Force Expressed by 3D-Printed Aligners with Different Thickness and Design Compared to Thermoformed Aligners: An in Vitro Study
Abstract
1. Introduction
2. Materials and Methods
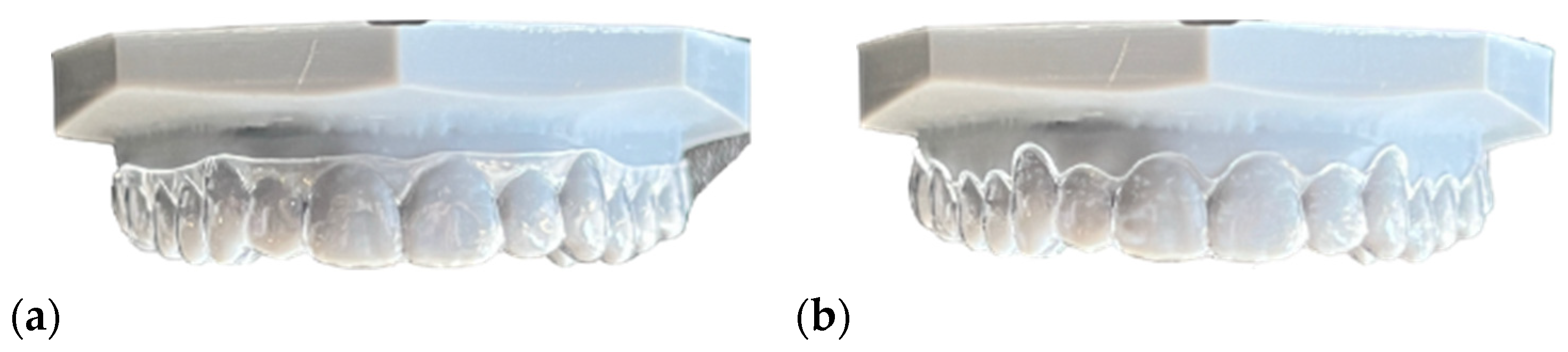
2.1. Sample Preparation
2.2. Aligners Selected
- Nine NOXI aligners made of Polyammide (PA) with a vertical and horizontal thickness gradient (vertical: 0.65 mm at the incisal margin, gradually increasing to 0.95 mm at the gingival margin; horizontal: 0.65 mm at the incisors, gradually increasing to 0.95 mm at the molars). The gingival margin of the aligner is trimmed 2 mm above the gingival contour (NHVH).
- Nine NOXI aligners made of Polyammide (PA) with a horizontal thickness gradient (0.65 mm at the incisors, increasing to 0.95 mm at the molars) and a gingival margin trimmed 2 mm above the gingival contour (NHH).
