Orthodontic Surgical Treatment of Impacted Mandibular Canines: Systematic Review and Case Report
Abstract
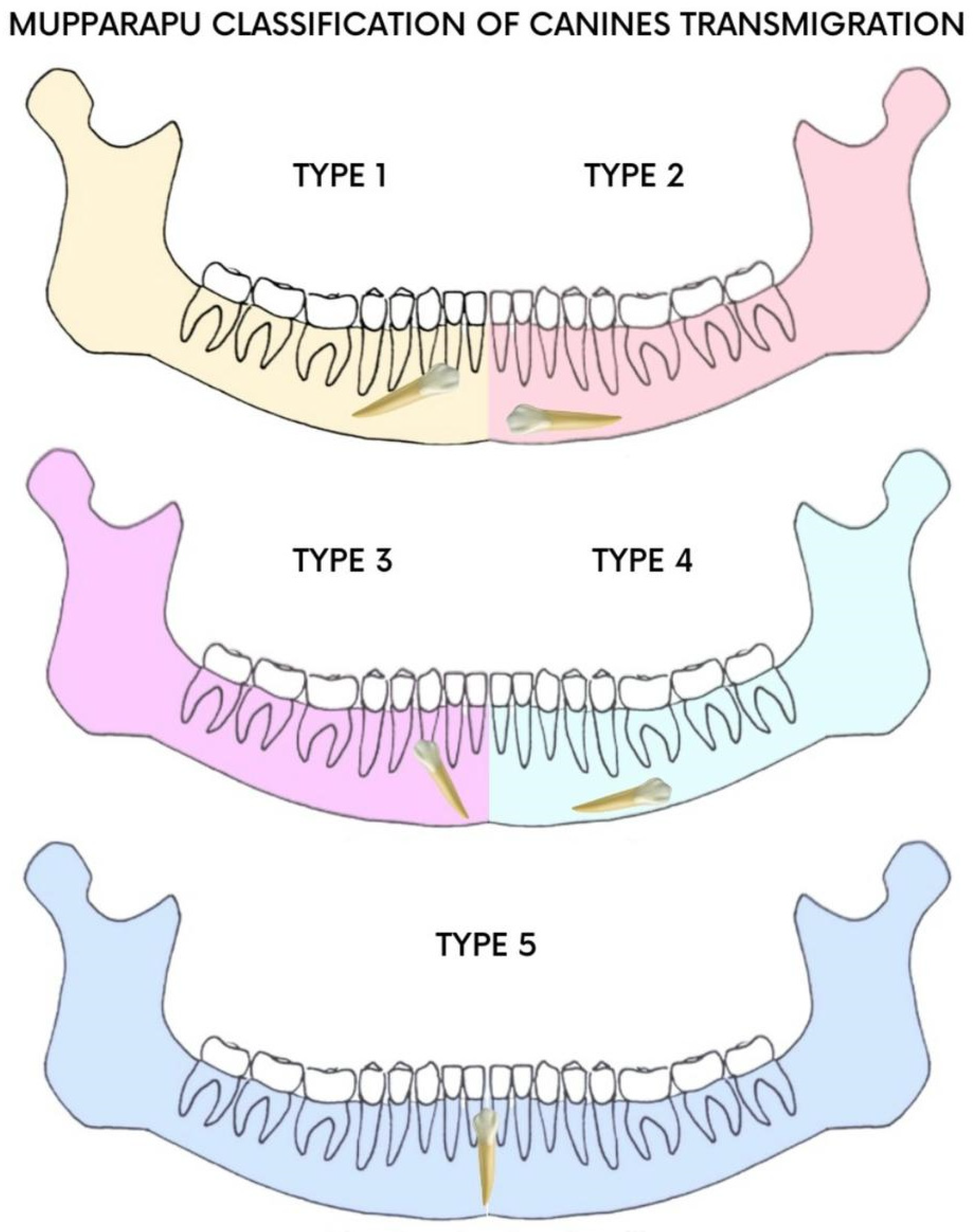
:1. Introduction
2. Materials and Methods
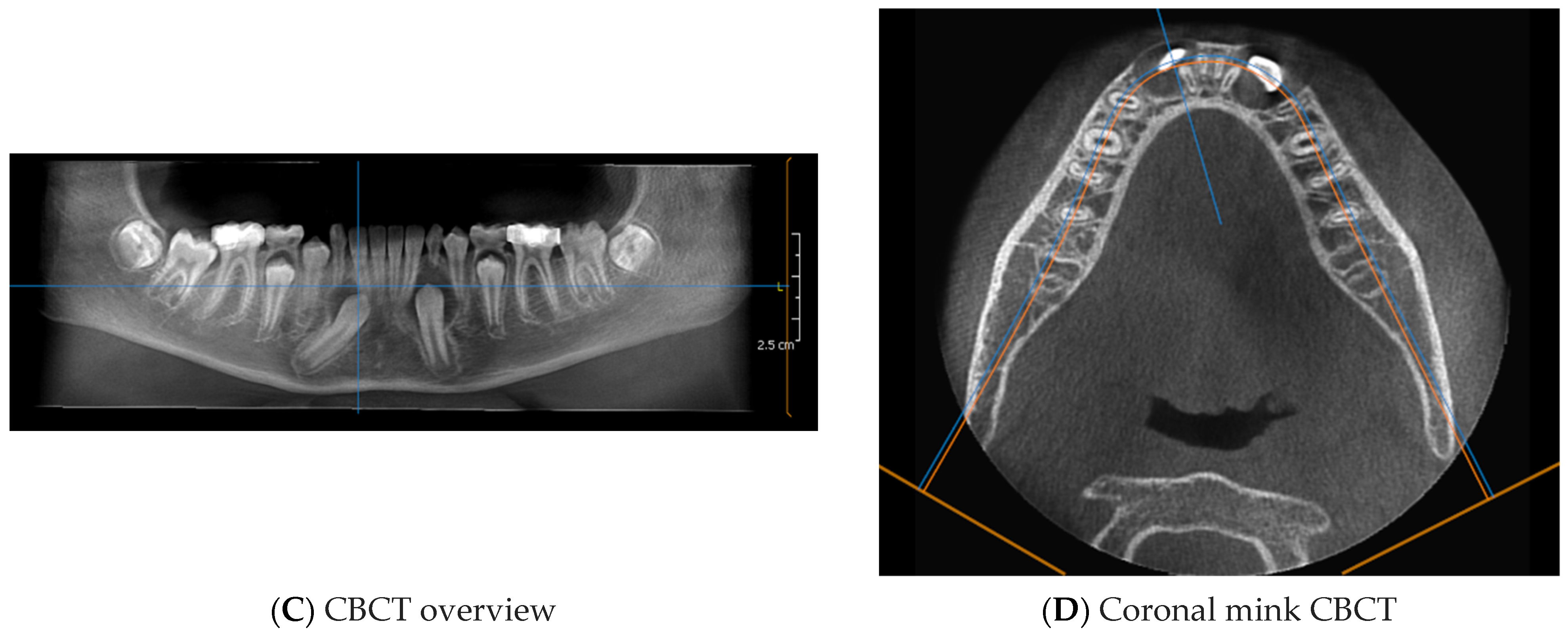
2.1. Systematic Literature Review Methodology
2.1.1. Search Strategies
