1. Introduction
Passive Dynamic Ankle–Foot Orthoses (PD-AFOs) are assistive medical devices prescribed for individuals affected by neuro-muscular deficits of the ankle dorsiflexor muscles, usually associated with neurological conditions like cerebral palsy [
1,
2,
3], stroke [
4,
5,
6], and hemiplegia [
7,
8]. These orthoses aim at restoring physiological ankle kinematics and dynamics by supporting the foot of the affected limb, especially in the swing phase of walking. While standard AFOs are mainly designed to support the foot and ankle in the swing phase of walking, PD-AFOs can also address impairments and deficits of the ankle plantarflexor muscles by incorporating energy-storing and -returning mechanisms into their design. For this purpose, variable-stiffness mechanical springs or the high elastic properties of composite materials have been used to store energy and to mimic the physiological gait pattern [
1,
3,
7,
9,
10,
11]. This ability to store and return energy effectively reduces the reliance on muscle activation, leading to lower energy expenditure and improved gait efficiency. According to Bregman et al. [
12], around a 10% decrease in energy cost can be achieved by walking with a PD-AFO. Brehm et al. [
13] reported a significant 9% lower net non-dimensional energy cost of walking in a population of children walking with either a posterior leaf spring or a solid ankle–foot orthosis. In the systematic review by Daryabor et al. [
14], four studies reported a significant reduction in total and net energy cost using different types of AFOs in people with stroke. Bleyenheuft et al. [
15] reported an almost significant reduction in energy cost with either a posterior leaf spring or the articulated Chignon
® orthosis during treadmill walking. A significant reduction in energy cost was also reported with a carbon-fiber AFO [
16]. The mechanism behind these energy savings is attributed to the ability of PD-AFOs to optimize ankle kinematics and dynamics. PD-AFOs can effectively control ankle plantarflexion and dorsiflexion, reducing excessive ankle movements and promoting more natural gait patterns [
17,
18]. PD-AFOs can also enhance balance, reduce pain, and improve overall quality of life for individuals with gait impairments. Efficient and comfortable walking result in increased participation in activities of daily living and improved social engagement [
19]. It should, though, be highlighted that outcome measures of energy expenditure often differ between studies and AFOs’ performance can be difficult to compare. Normalized oxygen consumption, either in mL/kg/m or mL/kg/min, normalized energy cost in J/kg/m, heart rate, and physiological cost index have all been used to quantify the energetic contribution of dynamic AFOs in different motor tasks. While the net energetic effect of dynamic AFOs is mostly calculated as the difference in energy consumption in gait between AFO and shod (no AFO) conditions, the actual energy stored and released due to the elastic deformation of the orthosis is seldom measured or reported [
3].
The adoption of 3D printing technologies in the production of AFOs offers substantial advantages over traditional plaster casting and manual molding manufacturing methods. While the latter are inherently variable and time-consuming, 3D printing enables the creation of highly personalized orthoses through 3D scanning and 3D modeling tools. This digital workflow allows for precise replication of patient anatomy, leading to devices with improved fit and comfort and which can be tailored to individual patient needs [
20]. Three-dimensionally printed AFOs have shown comparable or superior biomechanical and kinematic effects to conventional AFOs, including improvements in gait speed and foot plantar pressure [
21,
22]. The technology offers advantages such as design optimization, reduced labor and production costs, and weight savings [
23]. Three-dimensional printing techniques such as fused deposition modeling and selective laser sintering allow for the creation of AFOs with mechanical properties similar to traditional carbon-fiber AFOs [
23,
24]. Higher satisfaction and comfort have been reported for 3D-printed AFOs compared to conventional ones, particularly in terms of weight and ease of use [
21,
22]. Furthermore, 3D printing facilitates rapid prototyping and design iterations, allowing for real-time adjustments based on patient feedback or clinical observations. This feature contrasts with the lengthy and iterative nature of traditional orthosis fabrication. The capacity for on-demand production and decentralized manufacturing also enhances accessibility, particularly in remote areas. Additionally, the ability to use a wide variety of materials allows for orthoses to be created with specific mechanical properties which can replicate or improve upon traditional AFOs [
24]. The reduction in material waste and the ability to digitally store orthotic designs, thus reducing time and costs in case a replacement AFO is required, also allow for more efficient and less expensive orthotic care.
