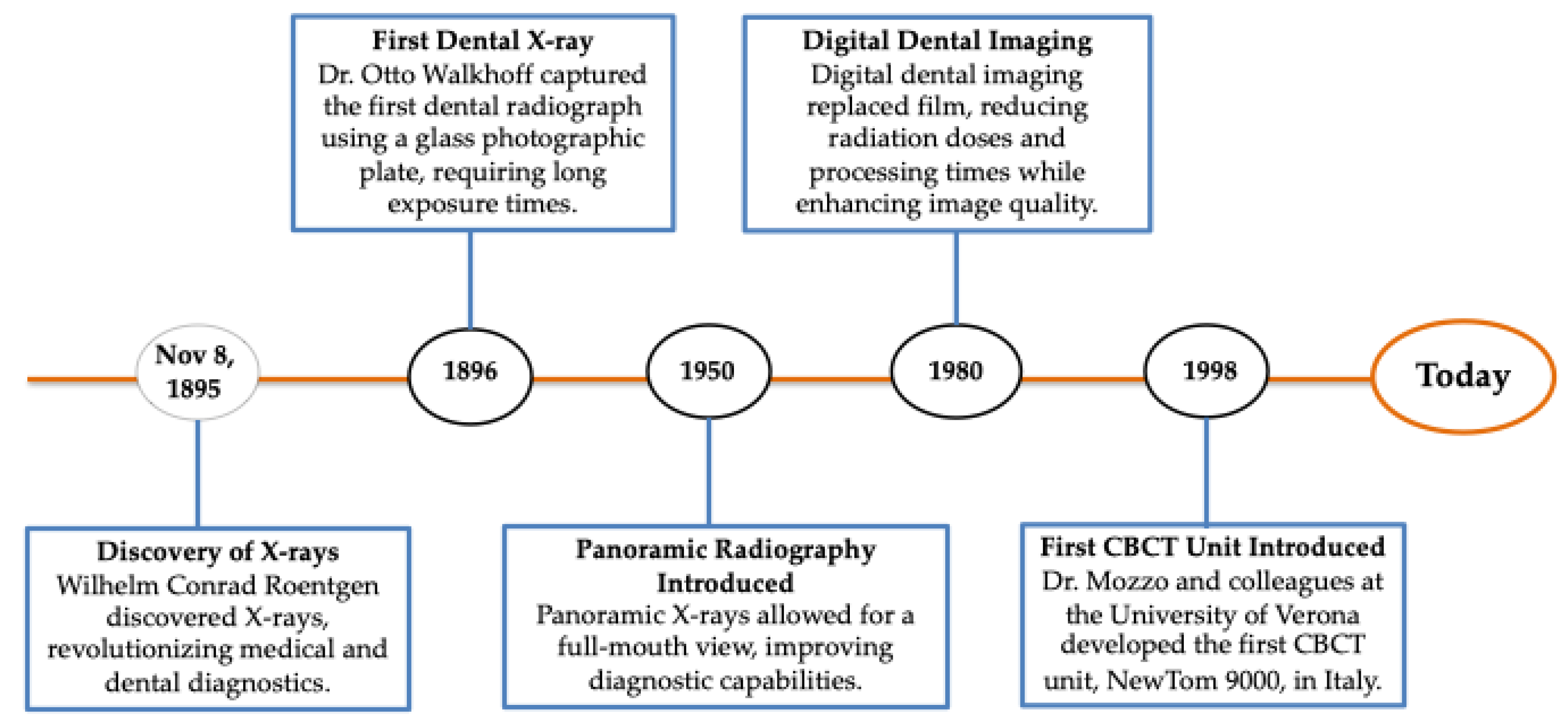
Dental imaging has its origins in the revolutionary discovery of X-rays by Wilhelm Conrad Roentgen on 8 November 1895 (Figure 1). This innovation revolutionized medical diagnosis by allowing visualization of internal structures without invasive procedures [1]. Roentgen’s contribution was so significant that he received the first Nobel Prize in Physics in 1901, highlighting the transformative impact of X-ray technology on both medicine and dentistry. Shortly after the discovery of X-rays, radiography was introduced into dentistry, with Dr. Otto Walkhoff performing the first dental radiograph in 1896. Early methods were rudimentary, relying on glass photographic plates and long exposure times that resulted in high radiation doses [3]. Over time, improvements like faster film speeds and safety measures like lead aprons have made dental radiography much safer and more practical. The mid-20th century marked a major advancement in dental imaging with the introduction of panoramic radiography in the 1950s, enabling full-mouth views. This was followed by the appearance of digital radiography in the 1980s, which improved diagnostic accuracy, reduced processing time and radiation exposure, and greatly enhanced workflow efficiency.
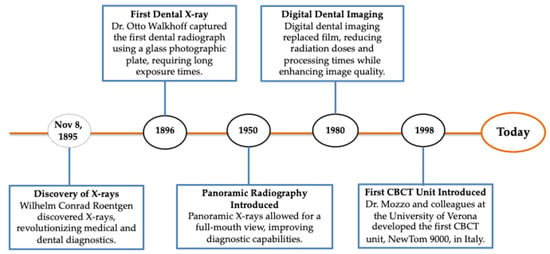
Figure 1.
Timeline of key advancements in intraoral radiographic imaging. This figure depicts the major milestones in dental imaging, starting with the discovery of X-rays by Wilhelm Conrad Roentgen in 1895. It includes the first dental radiograph by Dr. Otto Walkhoff in 1896, the introduction of panoramic radiography in 1950, the transition to digital imaging in the 1980s, and the development of Cone Beam Computed Tomography (CBCT) in 1998 by Dr. Mozzo and colleagues. These innovations have improved diagnostic accuracy, reduced radiation exposure, and revolutionized surgical planning in dentistry.
Today, dental imaging plays a vital role in the diagnosis and management of conditions such as dental caries, periodontal disease, fractures, and jaw pathologies. Continued technological advances have introduced tools such as digital sensors, artificial intelligence (AI), and three-dimensional (3D) imaging systems such as Cone Beam Computed Tomography (CBCT). These innovations provide high-resolution images and improve diagnostic accuracy through AI-enabled analysis and integrated digital workflows [4]. This progression lays the groundwork for exploring how these technologies have specifically enhanced surgical planning and execution in modern dental practice.
Advanced imaging technologies like AI, CBCT, AR, and VR are reshaping dental care. This review explores their development and integration into diagnostics, surgery, and clinical training. It evaluates their clinical impact, technological advancements, and educational value, while also highlighting current challenges and proposing future directions for research and implementation in precision dentistry.
2. Materials and Methods
This study employs a structured narrative literature review to synthesize and critically evaluate recent advancements in dental imaging technologies, focusing on CBCT, AI, AR, and VR in diagnostic imaging, surgical planning, and dental education.
Search Strategy: We conducted a comprehensive search using PubMed, Scopus, Web of Science, and Google Scholar for English-language peer-reviewed articles published between 2010 and 2025. The following keyword combinations were used: “dental imaging”, “CBCT”, “artificial intelligence in dentistry”, “augmented reality”, “virtual reality”, “3D printing”, and “digital dentistry”. Boolean operators were applied to refine the search.
Selection Process: From the 2015 initial results, duplicates were removed, and 134 full-text articles were screened. Of these, 68 studies met the inclusion criteria and were included in the final synthesis.
Inclusion Criteria: Studies were included if they:
- Focused on the application of CBCT, AI, AR/VR, or related digital imaging technologies in dentistry;
- Provided empirical data (clinical trials, observational studies, or systematic reviews) or were technical papers with clear relevance to diagnostics, surgery, or education;
- They were published in peer-reviewed journals.
Exclusion Criteria: We excluded non-English studies, abstracts without full-text access, conference proceedings, non-peer-reviewed materials, and papers lacking clinical applicability.
Thematic Grouping: Included studies were grouped into three primary domains: (1) Diagnostics and Imaging; (2) Surgical Planning and Intraoperative Support; and (3) Dental Education and Simulation. Subthemes within each domain were identified during full-text analysis.
Quality Consideration: Although formal bias assessment tools (e.g., PRISMA, AMSTAR) were not employed due to the narrative nature of this review, studies were evaluated qualitatively based on:
- Relevance to dental clinical practice,
- Level of evidence (e.g., randomized controlled trials, cohort studies, technical validation),
- Technological innovation and clinical impact.