2.1.2. Inclusion and Exclusion Criteria
2.1.3. Article Identification Procedure
2.1.4. Study Evaluation
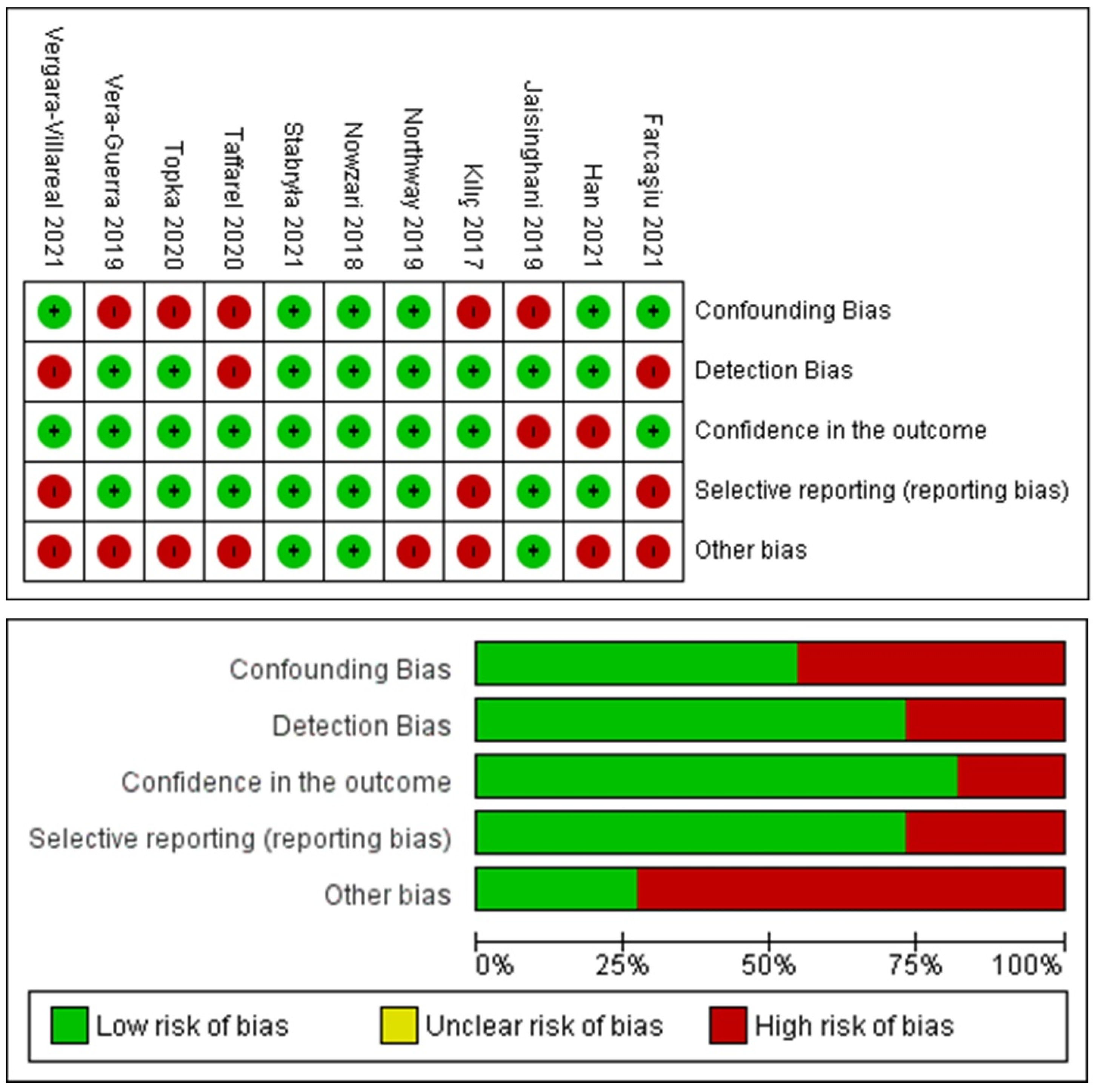
2.1.5. Risk-of-Bias Evaluation
3. Results
3.1. Study Selection and Characteristics
3.2. Risk-of-Bias Assessment Findings
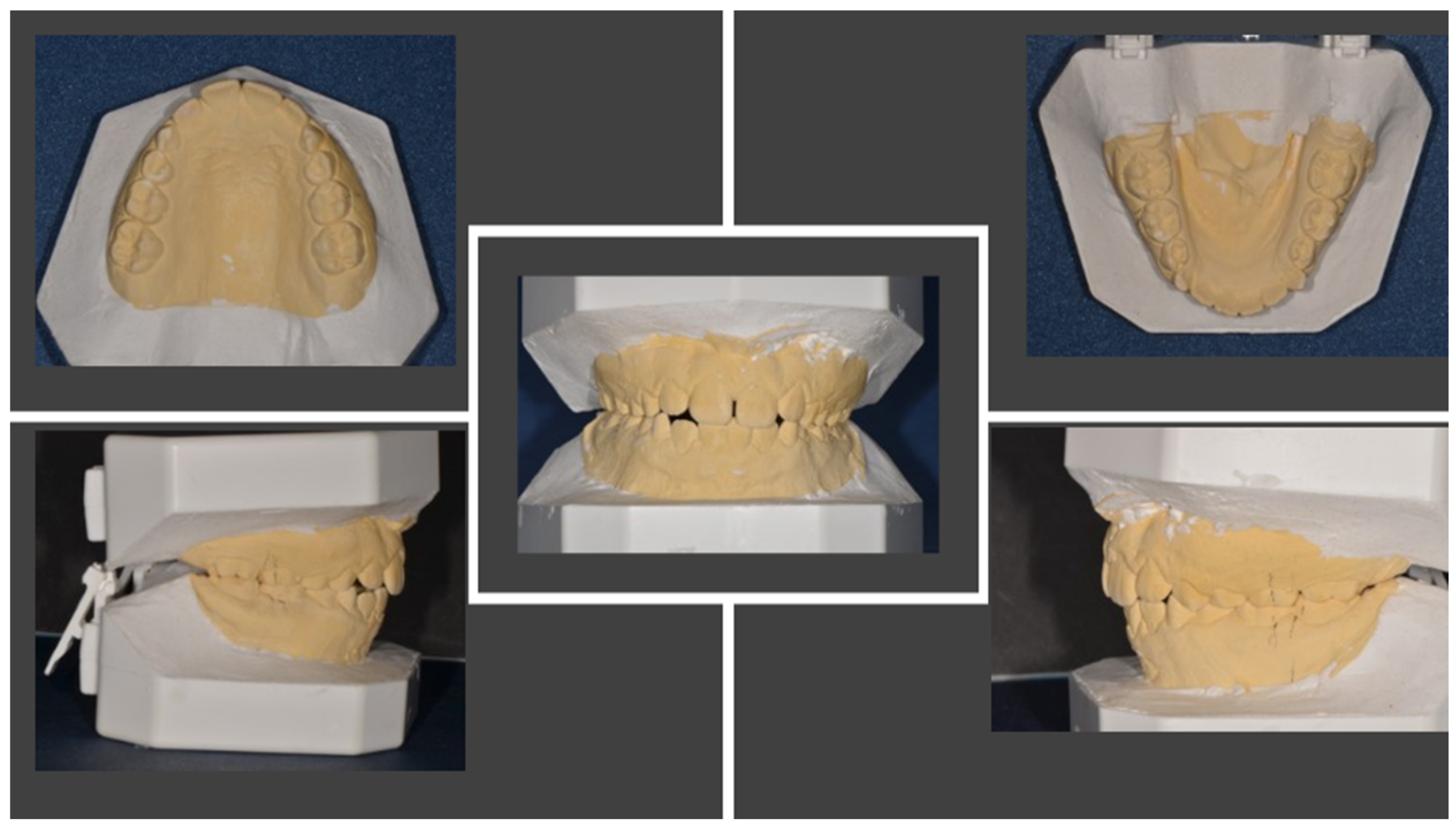
