Abstract
The aim of the present study was to evaluate in a clinical setting the bracket survival of lingual brackets bonded with the KommonBase system, and to compare it to the survival of a customized lingual bracket system. Two convenience samples of 13 consecutive patients treated with lingual fixed appliances with KommonBase extensions (Group 1) and 14 consecutive patients treated with customized Incognito™ lingual fixed appliances were retrospectively enrolled (Group 2). First time debondings were recorded from the files. Data were submitted to statistical analysis and a Log-rank test was used to compare the Kaplan–Meier survival curves between the two groups. Statistical significance was set as p < 0.05. Lingual brackets bonded with the KommonBase system showed a failure rate of 8%, while Incognito brackets showed a failure rate of 7.1%. The Log-rank test comparing the Kaplan–Meier survival curves revealed no statistically significant difference between the two groups (p = 0.343). Most debondings occurred during the first 6 months. Upper incisors and canines were less prone to debond than premolars and molars. In conclusion, no difference in bracket survival was observed between the KommonBase system and a customized lingual appliance.
1. Introduction
The increasing demand for orthodontic treatment from adult patients has encouraged the use of orthodontic appliances with a low impact on aesthetics, such as lingual brackets [1]. On the other hand, despite the aesthetic advantage for the patients, there are some actual difficulties for the clinician due to the limited accessibility and the uneven morphology of the lingual tooth surface. These difficulties are not only related to the routine management of orthodontic patients, like archwire and ligature changes, or the application of auxiliaries, but also to an important phase such as bracket positioning. Indeed, bonding lingual brackets with the necessary precision is complicated by: the limited access and visibility to the lingual surfaces; the greater variability in tooth surface anatomy; the reduced clinical crown height; and tongue interference [2,3]. In addition, the effectiveness of the bonding procedure can be compromised by a challenging isolation from moisture and saliva [4]. For these reasons, indirect bonding is widely considered the preferred technique in lingual orthodontics because it reduces rotational and vertical errors and increases the overall bracket position accuracy [3,5]. Indeed, it is known that indirect bonding simplifies field isolation and results in a reduction in chairside time for bracket bonding [6,7,8]. Indirect bonding was first described in 1972 by Silverman et al. [9] with the purpose of reducing chairside time and improving the precision of bracket placement: brackets are first placed on a dental cast, then transferred to the patient’s mouth through a transfer tray on all teeth of the same arch simultaneously. However, there are contradicting results regarding the real accuracy in bracket positioning [3,10], and full or partial transfer trays are not indicated for cases with severely crowded teeth or when large tooth movements due to extractions, expansion or distalization are expected [11].
The KommonBase system [12,13] is an alternative indirect bonding system that allows custom placement of any type of lingual bracket at a custom distance from the tooth surface through a customized composite resin base. A high flow filled flowable resin is placed to fill the gap between the metal bracket base and the tooth surface, followed by the application of a high flow unfilled flowable resin to extend the resin base to completely cover the lingual tooth surface [13]. The KommonBase system thus presents the advantage of offering a large, self-positioning bonding base that allows precise positioning of any standard lingual orthodontic bracket chosen by the practitioner, without depending on a customized bracket system. This extended bonding base allows for single tooth bonding in presence of severely crowded teeth, or for rebonding in case of debonding [11]. This system is offering several advantages, such as the possibility of using a straight wire instead of a mushroom-shaped wire, an immediate bonding of all brackets even on severely crowded teeth, and an easier rebonding procedure in case of debonding [11]. Despite these advantages, it should be evaluated whether the presence of the custom resin base affects bonding strength, given the importance of debonding rates from a clinical perspective [14,15,16].
The aim of the present study was to evaluate in a clinical setting the bracket survival of lingual brackets bonded with the KommonBase system, and compare it to the survival of a customized lingual bracket system.