Recently, a novel 3D-printed PD-AFO made from fiberglass-reinforced polyamide has been developed for individuals with foot drop dissatisfied with off-the-shelf devices. This PD-AFO has been reported to improve gait parameters and ankle kinematics compared to no-AFO conditions and to be more comfortable than standard polypropylene leaf spring AFOs [
17]. These AFOs can be individually dimensioned to achieve the desired stiffness and, due to the high properties of the polyamide-based composite material, the calf-shell can sustain large angular displacements without plastic deformation and without the need for torsion springs, e.g., as in [
3]. Thus, it is plausible that some elastic energy can be stored and released in the stance phase of gait. While AFOs are designed primarily to prevent excessive plantarflexion during the swing phase, understanding PD-AFO energetics is crucial for optimizing design, especially when ankle plantarflexor muscles are compromised.
Therefore, this pilot study aimed to (1) investigate if any elastic energy is absorbed/released by the novel custom PD-AFO and (2) determine the timing of energy absorption/release during gait. In order to address these aims, the kinematics of the novel 3D-printed dynamic custom AFO were recorded in a population of individuals with foot drop during gait.
2. Materials and Methods
Eight custom PD-AFOs were designed and manufactured for a population of individuals (3F, 5M; age 62.0 ± 13.1 years, BMI 25.8 ± 2.5 kg/m2) affected by unilateral foot drop condition due to compression of the lumbosacral spine. Ethical approval was granted for the study by the local Ethical Committee (0016384, 23 December 2019) and informed consent was signed by all participants in the study.
In all participants, ankle dorsiflexor muscle strength was scored ≤3 according to the Medical Research Council (MRC) scale [
25], whereas the ankle plantarflexor muscles strength was scored ≤4. With the exception of ankle dorsiflexion impairment, all participants showed good residual mobility in the affected limb (i.e., they were capable of walking without crutches or other walking aids albeit with compensations at the lower limb joints). The procedure for the design and production of the AFOs has been previously documented by the same authors [
26]. In summary, the leg and foot of each participant were scanned in upright double-leg standing using a Kinect-based 3D scanner (Microsoft, Redmond, WA, US). The custom PD-AFOs were designed using Blender (version 4.4,
https://www.blender.org/) and aligned to the 3D model of the leg and foot in weight bearing. Anatomical congruence was pursued at the foot plantar surface and at the calf shell to ensure comfort and proper fixation of the AFO to the leg. The calf-shell was aligned to the calf midline, as to be oriented along the anatomical axis of the patient’s tibia. The AFOs were manufactured via selective laser sintering of a fiberglass-reinforced polyamide powder (Windform
® GT, CRP Technology, Modena, Italy). This 3D printing technology allows us to obtain parts with a resolution of about 0.1 mm. Since the stiffness of the present AFO is highly sensitive to the cross-section dimensions of the calf-shell, selective laser sintering is critical to the correct optimization of the AFO mechanical properties. The concave shape of the calf-shell increases the moment of inertia of the cross-section, allowing it to bend almost as a rigid body around the
X-axis as in
Figure 1b, which is designed to be close to the physiological ankle–joint axis [
26]. The bending stiffness of the AFO calf-shell in anatomical plantarflexion (
p) and dorsiflexion (
d) were measured by applying a 15 deg rotation in both directions using a custom apparatus (
Figure 1a) [
27].