3. Evolution of Radiographic Practice: From Traditional to Digital Imaging
Conventional dental imaging began with periapical and panoramic radiographs, which provided essential but limited two-dimensional views of dental structures. These modalities were often hindered by overlapping anatomical features and a lack of depth perception, making it difficult to visualize complex pathologies and accurately plan surgical interventions [3]. Despite these limitations, traditional radiographs formed the foundation of modern dental imaging and continue to be used in certain cases due to their simplicity, accessibility, and low cost.
The transition to digital radiography marked a significant advance in dental imaging, introducing technologies that improved both diagnostic accuracy and patient safety. Among these advances, notable were charge-coupled devices (CCDs) and complementary metal-oxide-semiconductor (CMOS) sensors, which allowed for real-time image capture, improved resolution, and lower radiation exposure [5]. While CCDs are known for their excellent image quality, CMOS sensors offer comparable resolution with added advantages such as lower power consumption and reduced cost, leading to their increasing use in clinical practice. At the same time, photostimulating phosphor (PSP) plates emerged as a flexible and reusable option. These plates store X-ray energy for delayed scanning, offering greater patient comfort, especially in cases with limited mouth opening or anatomical constraints. However, PSP systems are not without flaws; image artifacts can occur due to contamination or improper plate handling, which can result in diagnostic errors.
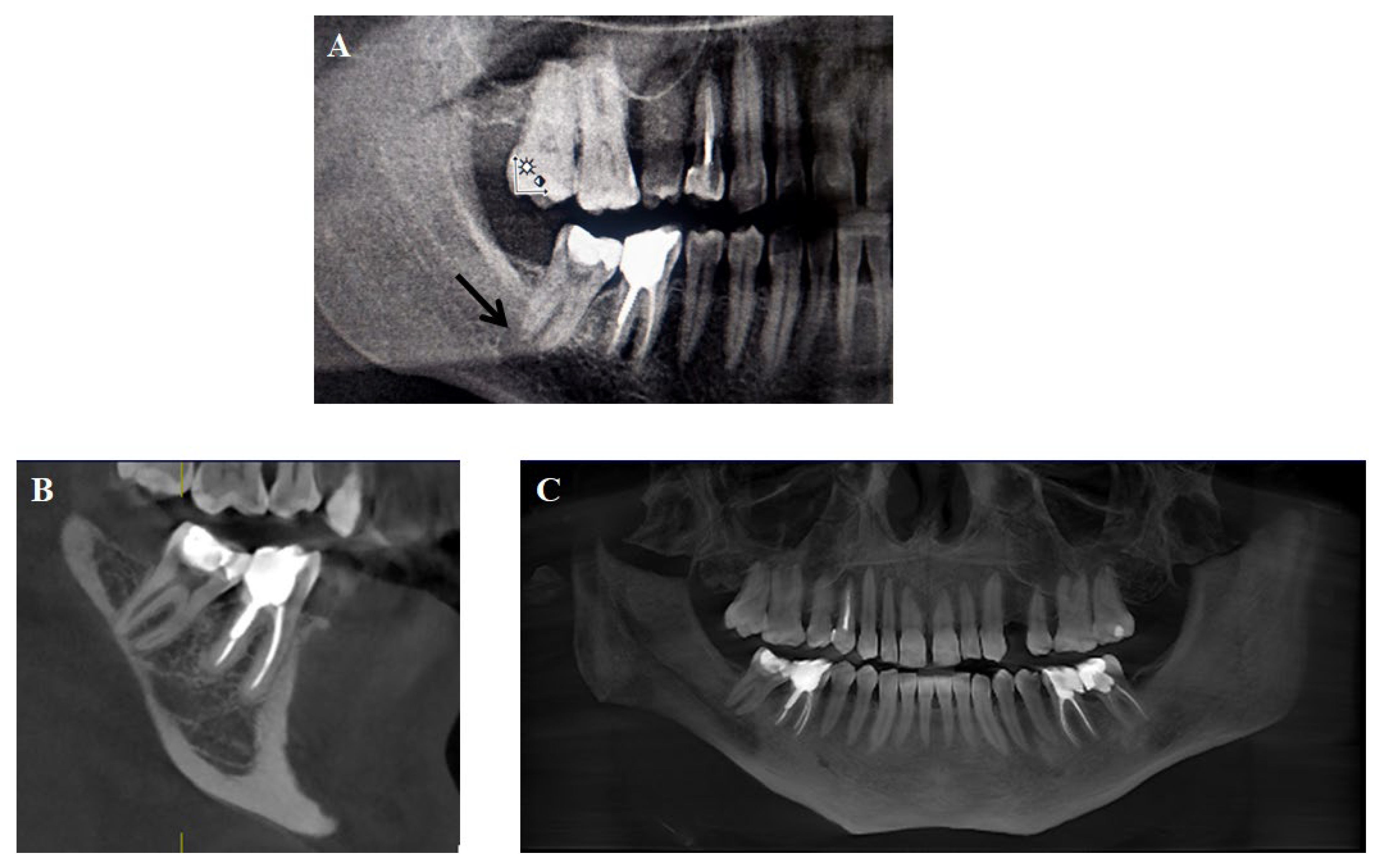
These artifacts can mimic pathological conditions, such as cysts (Figure 2) or other lesions, complicating diagnosis and treatment planning. This underscores the importance of strict quality control in imaging systems, especially those using phosphor plates, which are more susceptible to contamination and physical damage [6].
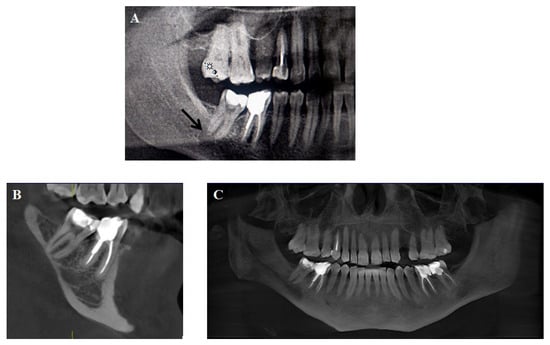
Figure 2.
(A) Panoramic radiograph of a 38-year-old male showing a well-defined, round radiolucent area near the distal root of the right mandibular second molar (black arrow), initially suggestive of a cystic lesion. (B) Coronal CBCT section of the same region reveals intact cortical margins and no sign of a cyst, effectively ruling out pathology. (C) Panoramic reconstruction confirms complete resolution of the radiolucency, indicating that it was an artifact caused by contamination or improper handling of the phosphor storage plate. This case illustrates the importance of correlating panoramic radiographs with CBCT findings to avoid diagnostic errors and unnecessary treatment. Image courtesy of Nebi Cemeta.
4. Modern Imaging Technologies
4.1. Portable Imaging Devices
The development of portable dental imaging devices marks an important step towards expanding diagnostic access, especially in remote, underserved, or emergency settings. These compact, battery-operated systems are suitable for use in mobile dental units, with patients confined to their homes and during humanitarian missions, allowing clinicians to perform imaging on site without the need for patients to visit a dental clinic [7].
Modern portable devices often feature wireless data transfer and cloud integration, enabling real-time image sharing with specialists and facilitating collaborative treatment planning. These capabilities are particularly valuable for remote consultations and telemedicine applications. Looking ahead, portable imaging systems are expected to incorporate AI-assisted diagnostics and potentially 3D imaging, further increasing their effectiveness in decentralized and field-based dental care [8].
4.2. CBCT: A Foundation for 3D Visualization
The introduction of CBCT marked a transformative advance in dental imaging, providing high-resolution 3D reconstructions of maxillofacial anatomy. Unlike conventional radiographs, CBCT allows clinicians to evaluate structures from multiple angles, significantly improving diagnostic accuracy in fields such as implantology, orthodontics, endodontics, and maxillofacial pathology [9,10]. Metrics such as spatial resolution and artifact suppression highlight the superiority of CBCT over conventional panoramic radiography. CBCT offers resolution thresholds ranging from approximately 75 to 200 μm, compared to 300–500 μm for 2D panoramic imaging. This enhanced resolution is particularly critical for detecting fine anatomical details such as accessory canals, root fractures, or cortical bone defects that may be missed on conventional radiographs. Additionally, CBCT systems employ sophisticated image reconstruction algorithms that minimize artifacts from overlapping structures or metal restorations, improving diagnostic confidence and reducing false positives [9,10].