2. Materials and Methods
A convenience sample of 13 consecutive patients treated with lingual fixed appliances at Hopital Bretonneau (Paris, France) were retrospectively enrolled (Group 1). Inclusion criteria were as follows: STb lingual brackets (Ormco, Washington, DC, USA), bonded with indirect bonding with KommonBase extensions, and lingual fixed appliance bonded at least 6 months prior to enrollment. On the other hand, 14 consecutive patients treated with lingual fixed appliances in a private practice (Geneva, Switzerland) were retrospectively enrolled as a control group (Group 2), the inclusion criteria being the use of customized Incognito™ lingual brackets (3M Unitek, St. Paul, MN, USA), bonded at least 6 months prior to enrollment.
2.1. Bonding Procedure for Group 1
After the preparation of the STb brackets for indirect bonding with KommonBase extension by the laboratory (high flow filled flowable resin: Gradia Direct Flo, GC, Tokyo, Japan, and high flow unfilled flowable resin: Prossimo Add-On Gel, GC, Tokyo, Japan), the brackets were bonded on the patients’ teeth all at once through 3D-printed acrylic transfer jigs: after cleaning and polishing with pumice and rubber cup, the enamel surface was first sandblasted with 50 μm aluminum oxide powder spray at 4 bar; then etched with 37% phosphoric acid for 15 s, rinsed with water spray for 15 s and air-dried; a universal bonding primer (OrthoSolo, Ormco, Washington, DC, USA) was then applied with a brush as a thin layer and gently blown and light-cured for 10 s; a flowable light-curing composite (Flow-Tain™ LV, Reliance Orthodontics Products, Itasca, IL, USA) was used to bond the resin base to the conditioned enamel surface, the excess was gently removed and the base was light-cured for 40 s (Table 1).

Table 1.
Bonding procedures for the two groups.
2.2. Bonding Procedure for Group 2
The teeth were cleaned, sandblasted, etched, rinsed and air-dried as described for Group 1. Then, the recommended producer procedure was followed: A thin layer of chemical cure sealant (Maximum Cure®, Reliance Orthodontics Products, Itasca, IL, USA) was applied both to the base of the brackets and to the enamel. The brackets were subsequently seated all at once through a double-layer vacuum-formed transfer tray. The tray was firmly hold in place for 3 min, then was removed after an additional minute (Table 1).
2.3. Data Collection
The debondings were recorded from the files. Only first time debondings were taken into account. The observation period was cut off at 16 months.
2.4. Statistical Analysis
Descriptive statistics were computed for all the variables. Kaplan–Meier survival curves were calculated for the brackets in both groups. A Log-rank test was used to compare the curves between the two groups. A Chi-squared test was used to evaluate the debonding frequency between anterior and posterior brackets. Statistical significance was set as p < 0.05. All analysis were performed using SPSS software (SPSS for Windows version 19, IBM, Armonk, NY, USA).
3. Results
Group 1 included a total of 300 brackets, while Group 2 comprised a total of 308 brackets. Debonding frequencies are reported in Table 2.

Table 2.
Frequencies of debondings in the two groups.
The distribution of failures over time is reported in Figure 1.
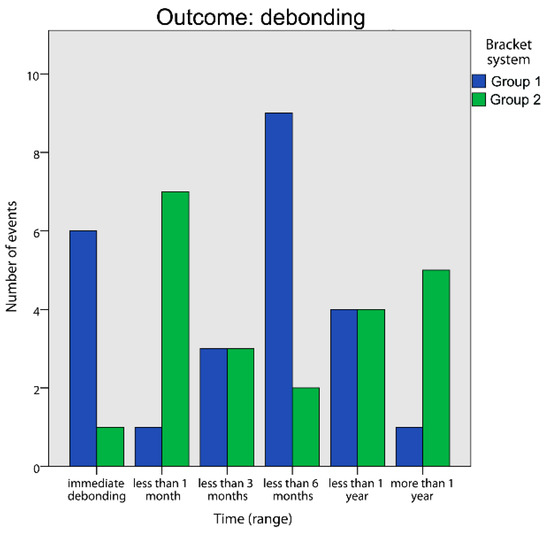
Figure 1.
