Daily Physical Activity and Sleep Measured by Wearable Activity Trackers during the Coronavirus Disease 2019 Pandemic: A Lesson for Preventing Physical Inactivity during Future Pandemics
Abstract
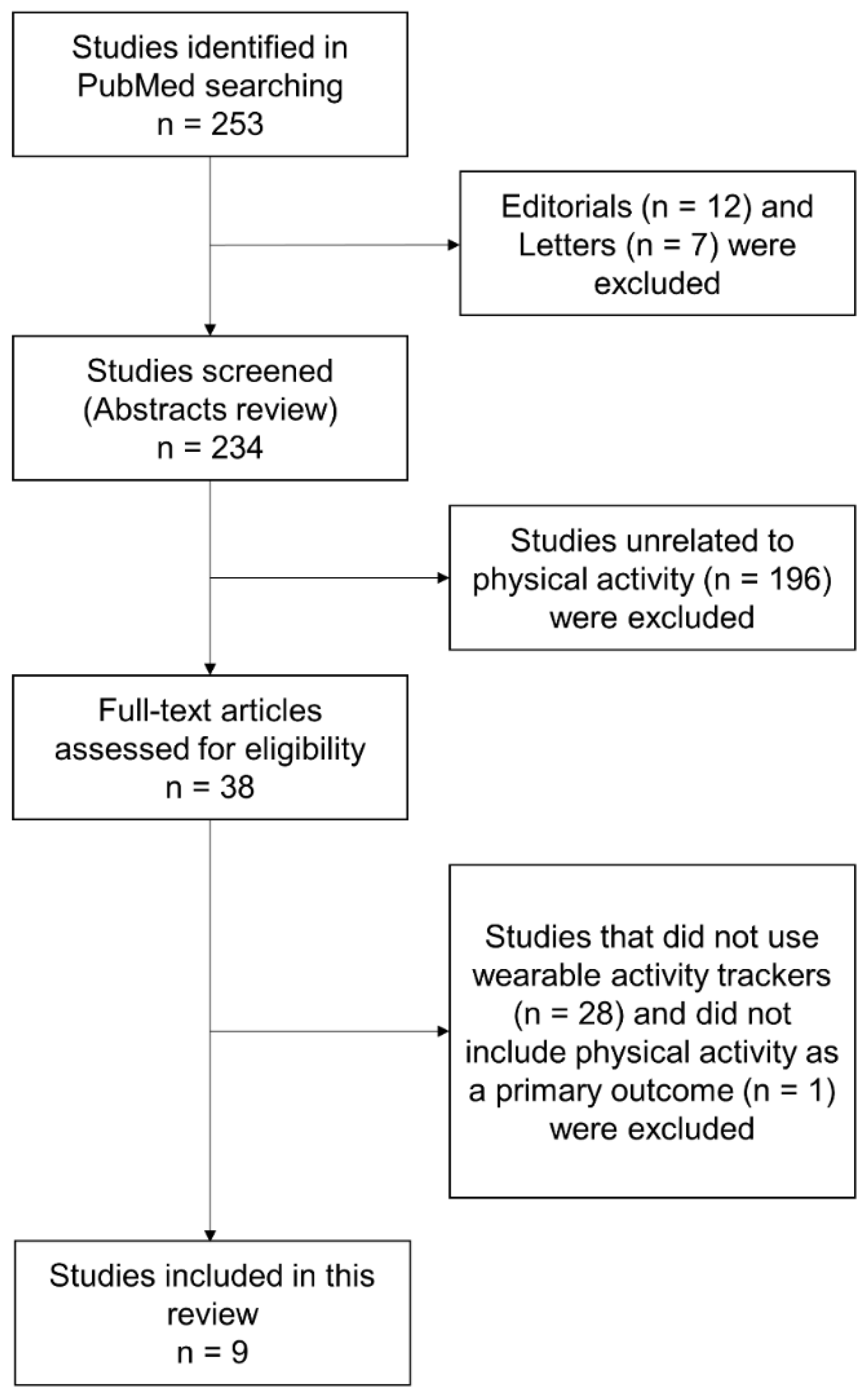
1. Introduction
2. Physical Activity during the COVID-19 Pandemic
3. Future Perspectives of Wearable Devices during Pandemics
4. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Coronavirus Cases–Worldometer. Available online: https://www.worldometers.info/coronavirus/ (accessed on 1 September 2021).