- Nine NOXI aligners made of Polyammide (PA) with a horizontal thickness gradient (0.65 mm at the incisors, increasing to 0.95 mm at the molars) and a gingival margin trimmed at the zenith of the tooth (NHZ).

- Nine F22 aligners with a straight gingival margin (cut at the zenith) made of EvoFlex (Bay Materials LLC, Fremont, CA, USA) with a thickness of 0.76 mm (F22).
- Nine aligners with a scalloped gingival margin made of EvoFlex with a thickness of 0.76 mm (AS).
2.2.1. Mechanical Properties of Polyamide
2.2.2. Mechanical Properties of EvoFlex
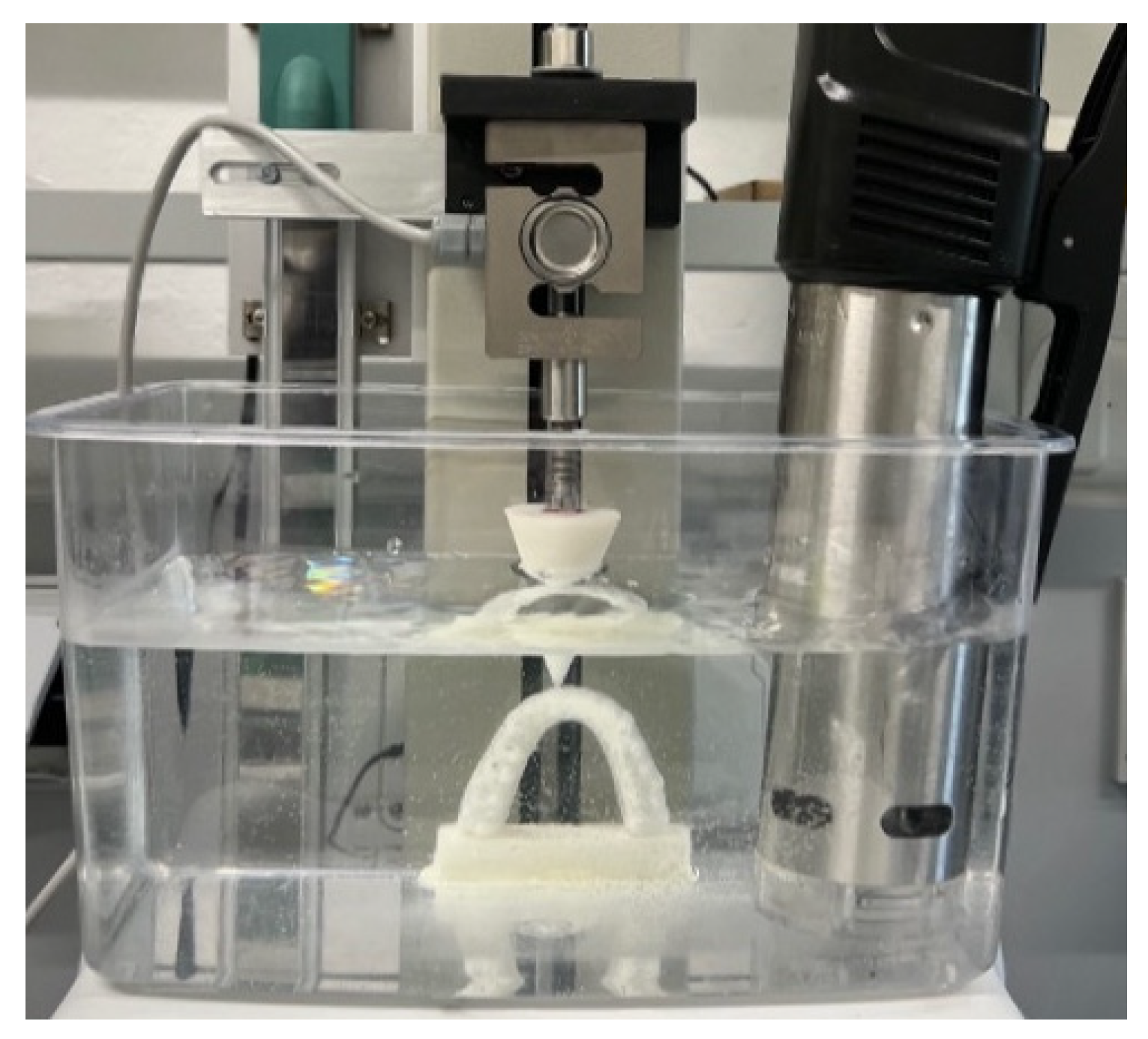
2.3. Preparation and Testing Model Creation
