Abstract
This systematic review investigates the effectiveness of virtual reality as a tool in the treatment of eating disorders, either alone or in combination with other therapies. The limitations of traditional therapies, along with the high prevalence of eating disorders, have driven research into the use of virtual reality techniques as a new approach to treatment. The review includes studies published between November 2021 and February 2025, focusing on virtual reality-based interventions for anorexia nervosa, bulimia nervosa, binge eating disorder, and body image disturbances. A total of 228 articles were screened, with eight meeting the inclusion criteria. The studies show that virtual reality interventions, particularly when combined with other therapeutic techniques, can significantly improve psychological and behavioral factors related to eating disorders. Virtual reality exposure and inhibitory control training were the main interventions. The results indicate that virtual reality exposure is effective in reducing body concerns, food anxiety, and attentional bias, while inhibitory control training shows mixed results in binge eating disorder treatment. Despite the promising findings, limitations such as small sample sizes and lack of follow-up highlight the need for further research. Future studies should aim to include larger, more diverse samples and explore the long-term effectiveness of the interventions.
1. Introduction
In recent years, technological advancements have gained increasing relevance across various fields, including psychology. These innovations have introduced new forms of treatment and therapy, while also enhancing existing approaches [1]. Among these emerging technologies, virtual reality (VR) has been progressively integrated into psychological practice. VR enables the creation of immersive environments with which individuals can interact in a highly ecologically valid manner, while maintaining a high level of control [2]. VR not only has the potential to enhance therapeutic outcomes but also offers insights into the nature of psychological disorders and the factors contributing to them, facilitating more personalized and targeted treatment interventions.
Building on this potential, VR offers users immersive three-dimensional environments that address limitations of traditional exposure therapies, such as difficulties in recreating certain scenarios and reliance on patients’ imagination. VR enables controlled and repeatable exposure, allowing therapists to adjust difficulty levels to suit individual patients’ needs, which can enhance engagement and acceptance of treatment [2,3]. Immersion and interaction are important factors that contribute to the sense of presence—the feeling of “being there” within the virtual environment—which is essential for the effectiveness of VR interventions [4]. This heightened sense of presence allows patients to engage more deeply with therapeutic exercises while remaining in a safe and supervised setting. In the context of eating disorders (EDs), VR is emerging as a promising tool by providing personalized and immersive experiences that can be tailored to address specific triggers and symptoms, making the therapy more engaging and effective [5]. Additionally, VR can augment accessibility by reducing costs and barriers to treatment, potentially reaching a wider range of patients, as it does not always require the physical presence of both therapist and patient [6].
Recent data indicate that between 5.5% and 17.9% of adolescent and young women and between 0.6% and 2.4% of adolescent and young men in Western countries have experienced EDs [7]. These disorders pose a significant challenge for professionals due to their complexity and multifactorial nature. Anorexia nervosa (AN), bulimia nervosa (BN), and binge eating disorder (BED) are the main EDs [8]. EDs are associated with high mortality rates, including suicide, and often co-occur with other health conditions and psychological disorders [9,10]. Significantly, EDs often manifest during adolescence, a critical period for growth and development, potentially leading to growth issues and impeding proper development, resulting in long-term repercussions for the patient’s life [11,12]. Various therapies are employed in the treatment of EDs, such as cognitive behavioral therapy (CBT), exposure therapy, and family-based therapy, among others. CBT is one of the most widely used treatments, being particularly effective for BN and BED, with effectiveness rates ranging from 40% to 60% [13,14]. Relapse rates can be significant, often exceeding 30%. However, when combined with other interventions—like nutritional counseling or pharmacotherapy—treatment outcomes improve, with remission rates increasing and relapse rates decreasing [14,15]. Family-based therapy has shown significant effectiveness, especially in adolescents with anorexia nervosa, by actively involving family members in the treatment process to support recovery and address dysfunctional family dynamics [16]. Table 1 provides a description of the three most common EDs.

Table 1.
Brief description of three most common EDs.
VR, either in combination with other therapies or as a standalone intervention, has emerged as a promising tool to enhance the efficacy of ED treatments. The most recent review in the field of ED and VR therapies was conducted by Ciążyńska and Maciaszek [6]. This review categorized various VR interventions used in the treatment of EDs. One category involves VR-based body exposure therapy aimed at reducing body dissatisfaction and related emotional responses, which has shown effectiveness in improving body image disturbances [17,18]. In VR body exposure therapy, a generic avatar with a similar complexion to the participant or an avatar with the exact silhouette of the participant is often used. The participant can see this avatar in the third person, for example, through a mirror [17,18]. Another category focuses on VR cue exposure therapy, which has demonstrated effectiveness in reducing binge eating and purging episodes among patients with BN and BED, with sustained positive outcomes observed even at six-month follow-ups [19,20]. VR cue exposure therapy typically involves presenting patients with relevant foods and environments, allowing the participant to manipulate the food [19,20]. Additionally, VR interventions have been developed to support treatments like Acceptance and Commitment Therapy, enhancing their effectiveness [21]. This therapy includes a VR environment where both the therapist and the patient are present. The therapist guides the patient through various tasks and games designed to improve the communication of thoughts and feelings and to focus on the most important aspect of their lives [21]. VR has also been employed in inhibitory control training (ICT) to reduce binge eating episodes, showing promising results [22]. In ICT, a table with different colored plates containing vegetables or binge food is used. The participant must follow the instructions to reach for and grasp the required food or withhold a response [22]. Regarding the target population, VR-based therapies may be particularly beneficial for adolescents and young adults, who are generally more familiar and comfortable with technology. They also have a lower probability of experiencing virtual sickness and a greater likelihood of having used this technology before—usually related to games—thus having a positive perception of this technology, which facilitates its adaptation to treatments [23]. ED are rising in this population, and they are more prone to use social media and be exposed to harmful ED-promoting content, such as weight loss trends and extreme fitness or thinness [24]. Patients with severe levels of EDs who have not responded to traditional treatments may also benefit from these techniques. In addition to the advantages mentioned previously, a more specific example in severe cases of anorexia nervosa is that VR can provide a controlled environment that allows patients to confront fears related to food and body image without the risks associated with direct exposure [6].