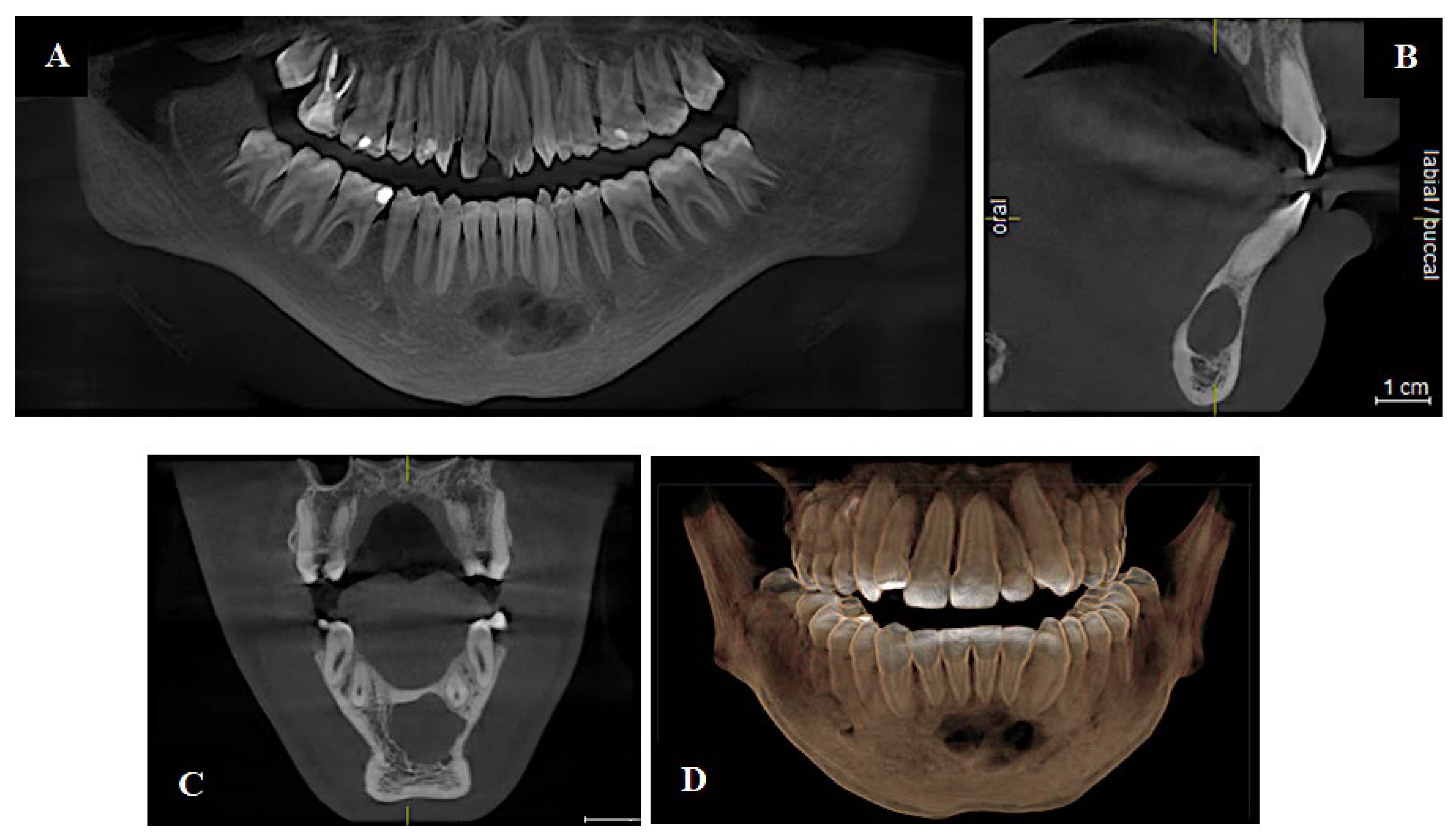
In implantology, CBCT provides essential information on bone density, nerve pathways, and sinus anatomy, helping to ensure accurate and safe implant placement. In orthodontics, it facilitates the evaluation of impacted teeth and craniofacial anomalies. For endodontics, CBCT reveals hidden canals and periapical lesions that are often not seen on 2D images. It also plays a key role in the evaluation of the temporomandibular joint (TMJ) by visualizing bony changes associated with conditions such as ankylosis, erosion, and osteoarthritis [11,12]. In oral and maxillofacial surgery (Figure 3), CBCT supports comprehensive preoperative planning, intraoperative navigation, and postoperative evaluation of fractures, pathologies, and reconstructive procedures [13,14].
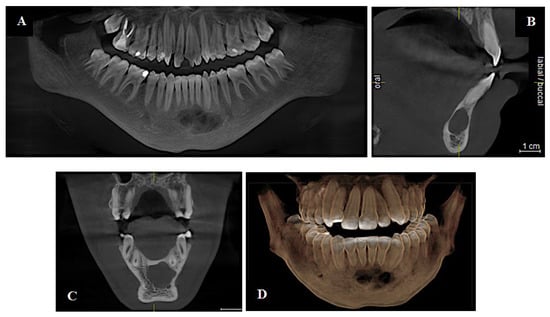
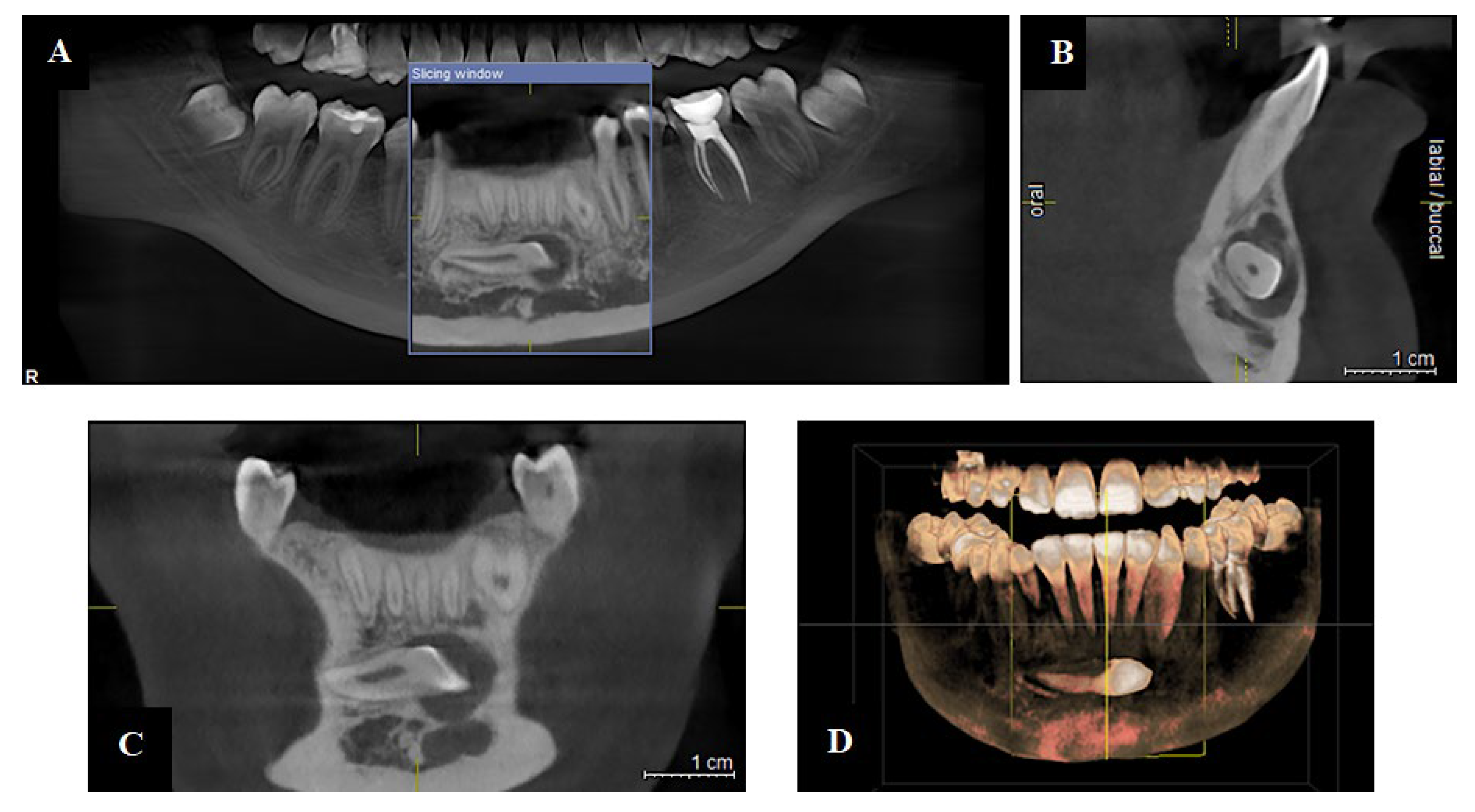
Figure 3.