2.4. Testing Procedure
2.5. Statistical Analysis
2.5.1. Repeatability Test
2.5.2. Descriptive Statistics
2.5.3. Statistical Tests
2.5.4. Force Analysis Among Points
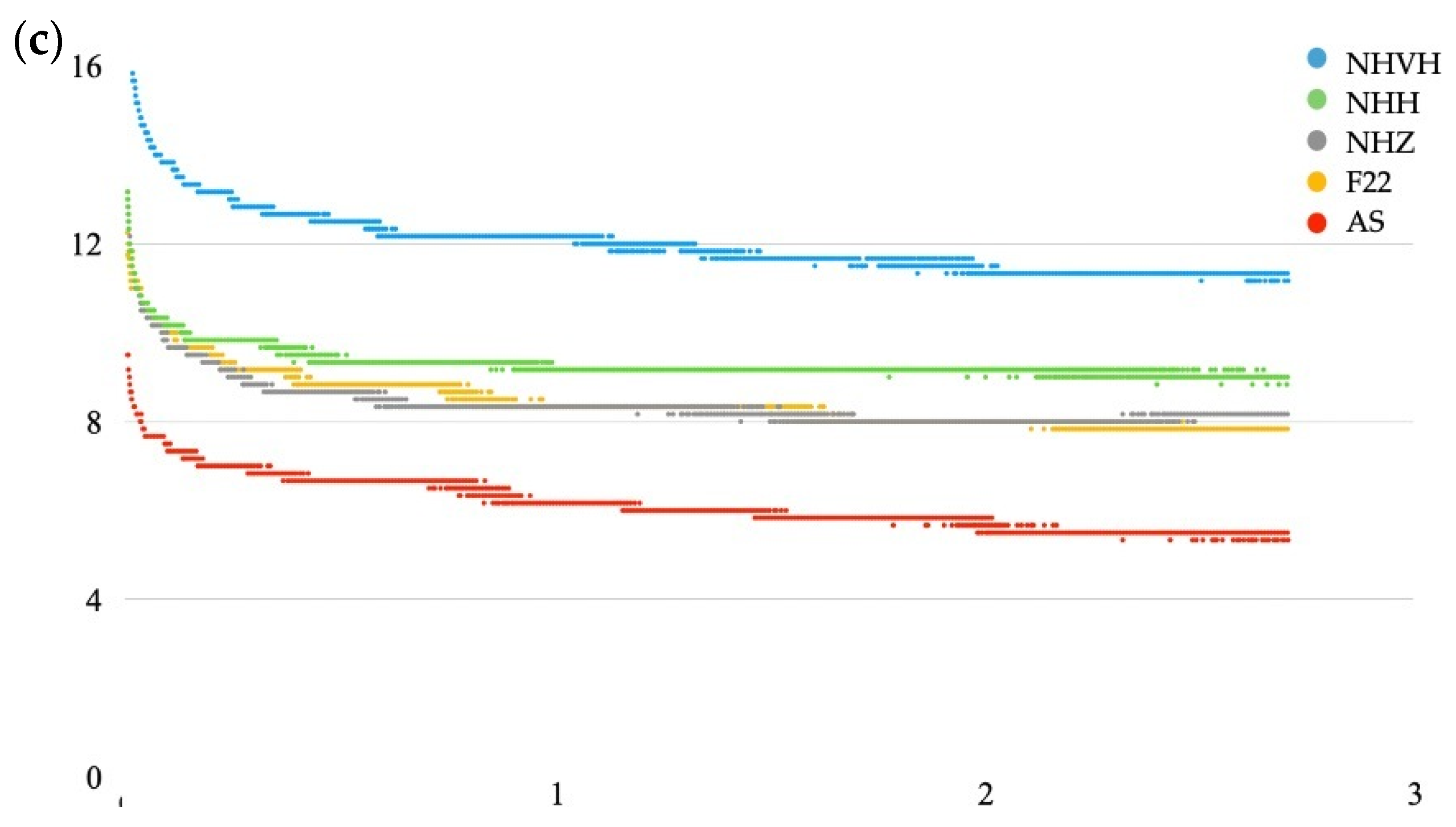
2.5.5. Force Decay (Stress Relaxation)
2.5.6. Effect Measurements
2.5.7. Comparison of Force Between Incisor and Molar
2.5.8. Sample Size
2.5.9. Software
3. Results
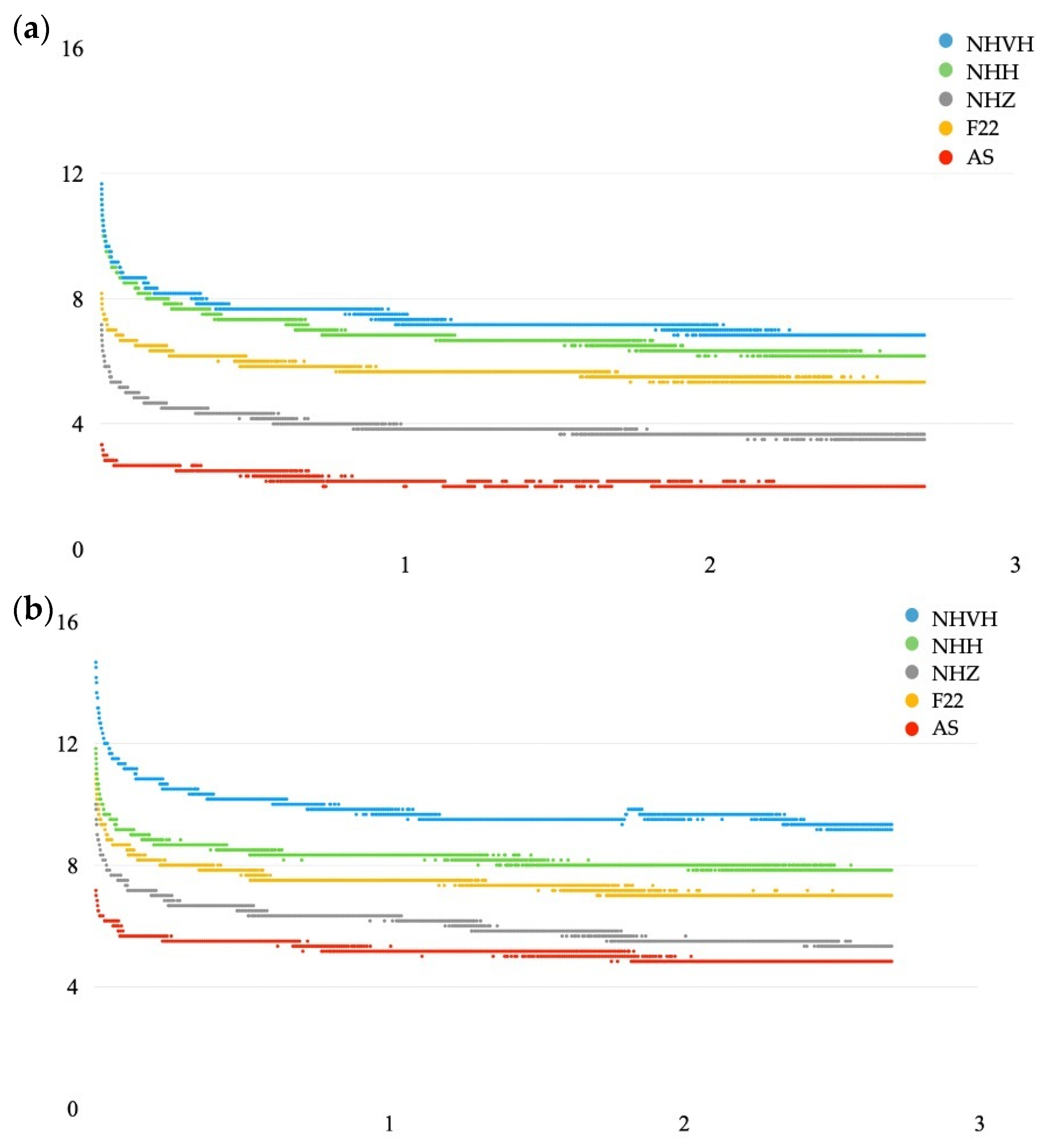
3.1. Incisor (1.1)
- At the gingival point, the NHVH aligner exerted the highest average force, followed by NHH, F22, NHZ, and AS;
- At the middle point, NHVH again showed the highest force, followed by NHH, NHZ, F22, and AS;
- At the incisal point, NHH had the highest force, followed by NHVH, NHZ, F22, and AS (Table 2).