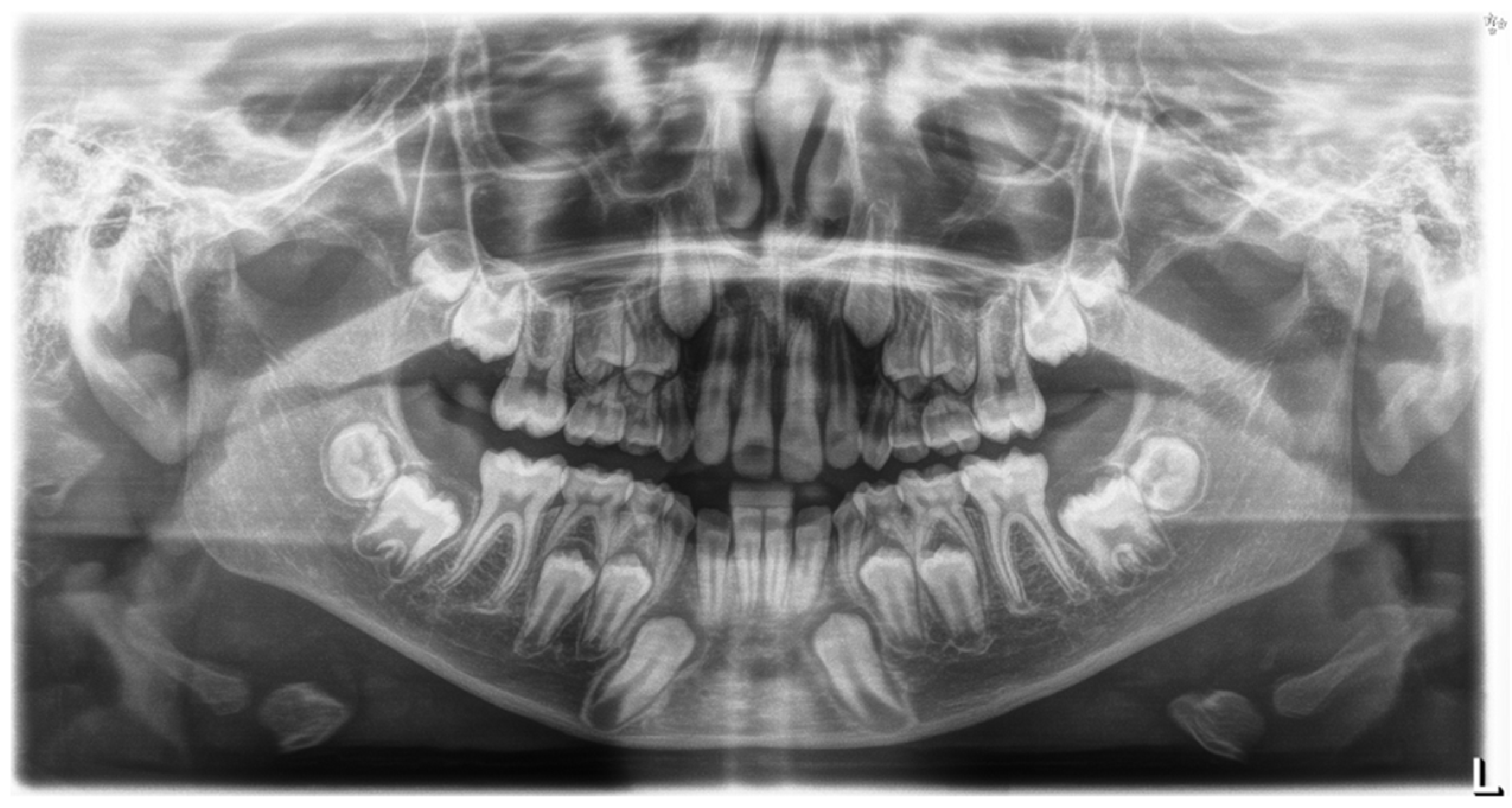
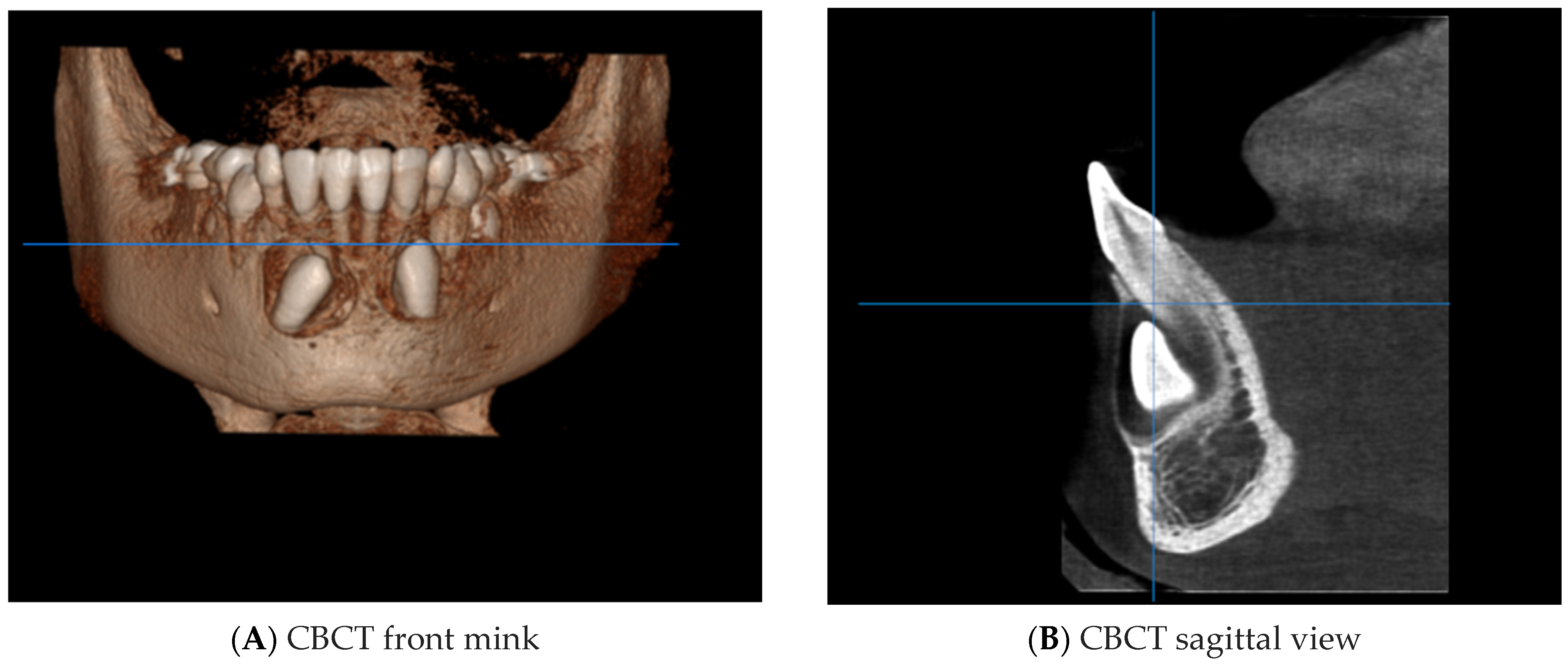
4. Case Report
- Canine angle to the midline;
- Horizontal position of the canine root apex;
- Vertical height of the canine crown;
- Canine overlap of adjacent tooth;
- Buccal–lingual position of the canine.