Frequency of debondings over time for Group 1 and Group 2.
The Log-rank test comparing the Kaplan–Meier survival curves (Figure 2) revealed no statistically significant difference between the two groups (p = 0.343), though the two curves differ in the middle part of the observational period. Upper incisors and canines were less prone to debond than premolars and molars (Table 3) showing a statistically significant difference (Table 4).
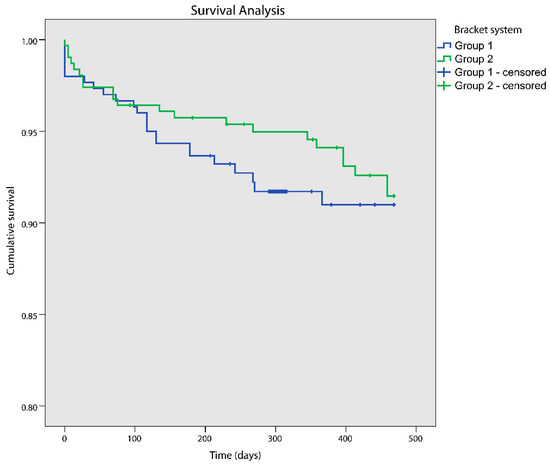
Figure 2.
Kaplan–Meier survival curves for Group 1 and Group 2. “Censored” patients are patients where no debondings occurred within the study duration: the timepoints where they exit the study (after minimum 6 months follow-up) are marked by crosses on the survival curves.

Table 3.
Frequencies of debondings per tooth category.

Table 4.
Chi-squared test for debonding frequency between anterior and posterior brackets.
4. Discussion
Incognito™ customized brackets have an extended gold alloy base and are metal-casted. However, instead of fully customized brackets, some practitioners prefer to use standard lingual brackets and a straightwire archwire, instead of the “mushroom-shaped” robot-bended lingual archwire offered by the Incognito™ system. This implies that the brackets are placed more gingivally than usual, that the canines’ brackets are rotated 10–15°, and that some brackets are placed at an increased distance from the tooth surface [12]. This is performed on a digital setup derived from the malocclusion model: the brackets are digitally placed on each tooth on an ideal continuous arch. At this point, acrylic transfer jigs can be 3D-printed and used to place any commercial standard bracket, according to the individual preferences of the practitioner, on the malocclusion model at the exact planned position. The KommonBase system, with its extended bonding base, allows for single tooth bonding in presence of severely crowded teeth, or for rebonding in case of debonding [11].
Understanding the risk of bracket bonding failure with such techniques is of great importance, since bracket debondings have an impact on overall treatment time [17]. The overall failure rate for both types of lingual brackets (7.6%) was only slightly higher than the failure rate reported for labial straightwire brackets (5.7%) [18]. The present finding is in accordance with other studies that found similar failure rates between lingual and labial brackets [10,19]. The increased bonding surface and enamel sandblasting performed before lingual brackets bonding could suggest a decreased failure rate, although a systematic review with meta-analysis confirmed that enamel sandblasting does not provide an advantage in terms of bonding strength [20]. Moreover, MacColl et al. observed a significant effect of bracket’s base surface area on bonding strength up to an area of 6.82 mm2, beyond which it seems pointless to increase [21]. Because, however, conventional labial brackets and different types of lingual brackets can have a base area larger than this anyway (ranging from 9 mm2 to 35 mm2 [22]), this can further explain the similar failure rate observed in the present study.