While VR has shown significant promise in treating EDs, there is a pressing need for further research to strengthen these findings. Conducting studies with larger participant groups and longer follow-up periods will help verify the long-term effectiveness of VR-based interventions and enhance the quality of the techniques used. Additionally, the rapid advancements in VR technology highlight the necessity for up-to-date research. As software and hardware continue to evolve, relying on older studies may lead to conclusions based on outdated technology. Therefore, current and ongoing investigations are essential to fully capitalize on the potential of VR in ED treatment and ensure that therapeutic approaches remain relevant and effective. The review by Ciążyńska and Maciaszek [6] provides a broad overview of the potential applications of VR treatment, as well as in the assessment and evaluation of relevant EDs. However, although they describe various approaches, they do not explore each one in depth or assess their actual effectiveness, either as standalone interventions or in combination with other treatments. Additionally, they include studies that lack empirical data to substantiate the efficacy of the treatment. The present review aims to evaluate the available evidence from November 2021 up to February 2025 on virtual VR-based treatments as therapeutic tools for EDs. The goal is to analyze the current state to discuss the potential of VR therapies as alternatives or complements to usual treatments. Finally, future research directions will be proposed to overcome the current limitations and explore new therapeutic applications.
2. Materials and Methods
2.1. Eligibility Criteria
Studies were included in the present review if they met all of the following criteria. They were published between November 2021—the cutoff date for articles included in the review by Ciążyńska and Maciaszek [6]—and February 2025, and they incorporated VR-based interventions in the treatment of EDs. The participant samples consisted of individuals diagnosed with EDs according to DSM-5 criteria, such as AN, BN, BED, or individuals exhibiting significant body image disturbances associated with EDs. Additionally, the studies provided results on the effectiveness of VR-based interventions, including changes in eating behaviors, body perceptions, and other psychologically relevant outcomes. Studies were excluded from the review if they were not written in English or Spanish; if they focused on technologies other than VR, such as augmented reality, the “metaverse”, or virtual therapies without VR elements; if they were reviews, meta-analyses, opinion letters, or conference papers; if they were not focused on treatment interventions (e.g., assessment studies) or were unrelated to EDs; if they were not conducted with human participants; or if they did not include empirical data on the effects of VR interventions.
2.2. Search Strategies and Data Extraction
To identify relevant studies, we conducted a comprehensive search of the databases PsycNet, Web of Science, PubMed, Scopus, and EBSCOhost. Given EDs have a multidisciplinary focus—encompassing general medicine, psychology, and psychiatry—it is necessary to use relevant multidisciplinary databases to cover this field comprehensively. The databases used in this systematic review are considered principal sources for a properly systematic search, covering a wide range of articles and years and offering a refine search system [25]. One author performed the search using the following terms: (“virtual reality” AND (“treatment” OR therap*” OR “program” OR “interv*”) AND (“eating disorder” OR “body image”) NOT (“review” OR “meta-analysis”). The literature search was conducted on 9 July 2024 and updated on 17 February 2025 and 7 March 2025. We adhered to the PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-Analyses; [26]) to systematically identify and analyze the available scientific literature. Data extraction was carried out using a standardized table that included the first author and year of publication, a description of the sample, details of the study design and intervention, questionnaires used, behavioral and physiological measures collected, and the main results with their effect size. Detailed data on the study variables can be found in the Supplementary Table S1.
2.3. Quality Analyses of the Studies
To evaluate the risk of bias in the included studies, two authors independently used the latest version of the Cochrane Collaboration’s Risk-of-Bias tool (RoB 2.0; [27]). In the cases where the two authors reached different conclusions regarding the overall level of risk or domain level of an article, they reviewed the point, discussed the pros and cons, and reached a joint final conclusion. RoB 2.0 assesses five specific domains and provides an overall risk rating at three levels: low, some concerns, or high. A study is deemed to have a low risk of bias if it scores low across all five domains, while it is rated as having some concerns if at least one domain raises concerns. A high risk of bias is assigned when there is a high risk in at least one domain or multiple concerns that significantly reduce confidence in the results. RoB 2.0 provides questions for each section that, when answered, offer insight into the level of concern. The domains evaluated include bias from the randomization process, deviations from intended interventions, missing outcome data, measurement of outcomes, and selection of reported results.
