Abstract
Tooth eruption disturbances associated with developmental odontogenic cysts represent a particular challenge in orthodontic treatment. Early diagnosis, crucial for prompt and effective therapy, is possible with a thorough radiological analysis. Three-dimensional digital images provided by CBCT are indispensable to establish an interdisciplinary orthodontic–surgical treatment plan. The aim of this paper is to present a case of an odontogenic cyst in a nine-year-old male patient. Particular attention is paid to radiological findings, possible therapeutic approaches and potential complications connected with an attempt to improve the alignment of teeth. Orthodontic implications associated with cysts in growing patients are widely described according to clinical observations and literature review.
1. Introduction
Among all the possible causes of tooth eruption disturbances, the root cause is a physical barrier on the eruption path. The problem can result from a lack of space in the dental arch, which is often encountered and treated in orthodontic practice; however, a less frequent but more severe cause is existing soft or hard tissue pathology in the area of the developing tooth germ. The presence of a lesion can be asymptomatic and may be diagnosed by chance during an X-ray performed as a regular part of an orthodontic examination. In many cases, the only problem with the patient is dental malalignment. However, the increasing size of a lesion leads to serious consequences, including mobility of adjacent teeth, root resorption, extensive deterioration of bone structure, facial asymmetry and inflammatory symptoms [1].
According to the literature, a dentigerous cyst (described also as a follicular cyst) associated with unerupted teeth is the most frequent among cyst-like lesions [1,2]. On the basis of a histopathological survey performed by Mohamed et al. in a group of patients under 10 years of age, this type of pathology was predominant [2]. It is estimated that 10% of impacted teeth are associated with a dentigerous cyst, and the most common location is the area of the third mandibular molars and maxillary canines [3]. Other frequent cysts and tumors that can be concomitant with eruption disturbance are presented in Table 1. As stated in previous research, there is no significant correlation between the histological diagnosis and location of an unerupted tooth in the dental arch [3]. In some cases, clinical and radiological findings are inconclusive and may suggest an inflammatory cyst or ameloblastoma. Unlike an inflammatory lesion, a dentigerous cyst is not associated with symptoms of inflammation such as pulpitis of the periodontitis. Unicystic ameloblastoma can mimic a dentigerous cyst, especially when associated with an unerupted tooth. Both lesions are radiologically well defined and unilocular. In these cases, only microscopic observation of the characteristic ameloblastomatous epithelium can provide a proper differential diagnosis [4,5].

Table 1.
The most frequent cyst and tumors associated with unerupted teeth in growing patients.
2. Preliminary Diagnosis Based on Radiological Examination
Orthodontists are often the first specialists that can diagnose the presence of dental pathology, especially in growing patients. Radiographs are a routine part of the diagnostic process and treatment planning. In addition to providing basic information about the presence and position of unerupted teeth, OPG can be used as a screening method for the indication of asymptomatic hard tissue anomalies [9]. Crucial in OPG interpretation are the size of the lesion, its relation to anatomical structures, its internal complexity and the appearance of its borders [6,10]. The margins of the lesion are important in preliminary diagnosis and serve as a prognostic factor. Well-defined peripheries, which can be sclerotic or noncorticated, usually suggest the benign nature of a lesion. Nondefined margins can be diffused or invasive, which raises the suspicion of malignancy [6,10]. According to a radiographic study conducted by Langaroodi et al. [11], a nonaggressive odontogenic cyst and tumors are mostly single focal with visible borders and show a radiolucent image. Tooth germ involvement and displacement or root resorption that can coexist with benign lesions are particularly important findings for orthodontists. A greater root resorption tendency is observed in ameloblastoma, while dentigerous cysts more often dislocate roots rather than resorb them [12]. In more severe cases, enlargement of the pathology can lead to displacement of the floor of the maxillary sinus or pathological fracture of the mandible (depending on the location) [11,12].
3. Treatment Plan Supported with Radiological Analysis
Histopathological recognition supported by proper interpretation of OPG is the foundation for diagnosis. However, two-dimensional radiograph images have many limitations. The most significant are magnification and distortion of the image. Even if the patient is positioned properly, the object is enlarged by about 15–25% [12,13]. Moreover, magnification depends on the individual jaw shape and the area of the dental arch and is most apparent in the canine region [13]. Another problem is the overlap of structures and reflections of anatomical structures that can hinder interpretation [12]. Because of the reasons described above, panoramic X-rays are not sufficient to establish a treatment plan that demands a multidisciplinary approach; therefore, a cone-beam computed tomography (CBCT) examination is recommended. In order to plan optimal surgical access, surgeons need precise, three-dimensional information about the size and extent of the lesion that is not visible on the buccolingual display in OPG. Orthodontists require the accurate location of unerupted teeth, especially their spatial position relative to the roots of adjacent teeth, to assess the potential risk of root resorption during orthodontic traction [14]. The evaluation of alveolar boundary conditions is another crucial factor that determines orthodontic mechanics [15]. Measurements should include vertical and buccolingual dimensions of the alveolar bone, as well as the relationship with the position of teeth. CBCT helps to determine the boundary of tooth movement to avoid iatrogenic fenestrations and dehiscence [15,16].