An 8-camera motion analysis system (Vicon, Oxford UK) was used to track the position of 20 reflective markers placed on relevant body landmarks of the pelvis, femur, tibia, and foot/footwear according to the IOR-gait protocol [
28]. Three additional markers were placed on the posterior side of the calf-shell of each custom AFO (
Figure 1b). This allowed measuring the relative plantarflexion (
p) and dorsiflexion (
d) angles of the AFO calf-shell with respect to the foot. The ISB recommended convention was used to calculate hip, knee, and ankle joint rotations and the AFO calf-shell flexion/extension in gait [
29]. Ground reaction forces were sampled at 2000 Hz using two force plates embedded in the floor (Kistler, Winterthur, Switzerland). Ankle power was calculated using force plate and kinematic data and normalized to the participant’s body weight (W/kg). Five walking trials at self-selected speed were recorded for each participant in three conditions: wearing the custom AFO (
Figure 1c), wearing an off-the-shelf polypropylene leaf spring AFO (Codivilla Spring, Ottobock, Duderstadt, Germany), and shod (no-AFO). According to the current clinical practice at the authors’ institution, the Codivilla Spring is one of the most recommended off-the-shelf PD-AFOs for individuals with foot drop, when no other significant anatomical alterations are present. Furthermore, the stiffness of the Codivilla Spring is comparable to that of the custom PD-AFOs used here [
30]. For each custom AFO, the resisting torque T(
) in gait can be linearly correlated to the plantarflexion and dorsiflexion angles via the following equations:
where subscripts
p and
d are used to indicate plantarflexion and dorsiflexion directions, respectively. Finally, the AFO work was calculated as the dot product between T(