CBCT imaging of a 17-year-old patient presenting with a cystic lesion in the mandibular body. (A) Panoramic reconstruction showing the overall dentition and determining the full mesiodistal extent of the lesion, aiding in pre-surgical planning. (B) Sagittal view illustrating the lesion’s proximity to the tooth root and cortical borders. (C) Coronal view displaying buccolingual expansion and lesion involvement. (D) The 3D imaging provides a view of the lesion about the surrounding anatomical structures, facilitating planning of the surgical approach and risk assessment for nearby neurovascular elements. Image courtesy of Nebi Cemeta.
Despite its advantages, CBCT is not without limitations. The technology involves higher costs and infrastructure demands compared to conventional radiography, limiting its adoption in resource-constrained settings. Radiation exposure, though reduced through low-dose protocols, remains a concern for routine imaging, especially in pediatric or follow-up cases. Operator training and standardization of image interpretation are also necessary to ensure consistent diagnostic outcomes [10].
4.3. Photon-Counting Computed Tomography
Photon-Counting Computed Tomography (PCCT) represents a major advancement in dental imaging, offering enhanced spatial resolution, superior contrast, reduced image noise, intrinsic spectral data, and more efficient radiation dose usage. These features enable clearer visualization of anatomical structures, which is critical for accurate diagnosis and treatment planning in dentistry [15,16]. PCCT uses photon-counting detectors (PCDs) that directly convert individual X-ray photons into digital signals with high precision. This technology significantly minimizes metal artifacts from implants using techniques such as Iterative Metal Artifact Reduction (iMAR), Virtual Monoenergetic Imaging (VMI), and sinogram inpainting, thereby improving diagnostic reliability in implant-related cases [17]. Thanks to its high-resolution imaging and artifact reduction, PCCT is especially well-suited for complex diagnostic scenarios in orthodontics, implantology, and oral surgery.
4.4. Recent Advances in Radiation Protection in Dental Imaging
Radiation protection remains a main priority in dental imaging. The transition from film-based systems to digital radiography has significantly reduced radiation exposure, largely due to the use of high-sensitivity sensors such as CCD and CMOS, which produce high-quality images at lower doses [18].
Further improvements have been achieved through techniques like low-dose CBCT protocols, adaptive image filtering, and size-specific exposure modulation, which allow modern CBCT systems to automatically tailor radiation levels based on clinical requirements, minimizing unnecessary exposure [19]. In addition, deep learning algorithms now support noise removal from low-dose CT images, helping to maintain diagnostic accuracy while further reducing radiation [20].
Innovations in patient protection have also contributed to safety. Nanocomposite-coated protective garments offer improved comfort without compromising radiation attenuation. Meanwhile, traditional lead aprons and thyroid collars continue to play a vital role in protecting sensitive tissues during radiographic procedures [21].
5. Enhancement of Dental Imaging Protocols and Applications
Advancements in AI and digital technologies have significantly optimized dental imaging protocols. AI now plays a central role in improving image acquisition, processing, diagnostic accuracy, and radiation dose management. Integrated algorithms enable real-time exposure adjustments and post-processing noise removal, minimizing the need for repeat scans and promoting safer, higher-quality imaging outcomes [22].
5.1. AI Integration and Machine Learning (ML) in Dental Imaging
AI, including deep learning (DL) and machine learning (ML), has become a basis in the advancement of dental imaging. These technologies automate diagnostic processes, improve image interpretation, and support clinical decision-making in both routine care and complex surgical planning [2,23].
Modern AI models demonstrate superior performance in image classification, object detection, and segmentation, enabling accurate identification of dental caries, periodontal disease, root morphology, and anatomical landmarks essential for surgical navigation. By integrating multimodal data, such as CBCT scans with intraoral imaging, AI can generate comprehensive 3D reconstructions. These models enhance personalized treatment planning and preoperative simulations [24].
Commonly used deep learning architectures such as U-Net and ResNet have shown promising accuracy (>90%) in caries detection and landmark identification in CBCT datasets. However, many models lack external validation. For example, a study using U-Net for periapical lesion detection reported an AUC of 0.93, but was limited to a dataset from a single institution, raising concerns about generalizability [25]. Furthermore, when comparing across dental specialties, AI performance tends to be more robust in visualized tasks such as caries detection and landmark identification, while it is less validated in areas requiring contextual judgment, such as endodontic retreatment planning or TMJ pathology [24,25].
ML algorithms further elevate diagnostic precision through predictive modeling and longitudinal analysis. Clinical applications include early detection of bone loss, monitoring lesion progression, and identifying anatomical anomalies. In addition, radiomics, the extraction of high-dimensional features from medical images, reveals subtle, subvisual patterns linked to disease phenotypes. When combined with DL models, radiomics significantly enhances diagnostic sensitivity, particularly in areas such as maxillofacial oncology and endodontics [26,27,28].
Generative AI, particularly Generative Adversarial Networks (GANs), is playing an increasingly important role in dental imaging. These models enhance image quality by removing noise, reducing artifacts, and improving resolution. Additionally, GANs can generate synthetic training data, which is especially valuable for improving algorithm performance in detecting rare or underrepresented pathologies. Such capabilities also support scalable applications in dental education and tele-dentistry platforms [2].
Beyond diagnostics, AI contributes to clinical decision-support systems by analyzing large-scale imaging and clinical datasets to propose individualized treatment strategies. Applications include optimizing surgical guide design, predicting post-operative outcomes, and reducing intraoperative risk. The integration of AI and ML in dental imaging indicates a progression toward more accurate, efficient, and personalized patient care [29].
5.2. Imaging-Guided Diagnosis and Treatment Planning
Dental imaging is essential for accurate diagnosis and effective treatment planning across all clinical disciplines. High-resolution imaging enables early detection of pathologies and detailed visualization of critical anatomical features, including root morphology, canal systems, and bone density [18]. The integration of real-time analysis tools and AI-driven assessments increases diagnostic reliability and clinical decision-making.
Digital imaging also plays an important role in preoperative planning, helping to minimize intraoperative complications. It supports precise measurement and design for procedures such as implant placement, bone grafting, denture fabrication, and orthodontic interventions. By improving accuracy and reducing procedural risks, advanced imaging significantly contributes to the safety and success of modern dental care [30].
5.2.1. Endodontics
In endodontics, CBCT’s high-resolution capabilities are particularly useful for identifying complex canal morphologies, such as C-shaped or bifurcated roots, which are difficult to detect using 2D modalities. Its role is especially valuable in non-surgical retreatment and apical surgery, where spatial navigation is critical. These modalities are also effective in detecting periapical lesions, internal and external root resorption, and root fractures, all of which can significantly impact prognosis and treatment success [31].
For surgical endodontics, 3D imaging offers a preoperative insight into the anatomical relationships between roots and adjacent structures such as nerves and sinus cavities, thereby minimizing the risk of complications. Postoperative assessments also benefit from high-resolution imaging, allowing clinicians to monitor healing and confirm treatment efficacy [32].