In a study presented by Haney et al. [17], conventional radiographs were compared with CBCT according to their utility in establishing a treatment plan for impacted maxillary canines. The change from the 2D technique to 3D imaging resulted in a difference in the assessment of the actual mesiodistal (21%) and labiopalatal (16%) cusp tip position, which brought about modifications in the treatment approach [17].
An example of CBCT implementation in an orthodontic treatment plan is 3D biomechanics [15]. Because each patient with an odontogenic cyst presents a unique problem to solve, morphological reconstructions obtained with CBCT can be useful in planning the individual position of every orthodontic attachment and achieving a proper force vector. The distance of the virtual bracket from the center of resistance can be visualized, the tipping or translational movement can be better predicted, and the anchorage can be controlled [15].
4. Treatment Methods for Odontogenic Cyst-like Lesions
Two main surgical approaches can be applied, depending on the patient’s age and the size of the lesion (Table 2) [3,18,19]. The first, more radical method is aimed to remove the cyst completely in a one-step procedure called enucleation. The second approach, performed in various modifications (i.e., marsupialization, decompression), is focused on reducing the intracystic pressure to preserve the surrounding tissues and unerupted cyst-associated permanent teeth. This minimally invasive treatment is a gold standard in growing patients [19,20].

Table 2.
Two main surgical treatment methods for cyst-like odontogenic lesions.
A search in the PubMed/MEDLINE database revealed 49 articles describing the orthodontic–surgical approach to dentigerous cyst treatment in the last decade, 12 of which were published in the last 5 years and are summarized in Table 3 [18,19,20,21,22,23,24,25,26,27,28,29].

Table 3.
Summary of case reports from 2016 to 2021.
Hauer et al. [18] presented an alternative treatment approach for dentigerous cysts in growing patients. Taking the possible disadvantages of marsupialization into account, the authors suggested a single-step procedure containing cystectomy (enucleation) with the successful salvage of a cyst-associated permanent tooth. Surgical access to the lesion was similar to the standard enucleation procedure; however, in the area of the unerupted tooth, an incision was made to sharply separate the dental crown from the cystic wall (at the level of the cementoenamel junction). As a result, the tooth gained the ability to erupt without orthodontic traction. Although the researchers achieved promising results, the number of presented cases (7 patients, 15 cyst-associated teeth) is still not sufficient to consider this method as a new, risk-reduced treatment method [18].
5. Case Report
A nine-year-old male patient was referred for treatment to the Department of Orthodontics of the Central Teaching Hospital, Institute of Dentistry, Medical University of Lodz. Apart from an allergy to tree and grass pollen, the patient did not report any other relevant general disorders from an orthodontic perspective. Starting with an extraoral examination, facial asymmetry was revealed, visible as painless swelling that deformed the nasolabial sulcus (Figure 1). The submandibular lymph nodes on the right side were enlarged, hard, painless and movable relative to the skin and surrounding tissues.

Figure 1.
Extraoral photographs before treatment.
A functional assessment of the masticatory system did not reveal any kinematic jaw alteration. The movements of the mandible were symmetric, and their range was normal. Intraorally, mixed dentition was present with increased overjet and bilateral ½ cusp angle class II malocclusion. The oral vestibulum, in the area of the upper right primary canine (53) and first molar (54), was deformed due to alveolar bone expansion, and the overlying mucosa was red and swollen (Figure 2). The patient was referred for a radiological examination, as well as for a consultation at the Department of Oral Surgery.

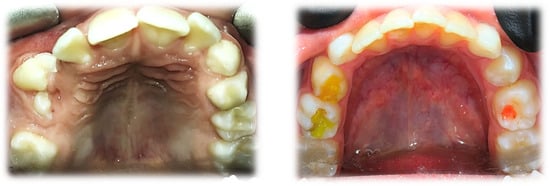
Figure 2.
Intraoral photographs before treatment.
A preliminary investigation with a panoramic radiogram was ordered to disclose the presence of erupted and unerupted teeth with their possible developmental or positional abnormalities, as well as to assess the condition of surrounding maxillofacial structures. The radiolucent, unilocular area with a diameter of approximately 3 cm, extending in the area above Teeth 53 and 54, was observed (Figure 3).