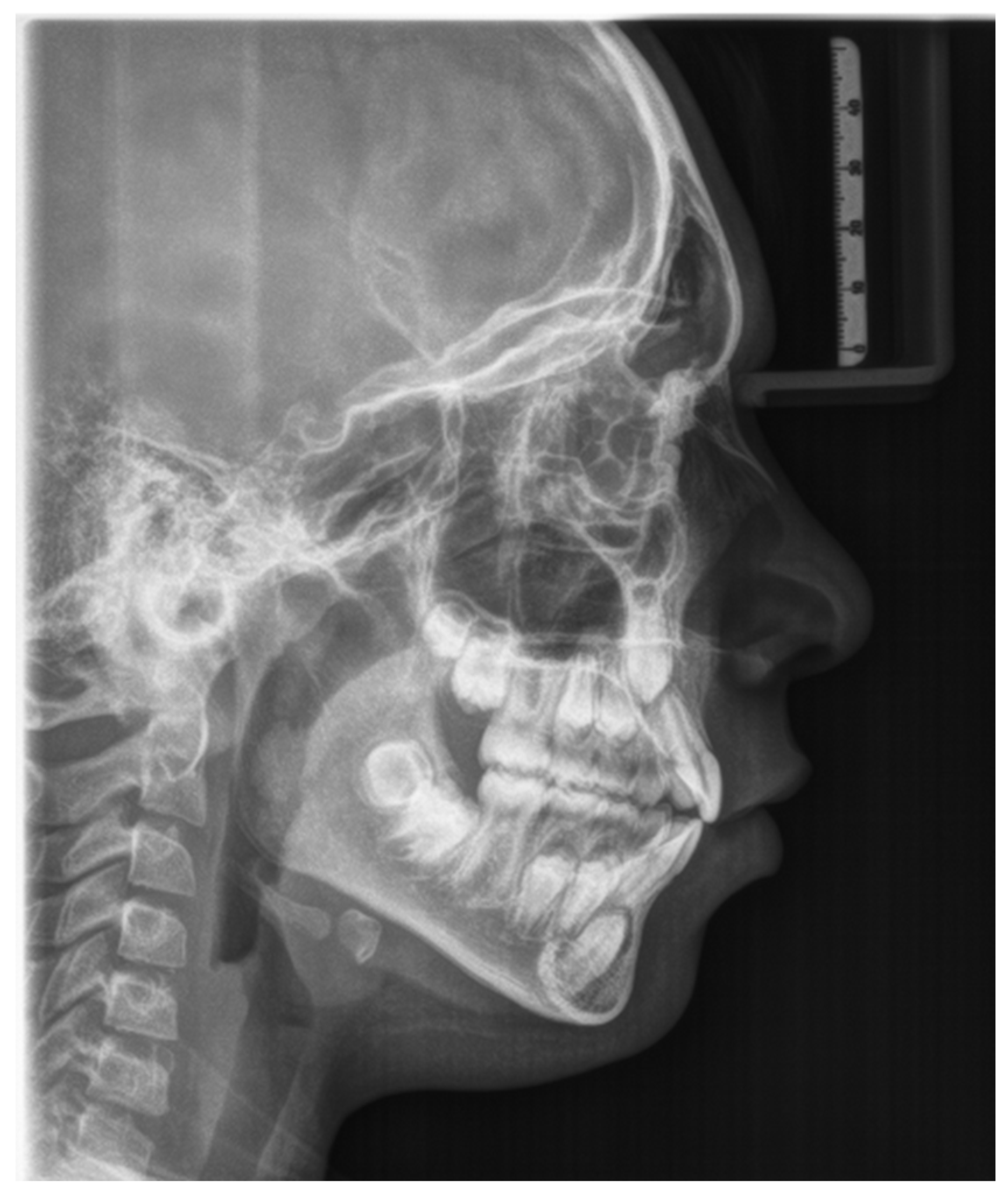
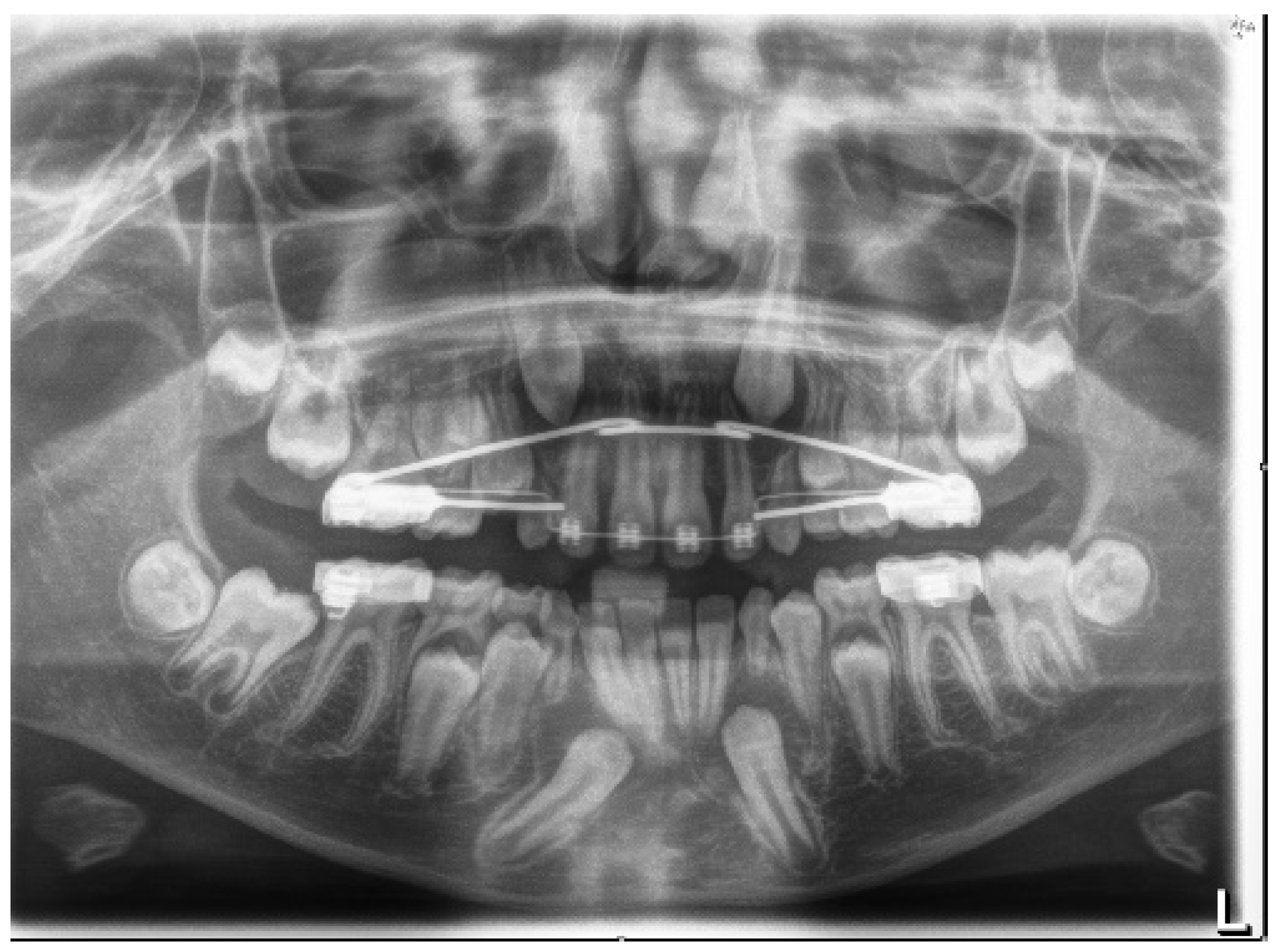
4.1. Phase 1: Initial Orthodontic Treatment
4.2. Phase 2: Surgical Technique
4.3. Orthodontic Traction
4.4. Phase 3: Final Orthodontic Treatment
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| IMC | Included mandibular canine |
| TMC | Transmigrated mandibular canine |
| IMXC | Included maxillary canine |
| OPT | Orthopantomography |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| CBCT | Cone-beam computed tomography |
| 4.3 | Lower mandibular canine |
| 4.1 | Lower-right central incisor |
| 4.2 | Lower-right lateral incisor |
References
- Cavuoti, S.; Matarese, G.; Isola, G.; Abdolreza, J.; Femiano, F.; Perillo, L. Combined Orthodontic-Surgical Management of a Transmigrated Mandibular Canine. Angle Orthod. 2015, 86, 681–691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alhammadi, M.; Asiri, H.; Almashraqi, A. Incidence, Severity and Orthodontic Treatment Difficulty Index of Impacted Canines in Saudi Population. J. Clin. Exp. Dent. 2018, 10, e327–e334. [Google Scholar] [CrossRef] [PubMed]
- Gündüz, K.; Çelenk, P. The Incidence of Impacted Transmigrant Canines: A Retrospective Study. Oral Radiol. 2010, 26, 77–81. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Laudadio, C.; Pede, C.D.; et al. The Efficacy of a New AMCOP® Elastodontic Protocol for Orthodontic Interceptive Treatment: A Case Series and Literature Overview. Int. J. Environ. Res. Public Health 2022, 19, 988. [Google Scholar] [CrossRef] [PubMed]
- Mupparapu, M. Patterns of Intra-Osseous Transmigration and Ectopic Eruption of Mandibular Canines: Review of Literature and Report of Nine Additional Cases. Dentomaxillofacial Radiol. 2002, 31, 355–360. [Google Scholar] [CrossRef]
- Majumdar, S.K.; Hossain, M.A.; De, N.; Chadda, D.; Bachhar, M.K.; Mishra, S. Effect of Diagnosis by Two-Dimensional Radiography Versus CBCT on Surgical Aspects of Transmigrated Impacted Mandibular Canines. J. Maxillofac. Oral Surg. 2020, 19, 461–467. [Google Scholar] [CrossRef]
- Laudadio, C.; Inchingolo, A.D.; Malcangi, G.; Limongelli, L.; Marinelli, G.; Coloccia, G.; Montenegro, V.; Patano, A.; Inchingolo, F.; Bordea, I.R.; et al. Management of Anterior Open-Bite in the Deciduous, Mixed and Permanent Dentition Stage: A Descriptive Review. J. Biol. Regul. Homeost. Agents 2021, 35, 271–281. [Google Scholar] [CrossRef]
- Montenegro, V.; Inchingolo, A.D.; Malcangi, G.; Limongelli, L.; Marinelli, G.; Coloccia, G.; Laudadio, C.; Patano, A.; Inchingolo, F.; Bordea, I.R.; et al. Compliance of Children with Removable Functional Appliance with Microchip Integrated during Covid-19 Pandemic: A Systematic Review. J. Biol. Regul. Homeost. Agents 2021, 35, 365–377. [Google Scholar] [CrossRef]
- Cirulli, N.; Ballini, A.; Cantore, S.; Farronato, D.; Inchingolo, F.; Dipalma, G.; Gatto, M.R.; Alessandri Bonetti, G. Mixed Dentition Space Analysis of a Southern Italian Population: New Regression Equations for Unerupted Teeth. J. Biol. Regul. Homeost. Agents 2015, 29, 515–520. [Google Scholar]
- Inchingolo, A.D.; Ceci, S.; Patano, A.; Inchingolo, A.M.; Montenegro, V.; Di Pede, C.; Malcangi, G.; Marinelli, G.; Coloccia, G.; Garibaldi, M.; et al. Elastodontic Therapy of Hyperdivergent Class II Patients Using AMCOP® Devices: A Retrospective Study. Appl. Sci. 2022, 12, 3259. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Laudadio, C.; Palmieri, G.; et al. Genetic Pattern, Orthodontic and Surgical Management of Multiple Supplementary Impacted Teeth in a Rare, Cleidocranial Dysplasia Patient: A Case Report. Medicina 2021, 57, 1350. [Google Scholar] [CrossRef] [PubMed]
- Bertl, M.H.; Frey, C.; Bertl, K.; Giannis, K.; Gahleitner, A.; Strbac, G.D. Impacted and Transmigrated Mandibular Canines: An Analysis of 3D Radiographic Imaging Data. Clin. Oral Investig. 2018, 22, 2389–2399. [Google Scholar] [CrossRef] [PubMed]