Posterior teeth were more prone to failure than incisors and canines, both in the upper and in the lower jaws. A similar result has been reported by many authors [19,23,24,25] and could be attributed to an increased occlusal force in the posterior area, although some contrasting findings are also present [26,27]. Never the less, this trend is similar for labial brackets [17]. Observing 150 patients over seven months, Khan et al. reported a failure rate of 6.4% for labial brackets, also reporting an increased failure rate for conditions like increased overbite, adolescents, lower arch, posterior teeth, and rounded NiTi wires [28]. Similarly, in a retrospective study on labial brackets, Sukhia et al. reported a failure risk 7.7 times higher for posterior teeth, and a risk increased by 1.15 times for every 1 mm increase in overbite [29].
The greatest number of debondings was observed during the earliest phase of treatment, within three to six months from the start of treatment (Figure 1). As bonding strength is not time-dependent [30], immediate failures can be ascribed to occlusal interferences or procedural mistakes, whilst debondings that happen later on can be attributed to the patient’s compliance, dietary habits or other factors. In addition, because only first time failures were considered, it is also possible that fewer failures in the long term were observed because the brackets most prone to failure were already debonded at that time.
Regarding the comparison of failure rates between the groups, no significant difference was observed. In a previous randomized clinical trial [4], the failure rate over a 12-month period for the Incognito and the Harmony lingual systems ranged from 1.9% to 5.5% with the use of different bonding materials and procedures. Sung et al. observed in an in vitro study that the extended resin base of the KommonBase system provided greater values of debonding force and shear bond strength compared to the Incognito system [31]. In another in vitro study, the KommonBase system showed significantly higher shear bond strength than Incognito™ brackets [22]. However, the results of the present study suggest that in vivo the KommonBase system is not offering a significant advantage over the Incognito system in terms of bracket failure rate, yet not bringing a disadvantage either. Therefore, the choice between the two systems should not rely on bond strength, the main advantage of the KommonBase system being the possibility to use any standard commercial lingual bracket, combined with an extended anatomic bonding base. Another interesting advantage of the KommonBase system is the possibility to bond each tooth individually if needed, due to the self-positioning base [11,12,13]. This can be an advantage in case of major crowding, or when some extractions are planned. However, data are needed about the accuracy of the bonding and re-bonding procedure, and this might be the topic of future studies.
Concerning the limitations of the present study, the limited sample size and the retrospective nature of this study did not allow to control some confounding factors, like the dietary habits of the patients. In addition, the two bracket systems were bonded using different materials: although this could be considered as a source of bias, the purpose of this study was not to compare two bonding materials, but the overall clinical performance of a lingual bracket system.
5. Conclusions
Lingual brackets bonded with the KommonBase system showed a failure rate of 8%. No difference was observed in terms of bracket survival between the KommonBase system and the Incognito™ customized lingual appliance. Most debondings occurred during the first 6 months. Upper incisors and canines were less prone to debond than premolars and molars.
Author Contributions
Conceptualization, M.A.C.; formal analysis, M.A.C. and M.T.; investigation, M.A.C. and P.M.C.; resources, C.M. and D.F.; validation, P.M.C.; writing—original draft preparation, M.T.; writing—review and editing, P.M.C. and M.A.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. Ethical review and approval were waived at the time of the study, because of its retrospective observational nature.
