The Effects of Periodontal Laser Therapy on Pain in Adult Patients with Orthodontic Treatment: A Randomized Clinical Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Subject Selection
- -
- Age between 18 and 55 years;
- -
- Presence of dentoalveolar disharmony (DAD) with mild crowding (3–7 mm);
- -
- No prior orthodontic treatment;
- -
- No prior anti-inflammatory treatment (NSAIDs).
- -
- Presence of carious lesions;
- -
- Signs of active periodontal disease;
- -
- Lesions of the oral mucosa;
- -
- Systemic conditions that have an impact on periodontal tissues (diabetes, immunological conditions, acute articular rheumatism, tuberculosis, etc.).
2.3. Periodontal Status
2.4. Orthodontic Protocol
2.5. LLLT Protocol
2.6. Statistical Analysis
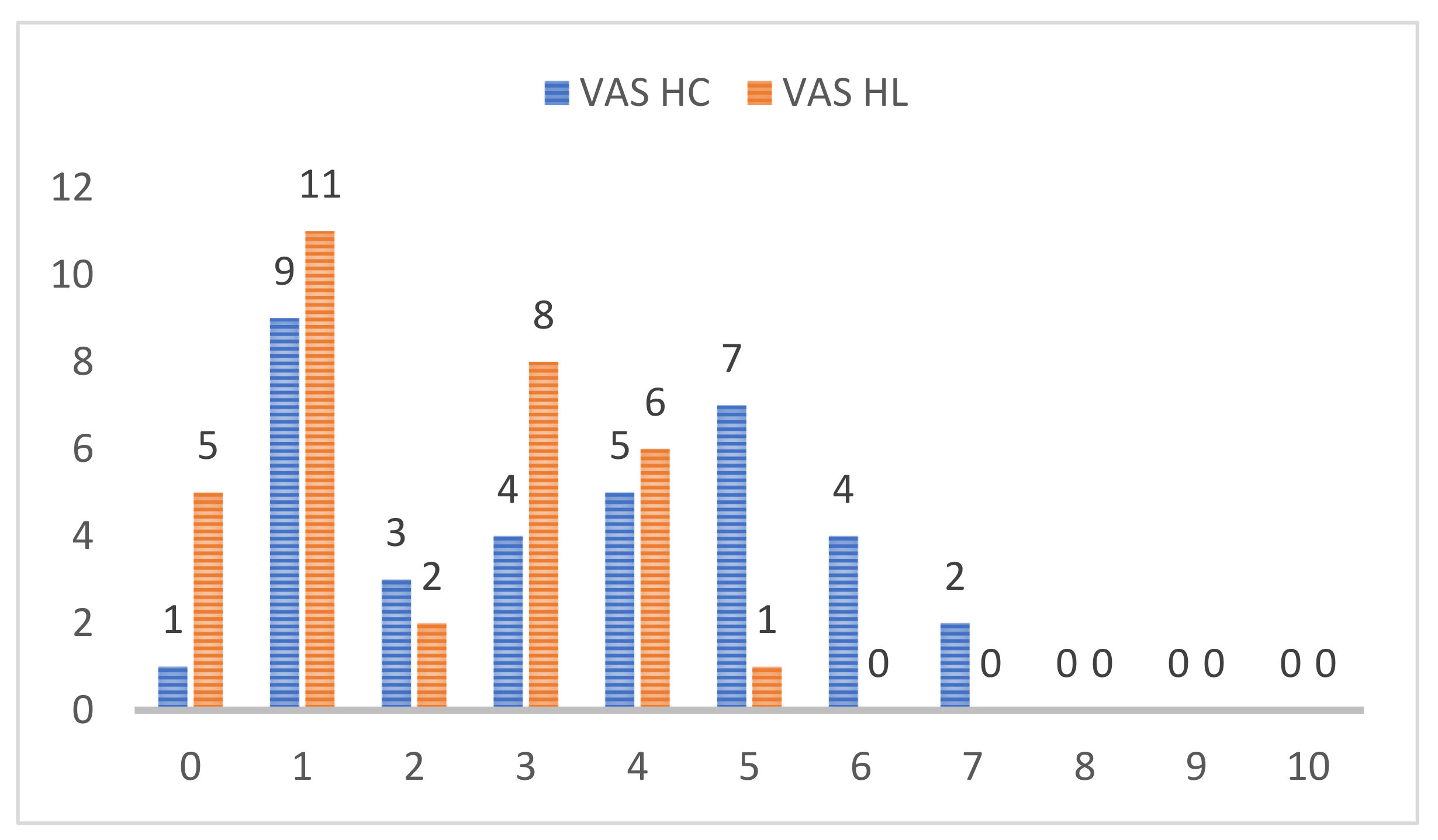
3. Results
4. Discussion
Limitations of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bergius, M.; Berggren, U.; Kiliaridi, S. Experience of pain during an orthodontic procedure. Eur. J. Oral Sci. 2002, 110, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Erdinc, A.M.; Dincer, B. Perception of pain during orthodontic treatment with fixed appliances. Eur. J. Orthod. 2004, 26, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Sonesson, M.; de Geer, E.; Subraian, J.; Petren, S. Efficacy of low-level laser therapy in accelerationg tooth movement, preventing relapse and managing acute pain during othodontic treatment in humans: A systematic review. BMC Oral Health 2017, 17, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scribante, A.; Gallo, S.; Celmare, R.L.; D’Anto, V.; Grippaudo, C.; Gandini, P.; Sfondrini, M.F. Orthodontic debonding and tooth sensitivity of anterior and posterior teeth: A prospective clinical trial. Angle Orthod. 2020, 90, 766–773. [Google Scholar] [CrossRef]
- Tecco, S.; D’Attilio, M.; Tetè, S.; Festa, F. Prevalence and type of pain during conventional and self-ligating orthodontic treatment. Eur. J. Orthod. 2009, 31, 380–384. [Google Scholar] [CrossRef]
- Li, Y.; Jacox, L.A.; Little, S.; Ko, C.C. Orthodontic tooth movement: The biology and clinical implications. Kaoshiung J. Med. Sci. 2018, 34, 207–2014. [Google Scholar] [CrossRef] [Green Version]
- Feller, L.; Khammissa, R.A.G.; Schechter, I.; Moodley, A.; Thamadakis, G.; Lemmer, J. Periodontal biological events associated with orthodontic tooth movement: The biomechanics of the cytoskeleton and the extracellular matrix. Sci. World J. 2015, 8, 11–17. [Google Scholar] [CrossRef] [Green Version]
- Vandevska-Radunovic, V. Neural modulation of inflammatory reactions in dental tissues incident to orthodontic tooth movement. A review of the literature. Eur. J. Orthod. 1999, 21, 231–247. [Google Scholar] [CrossRef]