Figure 3.
OPG before treatment.
That finding necessitated further diagnostics with CBCT (Figure 4, Figure 5, Figure 6 and Figure 7). A 3D radiograph confirmed a round, well-demarcated, noninflammatory cyst-like lesion extending from Teeth 11 to 15.
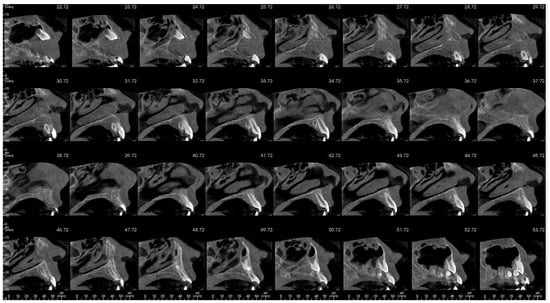
Figure 4.
CBCT before treatment—sagittal view.
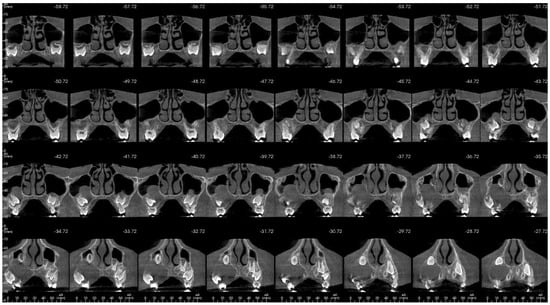
Figure 5.
CBCT before treatment—axial view.
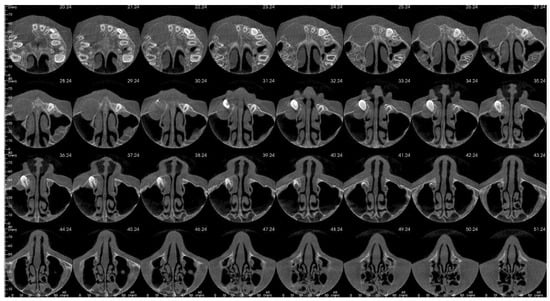
Figure 6.
CBCT before treatment—coronal view.
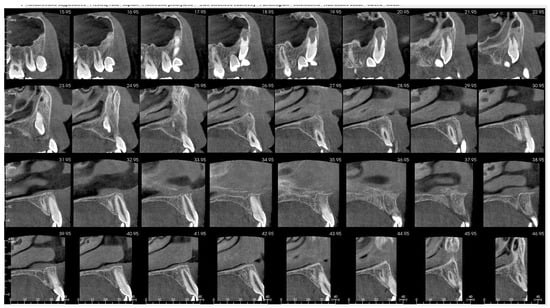
Figure 7.
OPG 3 months after surgery.
A hypodense focus representing a loss of osseous tissue surrounded the crown of the displaced upper right permanent canine. The unerupted first and second premolars were dislocated and rotated, and Tooth 12 also presented mesiorotation and mesioinclination. The teeth involved in the lesion had open apices and no sign of root resorption. The alveolar bone was deformed, especially in the vestibulopalatal dimension, with a noticeable displacement of the medial interior wall of the right maxillary sinus.
The extended diagnostic process also included a blood test with the level of thyroid hormones (TSH, fT3, fT4), and it did not reveal any deviation from standard. A microscopic verification by means of aspiration cytological biopsy was also performed. The result confirmed the cystic character of the pathology and denied the presence of a neoplastic lesion.
An interdisciplinary treatment plan was established to achieve the best therapeutic result and reduce the risk of complications. The first surgical step included a minimally invasive approach, and marsupialization was the method of choice. After the procedure, an alginate impression was taken, and an acrylic obturator was made. The aim was to maintain communication between the cyst and the oral cavity and reduce intracystic pressure. This helped to prevent the accumulation of debris in the post-surgery area and the formation of a fibrous scar that could be an obstacle to the eruption of teeth. A follow-up with radiological assessment was performed 2, 4 and 6 months after marsupialization. The size of the lesion decreased rapidly, and the unerupted 13 gradually migrated into a more promising position (Figure 7, Figure 8, Figure 9, Figure 10 and Figure 11). After 6 months, a second surgery was performed to remove the whole lesion. Bone scrapings were sent for histopathological verification. The examination confirmed a cyst composed of loose connective tissue. The epithelial lining was thin and acantholytic.

Figure 8.
CBCT 6 months after surgery—sagittal view.