3. Results
3.1. Articles Description
The search and screening process is summarized in Figure 1. Initially, 228 articles were identified across five databases: 44 in Scopus, 23 in PsycNet, 60 in Web of Science, 29 in PubMed, and 72 in EBSCOhost. After eliminating duplicates and irrelevant records, 73 articles remained. The selection process involved reviewing titles, abstracts, and full texts. Following the title and abstract screening, 21 articles were retained. A thorough full-text review led to the exclusion of 13 more articles: four did not use VR, two lacked empirical data, three were conference papers, and four were unrelated to ED treatment. The final sample comprised eight articles.
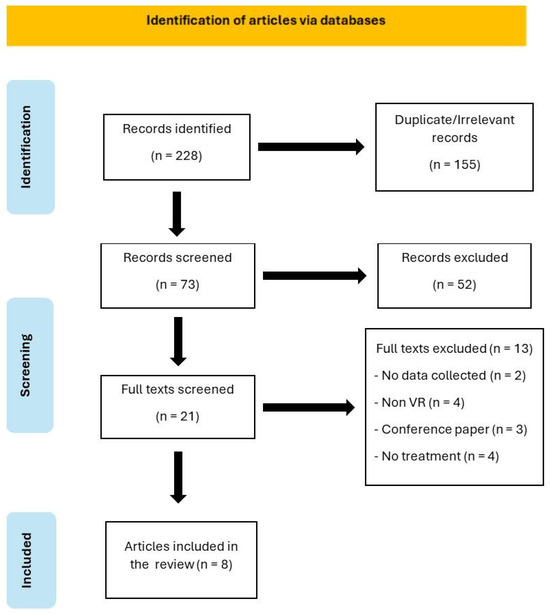
Figure 1.
PRISMA flowchart overview of the article selection process. Note: n = number, VR = virtual reality.
All the included articles focus on the treatment of ED using VR, with participants either diagnosed with EDs or healthy individuals selected based on personal characteristics that pose a risk for the onset or maintenance of EDs.
One of the articles included two separate studies [28]. Therefore, the following analysis is based on the nine studies rather than the eight articles included in the review. Among the studies, four involved multiple sessions, while five were single-session interventions. Table 2 presents a detailed summary of the articles included in this review.

Table 2.
Characteristics and main finding of the included studies.
Only two studies included follow-up periods, ranging from 1 to 12 months after the final intervention. Regarding the types of interventions, two main groups were identified: VR exposure and ICT. In the VR exposure group, five studies involved exposing the participants to virtual bodies, while two exposed the participants to relevant environments and stimuli. All these studies combined exposure with additional techniques. The second group consisted of two studies that used ICT. Figure 2 presents a graphical overview of the distribution of the studies and some of their key characteristics.
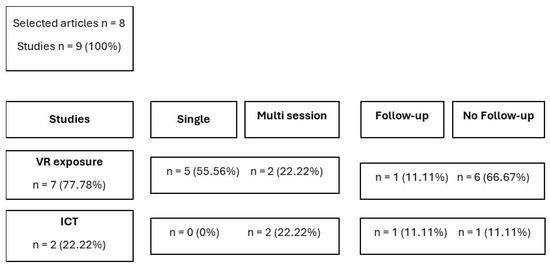
Figure 2.
Graphic overview of study type, number of sessions, and follow-up. Note: n = number, VR = virtual reality, ICT = inhibitory control training.
3.2. Quality Analyses
When assessing the quality of the studies using RoB 2.0, two studies were categorized as low risk, while seven were classified as having some concerns. Table 3 presents a detailed breakdown of the risk factors for each study, as outlined by RoB 2.0.

Table 3.
Risk of bias of the different studies included in the review.
The majority of the studies present some concerns in the randomization process [28,29,31,32,33,35]. The absence of a control group is the most common issue [28,29,31], followed by the absence of random allocation of participants due to the nature of the grouping variables [32,33]. Additionally, one study does not provide information on whether the groups had differences at baseline [35]. The study conducted by Manasse et al. [30] has some concerns in the selection of reported outcome, as the analyses chosen were not appropriate given the very low sample size of each group.
3.3. VR Exposure Intervention
Seven studies used VR exposure interventions combined with various techniques. In general, there is heterogeneity between the studies; the sample sizes vary between 20 to 145. Some studies used only one group, while others divided the sample into different comparison groups. Participants included those with AN, BN, and healthy individuals with attentional bias or ED-related concerns. There is also heterogeneity in the variables measured; the majority measured food or body concerns, and half measured behavioral variables related to attentional bias. Even when the same variable was measured, different questionnaires were used. For detailed measurements used in each study, consult Table 2 and Table S1.