- Popa, C.G.; Luchian, I.; Ioanid, N.; Goriuc, A.; Martu, I.; Bosinceanu, D.; Martu, M.A.; Tirca, T.; Martu, S. ELISA Evaluation of RANKL Levels in Gingival Fluid in Patients with Periodontitis and Occlusal Trauma. Rev. Chim. 2018, 69, 1578–1580. [Google Scholar] [CrossRef]
- Wilson, S.; Ngan, P.; Kess, B. Time course of the discomfort in young patients undergoing orthodontic treatment. Pediatr. Dent. 1989, 11, 107–110. [Google Scholar]
- Matys, J.; Jaszsczak, E.; Flieger, R.; Kostrzewska-Kaminiarz, L. Effect of ozone and diode laser (635 nm) in reducing orthodontic pain in the maxillary arch—A randomized clinical controlled trial. Lasers Med. Sci. 2020, 35, 487–496. [Google Scholar] [CrossRef] [Green Version]
- Scribante, A.; Gallo, S.; Pascadopoli, M.; Soleo, R.; di Fonso, F.; Politi, L.; Venugopal, A.; Marya, A.; Butera, A. Management of periodontal disease with adjuvant therapy with ozone and photobiomodulation (PBM): A randomized clinical trail. Photonics 2022, 9, 138. [Google Scholar] [CrossRef]
- Scribante, A.; Butera, A.; Alovisi, M. Customized minimally invasive protocols for the clinical and microbiological management of the oral microbiota. Microorganisms 2022, 10, 675. [Google Scholar] [CrossRef]
- Xiaoting, L.; Yin, T.; Yangxi, C. Interventions for pain during fixed orthodontic appliance therapy. A systematic review. Angle Orthod. 2010, 80, 925–932. [Google Scholar] [CrossRef]
- Li, F.J.; Zhang, J.Y.; Zeng, X.T.; Guo, Y. Low-level laser therapy for orthodontic pain: A systematic review. Laser Med. Sci. 2015, 30, 1789–1803. [Google Scholar] [CrossRef]
- Sakurai, Y.; Yamaguchi, M.; Abiko, Y. Inhibitory effect of low-level laser irradiationon LPS-stimulated prostaglandin E2 production and cyclooxygenase-2 in human gingival fibroblasts. Eur. J. Oral Sci. 2000, 108, 29–34. [Google Scholar] [CrossRef]
- Ren, C.; McGrath, C.; Yang, Y. The effectiveness of low-level diode laser therapy on orthodontic pain management: A systematic review and meta-analysis. Laser Med. Sci. 2015, 30, 1881–1893. [Google Scholar] [CrossRef] [Green Version]
- Song, W.; Yinan, C.J.Z.; Wenjing, C.; Sheng, S.; Huijie, S.; Ling, Z.; Ping, Y.; Svensson, P.; Wang, K. Effect of low-level laser therapy on tooth-related pain and somatosensory function evoked by orthodontic treatment. Int. J. Oral Sci. 2018, 10, 56–60. [Google Scholar]
- Isola, G.; Matarese, M.; Briguglio, F.; Grassia, V.; Picciolo, G.; Fiorillo, L.; Matarese, G. Effectiveness of low-level laser therapy during tooth movement: A randomized clinica trial. Materials 2019, 12, 2187. [Google Scholar] [CrossRef] [Green Version]