5.2.2. Implantology
Implantology uniquely benefits from CBCT by enabling digital planning of implant angulation and depth using guided surgery software. It also supports virtual mock-ups and prosthesis fit simulations, critical for full-arch reconstructions and immediate loading protocols. CBCT offers 3D visualization of bone volume, density, and the spatial relationship to critical anatomical landmarks, such as the maxillary sinuses, inferior alveolar nerve, and adjacent teeth [33].
In the postoperative phase, advanced imaging facilitates the evaluation of implant stability, supports immediate loading protocols, and allows for the early detection of complications such as peri-implantitis or mechanical failures. It also plays a key role in assessing graft integration following sinus lifts or bone augmentation procedures and in ensuring an optimal prosthetic fit. These advancements contribute to improved efficiency, clinical accuracy, and higher patient satisfaction [34].
5.2.3. Orthodontics
Orthodontic treatment planning utilizes CBCT not only for impacted tooth localization but also for analyzing airway dimensions and skeletal symmetry. This extends the technology’s role beyond dental alignment into comprehensive craniofacial assessment [35]. Figure 4 shows airway dimensions and bone density, all of which are critical for predicting tooth movement, planning anchorage strategies, and optimizing clinical outcomes.
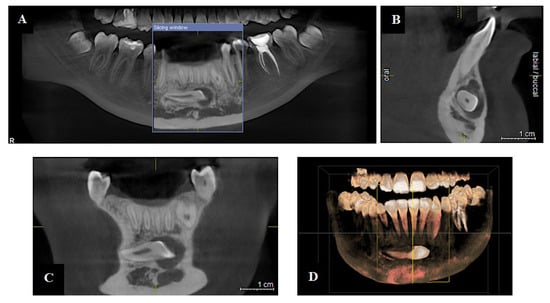
Figure 4.
CBCT images of a 14-year-old patient used for orthodontic assessment reveal an impacted tooth. (A) The panoramic reconstruction illustrates overall dental development and shows the abnormal positioning of the impacted tooth. (B) The sagittal view detects buccolingual orientation and proximity to adjacent roots, which may complicate eruption or require root protection during orthodontic movement. (C) The coronal slice displays the vertical impaction and spatial relationship with surrounding structures, informing both the anchoring strategy and surgical access. (D) The 3D reconstruction provides an integrated spatial assessment, enabling precise localization and facilitating interdisciplinary planning between the orthodontist and oral surgeon. Image courtesy of Nebi Cemeta.
CBCT imaging also enables 3D modeling and treatment simulation, supporting precise planning for clear aligners, bracket placement, and wire adjustments. These tools help to detect issues such as root resorption or bone loss, and enable timely modifications to the treatment plan. In addition, AI-driven technologies improve diagnostic precision by automating measurements, identifying cephalometric landmarks, and generating personalized treatment strategies, streamlining the planning process and enhancing clinical outcomes [36].
5.2.4. Forensic Dentistry
In forensic dentistry, radiographic imaging supports personal identification, bite mark analysis, and age estimation. Dental radiographs are uniquely individual and serve as reliable records in disaster victim identification and criminal investigations. CBCT enhances visualization of dental structures, restorations, and morphological features, thereby improving identification accuracy [37].
High-resolution imaging is also essential for bite mark comparisons in cases of abuse or assault, while radiographs documenting tooth development stages are widely used for age estimation [38]. The integration of AI further strengthens forensic evaluations by automating anomaly detection, enhancing reproducibility, and accelerating data analysis, establishing it as a powerful asset in modern forensic science [39]. However, standardized validation protocols and cross-jurisdictional comparisons are currently lacking, making broader forensic integration premature.
5.3. Protocol Optimization in Surgical Imaging
Advances in imaging technologies have significantly reshaped how dental surgeries are planned, executed, and monitored. Protocol optimization across the preoperative, intraoperative, and postoperative phases ensures safer, more precise interventions and better patient outcomes.
Preoperative Planning: In the early planning phase, high-resolution imaging technologies, particularly CBCT, are essential. CBCT provides detailed, three-dimensional views of bone density, nerve pathways, and vital anatomical landmarks. This information is critical for preparing for procedures such as dental implant placement, sinus augmentation, and periodontal surgeries. Moreover, CBCT data support the design of personalized surgical guides, which help clinicians predetermine the depth, angle, and positioning of instruments, thus reducing the risk of intraoperative complications [40]. The integration of CBCT with virtual treatment planning software adds another layer of precision. These systems enable step-by-step simulations of the surgical procedure, improving accuracy and reducing the likelihood of unexpected complications during surgery. Such virtual planning tools contribute to a patient-specific, precision-based approach, enhancing the overall safety and effectiveness of surgical interventions [41].
Intraoperative Navigation: During surgery, real-time imaging and navigation technologies further enhance clinical performance. Tools such as AR and 3D visual overlays allow pre-planned surgical pathways and guides to be projected directly onto the operative field. This dynamic feedback enables clinicians to make fine adjustments to instrument positioning, angulation, and depth, particularly useful in complex or minimally invasive procedures like guided implant placements, sinus lifts, or apical surgeries [42]. In addition, intraoperative CBCT provides immediate imaging feedback. It allows surgeons to verify the placement of implants or the extent of bone modifications while the procedure is still ongoing. This real-time validation supports in-procedure corrections, reducing surgical time, minimizing the risk of complications, and increasing accuracy, especially in anatomically challenging areas.
Postoperative Monitoring: Following surgery, postoperative imaging is important to evaluate healing, detect complications early, and monitor treatment success over time. Both digital radiography and CBCT are effective for follow-up assessments, offering high-detail imaging with relatively low radiation exposure. These modalities help clinicians track implant osseointegration, bone graft integration, and prosthetic stability. Furthermore, serial imaging allows for early detection of issues such as peri-implantitis, infection, or mechanical failures. This proactive approach enables timely intervention and helps prevent long-term complications. Objective postoperative monitoring not only supports clinical decision-making but also enhances the evidence base for future care strategies, contributing to the overall success of surgical outcomes.
Across surgical applications, CBCT remains the cornerstone of preoperative planning, whereas AI-enhanced intraoperative guidance is still in development. AR-based overlays show promise in enhancing spatial orientation during complex procedures but require more controlled validation in clinical environments.
6. The Digital Frontier: AR/VR Applications in Dental Surgery and Education
AR and VR are becoming valuable tools in dental education and surgical training. VR, in particular, offers a fully realistic experience where students and professionals can practice complex dental procedures in a risk-free environment [43,44]. These simulations allow for repeated practice, real-time feedback, and skill development without involving real patients. While VR-trained students show improved procedural accuracy, the strength of evidence varies. For instance, a randomized study with 42 dental students reported significant skill improvement using a haptic VR simulator (p < 0.05), but larger trials with long-term follow-up are scarce [45]. Similarly, AR studies often rely on observational data, limiting the ability to draw causal inferences.
AR enhances real-world environments by overlaying digital elements, such as anatomical markers or surgical guides, directly onto the operating field. This technology helps users understand space better and navigate in real time, which is especially useful in precise procedures like dental implants, jaw surgery, and complex orthodontic interventions [46,47]. Early studies show that AR may enhance learning outcomes in anatomy teaching and procedural planning, but stronger evidence is still needed [48].
Beyond individual learning, AR and VR are also enhancing teamwork in dental care through a broader approach known as Extended Reality (XR) [49]. XR encompasses AR, VR, and MR. These technologies enable remote consultations, real-time mentoring, and treatment planning with input from multiple specialists, even from different locations [50]. Integrating biosensors and eye-tracking systems further boosts interactivity by providing real-time feedback and tracking users’ physical responses, which supports both learning simulations and clinical applications [51,52,53].
However, several challenges make it difficult to widely use immersive technologies in dentistry. These include high costs, a lack of clear training standards, technical issues such as calibration, and concerns about data security. There are also not enough long-term studies comparing AR/VR with traditional training. Even with these challenges, the future of immersive technology in dentistry looks promising. As AR/VR systems continue to improve, they could transform the way dentists learn, diagnose, and treat patients, making procedures more accurate and more personalized. New tools like AI-powered simulations, real-time virtual guidance, and intelligent feedback systems could help make dental care faster, more accurate, and more accessible.