| Point | Aligner | n | Mean | SD | F (df1, df2) | p-Value | Eta-Squared |
|---|---|---|---|---|---|---|---|
| Gingival | AS | 10,752 | 1.4 | 0.2 | 297,934.011 (4, 37,236.278) | <0.001 * | 0.957 |
| F22 | 10,752 | 3.2 | 0.4 | ||||
| NHH | 10,752 | 3.2 | 0.4 | ||||
| NHVH | 10,752 | 7.2 | 0.6 | ||||
| NHZ | 10,752 | 2.8 | 0.3 | ||||
| Middle | AS | 10,752 | 4.3 | 0.5 | 98,293.072 (4, 43,204.643) | <0.001 * | 0.878 |
| F22 | 10,752 | 5.3 | 0.7 | ||||
| NHH | 10,752 | 5.9 | 0.4 | ||||
| NHVH | 10,752 | 8.7 | 0.6 | ||||
| NHZ | 10,752 | 5.5 | 0.4 | ||||
| Incisal | AS | 10,752 | 6.3 | 0.8 | 53,640.504 (4, 49,636.352) | <0.001 * | 0.797 |
| F22 | 10,752 | 7.8 | 0.7 | ||||
| NHH | 10,752 | 10.1 | 0.8 | ||||
| NHVH | 10,752 | 9.8 | 0.6 | ||||
| NHZ | 10,752 | 8.0 | 0.6 |
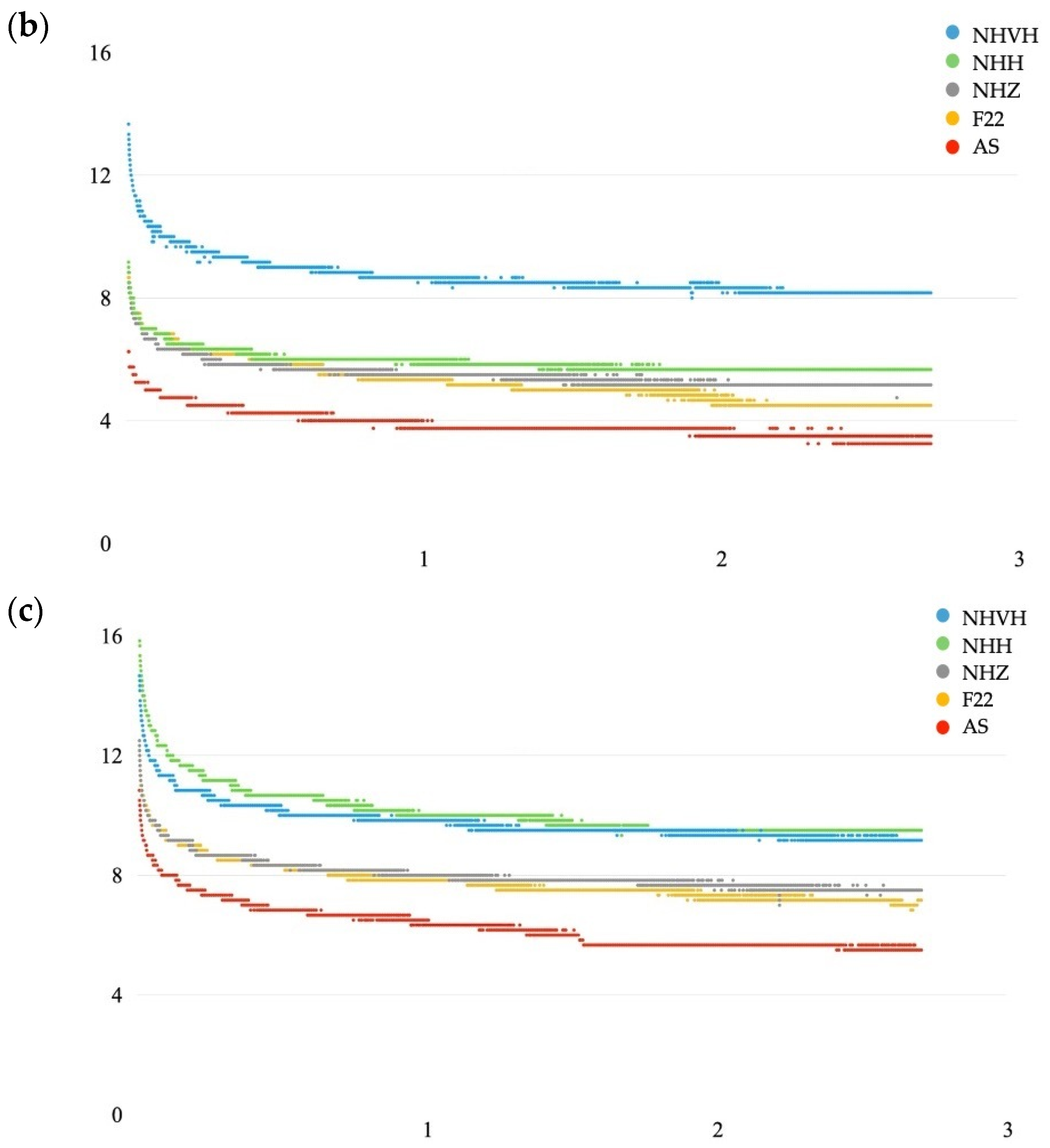
3.2. Molar (2.6)
4. Discussion
5. Conclusions
- The NOXI aligner with both horizontal and vertical gradients and a high margin exerted the greatest overall force, particularly at the gingival point where force dissipation was most evident. It was followed by the NOXI with a horizontal gradient and a high margin.
- No statistically significant differences in stress relaxation were observed among the five aligners tested.
- For aligners of the same thickness, the height of the margin significantly influenced the force exerted.
- The force applied was greater at the upper first molar than at the upper central incisor.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bonnick, A.M.; Nalbandian, M.; Siewe, M.S. Technological advances in nontraditional orthodontics. Dent. Clin. 2011, 55, 571–584. [Google Scholar] [CrossRef] [PubMed]
- Favero, L.; Cortelazzo, V.; Arreghini, A. Efficacia e vantaggi di una metodica invisibile a rivalutazione sequenziale: Il sistema Clear Aligner. Mondo Ortod. 2010, 35, 87–94. [Google Scholar] [CrossRef]
- Proffit, W.R.; Fields, H.W.; Sarver, D.M. Contemporary Orthodontics, 5th ed.; Elsevier: Filadelfia, PA, USA, 2013. [Google Scholar]
- Kesling, H.D. Coordinating the predetermined pattern and tooth positioner with conventional treatment. Am. J. Orthod. Oral Surg. 1946, 32, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Fang, D.; Zhang, N.; Chen, H.; Bai, Y. Dynamic Stress Relaxation of Orthodontic Thermoplastic Materials in a Simulated Oral Environment. Dent. Mater. J. 2013, 32, 946–951. [Google Scholar] [CrossRef]
- Tartaglia, G.M.; Mapelli, A.; Maspero, C.; Santaniello, T.; Serafin, M.; Farronato, M.; Caprioglio, A. Direct 3D Printing of Clear Orthodontic Aligners: Current State and Future Possibilities. Materials 2021, 14, 1799. [Google Scholar] [CrossRef]