- Deana, N.F.; Zaror, C.; Sandoval, P.; Alves, N. Effectiveness of low-level laser therapy in reducing orthodontic pain. A systematic review and meta-analysis. Pain Res. Manag. 2017, 2017, 8560652. [Google Scholar] [CrossRef]
- Silveira, P.C.; Silva, L.A.; Freitas, T.P.; Latini, A.; Pinho, L.A. Effects of low-power laser irradiation (LPLI) at different wave lengths and doses on oxidative stress and fibrogenesis parameters in ananimal model of wound healing. Laser Med. Sci. 2011, 26, 125–131. [Google Scholar] [CrossRef]
- Lim, H.M.; Lew, K.K.; Tay, D.K. A clinical investigation of the efficacy of low level laser therapy in reducing orthodontic postadjustment pain. Am. J. Orthod. Dentofac. Orthop. 1995, 108, 614–622. [Google Scholar] [CrossRef]
- Abtahi, S.M.; Mousavi, S.A.; Shafaee, H.; Tanbakuchi, B. Effect of low-level laser therapy on dental pain induced byseparator force in orthodontic treatment. Dent. Res. J. 2013, 10, 647–651. [Google Scholar]
- Guram, G.; Reddy, R.K.; Dharamsi, A.M.; Ismail, P.M.S.; Mishra, T.; Prakashkumar, M.D. Evaluation of low-level laser therapy on orthodontic tooth movement: A randomized control study. Contemp. Clin. Dent. 2018, 9, 105–109. [Google Scholar]
- Kim, W.T.; Bayome, M.; Park, J.B.; Park, J.H.; Baek, S.H.; Kook, Y.A. Effect of frequent laser irradiation on orthodontic pain. A single blind randomized clinical trial. Angle Orthod. 2013, 83, 611–616. [Google Scholar] [CrossRef]
- Tortamano, A. Low-level laser therapy for pain caused by placement of the first orthodontic archwire: A randomized clinical trial. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 662–667. [Google Scholar] [CrossRef]
- Turhani, D.; Scheriau, M.; Kapral, D.; Benesch, T. Pain relief by single low-level laser irradiation in orthodontic patients undergoing fixed appliance therapy. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 371–377. [Google Scholar] [CrossRef]
- Martu, A.; Agop-Forna, D.; Luchian, I.; Toma, V.; Picus, M.; Solomon, S. Influence of laser therapy as an adjunct to periodontaly optimizing orthodontic tooth movement. Rom. J. Oral Rehabil. 2019, 11, 161–169. [Google Scholar]
- Sobouti, F.; Rakhshan, V.; Chiniforush, N.; Khatami, M. Effects of laser-assisted cosmetic smile lift gingivectomy on postoperative bleeding and pain in fixed orthodontic patients: A controlled clinical trial. Prog. Orthod. 2014, 15, 66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abi-Ramia, L.B.; Stuani, A.S.; Stuani, A.S.; Stuani, M.B.S.; Moares Mendes, A. Effects of low-level laser therapy and orthodontic tooth movement on dental pulps in rats. Angle Orthod. 2010, 80, 116–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borzabadi-Farahani, A. The adjunctive soft-tissue diode laser in orthodontics. Compend. Contin. Educ. Dent. 2017, 38, e18–e31. [Google Scholar] [PubMed]