- Soh, S.M.; Kim, Y.; Kim, C.; Jang, U.S.; Lee, H.R. The rapid adaptation of SARS-CoV-2-rise of the variants: Transmission and resistance. J. Microbiol. 2021, 59, 807–818. [Google Scholar] [CrossRef]
- Alfano, V.; Ercolano, S. The Efficacy of Lockdown Against COVID-19: A Cross-Country Panel Analysis. Appl. Health Econ. Health Policy 2020, 18, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Thu, T.; Ngoc, P.; Hai, N.M.; Tuan, L.A. Effect of the social distancing measures on the spread of COVID-19 in 10 highly infected countries. Sci. Total Environ. 2020, 742, 140430. [Google Scholar] [CrossRef]
- Ding, X.; Clifton, D.; Ji, N.; Lovell, N.H.; Bonato, P.; Chen, W.; Yu, X.; Xue, Z.; Xiang, T.; Long, X.; et al. Wearable Sensing and Telehealth Technology with Potential Applications in the Coronavirus Pandemic. IEEE Rev. Biomed. Eng. 2021, 14, 48–70. [Google Scholar] [CrossRef] [PubMed]
- Hamasaki, H. Efficacy of wearable devices to measure and promote physical activity in the management of diabetes. Eur. Med. J. Diabetes 2018, 6, 62–69. [Google Scholar]
- Patel, V.; Orchanian-Cheff, A.; Wu, R. Evaluating the Validity and Utility of Wearable Technology for Continuously Monitoring Patients in a Hospital Setting: Systematic Review. JMIR Mhealth Uhealth 2021, 9, e17411. [Google Scholar] [CrossRef]
- Creaser, A.V.; Clemes, S.A.; Costa, S.; Hall, J.; Ridgers, N.D.; Barber, S.E.; Bingham, D.D. The Acceptability, Feasibility, and Effectiveness of Wearable Activity Trackers for Increasing Physical Activity in Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6211. [Google Scholar] [CrossRef]
- Singh, B.; Zopf, E.M.; Howden, E.J. Effect and feasibility of wearable physical activity trackers and pedometers for increasing physical activity and improving health outcomes in cancer survivors: A systematic review and meta-analysis. J. Sport Health Sci. 2021. [Google Scholar] [CrossRef]
- McDonough, D.J.; Su, X.; Gao, Z. Health wearable devices for weight and BMI reduction in individuals with overweight/obesity and chronic comorbidities: Systematic review and network meta-analysis. Br. J. Sports Med. 2021, 55, 917–925. [Google Scholar] [CrossRef]
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020, 29, e13074. [Google Scholar] [CrossRef] [PubMed]
- Blume, C.; Schmidt, M.H.; Cajochen, C. Effects of the COVID-19 lockdown on human sleep and rest-activity rhythms. Curr. Biol. 2020, 30, R795–R797. [Google Scholar] [CrossRef]
- Wright, K.P., Jr.; Linton, S.K.; Withrow, D.; Casiraghi, L.; Lanza, S.M.; Iglesia, H.; Vetter, C.; Depner, C.M. Sleep in university students prior to and during COVID-19 Stay-at-Home orders. Curr. Biol. 2020, 30, R797–R798. [Google Scholar] [CrossRef]
- Gao, C.; Scullin, M.K. Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: Integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Med. 2020, 73, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.H.; Marek, J.; Nálevka, P. Crowdsourced smartphone data reveal altered sleep/wake pattern in quarantined Chinese during the COVID-19 outbreak. Chronobiol. Int. 2020, 37, 1181–1190. [Google Scholar] [CrossRef]