- Voet, V.S.D.; Guit, J.; Loos, K. Sustainable Photopolymers in 3D Printing: A Review on Biobased, Biodegradable, and Recyclable Alternatives. Macromol. Rapid Commun. 2021, 42, 2000475. [Google Scholar] [CrossRef]
- Cremonini, F.; Vianello, M.; Bianchi, A.; Lombardo, L. A Spectrophotometry Evaluation of Clear Aligners Transparency: Comparison of 3D-Printers and Thermoforming Disks in Different Combinations. Appl. Sci. 2022, 12, 11964. [Google Scholar] [CrossRef]
- Gueche, Y.A.; Sanchez-Ballester, N.M.; Cailleaux, S.; Bataille, B.; Soulairol, I. Selective Laser Sintering (SLS), a New Chapter in the Production of Solid Oral Forms (SOFs) by 3D Printing. Pharmaceutics 2021, 13, 1212. [Google Scholar] [CrossRef]
- Hertan, E.; Lewis, H.G.; Kharlamov, A. Advancements in Clear Aligner Therapy: Direct 3D Printing and Biomechanical Innovations. J. Clin. Orthod. 2020, 54, 205–212. [Google Scholar]
- Eliades, G.; Zinelis, S.; Papageorgiou, S.N. Mechanical Properties and Clinical Performance of Clear Aligners and Fixed Appliances. J. Clin. Orthod. 2021, 53, 102–110. [Google Scholar]
- Jindal, P.; Juneja, M.; Siena, F.L.; Bajaj, D.; Breedon, P. Mechanical and geometric properties of thermoformed and 3D printed clear dental aligners. Am. J. Orthod. Dentofac. Orthop. 2019, 56, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Hazeveld, A.; Slater, J.J.H.; Ren, Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Chuchulska, B.; Zlatev, S. Linear Dimensional Change and Ultimate Tensile Strength of Polyamide Materials for Denture Bases. Polymers 2021, 13, 3446. [Google Scholar] [CrossRef] [PubMed]
- Lyu, X.; Cao, X.; Yan, J.; Zeng, R.; Tan, J. Biomechanical Effects of Clear Aligners with Different Thicknesses and Gingival-Margin Morphology for Appliance Design Optimization. Am. J. Orthod. Dentofac. Orthop. 2023, 164, 239–252. [Google Scholar] [CrossRef]
- Lombardo, L.; Martines, E.; Mazzanti, V.; Arreghini, A.; Mollica, F.; Siciliani, G. Stress Relaxation Properties of Four Orthodontic Aligner Materials: A 24-Hour In Vitro Study. Angle Orthod. 2016, 87, 11–18. [Google Scholar] [CrossRef]
- Beretta, M.; Federici Canova, F.; Gianolio, A.; Mangano, A.; Paglia, M.; Colombo, S.; Cirulli, N. ZeroExpander: Metal-free automatic palatal expansion for special-needs patients. Eur. J. Paediatr. Dent. 2021, 22, 151–154. [Google Scholar] [CrossRef]
- Campobasso, A.; Battista, G.; Lo Muzio, E.; Colombo, S.; Paglia, M.; Federici Canova, F.; Gianolio, A.; Beretta, M. New 3D printed polymers in orthodontics: A scoping review. Eur. J. Paediatr. Dent. 2023, 24, 224–228. [Google Scholar] [CrossRef]
- Albertini, P.; Mazzanti, V.; Mollica, F.; Pellitteri, F.; Palone, M.; Lombardo, L. Stress Relaxation Properties of Five Orthodontic Aligner Materials: A 14-Day In-Vitro Study. Bioengineering 2022, 9, 349. [Google Scholar] [CrossRef]