Four of these studies, Study 2 [28] and [29,34,35], focused on populations with AN and BN, all involving women except the study by Natali et al. [34], which had a mixed sample with a female majority. These studies consistently showed that VR exposure significantly reduced body-related concerns and food anxiety—[28] Study 2 and [34,35], stabilized body mass index (BMI; [35]), and reduced weight-related attentional bias [29]. Ascione et al. [29] used a single session of VR body exposure within attentional bias modification training (ABMT)—attentional bias is defined as the propensity to provide more attention to a stimulus or information, usually disorder-relevant information, than other information. Attentional bias toward body areas associated with weight gain is a maintaining factor in ED and may also contribute to the development of ED in healthy women [36,37]. Ascione et al. found reductions in both attentional bias toward weight-related areas and body dissatisfaction, but without a control group. Behrens et al. (Study 2, [28]) used multiple VR body exposure sessions with educational sessions, also without a control group, reporting significant reductions in fear of gaining weight (FGW) per session but no cumulative session-to-session differences. Natali et al. [34] employed a single session of VR exposure to a kitchen environment, comparing three conditions: baseline, social support (another avatar), and positive mood (a pet). The positive mood group demonstrated less food-related anxiety than the baseline, which served as a control group. Sansoni et al. [35] compared VR-CBT to a control group, finding significant reductions in binge eating, purging episodes, body-related concerns, FGW, and a more stable BMI in the VR-CBT group.
The remaining three studies involved healthy women, either based on their baseline attentional bias toward body areas [32,33] or high concern about weight and shape (Study 1, [28]). Both Meschberger-Annweiler et al. [32] and Miquel-Nabau et al. [33] used single-session VR body exposure within an ABMT, showing that VR-ABMT effectively reduced attentional biases. Comparison groups were based on initial attentional bias. Behrens et al. (Study 1, [28]) used a single session of VR body exposure combined with psychoeducation but found no significant improvements, marking it as the only study without intervention-related changes. The researchers suggested that the absence of significant changes in this study was due to the brief 15 min exposure being less effective than longer exposure. However, there are other differences between Behrens et al.’s Study 1 and 2 not mentioned by the authors. In Study 1, the educational session occurred immediately before exposure and focused on refraining from avoidance behaviors. In Study 2, the session was held on a different day and provided information on maladaptive cycles of fear of weight gain and avoidance behaviors, helping the participants understand how exposure could improve their well-being. The time between the first session and the first exposure allowed participants to reflect on the information they had been given for longer, draw their own conclusions, and seek out more information if they wished.
3.4. VR-ICT Intervention
Two studies employed VR-ICT interventions [30,31], both targeting mixed-gender populations with BED. Due the few studies included, the heterogeneity between them is minor. Both use similar techniques and samples, although they use different behavioral measures, and Max et al. are more exhaustive with questionnaires. For a detailed measurement used in each study, consult Table 2 and Table S1. Manasse et al. [30] conducted multiple-session training involving four groups: two VR groups (VR-ICT and VR-sham) and two non-VR groups (non-VR-ICT and non-VR-sham). The results indicated a significant reduction in loss of control across all groups. Similarly, Max et al. [31] used a multi-session intervention and reported a significant decrease in general ED psychopathology and the frequency of BED episodes.
4. Discussion
This systematic review aimed to evaluate the effectiveness of VR as a treatment tool for ED, whether used alone or in combination with other therapies. It sought to update the information provided by the review of Ciążyńska and Maciaszek [6] by analyzing articles published since that review. The prior review concluded that VR-based therapies successfully elicit realistic responses to virtual environments. These interventions can be integrated with various treatments and show potential in reducing harmful ED-related characteristics while enhancing protective factors for patients. VR exposure interventions effectively help to reduce attentional bias toward specific body areas, body-related concerns, and food anxiety and help to stabilize BMI. VR-ICT interventions help to reduce loss of control, ED psychopathology, and the frequency of BED episodes. These variables have been shown to contribute to the cause and maintenance of eating disorders. Therefore, their reduction or control contributes to a better prognosis for patients and their recovery [29,30,31,34,35].
The studies included in this review highlight the effectiveness of VR in ED treatment, with most demonstrating positive outcomes and improvements in the participants. The use of VR in therapy has proven to be a valuable tool that warrants serious consideration. However, further research is needed to strengthen the evidence base for VR interventions. The following sections will discuss the advantages and limitations of the studies reviewed.
4.1. Effectiveness of VR Exposure Intervention
Five of the seven studies that used VR exposure demonstrated that combining VR with other therapies or techniques improves psychological and behavioral factors related to ED [29,32,33,34,35]. The remaining two studies [28] showed limited results with VR exposure interventions. Overall, these findings suggest that VR exposure is an effective technique in the treatment of AN and BN, as well as in modifying risk factors for the development of these EDs.
Three studies [29,32,33] utilized ABMT with both women diagnosed with AN and healthy women with prior attentional biases. These studies used a similar task: an avatar was created for each participant replicating their body shape, and geometric figures were superimposed on various body areas to encourage balanced attention. The studies concluded that ABMT effectively reduces attentional bias and body dissatisfaction. While the VR task had good participant acceptance, excessively long sessions were reported as boring and tiring, risked being counterproductive, and potentially contributed to dropouts in future sessions.
Natali et al. [34] investigated whether VR exposure to a kitchen full of food in three different conditions could reduce food-related anxiety in patients with AN. Social support provided by an avatar was effective in reducing anxiety, although the avatar’s appearance was sometimes perceived as aversive. Nonetheless, the general impression of the VR environment was that it was realistic and provided a sense of safety greater than that experienced at home. This “safer” feeling has been previously linked to greater patient commitment to VR therapy [38], lowering the chances of dropouts. Although the inclusion in this study of participants from different gender identities is encouraging, it remains insufficient to explore potential differences or gaps.