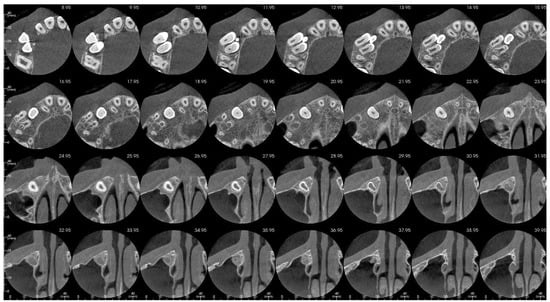
Figure 9.
CBCT 6 months after surgery—axial view.
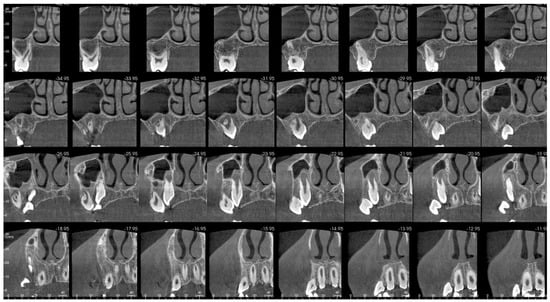
Figure 10.
CBCT 6 months after surgery—coronal view.
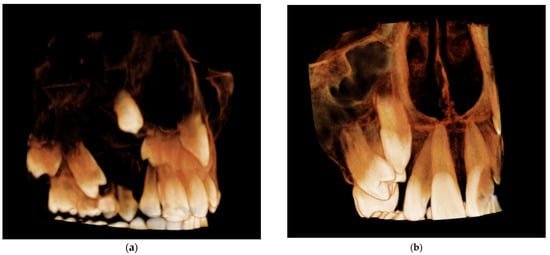
Figure 11.
Comparison of three-dimensional CBCT reconstruction before surgery (a) and 6 months after surgery (b).
The initial orthodontic treatment plan required modification. Primarily, it was assumed that the traction of 13 would be required. This meant the need for the surgical exposure of the 13 crown, bonding of the attachment to the enamel surface and the application of an orthodontic fixed appliance in the upper dental arch. However, regular observations of 13 movement led to anticipating a spontaneous eruption on the condition that it would not be hindered by the malposition of Teeth 14 and 15. For this reason, the surgical exposure was unfounded. The aim of further orthodontic procedures was a distal movement of 14 and 15, to release the 13 eruption path. This was performed by an initial alignment with the aid of a specially designed transpalatal arch. On the right side, palatally from the first molar, an additional loop and a hook were added to a wire to enable the attachment of the elastic chain and provide a force to derotate the upper right second premolar (Figure 12). Subsequently, an attempt of derotation and alignment of the upper right first premolar was undertaken. However, due to the severe vestibuloposiotion of 14 and unfavorable alveolar boundary conditions, cautious orthodontic mechanics were required. Informed consent was obtained with notification of a possible revision in the treatment plan in case of a necessity to extract 14. The next step was a preadjusted fixed appliance therapy (MBT prescription, slot 0.022″) starting with a light continuous NiTi wire and continuing with a typical wire sequence and sliding mechanics (Figure 13).
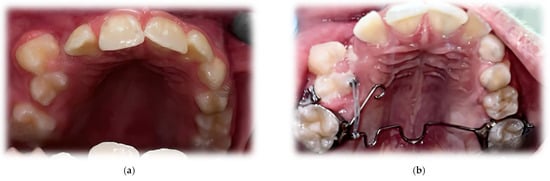
Figure 12.
Upper occlusal photograph 9 months after surgery (a) and during orthodontic treatment (b).
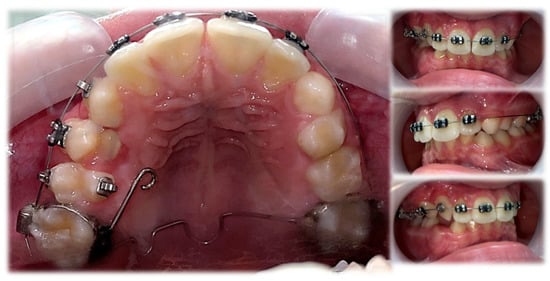
Figure 13.
Treatment progress.