- Samuels, R.H.; Rudge, S.J.; Mair, L.H. The Effect of Orthodontic Forces on the Dental Pulp. J. Orthod. 2016, 43, 73–81. [Google Scholar]
- Proffit, W.R.; Fields, H.W.; Larson, B.E.; Sarver, D.M.; Cozza, P. Ortodonzia Moderna, 6th ed.; Edra: Perignano, Italy, 2020. [Google Scholar]
- Kameyama, T.; Warita, H.; Matsumoto, Y.; Otsubo, K. A Mechanical Stress Model Applied to the Rat Periodontium: Using Controlled Magnitude and Direction of Orthodontic Force with an Absolute Anchorage. Oral Med. Pathol. 2002, 7, 1–7. [Google Scholar] [CrossRef][Green Version]
- Cremonini, F.; Pavan, F.; Pellitteri, F.; Palone, M.; Lombardo, L. Variation of gingival crevicular fluid volume in early orthodontic tooth movement with clear aligner: A pilot study. Sci. Rep. 2023, 14, 42–47. [Google Scholar] [CrossRef]
- Cowley, D.P.; Mah, J.; O’Toole, B. The Effect of Gingival-Margin Design on the Retention of Thermoformed Aligners. J. Clin. Orthod. 2012, 46, 697–702; quiz 705. [Google Scholar] [PubMed]
- Cremonini, F.; Brucculeri, L.; Pepe, F.; Palone, M.; Lombardo, L. Comparison of Stress Relaxation Properties between 3-Dimensional Printed and Thermoformed Orthodontic Aligners: A Pilot Study of In Vitro Simulation of Two Consecutive 8-Hours Force Application. APOS Trends Orthod. 2024, 14, 225–234. [Google Scholar] [CrossRef]
- Grassia, V.; d’Apuzzo, F.; Alansari, R.A.; Jamilian, A.; Sayahpour, B.; Adel, S.M.; Nucci, L. Instagram and Clear Aligner Therapy: A Content Analysis of Patient Perspectives. Semin. Orthod. 2024, 30, 123–130. [Google Scholar] [CrossRef]
- Sheridan, J.J.; Ledoux, W.; McMinn, R. Essix Appliances: Minor Tooth Movement with Divots and Windows. J. Clin. Orthod. 1994, 28, 659–663. [Google Scholar]
- Palone, M.; Longo, M.; Arveda, N.; Nacucchi, M.; Pascalis, F.; Spedicato, G.A.; Siciliani, G.; Lombardo, L. Micro-computed tomography evaluation of general trends in aligner thickness and gap width after thermoforming procedures involving six commercial clear aligners: An in vitro study. Korean J. Orthod. 2021, 51, 135–141. [Google Scholar] [CrossRef]
- Hertan, E.; McCray, J.; Bankhead, B.; Kim, K.B. Force Profile Assessment of Direct-Printed Aligners Versus Thermoformed Aligners and the Effects of Non-Engaged Surface Patterns. Prog. Orthod. 2022, 23, 49. [Google Scholar] [CrossRef]
- Edelmann, A.; English, J.D.; Chen, S.J.; Kasper, F.K. Analysis of the Thickness of 3-Dimensional-Printed Orthodontic Aligners. Am. J. Orthod. Dentofac. Orthop. 2020, 158, e91–e98. [Google Scholar] [CrossRef]
- McCarty, M.C.; Chen, S.J.; English, J.D.; Kasper, F. Effect of Print Orientation and Duration of Ultraviolet Curing on the Dimensional Accuracy of a 3-Dimensionally Printed Orthodontic Clear Aligner Design. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 889–897. [Google Scholar] [CrossRef]