- Caputo, E.L.; Reichert, F.F. Studies of Physical Activity and COVID-19 during the Pandemic: A Scoping Review. J. Phys. Act. Health 2020, 17, 1275–1284. [Google Scholar] [CrossRef] [PubMed]
- Peçanha, T.; Goessler, K.F.; Roschel, H.; Gualano, B. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am. J. Physiol. Heart Circ. Physiol. 2020, 318, H1441–H1446. [Google Scholar] [CrossRef]
- Hamer, M.; Kivimäki, M.; Gale, C.R.; Batty, G.D. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK. Brain Behav. Immun. 2020, 87, 184–187. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T.; Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Sun, S.; Folarin, A.A.; Ranjan, Y.; Rashid, Z.; Conde, P.; Stewart, C.; Cummins, N.; Matcham, F.; Dalla Costa, G.; Simblett, S.; et al. RADAR-CNS Consortium. Using Smartphones and Wearable Devices to Monitor Behavioral Changes During COVID-19. J. Med. Internet Res. 2020, 22, e19992. [Google Scholar] [CrossRef]
- Raeisi, T.; Mozaffari, H.; Sepehri, N.; Darand, M.; Razi, B.; Garousi, N.; Alizadeh, M.; Alizadeh, S. The negative impact of obesity on the occurrence and prognosis of the 2019 novel coronavirus (COVID-19) disease: A systematic review and meta-analysis. Eat Weight Disord. 2021, 1–19. [Google Scholar] [CrossRef]
- Kańtoch, E.; Kańtoch, A. Cardiovascular and Pre-Frailty Risk Assessment during Shelter-In-Place Measures Based on Multimodal Biomarkers Collected from Smart Telemedical Wearables. J. Clin. Med. 2021, 10, 1997. [Google Scholar] [CrossRef]
- Mishra, R.; Park, C.; York, M.K.; Kunik, M.E.; Wung, S.F.; Naik, A.D.; Najafi, B. Decrease in Mobility during the COVID-19 Pandemic and Its Association with Increase in Depression among Older Adults: A Longitudinal Remote Mobility Monitoring Using a Wearable Sensor. Sensors 2021, 21, 3090. [Google Scholar] [CrossRef]
- Woodruff, S.J.; Coyne, P.; St-Pierre, E. Stress, physical activity, and screen-related sedentary behaviour within the first month of the COVID-19 pandemic. Appl. Psychol. Health Well Being 2021, 13, 454–468. [Google Scholar] [CrossRef]
- Sher, L. The impact of the COVID-19 pandemic on suicide rates. QJM 2020, 113, 707–712. [Google Scholar] [CrossRef] [PubMed]
- Ong, J.L.; Lau, T.; Massar, S.; Chong, Z.T.; Ng, B.; Koek, D.; Zhao, W.; Yeo, B.; Cheong, K.; Chee, M. COVID-19-related mobility reduction: Heterogenous effects on sleep and physical activity rhythms. Sleep 2021, 44, zsaa179. [Google Scholar] [CrossRef] [PubMed]
- Pépin, J.L.; Bruno, R.M.; Yang, R.Y.; Vercamer, V.; Jouhaud, P.; Escourrou, P.; Boutouyrie, P. Wearable Activity Trackers for Monitoring Adherence to Home Confinement During the COVID-19 Pandemic Worldwide: Data Aggregation and Analysis. J. Med. Internet Res. 2020, 22, e19787. [Google Scholar] [CrossRef] [PubMed]
- Capodilupo, E.R.; Miller, D.J. Changes in health promoting behavior during COVID-19 physical distancing: Utilizing wearable technology to examine trends in sleep, activity, and cardiovascular indicators of health. PLoS ONE 2021, 16, e0256063. [Google Scholar] [CrossRef]