6. Discussion
The aim of this paper was to present a case of a nine-year-old patient with a maxillary cyst-like lesion to exemplify the role of a well-planned interdisciplinary treatment supported by a thorough analysis of radiological records. Screening and diagnostic strategy depend on the size of the lesion and the patient’s age. In mixed dentition, the period when the cyst is associated with an unerupted tooth, the treatment of choice should be minimally invasive to preserve the germ and create favorable conditions for its further development and appearance in the oral cavity. Developmental age requires a different approach in comparison to adult patients because an intervention should not disturb the growth of the stomatognathic system. Due to the harmful effect of ionizing radiation, the objective of numerous studies has been to find an alternative that could decrease the need for X-ray exposure. In some maxillofacial pathologies, such as rhinosinusitis, researchers have confirmed that USG can be a fast, safe and efficient screening method [30]. Thus, the use of ultrasonography as a scientifically proven diagnostic tool for odontogenic cysts still requires further investigation. The comparison of USG pictures with clinical, radiological and histopathological findings presented in previous research is promising [31,32]. However, with respect to bone disturbances, achieving a similar sensitivity and specification as CBCT is impossible when the cortical bone is thick and intact. X-rays still remain the gold standard in the diagnostic protocol [33]. An important aspect is a well-judged referral for radiological examination. According to ADA recommendations for limiting radiation exposure [33], X-rays are permitted in the orthodontic diagnostic process, provided that the as low as reasonably achievable (ALARA) principle according to the patient’s exposure is respected. ADA allows taking panoramic X-rays in children with primary and mixed dentition to evaluate general dentofacial growth and development. Additionally, the specific indications that can be observed in orthodontic practice are presented, such as tooth malposition or impaction, swelling or facial asymmetry, abnormal growth and unexplained absence of teeth or ectopic eruption [33]. Although there are no clear guidelines according to radiological diagnosis in new orthodontic patients, in this paper, the suggested algorithm (including the suspicion of a cyst-like lesion) is presented in Figure 14 [9,34].
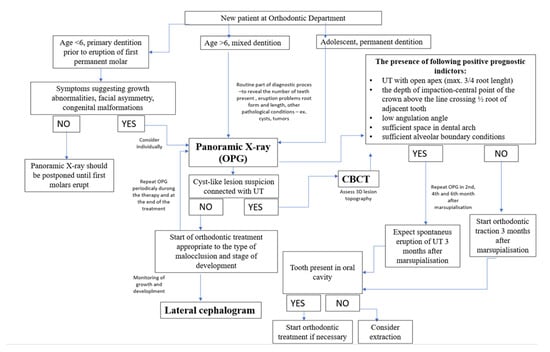
Figure 14.
X-ray diagnostic algorithm in new orthodontic patient. Legend: UT—unerupted tooth.
The presented case emphasizes the significance of routine orthodontic screening in the detection of odontogenic cyst-like lesions. Prompt preliminary diagnosis and referral to the surgery department allowed starting the treatment in the best possible developmental period and resulted in the successful eruption of affected teeth. The ability of teeth to erupt is correlated with root formation, with onset after 2/3 of the root length is formed [35]. An unerupted tooth with an open apex associated with a cyst also has the potential to appear spontaneously in the oral cavity after the marsupialization procedure [35,36]. The reduction of intracystic pressure performed at this stage of tooth development increases the chances of tooth eruption. Myiawaki et al. [36] radiologically assessed the eruption of the lower second premolars associated with a follicular cyst. The rate of eruption was correlated with the gradually decreasing size of the lesion and accelerated rapidly in the first three months after marsupialization. This process coexisted with intensive bone regeneration in the disturbed area, as well as with the promising change of tooth germ inclination. Thus, radiological findings lead to another important piece of information: the development of the root is continued even if the tooth coexists with an enlarging lesion. For this reason, marsupialization is the first-choice method in growing patients and should be performed at a proper time to control the eruption process [36]. Hyomoto et al. [37] reported that the average time required for the appearance of a tooth in the oral cavity was 109 days after the marsupialization procedure. The authors also presented the clinical determinants that promoted the spontaneous eruption of cyst-associated teeth. According to measurements, orthodontic traction was not necessary when the depth of an unerupted lower premolar cusp did not exceed 4.4 mm. The angulation of a tooth germ (understood in this paper as the angle between its long axis and the bisector of the axes of adjacent teeth) is the second determining factor. The value of 17.3° ± 16.7° was observed when the maxillary canines erupted. The authors also highlighted the significance of root maturity (1/2 root length). However, there was no significant correlation between the size of the lesion and the eruption space. Another study, in addition to similar factors mentioned above, highlighted the significance of patients’ age, which should be less than 10 years, to expect mandibular premolar eruption [37].