- Can, E.; Panayi, N.; Polychronis, G.; Papageorgiou, S.N.; Zinelis, S.; Eliades, G.; Eliades, T. In-House 3D-Printed Aligners: Effect of In Vivo Ageing on Mechanical Properties. Eur. J. Orthod. 2022, 44, 51–55. [Google Scholar] [CrossRef]
- Lee, S.Y.; Kim, H.; Kim, H.J.; Chung, C.J.; Choi, Y.J.; Kim, S.J.; Cha, J.Y. Thermo-Mechanical Properties of 3D Printed Photocurable Shape Memory Resin for Clear Aligners. Sci. Rep. 2022, 12, 6246. [Google Scholar] [CrossRef] [PubMed]
- Shirey, N.; Mendonca, G.; Groth, C.; Kim-Berman, H. Comparison of Mechanical Properties of 3-Dimensional Printed and Thermoformed Orthodontic Aligners. Am. J. Orthod. Dentofac. Orthop. 2023, 163, 720–728. [Google Scholar] [CrossRef] [PubMed]


| Force (N) | Force (N) | Force (N) | |
|---|---|---|---|
| Inter-Item Correlation Matrix Gingival Incisor | 1.00 | 0.90 | 0.96 |
| 0.90 | 1.00 | 0.92 | |
| 0.96 | 0.92 | 1.00 | |
| Inter-Item Correlation Matrix Middle Incisor | 1.00 | 0.94 | 0.94 |
| 0.94 | 1.00 | 0.93 | |
| 0.94 | 0.93 | 1.00 | |
| Inter-Item Correlation Matrix Incisal Incisor | 1.00 | 0.94 | 0.96 |
| 0.94 | 1.00 | 0.92 | |
| 0.96 | 0.92 | 1.00 | |
| Inter-Item Correlation Matrix Gingival Molar | 1.00 | 0.97 | 0.92 |
| 0.97 | 1.00 | 0.93 | |
| 0.92 | 0.93 | 1.00 | |
| Inter-Item Correlation Matrix Middle Molar | 1.00 | 0.91 | 0.91 |
| 0.91 | 1.00 | 0.92 | |
| 0.91 | 0.92 | 1.00 | |
| Inter-Item Correlation Matrix Occlusal Molar | 1.00 | 0.96 | 0.96 |
| 0.96 | 1.00 | 0.96 | |
| 0.96 | 0.96 | 1.00 |
| Material | Point | Initial Force (N) | Final Force (N) | Stress Relaxation (%) | Mean | Median | SD | 25th Percentile | 75th Percentile | p-Value |
|---|---|---|---|---|---|---|---|---|---|---|
| AS | Gingival | 2.0 | 1.0 | 50.0 | 50.3 | 50.0 | 1.3 | 49.2 | 51.7 | 0.212 |
| Middle | 6.6 | 3.5 | 51.7 | |||||||
| Incisal | 10.8 | 5.5 | 49.2 | |||||||
| F22 | Gingival | 5.2 | 2.0 | 51.9 | 46.8 | 47.6 | 5.5 | 41.0 | 51.9 | |
| Middle | 6.6 | 3.5 | 47.6 | |||||||
| Incisal | 5.5 | 8 | 41.0 | |||||||
| NHH | Gingival | 6.0 | 2.8 | 53.3 | 44.7 | 42.9 | 7.8 | 38.0 | 53.3 | |
| Middle | 9.2 | 5.6 | 38.0 | |||||||
| Incisal | 16.3 | 9.5 | 42.9 | |||||||
| NHVH | Gingival | 11.7 | 6.5 | 44.4 | 40.7 | 40.1 | 3.5 | 37.4 | 44.4 | |
| Middle | 13.7 | 8.7 | 40.1 | |||||||
| Incisal | 14.7 | 9.7 | 37.4 | |||||||
| NHZ | Gingival | 4.3 | 2.5 | 46.5 | 42.5 | 40.9 | 3.5 | 40.0 | 46.5 | |
| Middle | 8.8 | 5.2 | 40.9 | |||||||
| Incisal | 12.5 | 7.5 | 40.0 |
| Point | Aligner | n | Mean | SD | F (df1, df2) | p-Value | Eta-Squared |
|---|---|---|---|---|---|---|---|
| Gingival | AS | 10,752 | 2.2 | 0.2 | 209,619.977 (4, 39,266.816) | <0.001 * | 0.940 |
| F22 | 10,752 | 5.7 | 0.4 | ||||