7. Limitations and Challenges in AI Integration
Despite the growing enthusiasm for AI in dental radiology, its widespread integration into clinical practice faces several technological, ethical, and operational barriers. These limitations can reduce accuracy, accessibility, and clinician trust in AI systems. The following Table 1 summarizes the most significant limitations and integration challenges, as identified in the current literature, and categorizes them for easier interpretation.

Table 1.
Main limitations and challenges in the integration of AI in dental imaging.
Deep learning systems often lack transparency, making it difficult to interpret or justify their decisions, an issue that raises significant concerns in clinical settings. To address these risks, including automation bias and the black-box nature of AI, several regulatory and ethical frameworks have been introduced. The European Union’s Artificial Intelligence Act (2021), for example, proposes a risk-based approach that requires transparency, human surveillance, and stability in healthcare AI applications [59]. Similarly, the U.S. Food and Drug Administration (FDA) has developed guidelines under its Software as a Medical Device (SaMD) framework, emphasizing quality assurance, validation, and continuous monitoring of AI tools [60,61]. These initiatives aim to safeguard patient safety and ensure accountability across the AI lifecycle.
Despite these efforts, implementation remains inconsistent, and widespread clinical adoption hinges on the availability of validated, interoperable systems and robust regulatory enforcement. This lack of uniformity introduces medico-legal and decision-making challenges, particularly in high-stakes diagnostic scenarios. For instance, convolutional neural networks (CNNs), despite their high diagnostic accuracy, operate through abstract feature extraction layers that are not easily interpretable by clinicians. In dental imaging, CNNs have demonstrated strong performance in detecting periapical lesions and periodontal bone loss; yet the reasoning behind specific outputs often remains opaque. This ambiguity hinders validity efforts and can decrease clinical trust, especially when treatment decisions or legal responsibilities demand clear explanations. Therefore, advancing explainable AI (XAI) models and implementing transparency protocols are critical steps toward responsible and effective clinical integration [61,62,64].
Addressing these multifaceted issues requires a multidisciplinary approach that incorporates rigorous validation trials, diverse training datasets, strong regulatory oversight, and continued clinician education.
8. Future Perspectives
The future of dental imaging is ready to significantly improve clinical practice by making diagnostics more accurate, efficient, and accessible globally. While emerging technologies promise broad advancements, their global accessibility remains limited due to cost and infrastructure barriers. A principal direction is the development of real-time, AI-based feedback systems designed to assist clinicians during procedures. These systems can continuously process live imaging data, identify anomalies, refine scan settings, and support decision-making in the moment. Their integration into clinical workflows can potentially improve operations and reduce reliance on post-procedural diagnostics [65].
Another transformative direction is the combination of multimodal technologies, particularly the incorporation of AR, VR, and 3D modeling into routine dental procedures. These tools are expected to become the standard for surgical planning, patient education, and clinical training. As AR and VR systems evolve to be more comprehensive, they will increase surgical accuracy, promote experiential learning in education, and improve communication between clinicians and patients. In parallel, 3D printing, enabled by high-resolution imaging, will continue to advance, enabling the rapid and personalized production of surgical guides, prostheses, and anatomical models to individual patient scans [43,66,67].
Equitable access to these innovations remains a priority. The development of affordable, mobile, and AI-enabled diagnostic tools is essential for reducing irregularities in access to oral healthcare. These technologies can provide reliable, high-quality diagnostics to underserved and remote communities, contributing to greater global oral health equity [68].
To ensure the responsible and lasting impact of these innovations, collaboration among researchers, clinicians, engineers, and policymakers is essential. Priorities include establishing ethical and legal frameworks, enhancing interoperability, and ensuring AI technologies are transparent, explainable, and safely integrated into practice. Long-term validation and real-world evidence will also be crucial for adoption and scalability. Ultimately, the convergence of AI, AR/VR, and digital imaging represents an important step toward smarter, more personalized dental care. When carefully applied, these tools can improve diagnostic accuracy, surgical outcomes, and the overall patient experience.
9. Conclusions
Dental imaging has evolved from traditional X-rays to advanced digital tools powered by AI, 3D imaging, and virtual technologies. These innovations have greatly improved the diagnostic accuracy, plan treatments, and surgical procedures, leading to better patient care. The integration of technologies such as CBCT, AI-assisted diagnostics, AR, VR, and 3D printing continues to enhance both clinician capabilities and patient experiences.
Although there are still challenges, such as high costs and the need for more real-world testing, the future looks promising. As technology continues to improve and become more widely available, dental imaging will become more accurate, less invasive, and more personalized for each patient.
Author Contributions
Conceptualization, A.M.; methodology, A.M. and G.H.; software, G.H.; formal analysis, G.H.; data curation, A.M. and G.H.; writing—original draft preparation, A.M. and G.H.; writing—review and editing, A.M. and G.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Shah, P.; Zalavadia, K. Recent Advances in Dental Imaging. Sch. J. Dent. Sci. 2021, 8, 184–188. [Google Scholar] [CrossRef]
- Katsumata, A. Deep learning and artificial intelligence in dental diagnostic imaging. Jpn. Dent. Sci. Rev. 2023, 59, 329–333. [Google Scholar] [CrossRef]
- Pauwels, R. History of Dental Radiography: Evolution of 2D and 3D Imaging Modalities. Med. Phys. Int. J. 2020, 3, 235–277. [Google Scholar]
- de Magalhães, A.A.; Santos, A.T. Advancements in Diagnostic Methods and Imaging Technologies in Dentistry: A Literature Review of Emerging Approaches. J. Clin. Med. 2025, 14, 1277. [Google Scholar] [CrossRef]
- Jayachandran, S. Digital Imaging in Dentistry: A review. Contemp. Clin. Dent. 2017, 8, 193–194. [Google Scholar] [CrossRef]
- Elkhateeb, S.M.; Aloyouny, A.Y.; Omer, M.M.S.; Mansour, S.M. Analysis of photostimulable phosphor image plate artifacts and their prevalence. World J. Clin. Cases 2022, 10, 437–447. [Google Scholar] [CrossRef]