In the presented case, the prompt eruption of Tooth 13 after marsupialization was possible due to the existence of promising factors, as described above and highlighted in Figure 15. The apex was open, and the root (R) did not achieve 2/3 of its final length. Because the adjacent teeth were malpositioned, as a reference line to assess angulation (A), the midline was chosen (as an analogy to Ericson and Kurol’s classification) [38]. The low value of the angle and almost-parallel position of the canine germ according to the midline gave a reasonable assumption that a spontaneous eruption was possible. The cusp depth (D) is appropriate to the stage of development because, according to Coulter et al. [39], the predominant vertical eruption path can be still expected. The upper right premolars revealed a less favorable position, inclined more horizontally. CBCT confirmed vesibuloposition with a poor alveolar boundary condition that required careful application of orthodontic force to achieve their proper alignment.
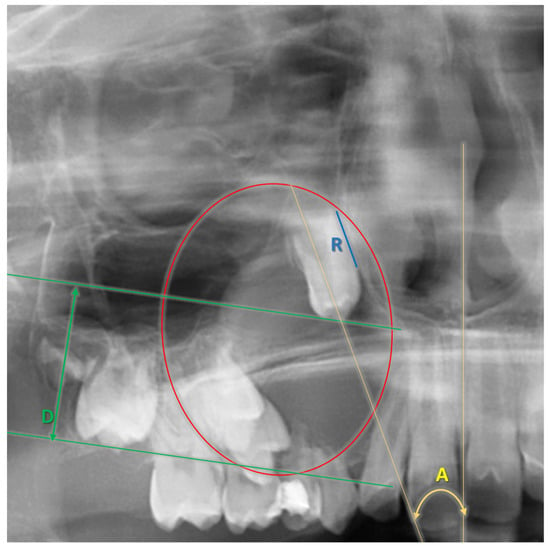
Figure 15.
Factors determining the chance for spontaneous eruption after marsupialization A—angulation; D—depth of cusp; R—root development.
7. Conclusions
Radiological examination plays an essential role in orthodontic treatment planning. It is particularly important to obtain a three-dimensional visualization of orofacial structures in cases that qualify for interdisciplinary orthodontic–surgical therapy. The presented case demonstrates the role of a panoramic radiograph, which can be a screening procedure, allowing for the detection of intraosseous aberrations such as cysts and odontogenic tumors. Early recognition of the lesion, further supported with CBCT, enabled the planning of a less-invasive surgical treatment, and the onset of the whole procedure was the most promising when it came to the prognosis of the spontaneous eruption of teeth adjacent to the cyst. Marsupialization, considered the gold standard in dentigerous cyst treatment in growing patients, was performed when the development of the canine root was uncompleted, which led to its appearance in the oral cavity without the need for orthodontic traction. Further alignment with fixed appliances is required to achieve proper occlusal conditions.
Author Contributions
Conceptualization, P.S. and A.N.; methodology, P.S. and P.K.; validation, P.K. and K.M. formal analysis, A.N.; investigation, A.N. and P.S.; resources, A.N.; writing—original draft preparation, A.N. and P.S.; writing—review and editing, A.N., P.K. and K.M.; supervision, P.K. and K.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from the patient involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Koong, B. Cysts and Cyst-like Lesions Involving the Jaws. In Atlas Oral Maxillofac Radiol; John Wiley & Sons Ltd.: Hoboken, NJ, USA, 2017; pp. 108–139. [Google Scholar]
- Mohammed, M.; Mahomed, F.; Ngwenya, S. A survey of pathology specimens associated with impacted teeth over a 21-year period. Med. Oral Patol. Oral Y Cir. Bucal 2019, 24, e571. [Google Scholar] [CrossRef] [PubMed]
- Maltoni, I.; Maltoni, M.; Santucci, G.; Ramina, F.; Lombardo, L.; Siciliani, G. Marsupialization of a dentigerous cyst followed by orthodontic traction of two retained teeth: A case report. Int. Orthod. 2019, 17, 365–374. [Google Scholar] [CrossRef] [PubMed]
- Oliveira-Neto, H.H.; Spíndula-Filho, J.V.; Dallara, M.C.S.; Silva, C.M.; Mendonça, E.F.; Batista, A.C. Unicystic ameloblastoma in a child: A differential diagnosis from the dentigerous cyst and the inflammatory follicular cyst. J. Dent. Child. 2007, 74, 245–249. [Google Scholar]
- Dunsche, A.; Babendererde, O.; Lüttges, J.; Springer, I.N. Dentigerous cyst versus unicystic ameloblastoma–differential diagnosis in routine histology. J. Oral Pathol. Med. 2003, 32, 486–491. [Google Scholar] [CrossRef]