| NHH | 10,752 | 7.4 | 0.6 | ||||
| NHVH | 10,752 | 6.8 | 0.7 | ||||
| NHZ | 10,752 | 4.0 | 0.4 | ||||
| Middle | AS | 10,752 | 5.2 | 0.3 | 140,950.949 (4, 45,639.097) | <0.001 * | 0.913 |
| F22 | 10,752 | 7.4 | 0.5 | ||||
| NHH | 10,752 | 9.8 | 0.6 | ||||
| NHVH | 10,752 | 8.3 | 0.4 | ||||
| NHZ | 10,752 | 6.1 | 0.6 | ||||
| Occlusal | AS | 10,752 | 6.1 | 0.6 | 127,554.367 (4, 46,685.640) | <0.001 * | 0.905 |
| F22 | 10,752 | 8.4 | 0.7 | ||||
| NHH | 10,752 | 12.0 | 0.8 | ||||
| NHVH | 10,752 | 9.3 | 0.4 | ||||
| NHZ | 10,752 | 8.4 | 0.6 |
| Material | Point | Initial Force (N) | Final Force (N) | Stress Relaxation (%) | Mean | Median | SD | 25th Percentile | 75th Percentile | p-Value |
|---|---|---|---|---|---|---|---|---|---|---|
| AS | Gingival | 3.3 | 2.0 | 39.4 | 39.0 | 39.4 | 5.5 | 33.3 | 44.2 | 0.284 |
| Middle | 7.2 | 4.8 | 33.3 | |||||||
| Incisal | 9.5 | 5.3 | 44.2 | |||||||
| F22 | Gingival | 8.2 | 5.3 | 34.6 | 35.9 | 36.4 | 1.1 | 34.6 | 36.6 | |
| Middle | 11.0 | 7.0 | 36.4 | |||||||
| Incisal | 12.3 | 7.8 | 36.6 | |||||||
| NHH | Gingival | 11.2 | 6.2 | 44.6 | 39.0 | 38.5 | 2.6 | 36.7 | 41.9 | |
| Middle | 11.8 | 7.8 | 34.4 | |||||||
| Incisal | 13.2 | 8.8 | 33.3 | |||||||
| NHVH | Gingival | 11.7 | 6.8 | 41.9 | 37.4 | 34.4 | 6.2 | 33.3 | 44.6 | |
| Middle | 14.7 | 9.2 | 36.7 | |||||||
| Incisal | 18.2 | 11.3 | 38.5 | |||||||
| NHZ | Gingival | 7.2 | 3.5 | 51.4 | 45.4 | 47.0 | 6.9 | 37.9 | 51.4 | |
| Middle | 10.0 | 5.3 | 47.0 | |||||||
| Incisal | 13.2 | 8.2 | 37.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cremonini, F.; Pancari, C.; Brucculeri, L.; Karami Shabankare, A.; Lombardo, L. Force Expressed by 3D-Printed Aligners with Different Thickness and Design Compared to Thermoformed Aligners: An in Vitro Study. Appl. Sci. 2025, 15, 2911. https://doi.org/10.3390/app15062911
Cremonini F, Pancari C, Brucculeri L, Karami Shabankare A, Lombardo L. Force Expressed by 3D-Printed Aligners with Different Thickness and Design Compared to Thermoformed Aligners: An in Vitro Study. Applied Sciences. 2025; 15(6):2911. https://doi.org/10.3390/app15062911
Chicago/Turabian StyleCremonini, Francesca, Carolina Pancari, Luca Brucculeri, Ariyan Karami Shabankare, and Luca Lombardo. 2025. "Force Expressed by 3D-Printed Aligners with Different Thickness and Design Compared to Thermoformed Aligners: An in Vitro Study" Applied Sciences 15, no. 6: 2911. https://doi.org/10.3390/app15062911
APA StyleCremonini, F., Pancari, C., Brucculeri, L., Karami Shabankare, A., & Lombardo, L. (2025). Force Expressed by 3D-Printed Aligners with Different Thickness and Design Compared to Thermoformed Aligners: An in Vitro Study. Applied Sciences, 15(6), 2911. https://doi.org/10.3390/app15062911