- Martins, G.C.; Rocha, T.G.; de Lima Azeredo, T.; de Castro Domingos, A.; Visconti, M.A.; Villoria, E.M. Hand-held dental X-ray device: Attention to correct use. Imaging Sci. Dent. 2023, 53, 265–266. [Google Scholar] [CrossRef]
- Nitschke, J.; Schorn, L.; Holtmann, H.; Zeller, U.; Handschel, J.; Sonntag, D.; Lommen, J. Image quality of a portable X-ray device (Nomad Pro 2) compared to a wall-mounted device in intraoral radiography. Oral Radiol. 2021, 37, 224–230. [Google Scholar] [CrossRef]
- Kazimierczak, W.; Wajer, R.; Komisarek, O.; Dyszkiewicz-Konwińska, M.; Wajer, A.; Kazimierczak, N.; Janiszewska-Olszowska, J.; Serafin, Z. Evaluation of a Vendor-Agnostic Deep Learning Model for Noise Reduction and Image Quality Improvement in Dental CBCT. Diagnostics 2024, 14, 2410. [Google Scholar] [CrossRef]
- Baccher, S.; Gowdar, I.; Guruprasad, Y.; Solanki, R.; Medhi, R.; Shah, M.; Mehta, D. CBCT: A Comprehensive Overview of its Applications and Clinical Significance in Dentistry. J. Pharm. Bioallied Sci. 2024, 16, S1923–S1925. [Google Scholar] [CrossRef]
- Hora, B.; Varghese, A.; Patil, P.; Anbalagan, S.; Sagolsem, C.; Shaik, N. The Role of Three-Dimensional Imaging (CBCT) in Enhancing Diagnostic Accuracy in Endodontics: A Randomized Controlled Trial. J. Pharm. Bioallied Sci. 2024, 16, S874–S876. [Google Scholar] [CrossRef]
- Vasegh, Z.; Safi, Y.; Azar, M.S.; Ahsaie, M.G.; Arianezhad, S.M. Assessment of bony changes in temporomandibular joint in patients using cone beam computed tomography—A cross sectional study. Head Face Med. 2023, 19, 47. [Google Scholar] [CrossRef]
- Weiss, R., 2nd; Read-Fuller, A. Cone Beam Computed Tomography in Oral and Maxillofacial Surgery: An Evidence-Based Review. Dent. J. 2019, 7, 52. [Google Scholar] [CrossRef]
- Joachim, M.V.; Miloro, M. The Evolution of Virtual Surgical Planning in Craniomaxillofacial Surgery: A Comprehensive Review. J. Oral Maxillofac. Surg. 2025, 83, 294–306. [Google Scholar] [CrossRef]
- Srinivas-Rao, S.; Cao, J.; Marin, D.; Kambadakone, A. Dual-Energy Computed Tomography to Photon Counting Computed Tomography: Emerging Technological Innovations. Radiol. Clin. N. Am. 2023, 61, 933–944. [Google Scholar] [CrossRef]
- Zanon, C.; Pepe, A.; Cademartiri, F.; Bini, C.; Maffei, E.; Quaia, E.; Stellini, E.; Di Fiore, A. Potential Benefits of Photon-Counting CT in Dental Imaging: A Narrative Review. J. Clin. Med. 2024, 13, 2436. [Google Scholar] [CrossRef]
- Dogra, S.; Shekhrajka, N.; Moonis, G. A Review of Applications of Photon-Counting Computed Tomography in Head and Neck Imaging. Br. J. Radiol. 2024, tqae226. [Google Scholar] [CrossRef]
- Shah, N.; Bansal, N.; Logani, A. Recent advances in imaging technologies in dentistry. World J. Radiol. 2014, 6, 794–807. [Google Scholar] [CrossRef]
- Kaasalainen, T.; Uusitalo, A.; Mäki, M. Dental cone beam CT: An updated review. Phys. Med. 2022, 88, 193–217. [Google Scholar] [CrossRef]
- Miragall, M.F.; Knoedler, S.; Kauke-Navarro, M.; Saadoun, R.; Grabenhorst, A.; Grill, F.D.; Ritschl, L.M.; Fichter, A.M.; Safi, A.-F.; Knoedler, L. Face the Future—Artificial Intelligence in Oral and Maxillofacial Surgery. J. Clin. Med. 2023, 12, 6843. [Google Scholar] [CrossRef]
- Tsapaki, V. Radiation Protection in Dental Radiology—Recent Advances and Future Directions. Phys. Med. 2017, 44, 222–226. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Zhang, Y.; Kalra, M.K.; Lin, F.; Chen, Y.; Liao, P.; Zhou, J.; Wang, G. Low-Dose CT With a Residual Encoder-Decoder Convolutional Neural Network. IEEE Trans. Med. Imaging 2017, 36, 2524–2535. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Hao, J.; Lin, H.; Pan, W.; Yang, J.; Feng, Y.; Wang, G.; Li, J.; Jin, Z.; Zhao, Z.; et al. Deep Learning-Enabled 3D Multimodal Fusion of Cone-Beam CT and Intraoral Mesh Scans for Clinically Applicable Tooth-Bone Reconstruction. Patterns 2023, 4, 100825. [Google Scholar] [CrossRef]
- Shujaat, S.; Riaz, M.; Jacobs, R. Synergy between artificial intelligence and precision medicine for computer-assisted oral and maxillofacial surgical planning. Clin. Oral Investig. 2023, 27, 897–906. [Google Scholar] [CrossRef] [PubMed]
- Kot, W.Y.; Au Yeung, S.Y.; Leung, Y.Y.; Leung, P.H.; Yang, W.F. Evolution of deep learning tooth segmentation from CT/CBCT images: A systematic review and meta-analysis. BMC Oral Health 2025, 25, 800. [Google Scholar] [CrossRef]
- Vial, A.; Stirling, D.; Field, M.; Ros, M.; Ritz, C.; Carolan, M.; Holloway, L.; Miller, A.A. The Role of Deep Learning and Radiomic Feature Extraction in Cancer-Specific Predictive Modelling: A Review. Transl. Cancer Res. 2018, 7, 803–816. [Google Scholar] [CrossRef]
- Hung, K.F.; Ai, Q.Y.H.; Wong, L.M.; Yeung, A.W.K.; Li, D.T.S.; Leung, Y.Y. Current Applications of Deep Learning and Radiomics on CT and CBCT for Maxillofacial Diseases. Diagnostics 2022, 13, 110. [Google Scholar] [CrossRef]
- Mayerhoefer, M.E.; Materka, A.; Langs, G.; Häggström, I.; Szczypiński, P.; Gibbs, P.; Cook, G. Introduction to Radiomics. J. Nucl. Med. 2020, 61, 488–495. [Google Scholar] [CrossRef]
- Tandon, D.; Rajawat, J. Present and Future of Artificial Intelligence in Dentistry. J. Oral Biol. Craniofacial Res. 2020, 10, 391–396. [Google Scholar] [CrossRef]
- Iruvuri, A.G.; Miryala, G.; Khan, Y.; Ramalingam, N.T.; Sevugaperumal, B.; Soman, M.; Padmanabhan, A. Revolutionizing Dental Imaging: A Comprehensive Study on the Integration of Artificial Intelligence in Dental and Maxillofacial Radiology. Cureus 2023, 15, e50292. [Google Scholar] [CrossRef]
- Ríos-Osorio, N.; Quijano-Guauque, S.; Briñez-Rodríguez, S.; Velasco-Flechas, G.; Muñoz-Solís, A.; Chávez, C.; Fernandez-Grisales, R. Cone-Beam Computed Tomography in Endodontics: From the Specific Technical Considerations of Acquisition Parameters and Interpretation to Advanced Clinical Applications. Restor. Dent. Endod. 2023, 49, e1. [Google Scholar] [CrossRef] [PubMed]
- Schloss, T.; Sonntag, D.; Kohli, M.R.; Setzer, F.C. A Comparison of 2- and 3-Dimensional Healing Assessment after Endodontic Surgery Using Cone-Beam Computed Tomographic Volumes or Periapical Radiographs. J. Endod. 2017, 43, 1072–1079. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, B.; Liu, Y.Y.; Luo, Y.; Wu, Y.; Xiang, L.; Yang, X.; Qu, Y.; Tian, T.; Man, Y. Recent Advances in Digital Technology in Implant Dentistry. J. Dent. Res. 2024, 103, 787–799. [Google Scholar] [CrossRef]
- Bianchi, J.; Mendonca, G.; Gillot, M.; Oh, H.; Park, J.; Turkestani, N.A.; Gurgel, M.; Cevidanes, L. Three-Dimensional Digital Applications for Implant Space Planning in Orthodontics: A Narrative Review. J. World Fed. Orthod. 2022, 11, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Polizzi, A.; Serra, S.; Leonardi, R. Use of CBCT in Orthodontics: A Scoping Review. J. Clin. Med. 2024, 13, 6941. [Google Scholar] [CrossRef]
- Pandey, R.; Kamble, R.; Kanani, H. Revolutionizing Smiles: Advancing Orthodontics Through Digital Innovation. Cureus 2024, 16, e64086. [Google Scholar] [CrossRef]
- Perkins, H.; Chiam, T.L.; Forrest, A.; Higgins, D. 3D Dental Images in Forensic Odontology: A Scoping Review of Superimposition Approaches Utilizing 3D Imaging. Forensic Imaging 2025, 40, 200622. [Google Scholar] [CrossRef]
- Christoloukas, N.; Mitsea, A.; Rontogianni, A.; Papadakis, E.; Angelopoulos, C. Evaluation of Bitemark Analysis’s Potential Application in Forensic Identification: A Systematic Review. Diagnostics 2024, 14, 1180. [Google Scholar] [CrossRef]