- Azeem, M.; Afzal, A.; Ahmed, Z.; Ali, M.M.; Haq, A.U.; Hamid, W.U. Investigation of Transmigrated Mandibular Canines. Dent. Press J. Orthod. 2019, 24, 65. [Google Scholar] [CrossRef] [PubMed]
- Cakir Karabas, H.; Ozcan, I.; Erturk, A.F.; Guray, B.; Unsal, G.; Senel, S.N. Cone-Beam Computed Tomography Evaluation of Impacted and Transmigrated Mandibular Canines: A Retrospective Study. Oral Radiol. 2021, 37, 403–411. [Google Scholar] [CrossRef] [PubMed]
- Crescini, A.; Baccetti, T.; Rotundo, R.; Mancini, E.A.; Prato, G.P. Tunnel Technique for the Treatment of Impacted Mandibular Canines. Int. J. Periodontics Restor. Dent. 2009, 29, 213–218. [Google Scholar]
- Plaza, S.P. Orthodontic Traction of a Transmigrated Mandibular Canine Using Mini-Implant: A Case Report and Review. J. Orthod. 2016, 43, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Dalessandri, D.; Parrini, S.; Rubiano, R.; Gallone, D.; Migliorati, M. Impacted and Transmigrant Mandibular Canines Incidence, Aetiology, and Treatment: A Systematic Review. Eur. J. Orthod. 2017, 39, 161–169. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. PLoS Med. 2021, 18, e1003583. [Google Scholar] [CrossRef]
- Kılıç, N.; Oktay, H. Orthodontic Intervention to Impacted and Transposed Lower Canines. Case Rep. Dent. 2017, 2017, 4105713. [Google Scholar] [CrossRef] [Green Version]
- Northway, W. Orthodontic Management of a Dental Anomaly Pattern (DAP) Including Mandibular Canine Transmigration: A Case Report: A Challenging Treatment but Worth It! Angle Orthod. 2019, 89, 149–162. [Google Scholar] [CrossRef] [Green Version]
- Vera-Guerra, J.A.; Herrera-Atoche, J.R.; Colomé-Ruiz, G.E. Orthodontic Treatment of Bilateral Impacted Mandibular Canines and a Mupparapu Type 2 Transmigration. Case Rep. Dent. 2019, 2019, 7638959. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farcaşiu, C.; Dinescu, M.I.; Tărlungeanu, D.I.; Bataiosu, M.; Daguci, C.; Daguci, L.; Dina, M.N.; Andrei, O.-C. A Rare Case of Transmigrated Mandibular Canine and Combined Orthodontic–Surgical Management. Rom. J. Morphol. Embryol. 2022, 62, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Vergara-Villareal, P.; Del Castillo, K.; Ramírez-Ossa, D.; Barbosa-Liz, D. An Innovative Therapeutic Alternative for Correcting the Direction of Eruption of a Lower Mandibular Cuspid: A Mixed Dentition Case Report. Int. J. Orthod. Rehabil. 2021, 12, 79. [Google Scholar] [CrossRef]
- Stabryła, J.; Plakwicz, P.; Kukuła, K.; Zadurska, M.; Czochrowska, E.M. Comparisons of Different Treatment Methods and Their Outcomes for Impacted Maxillary and Mandibular Canines: A Retrospective Study. J. Am. Dent. Assoc. 2021, 152, 919–926. [Google Scholar] [CrossRef]
- Nowzari, H.; Rodriguez, A.E. Impacted Teeth: Closed Flap Surgery. J. Esthet. Restor. Dent. 2019, 31, 233–239. [Google Scholar] [CrossRef]
- Topka, A.; Racka-Pilszak, B.; Wojtaszek-Słomińska, A.; Orzelska-Blomberg, M. Surgical-Orthodontic Treatment of Impacted Permanent Canines in the Mandible: Two Case Reports. Jstoma 2020, 72, 282–290. [Google Scholar] [CrossRef]
- Taffarel, I.A.; Taffarel, I.P.; Gasparello, G.G.; Pithon, M.M.; Tanaka, O.M. Transmigrated Mandibular Canine Guided into Its Normal Position. J. Clin. Diagn. Res. 2020, 14, ZD01–ZD04. [Google Scholar] [CrossRef]
- Jaisinghani, A.P.; Pradhan, T.; Keluskar, K.M.; Takane, V. Treatment of a Transmigrated and an Impacted Mandibular Canine along with Missing Maxillary Central Incisor: A Case Report. Orthod. Waves 2019, 78, 84–92. [Google Scholar] [CrossRef]
- Hamdan, H.A.; Grünheid, T.; Larson, B.E. Effect of Orthodontic Treatment with Preadjusted Edgewise Appliances on the Buccolingual Inclination of Mandibular Canines: A CBCT Study. Orthod. Craniofac. Res. 2015, 18, 156–164. [Google Scholar] [CrossRef]