Sansoni et al. [35] was the only study to include women with BN, confirming that VR-CBT was more effective than treatment as usual (TAU) in reducing preoccupation with weight and FGW, as well as in reducing binge eating and purging episodes in the post test and 1-month follow-up. Furthermore, BMI remained more stable over the 12-month follow-up in the VR-CBT group compared to the TAU group. However, the relatively small sample size limits the generalizability of these findings.
Finally, Behrens et al. [28] presented two studies on VR exposure: one involving healthy women with high concerns about weight and shape and the other involving women with AN. In the first study, healthy participants received a brief psychoeducational session and were then exposed for 15 min to an avatar with a 30% weight gain. This study did not find significant differences in pre- and post-exposure measures. In the second study, women with AN received an initial educational session followed by four exposure sessions to a VR avatar with an average body shape. The four sessions involved 30 min of exposure. This study effectively reduced FGW between pre- and post-exposure, but there were no significant differences between sessions, indicating that the improvements were not maintained across sessions. The difference in the educational session and the absence of a comparison group exposed to a different VR technique or no exposure at all makes it difficult to determine whether the limited results were due to the need for longer exposures or more sessions, or if pure VR exposure combined with some type of educational sessions has limited effectiveness on the studied variables.
4.2. Effectiveness of VR-ICT Intervention
The two studies that used VR-ICT interventions present mixed results, preventing a definitive conclusion about the effectiveness of VR-ICT in treating BED. On the one hand, ICT appeared to reduce some harmful BED behaviors and led to certain psychological improvements. However, it did not improve ICT performance [31]. The authors identified this lack of performance improvement between sessions as a potential risk factor for long-term relapse in BED. On the other hand, Manasse et al. [30] found that all groups, regardless of the intervention type, reduced their loss of control. They argued that engaging in recurrent training, whether ICT or a sham intervention, acted as a reminder of participants’ eating goals, prompting greater efforts to reduce BED behaviors. If this argument holds, the results found by Max et al. [31] could be attributed to the task reminding participants of their personal goals rather than the use of ICT or VR.
To clarify the actual effectiveness of ICT in VR, the strengths of both studies should be combined: ensuring a sufficient sample size to produce meaningful results and using groups that combine or exclude both ICT and VR. Furthermore, VR-ICT seems to have high acceptability among patients [30], which makes it a viable alternative for introducing ICT without requiring participants to visit a laboratory. Current research suggests that while there are promising outcomes, VR-ICT alone may not be sufficient for treating BED.
4.3. Limitations
A common limitation in most of the studies is the lack of follow-up to verify whether the improvements are maintained over time or if more sessions are needed to consolidate learning. EDs have a significant impact on both the physical and mental health of patients and can even lead to death [9]. Ensuring the long-term maintenance of the benefits observed in studies could help reduce these negative effects and decrease the likelihood of relapse.
Another limitation is the lack of standardized software or protocols for the application of VR techniques. Each study uses its own software and protocol, making it difficult to compare them and to determine whether the results achieved are influenced by specific characteristics of the tools used, the capability of the software to induce a sense of presence, or if the use of certain devices interferes with the correct application of VR techniques. It would be advisable for researchers to consider offering their software for commercial use with appropriate validity measures and standardized protocols to promote more replicable research.
Another limitation in various studies is the small sample size. Obtaining large samples in ED research is challenging, especially when focusing on a specific ED or attempting to include a significant number of men to increase sample diversity and, consequently, the generalizability of results. Strict eligibility criteria and participant dropouts often reduce the number of eligible participants, as seen in multiple studies in this review [30,34]. However, it is necessary to make efforts to increase sample sizes in experiments to ensure robust conclusions.
Linked to this limitation, some studies include both men and women in their samples but do not explore gender differences, likely due to the low number of men. This is important because, although EDs are more prevalent in women [7], men also suffer from them. Many studies focus on women for this reason, and because it is easier to obtain significant samples of women. However, other studies indicate that ICT is more effective in men than in women [39]. Future research with sufficient samples of both men and women is needed to explore possible gender differences in VR interventions. The absence of a control group not enrolled in VR interventions is another gap in many of the studies analyzed. While the studies demonstrate effectiveness compared to pre-intervention measurements, they do not provide evidence regarding whether VR interventions are more effective than non-VR interventions. Further research is also needed on the use of VR for treating BN, as the results are scarce.
It is also important to consider the limitations of the present systematic review. The criterion of including only research written in English and Spanish limited the range of the search. Articles that could potentially be included in this review but are not written in these languages may have been excluded. Additionally, the effectiveness of these interventions can be influenced by session and sample length, participant engagement, and the heterogeneity of techniques and measures used. These differences make general conclusions more difficult to apply and sometimes they focus on particular cases.
5. Conclusions
The studies analyzed in this review suggest that VR has potential as a tool for treating ED. Most studies reported improvements in various ED-related aspects among participants, and some showed that VR-based interventions were more effective than non-VR treatments. Overall, VR was well accepted by participants, who did not perceive it as difficult to use. VR could potentially increase patient engagement by reducing dropouts due to boredom or fatigue and eliminating barriers such as distance or the need for participants and facilitators to be in the same location. Additionally, VR is often perceived as a safer environment than real-life settings, which may encourage patients to engage more readily in exposure therapy. Furthermore, the capability of VR to be personalized for each person could benefit patients by allowing them to work with personally significant stimuli and information. The option of using eye-tracking in a 3D realistic environment provides direct information to the therapist about variables that affect EDs but are not easily detectable by other techniques.