) and α as follows:
where W
p(
) and W
d(
) represent the energy absorbed and released by the AFO in the stance phase of walking during ankle plantarflexion and dorsiflexion rotations, respectively. W(
) is assumed to be positive (energy released) when vectors T(
) and
have the same direction (plantarflexion or dorsiflexion) and negative (energy absorbed) when they have opposite directions. Work was normalized to the participant’s weight (J/kg).
The non-parametric paired Wilcoxon signed rank test was used to assess the effect of the AFO on kinetic and spatio-temporal parameters (α = 0.05).
3. Results
The measured stiffnesses of the eight custom PD-AFOs were in the range of 0.15–0.23 N*m/deg and 0.10–0.27 N*m/deg in plantarflexion and dorsiflexion, respectively.
Patients walked faster while wearing the PD-AFO with respect to the shod condition (normalized speed AFO = 53.8 ± 14.0 %height/s; normalized speed SHOD = 50.8 ± 15.0 %height/s; p = 0.015). No difference in walking speed was observed with respect to the Codivilla Spring (normalized speed CODIVILLA = 53.6 ± 15.3 %height/s; p > 0.05).
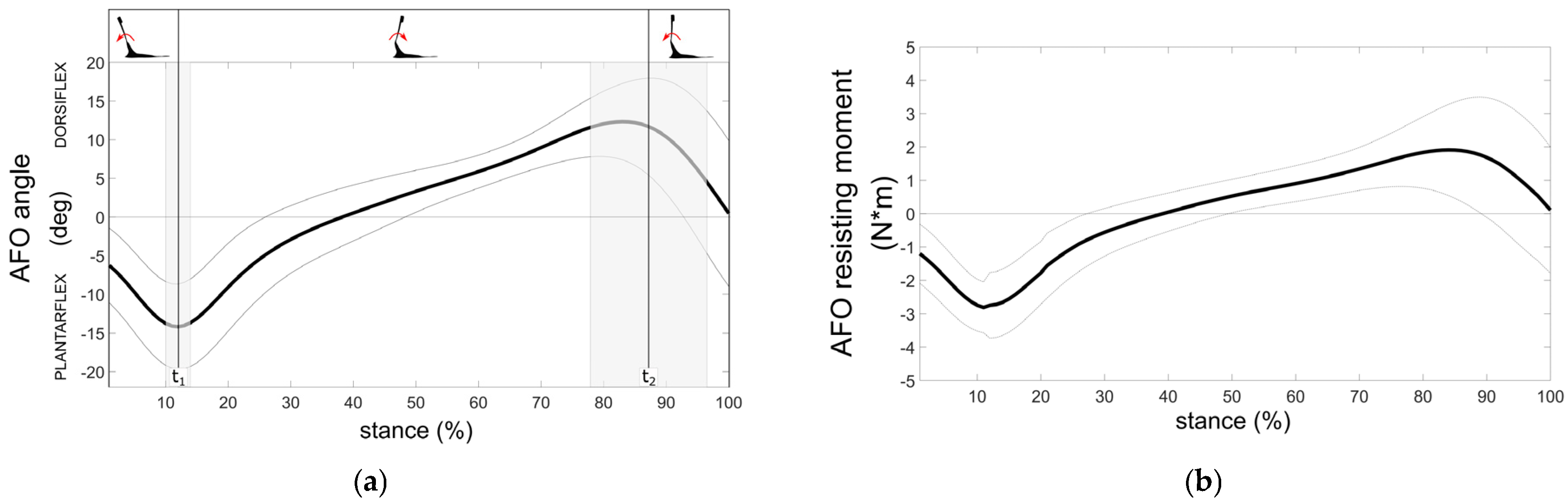
Figure 2a shows the mean temporal profiles (±1SD) of the calf-shell plantarflexion/dorsiflexion angle (deg) during the normalized stance phase duration. Similarly to what is generally observed for ankle motion, plantarflexion of the PD-AFO at early stance is followed by dorsiflexion during midstance and by late-stance plantarflexion. This motion generates a resisting torque due to the PD-AFO stiffnesses k
p and k
d (
Figure 2b).
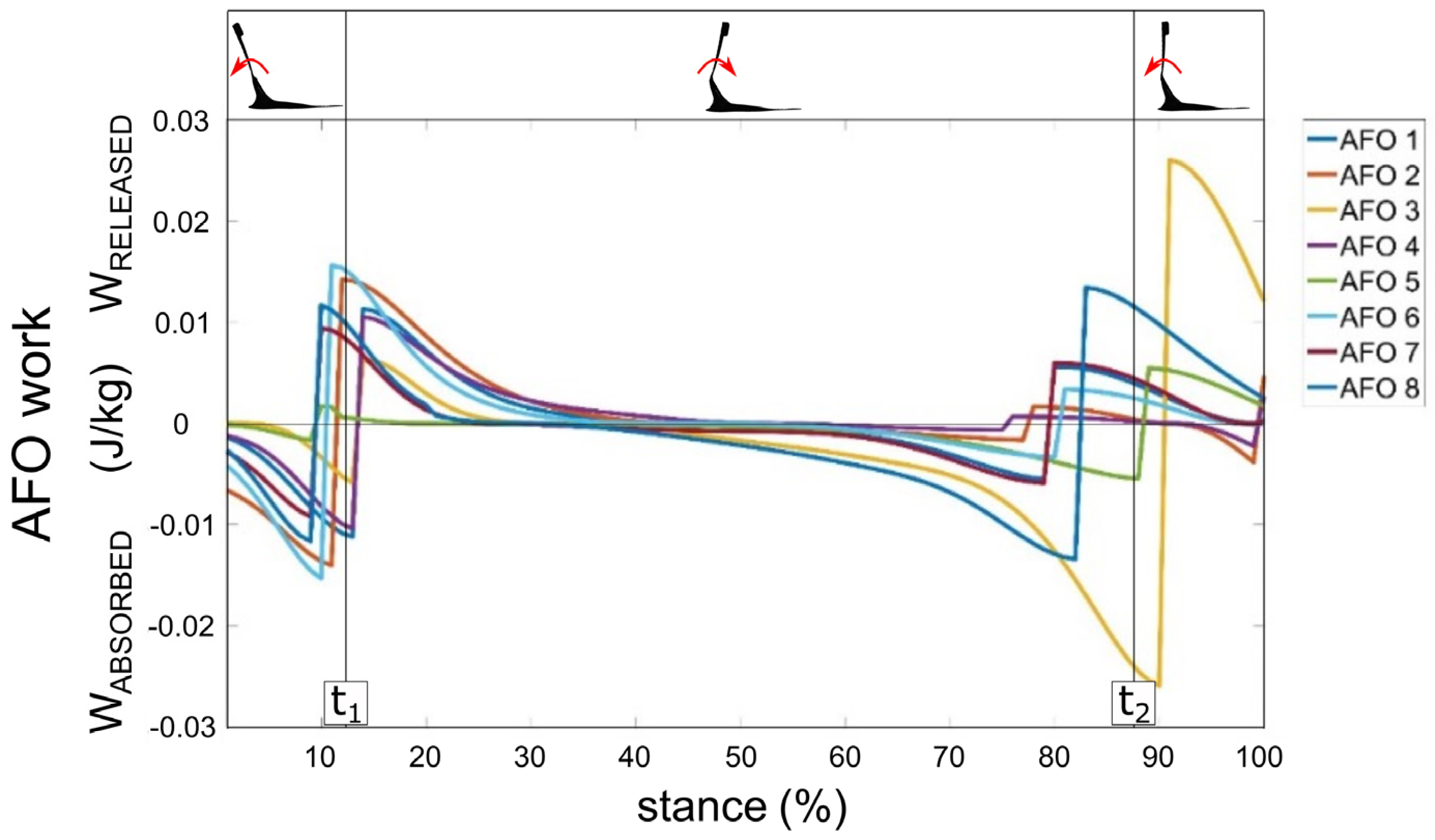