- Mârțu, S.; Amălinei, C.; Tatarciuc, M.; Rotaru, M.; Potârniche, O.; Liliac, L.; Căruntu, I.D. Healing process and laser therapy in the superficial periodontium: A histological study. Rom. J. Morophol. Embryol. 2012, 53, 111–116. [Google Scholar]
- Mizutani, K.; Musya, Y.; Wakae, K. A clinical study on serum prostaglandin E2 with low-level lasertherapy. Photomed. Laser Surg. 2004, 22, 537–539. [Google Scholar] [CrossRef] [PubMed]
- Sioustis, I.A.; Martu, M.A.; Aminov, L.; Pavel, M.; Cianga, P.; Kappenberg-Nitescu, D.C.; Luchian, I.; Solomon, S.M.; Martu, S. Salivary metalloproteinase-8 and metalloproteinase-9 evaluation in patients undergoing fixed orthodontic treatment before and after periodontal Therapy. Int. J. Environ. Res. Public Health 2021, 18, 1583. [Google Scholar] [CrossRef]
- Luchian, I.; Martu, M.A.; Tatarciuc, M.; Scutariu, M.M.; Ioanid, N.; Pasarin, L.; Kappenberg-Nitescu, D.C.; Sioustis, I.A.; Solomon, S.M. Using fem to assess the effect of orthodontic forces on affected periodontium. Appl. Sci. 2021, 11, 7183. [Google Scholar] [CrossRef]
- Ronen, A.; Shochat, T.; Eidelman, L. Sex differences in physiological responses to pain throughout surgical procedures. Harefuah 2017, 1, 342–344. [Google Scholar]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lazăr, A.-P.; Dakó, T.; Bud, A.; Vlasa, A.; Ormenișan, A.; Mârțu, M.-A.; Păcurar, M.; Lazăr, L. The Effects of Periodontal Laser Therapy on Pain in Adult Patients with Orthodontic Treatment: A Randomized Clinical Trial. Appl. Sci. 2022, 12, 3601. https://doi.org/10.3390/app12073601
Lazăr A-P, Dakó T, Bud A, Vlasa A, Ormenișan A, Mârțu M-A, Păcurar M, Lazăr L. The Effects of Periodontal Laser Therapy on Pain in Adult Patients with Orthodontic Treatment: A Randomized Clinical Trial. Applied Sciences. 2022; 12(7):3601. https://doi.org/10.3390/app12073601
Chicago/Turabian StyleLazăr, Ana-Petra, Timea Dakó, Anamaria Bud, Alexandru Vlasa, Alina Ormenișan, Maria-Alexandra Mârțu, Mariana Păcurar, and Luminița Lazăr. 2022. "The Effects of Periodontal Laser Therapy on Pain in Adult Patients with Orthodontic Treatment: A Randomized Clinical Trial" Applied Sciences 12, no. 7: 3601. https://doi.org/10.3390/app12073601
APA StyleLazăr, A.-P., Dakó, T., Bud, A., Vlasa, A., Ormenișan, A., Mârțu, M.-A., Păcurar, M., & Lazăr, L. (2022). The Effects of Periodontal Laser Therapy on Pain in Adult Patients with Orthodontic Treatment: A Randomized Clinical Trial. Applied Sciences, 12(7), 3601. https://doi.org/10.3390/app12073601