Moreover, VR interventions can potentially reduce healthcare costs by decreasing the need for in-person visits and enabling remote therapy. This eliminates the need to move around to practice in different meaningful environments, such as a public swimming pool, a kitchen, or a fitting room, or have a wide range of stimuli for the practice, –such as a great amount of pizza, candies, or people observing. VR interventions also have the potential to reduce dropout rates, reducing the need for repeated treatments and lowering overall healthcare costs.
However, several challenges remain. The lack of large sample sizes, the absence of control groups in some studies, and the limited follow-up assessments make it difficult to determine whether the benefits are maintained over time and whether VR is truly more effective than other interventions. The current panorama allows us to easily be in contact with any part of the world, and searching for entities or groups of researchers willing to collaborate by providing more participants is an option that currently exists and is relatively easy to carry out. A control group with a sham VR intervention and a control group with the classic usual treatment would help discern whether the results are similar to those of usual treatment or whether they have a greater effect than a neutral situation in VR. Future research should focus on larger sample sizes, include control groups, and conduct long-term follow-ups to verify the effectiveness of VR-based interventions. Moreover, it is essential to develop more personalized VR treatments that address the specific needs of each patient and cover a broader range of therapeutic aspects.
Finally, some ethical considerations must be taken into account when using VR in therapy. VR platforms often collect sensitive personal information and health data, so it is important to have software that ensures privacy and does not collect patient data for activities other than the therapy itself. Ensuring robust encryption protocols, secure storage systems, and strict access controls is essential to protect patient privacy. VR has a certain initial cost that can still be considered high. Access to VR technology may be limited for certain populations due to socioeconomic factors or disabilities, potentially exacerbating health inequalities. Efforts should be made to make VR solutions accessible and inclusive. The immersive nature of VR can lead to intense emotional and psychological experiences. While this can be beneficial for therapy, it also poses risks, such as increased anxiety or distress. Careful monitoring and providing appropriate support and debriefing are crucial.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/app15063334/s1, Table S1: Detailed characteristics of included studies.
Author Contributions
Conceptualization, M.T.M.-M. and J.G.-M.; methodology, M.A.-L., M.T.M.-M. and J.G.-M.; validation, M.T.M.-M.; formal analysis, M.A.-L. and M.T.M.-M.; investigation, M.A.-L.; data curation, M.A.-L. and M.T.M.-M.; writing—original draft preparation, M.A.-L. and M.T.M.-M.; writing—review and editing, M.T.M.-M. and J.G.-M.; visualization, M.T.M.-M.; supervision, J.G.-M.; project administration, J.G.-M.; funding acquisition, J.G.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the Spanish Ministry of Science and Innovation (Agencia Estatal de Investigación, Ministerio de Ciencia e Innovación, Spain), Grant PID2019-108657RB-I00 funded by MCIN/AEI/10.13039/501100011033. This study was also funded by “Fundació La Marató de TV3”, Grant 202217-10.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Hilty, D.M.; Randhawa, K.; Maheu, M.M.; McKean, A.J.S.; Pantera, R.; Mishkind, M.C.; Rizzo, A. A Review of Telepresence, Virtual Reality, and Augmented Reality Applied to Clinical Care. J. Technol. Behav. Sci. 2020, 5, 178–205. [Google Scholar] [CrossRef]
- Cieślik, B.; Mazurek, J.; Rutkowski, S.; Kiper, P.; Turolla, A.; Szczepańska-Gieracha, J. Virtual Reality in Psychiatric Disorders: A Systematic Review of Reviews. Complement. Ther. Med. 2020, 52, 102480. [Google Scholar] [CrossRef]
- Clus, D.; Larsen, M.E.; Lemey, C.; Berrouiguet, S. The Use of Virtual Reality in Patients with Eating Disorders: Systematic Review. J. Med. Internet Res. 2018, 20, e157. [Google Scholar] [CrossRef]
- Rauschnabel, P.A.; Felix, R.; Hinsch, C.; Shahab, H.; Alt, F. What Is XR? Towards a Framework for Augmented and Virtual Reality. Comput. Human Behav. 2022, 133, 107289. [Google Scholar] [CrossRef]