- Krasny, M.; Krasny, K.; Wojtowicz, A. En Bloc Autotransplantation of Retained Canine in the Mandible: A Case Presentation. Int. J. Periodontics Restor. Dent. 2020, 40, 403–407. [Google Scholar] [CrossRef]
- Aras, M.; Halicioglu, K.; Yavuz, M.; Caglaroglu, M. Evaluation of Surgical-Orthodontic Treatments on Impacted Mandibular Canines. Med. Oral 2011, e925–e928. [Google Scholar] [CrossRef] [Green Version]
- Paolone, M.G.; Kaitsas, R.; Paolone, G.; Kaitsas, V. Lingual Orthodontics and Forced Eruption: A Means for Osseous and Tissue Regeneration. Prog. Orthod. 2008, 9, 46–57. [Google Scholar] [PubMed]
- Kaitsas, R.; Paolone, M.G.; Paolone, G. Guided Orthodontic Regeneration: A Tool to Enhance Conventional Regenerative Techniques in Implant Surgery. Int. Orthod. 2015, 13, 539–554. [Google Scholar] [CrossRef] [PubMed]
- Crescini, A.; Nieri, M.; Buti, J.; Baccetti, T.; Mauro, S.; Pini Prato, G.P. Short- and Long-Term Periodontal Evaluation of Impacted Canines Treated with a Closed Surgical? Orthodontic Approach. J. Clin. Periodontol. 2007, 34, 232–242. [Google Scholar] [CrossRef] [PubMed]
- Chaushu, S.; Becker, A.; Zeltser, R.; Branski, S.; Vasker, N.; Chaushu, G. Patients Perception of Recovery after Exposure of Impacted Teeth: A Comparison of Closed- versus Open-Eruption Techniques. J. Oral Maxillofac. Surg. 2005, 63, 323–329. [Google Scholar] [CrossRef]
- Malcangi, G.; Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Garibaldi, M.; Inchingolo, A.M.; Piras, F.; Cardarelli, F.; Settanni, V.; et al. Impacted Central Incisors in the Upper Jaw in an Adolescent Patient: Orthodontic-Surgical Treatment—A Case Report. Appl. Sci. 2022, 12, 2657. [Google Scholar] [CrossRef]
- Özer, M.; Şener, I.; Bayram, M. Bilaterally Impacted Maxillary Central Incisors: Surgical Exposure and Orthodontic Treatment: A Case Report. J. Contemp. Dent. Pract. 2006, 7, 98–105. [Google Scholar] [CrossRef] [Green Version]
- Chaushu, S.; Zilberman, Y.; Becker, A. Maxillary Incisor Impaction and Its Relationship to Canine Displacement. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 144–150, discussion 150. [Google Scholar] [CrossRef]
- Han, L.; Mei, L.; Zhang, C.; Wu, T.; Wang, C. Correction of Class II Division 2 with Crowding and Bilateral Fully Transposed Impacted Mandibular Canines. Australas. Orthod. J. 2022, 38, 29–40. [Google Scholar] [CrossRef]
- Bishara, S.E.; Ortho, D. Impacted Maxitlary Canines: A Review. Am. J. Orthod. Dentofac. Orthop. 1992, 13, 159–171. [Google Scholar] [CrossRef]
- Boyd, R.L. Clinical Assessment of Injuries in Orthodontic Movement of Impacted Teeth. II. Surgical Recommendations. Am. J. Orthod. 1984, 86, 407–418. [Google Scholar] [CrossRef]
- Vermette, M.E.; Kokich, V.G.; Kennedy, D.B. Uncovering Labially Impacted Teeth: Apically Positioned Flap and Closed-Eruption Techniques. Angle Orthod. 1995, 65, 23–32, discussion 33. [Google Scholar] [CrossRef] [PubMed]


| Search Strategies | |
|---|---|
| keywords | Advanced keyword search ((canine) AND (mandibular)) AND (impacted) |
| Databases | PubMed, Cochrane, Scopus, Web of Science |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| English language | Non-English-language articles |
| Full text Human | Reviews |
| Research from 2017 to 2022 | Letters to the editor |
| Studies of patients aged 9–18 years with inclusion and/or transmigration of the mandibular canine | Studies on patients with genetic syndromes |
| Original prospective and retrospective studies on human subjects | Studies on patients with severe facial malformations |
| Studies including a clear description of the materials and techniques applied | |
| Studies with surgical and orthodontic techniques |