- Anjana, G.; Balagopal Varma, U.P. Management of a dentigerous cyst: A two-year review. Int. J. Clin. Pediatric Dent. 2011, 4, 147. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.G.; Jang, H.S. Ameloblastoma: A clinical, radiographic, and histopathologic analysis of 71 cases. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2001, 91, 649–653. [Google Scholar] [CrossRef] [Green Version]
- Borghesi, A.; Nardi, C.; Giannitto, C.; Tironi, A.; Maroldi, R.; Di Bartolomeo, F.; Preda, L. Odontogenic keratocyst: Imaging features of a benign lesion with an aggressive behaviour. Insights Into. Imaging 2018, 9, 883–897. [Google Scholar] [CrossRef] [Green Version]
- Isaacson, K.G.; Jones, M.L. Guidelines for the Use of Radiographs in Clinical Orthodontics; British Orthodontic Society: London, UK, 2008. [Google Scholar]
- Vidya, L.; Ranganathan, K.; Praveen, B.; Gunaseelan, R.; Shanmugasundaram, S. Cone-beam computed tomography in the management of dentigerous cyst of the jaws: A report of two cases. Indian J. Radiol. Imaging 2013, 23, 342. [Google Scholar] [CrossRef]
- Langaroodi, A.J.; Lari, S.S.; Shokri, A.; Zarch, S.H.H.; Jamshidi, S.; Akbari, P. Intraosseous benign lesions of the jaws: A radiographic study. Iran. J. Radiol. 2014, 11, e7683. [Google Scholar]
- Cardoso, L.B.; Lopes, I.A.; Ikuta, C.R.S.; Capelozza, A.L.A. Study Between Panoramic Radiography and Cone Beam-Computed Tomography in the Diagnosis of Ameloblastoma, Odontogenic Keratocyst, and Dentigerous Cyst. J. Craniofac. Surg. 2020, 31, 1747–1752. [Google Scholar] [CrossRef]
- Devlin, H.; Yuan, J. Object position and image magnification in dental panoramic radiography: A theoretical analysis. Dentomaxillofaci. Radiol. 2013, 42, 29951683. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dalessandri, D.; Laffranchi, L.; Tonni, I.; Zotti, F.; Piancino, M.G.; Paganelli, C.; Bracco, P. Advantages of cone beam computed tomography (CBCT) in the orthodontic treatment planning of cleidocranial dysplasia patients: A case report. Head Face Med. 2011, 7, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kapila, S.D. Cone Beam Computed Tomography in Orthodontics: Indications, Insights, and Innovations; John Wiley & Sons: Hoboken, NJ, USA, 2014. [Google Scholar]
- Mah 2014, J.K.; Yi, L.; Huang, R.C.; Choo, H. Advanced Applications of Cone Beam Computed Tomography in Orthodontics. In Seminars in Orthodontics; WB Saunders: Philadelphia, PA, USA, 2011; Volume 17, No. 1; pp. 57–71. [Google Scholar]
- Haney, E.; Gansky, S.A.; Lee, J.S.; Johnson, E.; Maki, K.; Miller, A.J.; Huang, J.C. Comparative analysis of traditional radiographs and cone-beam computed tomography volumetric images in the diagnosis and treatment planning of maxillary impacted canines. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 590–597. [Google Scholar] [CrossRef]
- Hauer, L.; Seidlová, P.; Merglová, V.; Hrusak, D.; Böhmová, H.; Posta, P.; Gencur, J.; Netolicky, J. Complete removal of dentigerous cysts with preservation of associated teeth as an alternative to marsupialization in children and preadolescents. J. Cranio-Maxillofac. Surg. 2020, 48, 808–814. [Google Scholar] [CrossRef] [PubMed]
- Ghandour, L.; Bahmad, H.F.; Bou-Assi, S. Conservative treatment of dentigerous cyst by marsupialization in a young female patient: A case report and review of the literature. Case Rep. Dent. 2018, 2018, 7621363. [Google Scholar] [CrossRef] [Green Version]
- Oliveros-Lopez, L.; Fernandez-Olavarria, A.; Torres-Lagares, D.; Serrera-Figallo, M.A.; Castillo-Oyagüe, R.; Segura-Egea, J.J.; Gutierrez-Perez, J.L. Reduction rate by decompression as a treatment of odontogenic cysts. Med. Oral Patol. Oral Cir. Bucal 2017, 22, e643. [Google Scholar] [CrossRef]
- Chung, K.R.; Noh, M.K.; Oh, S.H.; Jeong, D.M.; Kim, S.H.; Nelson, G. Treatment of 2 impacted molars in a large dentigerous cyst (expansile cystic lesion) with combined orthodontic and surgical therapy. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 752–758. [Google Scholar] [CrossRef]
- Bowdin, L.M.; Anthonappa, R.P.; King, N.M. Dentigerous cyst formation following trauma to the primary incisors: A case report. Dent. Traumatol. 2021, 37, 155–159. [Google Scholar] [CrossRef]