- Riva, G.; Malighetti, C.; Serino, S. Virtual Reality in the Treatment of Eating Disorders. Clin. Psychol. Psychother. 2021, 28, 477–488. [Google Scholar] [CrossRef] [PubMed]
- Ciążyńska, J.; Maciaszek, J. Various Types of Virtual Reality-Based Therapy for Eating Disorders: A Systematic Review. J. Clin. Med. 2022, 11, 4956. [Google Scholar] [CrossRef]
- Silén, Y.; Keski-Rahkonen, A. Worldwide Prevalence of DSM-5 Eating Disorders among Young People. Curr. Opin. Psychiatry 2022, 35, 362–371. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association: Washington, DC, USA, 2013; ISBN 0-89042-555-8. [Google Scholar]
- American Psychiatric Association. The American Psychiatric Association Practice Guideline for the Treatment of Patients with Eating Disorders; American Psychiatric Association Publishing: Washington, DC, USA, 2023; ISBN 0-89042-584-1. [Google Scholar]
- Arcelus, J.; Mitchell, A.J.; Wales, J.; Nielsen, S. Mortality Rates in Patients With Anorexia Nervosa and Other Eating Disorders. Arch. Gen. Psychiatry 2011, 68, 724. [Google Scholar] [CrossRef]
- Micali, N.; Martini, M.G.; Thomas, J.J.; Eddy, K.T.; Kothari, R.; Russell, E.; Bulik, C.M.; Treasure, J. Lifetime and 12-Month Prevalence of Eating Disorders amongst Women in Mid-Life: A Population-Based Study of Diagnoses and Risk Factors. BMC Med. 2017, 15, 12. [Google Scholar] [CrossRef]
- Tanner, A.B. Unique Considerations for the Medical Care of Restrictive Eating Disorders in Children and Young Adolescents. J. Eat. Disord. 2023, 11, 33. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Bailey-Straebler, S.; Basden, S.; Doll, H.A.; Jones, R.; Murphy, R.; O’Connor, M.E.; Cooper, Z. A Transdiagnostic Comparison of Enhanced Cognitive Behaviour Therapy (CBT-E) and Interpersonal Psychotherapy in the Treatment of Eating Disorders. Behav. Res. Ther. 2015, 70, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Södersten, P.; Bergh, C.; Leon, M.; Brodin, U.; Zandian, M. Cognitive Behavior Therapy for Eating Disorders versus Normalization of Eating Behavior. Physiol. Behav. 2017, 174, 178–190. [Google Scholar] [CrossRef]
- Zipfel, S.; Giel, K.E.; Bulik, C.M.; Hay, P.; Schmidt, U. Anorexia Nervosa: Aetiology, Assessment, and Treatment. Lancet Psychiatry 2015, 2, 1099–1111. [Google Scholar] [CrossRef]
- Lock, J.; Le Grange, D. Family-based Treatment: Where Are We and Where Should We Be Going to Improve Recovery in Child and Adolescent Eating Disorders. Int. J. Eat. Disord. 2019, 52, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Keizer, A.; van Elburg, A.; Helms, R.; Dijkerman, H.C. A Virtual Reality Full Body Illusion Improves Body Image Disturbance in Anorexia Nervosa. PLoS ONE 2016, 11, e0163921. [Google Scholar] [CrossRef]
- Porras-Garcia, B.; Ferrer-Garcia, M.; Serrano-Troncoso, E.; Carulla-Roig, M.; Soto-Usera, P.; Miquel-Nabau, H.; Shojaeian, N.; de la Montaña Santos-Carrasco, I.; Borszewski, B.; Díaz-Marsá, M.; et al. Validity of Virtual Reality Body Exposure to Elicit Fear of Gaining Weight, Body Anxiety and Body-Related Attentional Bias in Patients with Anorexia Nervosa. J. Clin. Med. 2020, 9, 3210. [Google Scholar] [CrossRef] [PubMed]
- Ferrer-Garcia, M.; Pla-Sanjuanelo, J.; Dakanalis, A.; Vilalta-Abella, F.; Riva, G.; Fernandez-Aranda, F.; Forcano, L.; Riesco, N.; Sánchez, I.; Clerici, M.; et al. A Randomized Trial of Virtual Reality-Based Cue Exposure Second-Level Therapy and Cognitive Behavior Second-Level Therapy for Bulimia Nervosa and Binge-Eating Disorder: Outcome at Six-Month Followup. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 60–68. [Google Scholar] [CrossRef]
- Nameth, K.; Brown, T.; Bullock, K.; Adler, S.; Riva, G.; Safer, D.; Runfola, C. Translating Virtual Reality Cue Exposure Therapy for Binge Eating into a Real-World Setting: An Uncontrolled Pilot Study. J. Clin. Med. 2021, 10, 1511. [Google Scholar] [CrossRef]
- Matsangidou, M.; Otkhmezuri, B.; Ang, C.S.; Avraamides, M.; Riva, G.; Gaggioli, A.; Iosif, D.; Karekla, M. “Now I Can See Me” Designing a Multi-User Virtual Reality Remote Psychotherapy for Body Weight and Shape Concerns. Hum. Comput. Interact. 2022, 37, 314–340. [Google Scholar] [CrossRef]
- Manasse, S.M.; Lampe, E.W.; Juarascio, A.S.; Zhu, J.; Forman, E.M. Using Virtual Reality to Train Inhibitory Control and Reduce Binge Eating: A Proof-of-Concept Study. Appetite 2021, 157, 104988. [Google Scholar] [CrossRef]