| Authors | Journal | Study Design | Age | Symptoms | Treatment | Technique | Position | Final Periodontal Considerations |
|---|---|---|---|---|---|---|---|---|
| Kılıç et al. [19] | Case Reports in Dentistry | Case report | 13.9 | Asymptomatic | Orthodontic surgical exposure, elastic traction | Guided eruption in open technique | Transposed 4.3; impacted 3.3 | The mandibular canines were brought to their own spaces, without any discomfort or side effects such as root resorption, alveolar destruction, or gingival recession, and they were properly positioned in the dental arch. Periodontal tissues were healthy during the treatment and retention periods. |
| Northway et al. [20] | The Angle Orthodontist | case report | 11.7 | Asymptomatic | Orthodontic surgical exposure, elastic traction | Guided eruption in closed technique | Transmigrated 4.3 | At the final records appointment, the gingival height at the lower right canine was about 3 mm lower than that on the left side. However, there was a conspicuous improvement over the ensuing 7 years. |
| Vera Guerra et al. [21] | Case Reports in Dentistry | Case report | 14 | Asymptomatic | Orthodontic surgical exposure, elastic traction | Guided eruption in closed technique | Included 4.3; transmigrated 3.3 | Both canines were successfully brought to a functional position within the dental arch and with a healthy periodontium. |
| Farcaşiu et al. [22] | Romanian Journal of Morphology and Embryology | Case report | 10 | Asymptomatic | Orthodontic surgical exposure, elastic traction | Guided eruption in open technique | Transmigrated 3.3 | The aspect of the gingiva in the anterior region was good, meaning that there was a good level of supporting bone, and that the surgical sutures were not tensed, allowing a normal healing rate. |
| Vergara-Villareal et al. [23] | International Journal of Orthodontic Rehabilitation | Case report | 11 | Asymptomatic | Orthodontic surgical exposure, elastic traction | Guided eruption in open technique | Included 4.3 | Not reported. |
| Stabryła et al. [24] | The Journal of the American Dental Association | Retrospective study | 15 | Asymptomatic | Orthodontic surgical exposure, elastic traction | Guided eruption in closed technique; avulsion of transmigrated canines | Included and transmigrated 3.3 and 4.3 | No adverse effects of orthodontic extrusions—such as severe root resorption of adjacent teeth, enamel demineralization, loss of pulpal vitality, or gingival recession—were observed in this sample. |
| Han et al. [14] | Australasian Orthodontic Journal | Case report | 12 | Asymptomatic | Orthodontic surgical exposure, elastic traction | Guided eruption in open technique | Included 3.3 and 4.3 | The post-treatment CBCT scan showed that there was no buccal alveolar bone resorption around the mandibular canines after arch expansion, and that the canine roots were well aligned in the middle of the alveolar bone; good periodontal health around 4.3 and 3.3. |
| Nowzari et al. [25] | JERD | Pilot study | 15 | Asymptomatic | Orthodontic surgical exposure, elastic traction | Guided eruption in closed technique | Maxillary canines included; two mandibular canines included | Post-orthodontic treatment, the periodontal probing depth averaged 2.2 mm, and the zone of keratinized gingiva averaged 3.6 mm. No discernible radiographic bone loss or root resorption was noticed. Overall, gingival margins provided an esthetic appearance in all cases. |
| Topka et al. [26] | Journal of Stomatology | Case report | 11.1 | Asymptomatic | Orthodontic surgical exposure, metallic traction | Guided eruption in closed technique | Included 4.3 | Case 1: The second complication—namely, root resorption—was evidenced in Case 2 where, due to the presence of gingival recession of tooth 4.3, the patient was monitored by a periodontologist, who proposed coverage of the recession with an autogenic transplant at the right age for the patient. |