- Thurzo, A.; Kosnáčová, H.S.; Kurilová, V.; Kosmeľ, S.; Beňuš, R.; Moravanský, N.; Kováč, P.; Kuracinová, K.M.; Palkovič, M.; Varga, I. Use of Advanced Artificial Intelligence in Forensic Medicine, Forensic Anthropology and Clinical Anatomy. Healthcare 2021, 9, 1545. [Google Scholar] [CrossRef]
- Saini, R.S.; Bavabeedu, S.S.; Quadri, S.A.; Gurumurthy, V.; Kanji, M.A.; Kuruniyan, M.S.; Binduhayyim, R.I.H.; Avetisyan, A.; Heboyan, A. Impact of 3D Imaging Techniques and Virtual Patients on the Accuracy of Planning and Surgical Placement of Dental Implants: A Systematic Review. Digit. Health 2024, 10, 20552076241253550. [Google Scholar] [CrossRef]
- Yepes, J.F.; Al-Sabbagh, M. Use of cone-beam computed tomography in early detection of implant failure. Dent. Clin. N. Am. 2015, 59, 41–56. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.; Ma, L.; Zhang, B.; Fan, Y.; Qu, X.; Zhang, X.; Liao, H. Evaluation of the 3D Augmented Reality-Guided Intraoperative Positioning of Dental Implants in Edentulous Mandibular Models. Int. J. Oral Maxillofac. Implant. 2018, 33, 1219–1228. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.Y.; Chen, T.C.; Lin, C.J.; Huang, C.C.; Tsai, Y.H.; Tsai, Y.L.; Wang, C.Y. The Use of Augmented Reality (AR) and Virtual Reality (VR) in Dental Surgery Education and Practice: A Narrative Review. J. Dent. Sci. 2024, 19, S91–S101. [Google Scholar] [CrossRef] [PubMed]
- Fahim, S.; Maqsood, A.; Das, G.; Ahmed, N.; Saquib, S.; Lal, A.; Khan, A.A.G.; Alam, M.K. Augmented Reality and Virtual Reality in Dentistry: Highlights from the Current Research. Appl. Sci. 2022, 12, 3719. [Google Scholar] [CrossRef]
- Al-Saud, L.M.; Mushtaq, F.; Allsop, M.J.; Culmer, P.C.; Mirghani, I.; Yates, E.; Keeling, A.; Mon-Williams, M.A.; Manogue, M. Feedback and motor skill acquisition using a haptic dental simulator. Eur. J. Dent. Educ. 2017, 21, 240–247. [Google Scholar] [CrossRef]
- Mosch, R.; Alevizakos, V.; Ströbele, D.A.; Schiller, M.; von See, C. Exploring augmented reality for dental implant surgery: Feasibility of using smartphones as navigation tools. Clin. Exp. Dent. Res. 2025, 11, e70110. [Google Scholar] [CrossRef]
- Ayoub, A.; Pulijala, Y. The Application of Virtual Reality and Augmented Reality in Oral & Maxillofacial Surgery. BMC Oral Health 2019, 19, 238. [Google Scholar] [CrossRef]
- García-Robles, P.; Cortés-Pérez, I.; Nieto-Escámez, F.A.; García-López, H.; Obrero-Gaitán, E.; Osuna-Pérez, M.C. Immersive virtual reality and augmented reality in anatomy education: A systematic review and meta-analysis. Anat. Sci. Educ. 2024, 17, 514–528. [Google Scholar] [CrossRef]
- Reiners, D.; Davahli, M.R.; Karwowski, W.; Cruz-Neira, C. The Combination of Artificial Intelligence and Extended Reality: A Systematic Review. Front. Virtual Real. 2021, 2, 721933. [Google Scholar] [CrossRef]
- Dinh, A.; Yin, A.L.; Estrin, D.; Greenwald, P.; Fortenko, A. Augmented Reality in Real-time Telemedicine and Telementoring: Scoping Review. JMIR mHealth uHealth 2023, 11, e45464. [Google Scholar] [CrossRef]
- Moreno Arjonilla, J.; López Ruiz, A.; Jiménez, J.R.; Aguilera, J.; Jurado, J.M. Eye-tracking on Virtual Reality: A Survey. Virtual Real. 2024, 28, 38. [Google Scholar] [CrossRef]
- Aliwi, I.; Schot, V.; Carrabba, M.; Duong, P.; Shievano, S.; Caputo, M.; Wray, J.; de Vecchi, A.; Biglino, G. The Role of Immersive Virtual Reality and Augmented Reality in Medical Communication: A Scoping Review. J. Patient Exp. 2023, 10, 23743735231171562. [Google Scholar] [CrossRef] [PubMed]
- Lacoche, J.; Villain, E.; Foulonneau, A. Evaluating Usability and User Experience of AR Applications in VR Simulation. Front. Virtual Real. 2022, 3, 881318. [Google Scholar] [CrossRef]
- Tai, C.-J.; Tatakis, D.N.; Chien, H.H. The Applications and Limitations of Advanced (3-Dimensional) Radiographic Imaging Techniques. In Clinical Maxillary Sinus Elevation Surgery, 1st ed.; Kao, D.W.K., Ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2014; pp. 31–56. [Google Scholar] [CrossRef]
- Ghaffari, M.; Zhu, Y.; Shrestha, A. A Review of Advancements of Artificial Intelligence in Dentistry. Dent. Rev. 2024, 4, 100081. [Google Scholar] [CrossRef]
- Schwendicke, F.; Samek, W.; Krois, J. Artificial Intelligence in Dentistry: Chances and Challenges. J. Dent. Res. 2020, 99, 769–774. [Google Scholar] [CrossRef]
- Schwendicke, F.; Singh, T.; Lee, J.-H.; Gaudin, R.; Chaurasia, A.; Wiegand, T.; Uribe, S.; Krois, J. Artificial intelligence in dental research: Checklist for authors, reviewers, readers. J. Dent. 2021, 107, 103610. [Google Scholar] [CrossRef]
- Ducret, M.; Mörch, C.M. Focus on Artificial Intelligence Ethics in Dentistry. J. Dent. Sci. 2023, 18, 1409–1410. [Google Scholar] [CrossRef]
- European Commission. Proposal for a Regulation of the European Parliament and of the Council Laying Down Harmonised Rules on Artificial Intelligence (Artificial Intelligence Act). 2021. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A52021PC0206 (accessed on 21 April 2021).
- Khandare, L.; Sreekantha, D.K.; Sairam, K. A Study on Encryption Techniques to Protect the Patient Privacy in Health Care Systems. In Proceedings of the 2019 Innovations in Power and Advanced Computing Technologies (i-PACT), Vellore, India, 22–23 March 2019; IEEE: Piscataway, NJ, USA, 2019; pp. 1–5. [Google Scholar]
- FDA. Artificial Intelligence and Machine Learning (AI/ML)-Based Software as a Medical Device (SaMD) Action Plan; U.S. Food and Drug Administration: Silver Spring, MD, USA, 2022. Available online: https://www.fda.gov/media/145022/download (accessed on 25 March 2025).
- Yu, K.H.; Beam, A.L.; Kohane, I.S. Artificial intelligence in healthcare. Nat. Biomed. Eng. 2018, 2, 719–731. [Google Scholar] [CrossRef]
- Albano, D.; Galiano, V.; Basile, M.; Di Luca, F.; Gitto, S.; Messina, C.; Cagetti, M.G.; Del Fabbro, M.; Tartaglia, G.M.; Sconfienza, L.M. Artificial intelligence for radiographic imaging detection of caries lesions: A systematic review. BMC Oral Health 2024, 24, 274. [Google Scholar] [CrossRef]
- Jiang, F.; Jiang, Y.; Zhi, H.; Dong, Y.; Li, H.; Ma, S.; Wang, Y.; Dong, Q.; Shen, H.; Wang, Y. Artificial intelligence in healthcare: Past, present and future. Stroke Vasc. Neurol. 2017, 2, 230–243. [Google Scholar] [CrossRef]
- Farhadi Nia, M.; Ahmadi, M.; Irankhah, E. Transforming Dental Diagnostics with Artificial Intelligence: Advanced Integration of ChatGPT and Large Language Models for Patient Care. Front. Dent. Med. 2025, 5, 1456208. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.Y.; Kim, S.K.; Heo, S.J.; Koak, J.Y.; Kim, J.G. Dimensional Accuracy of Dental Models for Three-Unit Prostheses Fabricated by Various 3D Printing Technologies. Materials 2021, 14, 1550. [Google Scholar] [CrossRef] [PubMed]
- Fidvi, S.; Holder, J.; Li, H.; Parnes, G.J.; Shamir, S.B.; Wake, N. Advanced 3D Visualization and 3D Printing in Radiology. Adv. Exp. Med. Biol. 2023, 1406, 103–138. [Google Scholar] [CrossRef] [PubMed]
- Elani, H.W.; Giannobile, W.V. Harnessing Artificial Intelligence to Address Oral Health Disparities. JAMA Health Forum 2024, 5, e240642. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).