- Vlahovic, S.; Suznjevic, M.; Skorin-Kapov, L. A Survey of Challenges and Methods for Quality of Experience Assessment of Interactive VR Applications. J. Multimodal User Interfaces 2022, 16, 257–291. [Google Scholar] [CrossRef]
- Dane, A.; Bhatia, K. The Social Media Diet: A Scoping Review to Investigate the Association between Social Media, Body Image and Eating Disorders amongst Young People. PLoS Glob. Public Health 2023, 3, e0001091. [Google Scholar] [CrossRef] [PubMed]
- Gusenbauer, M.; Haddaway, N.R. Which Academic Search Systems Are Suitable for Systematic Reviews or Meta-analyses? Evaluating Retrieval Qualities of Google Scholar, PubMed, and 26 Other Resources. Res. Synth. Methods 2020, 11, 181–217. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; the PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Behrens, S.C.; Tesch, J.; Sun, P.J.B.; Starke, S.; Black, M.J.; Schneider, H.; Pruccoli, J.; Zipfel, S.; Giel, K.E. Virtual Reality Exposure to a Healthy Weight Body Is a Promising Adjunct Treatment for Anorexia Nervosa. Psychother. Psychosom. 2023, 92, 170–179. [Google Scholar] [CrossRef]
- Ascione, M.; Carulla-Roig, M.; Miquel-Nabau, H.; Porras-Garcia, B.; Meschberger-Annweiler, F.-A.; Serrano-Troncoso, E.; Ferrer-Garcia, M.; Moreno-Sánchez, M.; Gutierrez-Maldonado, J. Attentional Bias Modification Training Based on Virtual Reality and Eye Tracking in Anorexia Nervosa Patients. J. Clin. Med. 2023, 12, 5932. [Google Scholar] [CrossRef]
- Manasse, S.M.; Trainor, C.; Payne-Reichert, A.; Abber, S.R.; Lampe, E.W.; Gillikin, L.M.; Juarascio, A.S.; Forman, E.M. Does Virtual Reality Enhance the Effects of Inhibitory Control Training for Loss-of-Control Eating? A Pilot Factorial Experiment. Eat. Behav. 2023, 50, 101749. [Google Scholar] [CrossRef]
- Max, S.M.; Schag, K.; Giel, K.E.; Plewnia, C. Behavioural Biases in the Interaction with Food Objects in Virtual Reality and Its Clinical Implication for Binge Eating Disorder. Eat. Weight Disord. 2023, 28, 46. [Google Scholar] [CrossRef]
- Meschberger-Annweiler, F.-A.; Ascione, M.; Porras-Garcia, B.; Ferrer-Garcia, M.; Moreno-Sanchez, M.; Miquel-Nabau, H.; Serrano-Troncoso, E.; Carulla-Roig, M.; Gutiérrez-Maldonado, J. An Attentional Bias Modification Task, through Virtual Reality and Eye-Tracking Technologies, to Enhance the Treatment of Anorexia Nervosa. J. Clin. Med. 2023, 12, 2185. [Google Scholar] [CrossRef]
- Miquel-Nabau, H.; Briseño-Oloriz, N.; Porras-Garcia, B.; Ascione, M.; Meschberger-Annweiler, F.-A.; Ferrer-Garcia, M.; Moreno-Sanchez, M.; Serrano-Troncoso, E.; Carulla-Roig, M.; Gutiérrez Maldonado, J. Modification of Body-Related Attentional Bias through Virtual Reality and Eye-Tracking in Healthy Participants: Implications for Anorexia Nervosa Treatments. Brain Sci. 2023, 13, 764. [Google Scholar] [CrossRef] [PubMed]
- Natali, L.; Meregalli, V.; Rowlands, K.; Di Pietro, J.; Treasure, J.; Collantoni, E.; Meneguzzo, P.; Tenconi, E.; Favaro, A.; Fontana, F.; et al. Virtual Food Exposure with Positive Mood Induction or Social Support to Reduce Food Anxiety in Anorexia Nervosa: A Feasibility Study. Int. J. Eat. Disord. 2024, 57, 703–715. [Google Scholar] [CrossRef] [PubMed]
- Sansoni, M.; Varallo, G.; Malighetti, C.; Tuena, C.; Di Lernia, D.; Cesa, G.L.; Manzoni, G.M.; Castelnuovo, G.; Riva, G. Unlocking the Potential of Virtual Reality to Expand Treatment Frontiers for Bulimia Nervosa: A Pilot Study to Explore the Impact of Virtual Reality-Enhanced Cognitive-Behavioral Therapy. Virtual Real. 2024, 28, 79. [Google Scholar] [CrossRef]
- Dondzilo, L.; Basanovic, J.; Grafton, B.; Bell, J.; Turnbull, G.; MacLeod, C. A Serial Mediation Model of Attentional Engagement with Thin Bodies on Body Dissatisfaction: The Role of Appearance Comparisons and Rumination. Curr. Psychol. 2023, 42, 1896–1904. [Google Scholar] [CrossRef]
- Williamson, D.A.; White, M.A.; York-Crowe, E.; Stewart, T.M. Cognitive-Behavioral Theories of Eating Disorders. Behav. Modif. 2004, 28, 711–738. [Google Scholar] [CrossRef]
- Lindner, P. Better, Virtually: The Past, Present, and Future of Virtual Reality Cognitive Behavior Therapy. Int. J. Cogn. Ther. 2021, 14, 23–46. [Google Scholar] [CrossRef]
- Tang, W.S.W.; Ng, T.J.Y.; Wong, J.Z.A.; Ho, C.S.H. The Role of Serious Video Games in the Treatment of Disordered Eating Behaviors: Systematic Review. J. Med. Internet Res. 2022, 24, e39527. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).