- Aboujaoude, S.; Ziade, M.; Aoun, G. Five years follow-up of a spontaneous eruption of an impacted mandibular premolar associated with a dentigerous cyst treated by marsupialization. Cureus 2020, 12, e7370. [Google Scholar] [CrossRef] [Green Version]
- Tsironi, K.; Inglezos, E.; Vardas, E.; Mitsea, A. Uprighting an impacted permanent mandibular first molar associated with a dentigerous cyst and a missing second mandibular molar—A case report. Dent. J. 2019, 7, 63. [Google Scholar] [CrossRef] [Green Version]
- Alnofaie, H.; Alomran, O.; Ababtain, R.; Alomar, A. Spontaneous eruption of a deeply impacted premolar after conservative treatment of an associated dentigerous cyst: A case report. Cureus 2019, 11, e6414. [Google Scholar] [CrossRef] [Green Version]
- Aoki, N.; Ise, K.; Inoue, A.; Kosugi, Y.; Koyama, C.; Iida, M.; Baba, J.; Iwai, T.; Mitsudo, K. Multidisciplinary approach for treatment of a dentigerous cyst–marsupialization, orthodontic treatment, and implant placement: A case report. J. Med. Case Rep. 2018, 12, 305. [Google Scholar] [CrossRef] [PubMed]
- Abu-Mostafa, N.; Abbasi, A. Marsupialization of a large dentigerous cyst in the mandible with orthodontic extrusion of three impacted teeth. A case report. J. Clin. Exp. Dent. 2017, 9, e1162. [Google Scholar] [CrossRef] [Green Version]
- Şahin, O. Conservative management of a dentigerous cyst associated with eruption of teeth in a 7-year-old girl: A case report. J. Korean Assoc. Oral Maxillofac. Surg. 2017, 43 (Suppl. S1), S1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taysi, M.; Ozden, C.; Cankaya, A.B.; Yildirim, S.; Bilgic, L. Conservative approach to a large dentigerous cyst in an 11-year-old patient. J. Istanb. Univ. Fac. Dent. 2016, 50, 51–56. [Google Scholar] [CrossRef]
- Neagos, A.; Dumitru, M.; Vrinceanu, D.; Costache, A.; Marinescu, A.N.; Cergan, R. Ultrasonography used in the diagnosis of chronic rhinosinusitis: From experimental imaging to clinical practice. Exp. Ther. Med. 2021, 21, 611. [Google Scholar] [CrossRef]
- Sumer, A.P.; Danaci, M.; Ozen Sandikçi, E.; Sumer, M.; Celenk, P. Ultrasonography and Doppler ultrasonography in the evaluation of intraosseous lesions of the jaws. Dentomaxillofaci. Radiol. 2009, 38, 23–27. [Google Scholar] [CrossRef]
- Musu, D.; Rossi-Fedele, G.; Campisi, G.; Cotti, E. Ultrasonography in the diagnosis of bone lesions of the jaws: A systematic review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 122, e19–e29. [Google Scholar] [CrossRef] [PubMed]
- Dedeoğlu, N.; Duman, Ş.B.; Altun, O.; Arıkan, B. In vitro Comparison of Cone Beam Computed Tomography and Ultrasonography Imaging Methods in the Evaluation of Artificial Mandible Intraosseous Lesions. J. Dent. 2021, 22, 198–205. [Google Scholar]
- American Dental Association. Dental Radiographic Examinations: Recommendations for Patient Selection and Limiting Radiation Exposure; American Dental Association: Chicago, IL, USA, 2012. [Google Scholar]
- Yahara, Y.; Kubota, Y.; Yamashiro, T.; Shirasuna, K. Eruption prediction of mandibular premolars associated with dentigerous cysts. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 108, 28–31. [Google Scholar] [CrossRef]
- Miyawaki, S.; Hyomoto, M.; Tsubouchi, J.; Kirita, T.; Sugimura, M. Eruption speed and rate of angulation change of a cyst-associated mandibular second premolar after marsupialization of a dentigerous cyst. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 578–584. [Google Scholar] [CrossRef]
- Hyomoto, M.; Kawakami, M.; Inoue, M.; Kirita, T. Clinical conditions for eruption of maxillary canines and mandibular premolars associated with dentigerous cysts. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Ericson, S.; Kurol, J. Radiographic examination of ectopically erupting maxillary canines. Am. J. Orthod. Dentofac. Orthop. 1987, 91, 483–492. [Google Scholar] [CrossRef]
- Coulter, J.; Richardson, A. Normal eruption of the maxillary canine quantified in three dimensions. Eur. J. Orthod. 1997, 19, 171–183. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).