Figure 3 reports the temporal profiles of the work done by each of the eight custom PD-AFOs during the normalized stance phase duration. In all PD-AFOs, energy was absorbed during the load-acceptance phase (1–15% stance) and at late stance (50–90% stance). Energy was released up to midstance (15–50% stance) and during push-off (80–100% stance). At early stance, the maximum energy absorbed and released by the PD-AFOs was 0.011 ± 0.005 J/kg at 12 ± 2% (t
1 in
Figure 3) of the stance phase. At late stance, the maximum energy was 0.008 ± 0.007 J/kg at 88 ± 9% (t
2 in
Figure 3) of the stance phase. The average maximum energy released across the whole stance phase was 0.013 ± 0.005 J/kg.
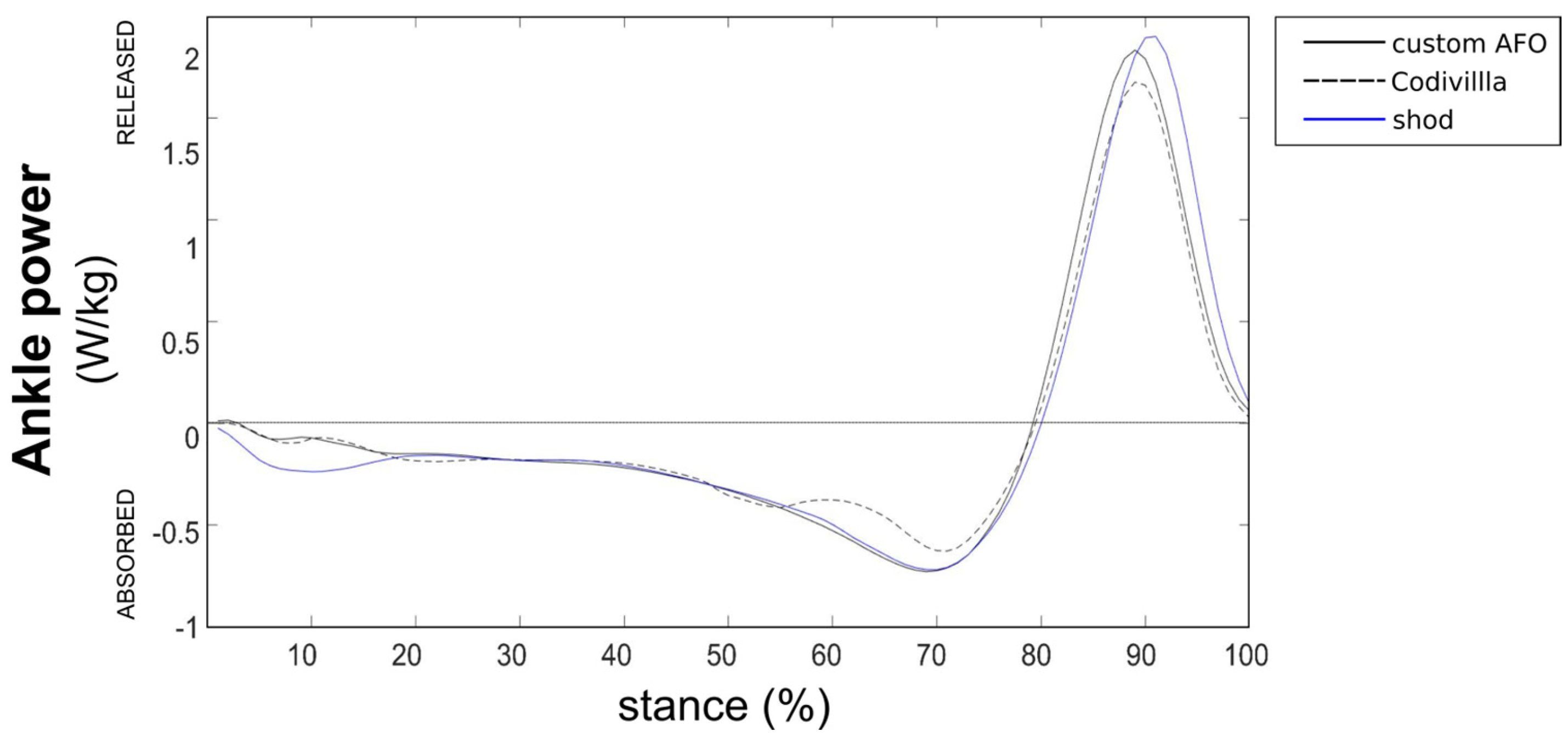
Figure 4 reports the inter-participant mean ankle power during the normalized stance phase duration in the PD-AFO and shod conditions. Although the difference was not statistically significant (
p = 0.06), a trend for reduced maximum normalized ankle power at push-off was observed. This was 1.9 W/kg and 2.0 W/kg, respectively, in the PD-AFO and shod conditions.
4. Discussion
Current advances in 3D printing technologies have enhanced the production of custom orthopedic devices fitting patients’ anatomy and with personalized mechanical properties. While 3D-printed custom orthoses are still more expensive than similar off-the-shell solutions, the costs are increasingly offset by the higher performance and the better comfort. In addition, significant anatomical alterations can only be addressed by such custom devices. PD-AFOs are recommended for individuals with mild foot drop instability, which may also need support in the push-off phase of walking due to weakness or insufficiency of the ankle plantarflexor muscles. While several commercial and custom AFOs are reported in the literature for different lower limb pathologies, only a few studies have investigated the energetics of PD-AFOs with respect to their design and mechanical properties [
9,
11]. In this study, we aimed at calculating the energetics of a novel custom PD-AFO in a population of individuals with mild foot drop condition.
Quantifying the energetic effects of a novel custom AFO in patients with foot drop is crucial for several reasons. First, this study provides objective, data-driven evidence of the AFO’s energetic contribution to gait dynamics. In vivo biomechanical measurements offer a quantitative assessment of how the device influences patients’ physiological exertion during ambulation, adding instrumental evidence to the subjective evaluations on comfort and ease of use. This is essential for validating the AFO’s potential to enhance functional mobility. Second, by quantifying the AFO’s impact on energy expenditure, clinicians can make informed decisions regarding prescription and customization of the device. Understanding the energetic benefits allows for personalized treatment plans, optimizing design and stiffness properties to maximize patient outcomes. This is particularly vital for patients with chronic conditions, where even small reductions in the metabolic cost per gait cycle can substantially improve quality of life. Furthermore, this study contributes to the broader scientific understanding of AFO interventions. These investigations allow researchers to better correlate AFO design parameters with AFO mechanics in gait and to identify key biomechanical parameters influencing AFO effectiveness. This knowledge can drive the development of more efficient and patient-centered orthotic solutions for foot drop and other gait impairments.