Informed Consent Statement
Patient consent was waived due to the retrospective nature of the study. Data analyzed were fully anonymized.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Shalish, M.; Cooper-Kazaz, R.; Ivgi, I.; Canetti, L.; Tsur, B.; Bachar, E.; Chaushu, S. Adult patients’ adjustability to orthodontic appliances. Part I: A comparison between Labial, Lingual, and InvisalignTM. Eur. J. Orthod. 2012, 34, 724–730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paul, W. Bonding techniques in lingual orthodontics. J. Orthod. 2013, 40, s20–s26. [Google Scholar] [CrossRef] [PubMed]
- Shpack, N.; Geron, S.; Floris, I.; Davidovitch, M.; Brosh, T.; Vardimon, A.D. Bracket placement in lingual vs labial systems and direct vs indirect bonding. Angle Orthod. 2007, 77, 509–517. [Google Scholar] [CrossRef] [Green Version]
- Mavreas, D.; Cuzin, J.F.; Boonen, G.; Vande Vannet, B. The effect of various adhesives, enamel etching, and base treatment on the failure frequency of customized lingual brackets: A randomized clinical trial. Eur. J. Orthod. 2018, 40, 249–253. [Google Scholar] [CrossRef]
- Grauer, D.; Proffit, W.R. Accuracy in tooth positioning with a fully customized lingual orthodontic appliance. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 433–443. [Google Scholar] [CrossRef]
- Sondhi, A. Efficient and effective indirect bonding. Am. J. Orthod. Dentofac. Orthop. 1999, 115, 352–359. [Google Scholar] [CrossRef]
- Wiechmann, D. Lingual Orthodontics (Part 3): Intraoral Sandblasting and Indirect Bonding. J. Orofac. Orthop. 2000, 61, 280–291. [Google Scholar] [CrossRef]
- Czolgosz, I.; Cattaneo, P.M.; Cornelis, M.A. Computer-aided indirect bonding versus traditional direct bonding of orthodontic brackets: Bonding time, immediate bonding failures, and cost-minimization. A randomized controlled trial. Eur. J. Orthod. 2021, 43, 144–151. [Google Scholar] [CrossRef]
- Silverman, E.; Cohen, M.; Gianelly, A.A.; Dietz, V.S. A universal direct bonding system for both metal and plastic brackets. Am. J. Orthod. 1972, 62, 236–244. [Google Scholar] [CrossRef]
- Li, Y.; Mei, L.; Wei, J.; Yan, X.; Zhang, X.; Zheng, W.; Li, Y. Effectiveness, efficiency and adverse effects of using direct or indirect bonding technique in orthodontic patients: A systematic review and meta-analysis | Kopernio. BMC Oral Health 2019, 19, 137. [Google Scholar] [CrossRef] [Green Version]
- Komori, A.; Takemoto, K.; Shimoda, T.; Miyashita, W.; Scuzzo, G. Precise direct lingual bonding with the KommonBase. J. Clin. Orthod. 2013, 47, 42–49. [Google Scholar] [PubMed]
- Fillion, D. Lingual straightwire treatment with the Orapix system. J. Clin. Orthod. 2011, 45, 488–497. [Google Scholar] [PubMed]
- Komori, A.; Fujisawa, M.; Iguchi, S. Le collage direct précis de brackets orthodontiques linguaux avec KommonBase. Int. Orthod. 2010, 8, 14–27. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Pascadopoli, M.; Gallo, S.; Ricaldone, F.; Kramp, D.D.; Valla, M.; Gandini, P.; Scribante, A. Effect of Enamel Pretreatment with Pastes Presenting Different Relative Dentin Abrasivity (RDA) Values on Orthodontic Bracket Bonding Efficacy of Microfilled Composite Resin: In Vitro Investigation and Randomized Clinical Trial. Materials 2022, 15, 531. [Google Scholar] [CrossRef] [PubMed]
- Kafle, D.; Mishra, R.K.; Hasan, M.R.; Saito, T. A Retrospective Clinical Audit of Bracket Failure among Patients Undergoing Orthodontic Therapy. Int. J. Dent. 2020, 2020, 8810964. [Google Scholar] [CrossRef]