| Taffarel et al. [27] | Journal of Clinical and Diagnostic Research | Case report | 12 | Asymptomatic | Orthodontic surgical exposure, elastic and metallic traction | Guided eruption in closed technique | Transmigrated 4.3 | Strong appearance of the ridges and trabecular bone; no negative effects (such as root resorption or periodontal problems). |
| Jaisinghani et al. [28] | Orthodontic Waves | Case report | 18 | Asymptomatic | Orthodontic surgical exposure, elastic and metallic traction, and TADS | Guided eruption in closed technique | Transmigrated 4.3 | Gingival recession on 4.3; not treated by the author as it was cosmetically negligible |
| Dental Reports | ||||
|---|---|---|---|---|
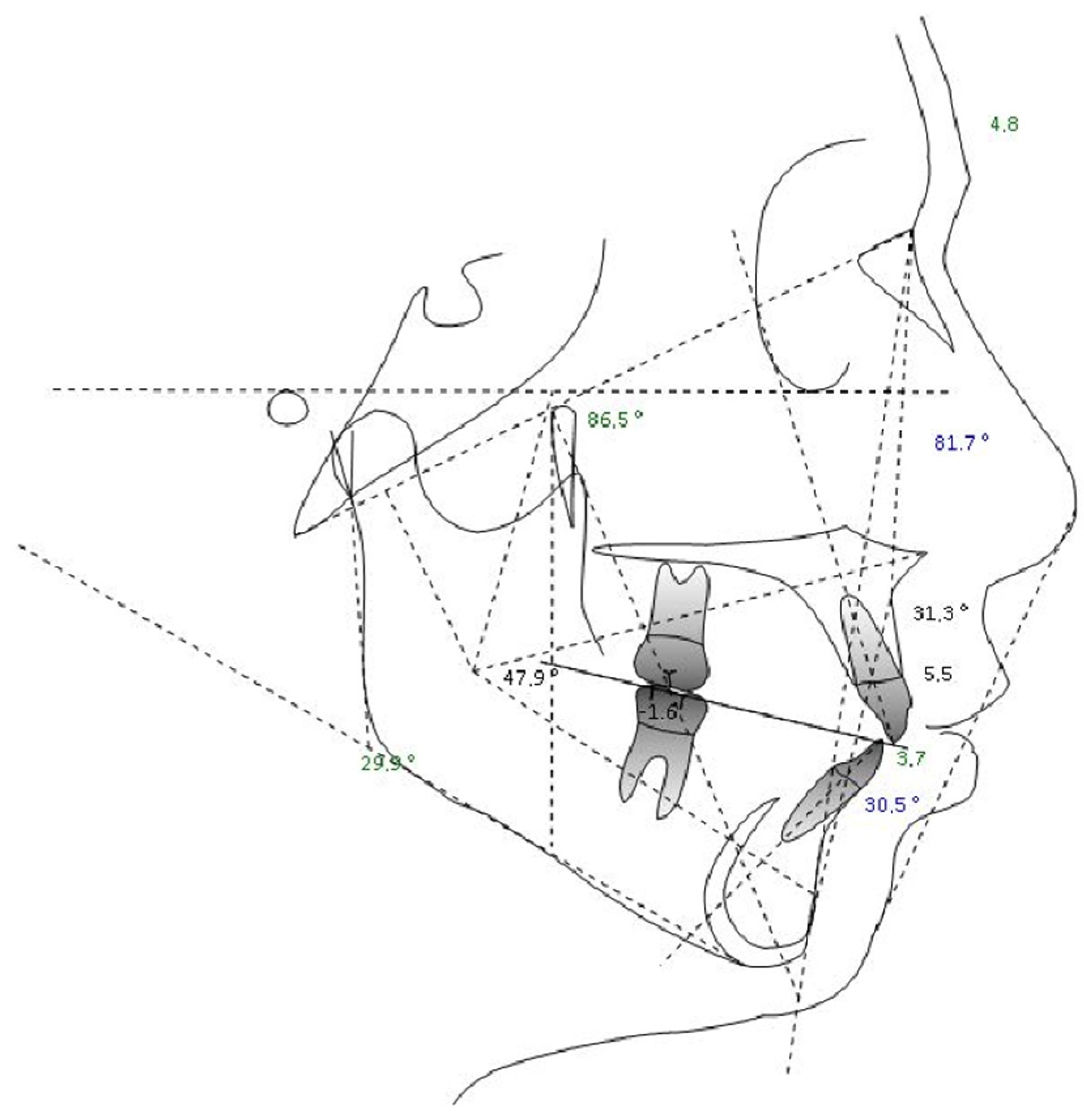
| Measure | Value | Mean | Deviation | Measurement Analysis |
| Molar report (A6-B6) −1, N | −1.6 | −3 ± 3 | N | Class I dental |
| Overjet (B1-A1 Horz.) | 1.8 | 2.5 ± 2.5 | N | Normal |
| Overbite (B1-A1 Vert.) | 0.2 | 2.5 ± 2.5 | N | Normal |
| Inferior incisor extrusion (B1-Occl.) | 0.5 | 1.25 ± 2 | N | Normal |
| Angolo Interincisivo (A1-B1 angle) | 118.2 | 132 ± 6 | -XX | |
| G02—Skeletal Reports | ||||
| Convexity (A-NPog) | 4.8 | 1 ± 2 | X | Class II bone |
| Lower face height (ANS-Xi-Pm) | 47.9° | 47 ± 4 | N | Facial meso |
| Dentoskeletal Ratios | ||||
| Upper molar position | 12.1 | 17 ± 3 | -X | Class III |
| Inferior incisor protrusion (B1-APog) | 3.7 | 1 ± 2.3 | X | Protrusion |
| Superior incisor protrusion (A1-APog) | 5.5 | 3.5 ± 2.3 | N | Normal |
| Lower incisor inclination | 30.5° | 22 ± 4 | XX | |
| Upper incisor inclination | 31.3° | 28 ± 4 | N | Normal |
| Occlusal plane inclination | 19.9° | 24.5 ± 4 | -X | |
| Craniofacial Reports | ||||
| Facial depth (PoOr-NPog) | 81.7° | 88.5 ± 3 | -XX | Facial dolic |
| Facial axis (BaN-PTGn) | 86.5° | 90 ± 3 | -X | Facial dolic |
| With facial icity | 68.4° | 68 ± 3.5 | N | Facial meso |
| Mandibular plane angle (GocMe-P) | 29.9° | 24.5 ± 4 | X | Facial dolic |
| Jaw depth (PoOr-NA) | 86.8° | 90 ± 3 | -X | Retrognathia |
| Palatal floor (PoOr-ANSPNS) | 0.3° | 1 ± 3.5 | N |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inchingolo, A.D.; Carpentiere, V.; Piras, F.; Netti, A.; Ferrara, I.; Campanelli, M.; Latini, G.; Viapiano, F.; Costa, S.; Malcangi, G.; et al. Orthodontic Surgical Treatment of Impacted Mandibular Canines: Systematic Review and Case Report. Appl. Sci. 2022, 12, 8008. https://doi.org/10.3390/app12168008
Inchingolo AD, Carpentiere V, Piras F, Netti A, Ferrara I, Campanelli M, Latini G, Viapiano F, Costa S, Malcangi G, et al. Orthodontic Surgical Treatment of Impacted Mandibular Canines: Systematic Review and Case Report. Applied Sciences. 2022; 12(16):8008. https://doi.org/10.3390/app12168008
Chicago/Turabian StyleInchingolo, Alessio Danilo, Vincenzo Carpentiere, Fabio Piras, Anna Netti, Irene Ferrara, Mariagrazia Campanelli, Giulia Latini, Fabio Viapiano, Stefania Costa, Giuseppina Malcangi, and et al. 2022. "Orthodontic Surgical Treatment of Impacted Mandibular Canines: Systematic Review and Case Report" Applied Sciences 12, no. 16: 8008. https://doi.org/10.3390/app12168008
APA StyleInchingolo, A. D., Carpentiere, V., Piras, F., Netti, A., Ferrara, I., Campanelli, M., Latini, G., Viapiano, F., Costa, S., Malcangi, G., Patano, A., Ceci, S., Mancini, A., Lucia, C., Scarano, A., Lorusso, F., Palermo, A., Ciocia, A. M., Inchingolo, F., ... Dipalma, G. (2022). Orthodontic Surgical Treatment of Impacted Mandibular Canines: Systematic Review and Case Report. Applied Sciences, 12(16), 8008. https://doi.org/10.3390/app12168008



