The present PD-AFOs were characterized by relatively low bending stiffness with respect to the average data reported for individuals with similar conditions. While no specific data are available in the literature to establish the correct stiffness of PD-AFOs for different degrees of ankle dorsi/plantarflexion deficits, in this study, a reference stiffness was used and adjusted according to the weight of each participant. Low bending stiffness allows for better foot and ankle dynamics in gait as it minimizes the restraint of the ankle in dorsiflexion, while providing sufficient support to resist passive ankle plantarflexion. A gait analysis study by Kerkum et al. [
3] on a population of children with cerebral palsy estimated the net work of a flexible AFO featuring a stiffness in plantarflexion similar to that of the present custom PD-AFO (0.11 ± 0.13 N*m/deg), albeit more rigid in dorsiflexion (0.7 ± 0.2 N*m/deg) by about 0.03 J/kg. Although not directly comparable to what measured here, Bregman et al. reported a positive work of 0.06 W/kg for AFOs with stiffness ranging from 1.4 to 23.5 N*m/deg [
12]. Despite the relatively low stiffness of the present PD-AFO, the ankle plantarflexion angle was significantly lower (
p < 0.05) in the swing phase when wearing the custom PD-AFO with respect to the shod condition [
17]. All participants in this study were affected by a foot drop condition, but only some of them suffered also from mild plantarflexion deficit. These individuals are likely to benefit the most by using low-stiffness PD-AFOs, as excessive rigidity of the calf-shell in plantarflexion would hinder the ankle joint physiological mobility in the push-off phase. Although further validation through a larger clinical trial is warranted, preliminary evidence seems to suggest that individuals with foot drop exhibiting mild plantarflexion weakness may benefit from PD-AFOs characterized by minimal plantarflexion stiffness. Consequently, a subsequent study will be designed to quantify the minimum plantarflexion stiffness of a PD-AFO necessary to provide adequate foot and footwear support during the swing phase of gait.
As far as the outcome of the present energetic analysis, the temporal profiles of the work calculated over the normalized stance phase duration were rather consistent across PD-AFOs (
Figure 4). At foot contact, all PD-AFOs absorbed some energy by plantarflexing the calf-shell, which was released to the ankle up to midstance. Subsequently, energy was absorbed to dorsiflex the calf-shell up to about 90% of the stance phase. This energy was released to the ankle at push-off. It is therefore plausible that this, albeit small, amount of energy may be used to improve foot and ankle propulsion at late stance or to decrease the amount of ankle net work required to walk at the same walking speed. Indeed, while the participants walked faster when wearing the PD-AFO with respect to the shod condition, the power released at the ankle was lower, albeit not statistically significant, in the PD-AFO condition. Although a larger dataset is needed to establish a correlation between varying AFO stiffness and gait expenditure relative to ankle plantar flexor deficits, this study provides a foundation for individualized prescription guidelines for AFOs in drop foot conditions.
These results should be critically assessed with respect to some limitations. Since no direct comparison with other custom AFO designs was performed in the same testing conditions, it is difficult to assess how the present low-stiffness design performs with respect to other—more rigid—custom dynamic AFOs. While the outcome of the energetic analysis was rather consistent across participants, the limited sample size prevents the present energetic data to be representative of the varying nature of the foot drop condition. Indeed, a larger foot drop population would allow us to include different walking patterns that may affect the present outcome. In addition, due to its flexibility, the AFO foot plate can also store and release some energy in the push-off phase and during metatarsophalangeal joint dorsiflexion and plantarflexion. Thus, it can be hypothesized that the actual positive work released to the ankle could be larger than what reported in this study by analyzing the energetics of the calf-shell only. Furthermore, no follow-up evaluations were conducted thus the long-term energetics of the PD-AFO, its effect on ankle power, and the biomechanical adaptations or changes in performance following familiarization.