- Namdari, M.; Amdjadi, P.; Bayat, A.; Seifi, M.; Alzwghaibi, A. Comparison of the failure rate, bonding time and ARI score of two orthodontic bonding systems: Self-Etch Primer and Conventional Etching Primer: A systematic review and meta-analysis. Int. Orthod. 2021, 19, 566–579. [Google Scholar] [CrossRef]
- Stasinopoulos, D.; Papageorgiou, S.N.; Kirsch, F.; Daratsianos, N.; Jäger, A.; Bourauel, C. Failure patterns of different bracket systems and their influence on treatment duration: A retrospective cohort study. Angle Orthod. 2018, 88, 338–347. [Google Scholar] [CrossRef] [Green Version]
- Jung, M.H. Survival analysis of brackets and tubes: A twelve-month assessment. Angle Orthod. 2014, 84, 1034–1040. [Google Scholar] [CrossRef]
- Ziebura, T.; Hohoff, A.; Flieger, S.; Stamm, T. Accidental debondings: Buccal vs fully individualized lingual multibracket appliances. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 649–654. [Google Scholar] [CrossRef]
- Baumgartner, S.; Koletsi, D.; Verna, C.; Eliades, T. The Effect of Enamel Sandblasting on Enhancing Bond Strength of Orthodontic Brackets: A Systematic Review and Meta-analysis. J. Adhes. Dent. 2017, 19, 463–473. [Google Scholar] [CrossRef]
- MacColl, G.A.; Rossouw, P.E.; Titley, K.C.; Yamin, C. The relationship between bond strength and orthodontic bracket base surface area with conventional and microetched foil-mesh bases. Am. J. Orthod. Dentofacial Orthop. 1998, 113, 276–281. [Google Scholar] [CrossRef]
- Sha, H.N.; Choi, S.H.; Yu, H.S.; Hwang, C.J.; Cha, J.Y.; Kim, K.M. Debonding force and shear bond strength of an array of CAD/CAM-based customized orthodontic brackets, placed by indirect bonding—An In Vitro study. PLoS ONE 2018, 13, e0202952. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cal-Neto, J.P.E.; Quintão, C.A.; de Oliveira Almeida, M.A.; Miguel, J.A.M. Bond failure rates with a self-etching primer: A randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 782–786. [Google Scholar] [CrossRef] [PubMed]
- Kinch, A.P.; Taylor, H.; Warltler, R.; Oliver, R.G.; Newcombe, R.G. A clinical trial comparing the failure rates of directly bonded brackets using etch times of 15 or 60 seconds. Am. J. Orthod. Dentofac. Orthop. 1988, 94, 476–483. [Google Scholar] [CrossRef]
- Petracci, E.; Farella, M.; Galeone, C.; Albano, A.; Ferraroni, M.; Decarli, A. Survival analysis with clustered observations f orthodontic brackets. Stat. Med. 2009, 28, 3483–3491. [Google Scholar] [CrossRef]
- Pandis, N.; Eliades, T. A comparative in vivo assessment of the long-term failure rate of 2 self-etching primers. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 96–98. [Google Scholar] [CrossRef]
- Chapman, J.L. Bond failure rates of two self-ligating brackets: A randomised clinical trial—PubMed. Aust. Orthod. J 2011, 27, 139–144. [Google Scholar]
- Khan, H.; Mheissen, S.; Iqbal, A.; Jafri, A.R.; Alam, M.K. Bracket Failure in Orthodontic Patients: The Incidence and the Influence of Different Factors. BioMed Res. Int. 2022, 2022, 5128870. [Google Scholar] [CrossRef]
- Sukhia, R.H.; Sukhia, H.R.; Azam, S.I.; Nuruddin, R.; Rizwan, A.; Jalal, S. Predicting the bracket bond failure rate in orthodontic patients: A retrospective cohort study. Int. Orthod. 2019, 17, 208–215. [Google Scholar] [CrossRef]
- Hajrassie, M.K.A.; Khier, S.E. In-vivo and in-vitro comparison of bond strengths of orthodontic brackets bonded to enamel and debonded at various times. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 384–390. [Google Scholar] [CrossRef]
- Sung, J.W.; Kwon, T.Y.; Kyung, H.M. Debonding forces of three different customized bases of a lingual bracket system. Korean J. Orthod. 2013, 43, 235–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).