- Zinner, C.; Matzka, M.; Leppich, R.; Kounev, S.; Holmberg, H.C.; Sperlich, B. The Impact of the German Strategy for Containment of Coronavirus SARS-CoV-2 on Training Characteristics, Physical Activity and Sleep of Highly Trained Kayakers and Canoeists: A Retrospective Observational Study. Front. Sports Act. Living 2020, 2, 579830. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.K.; Ndiaye, H.; Daniels, M.; Ahmed, F.; Triage-HF Plus investigators. Lockdown, slow down: Impact of the COVID-19 pandemic on physical activity-an observational study. Open Heart 2021, 8, e001600. [Google Scholar] [CrossRef] [PubMed]
- Evenson, K.R.; Goto, M.M.; Furberg, R.D. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 159. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, A.; Johannessen, E.; Hartvigsen, G.; Grimsgaard, S.; Hopstock, L.A. Consumer-Based Activity Trackers as a Tool for Physical Activity Monitoring in Epidemiological Studies During the COVID-19 Pandemic: Development and Usability Study. JMIR Public Health Surveill. 2021, 7, e23806. [Google Scholar] [CrossRef]
- Tan, L.; Yu, K.; Bashir, A.K.; Cheng, X.; Ming, F.; Zhao, L.; Zhou, X. Toward real-time and efficient cardiovascular monitoring for COVID-19 patients by 5G-enabled wearable medical devices: A deep learning approach. Neural Comput. Appl. 2021, 1–14. [Google Scholar] [CrossRef]
- Jiang, W.; Majumder, S.; Subramaniam, S.; Li, X.; Khedri, R.; Monday, T.; Abolghasemian, M.; Satia, I.; Deen, M.J. A Wearable Tele-Health System towards Monitoring COVID-19 and Chronic Diseases. IEEE Rev. Biomed. Eng. 2021. [Google Scholar] [CrossRef]
- Quer, G.; Radin, J.M.; Gadaleta, M.; Baca-Motes, K.; Ariniello, L.; Ramos, E.; Kheterpal, V.; Topol, E.J.; Steinhubl, S.R. Wearable sensor data and self-reported symptoms for COVID-19 detection. Nat. Med. 2021, 27, 73–77. [Google Scholar] [CrossRef]
- Unnikrishnan, R.; Misra, A. Diabetes and COVID19: A bidirectional relationship. Nutr. Diabetes 2021, 11, 21. [Google Scholar] [CrossRef] [PubMed]
- The Lancet Diabetes Endocrinology. Metabolic health: A priority for the post-pandemic era. Lancet Diabetes Endocrinol. 2021, 9, 189. [Google Scholar] [CrossRef]
- Hall, K.S.; Hyde, E.T.; Bassett, D.R.; Carlson, S.A.; Carnethon, M.R.; Ekelund, U.; Evenson, K.R.; Galuska, D.A.; Kraus, W.E.; Lee, I.M.; et al. Systematic review of the prospective association of daily step counts with risk of mortality, cardiovascular disease, and dysglycemia. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 78. [Google Scholar] [CrossRef] [PubMed]
- He, Z.; Wu, H.; Yu, F.; Fu, J.; Sun, S.; Huang, T.; Wang, R.; Chen, D.; Zhao, G.; Quan, M. Effects of Smartphone-Based Interventions on Physical Activity in Children and Adolescents: Systematic Review and Meta-analysis. JMIR Mhealth Uhealth 2021, 9, e22601. [Google Scholar] [CrossRef] [PubMed]
- Mercer, K.; Giangregorio, L.; Schneider, E.; Chilana, P.; Li, M.; Grindrod, K. Acceptance of Commercially Available Wearable Activity Trackers Among Adults Aged Over 50 and With Chronic Illness: A Mixed-Methods Evaluation. JMIR Mhealth Uhealth 2016, 4, e7. [Google Scholar] [CrossRef]
- Global Digital Overview. DataReportal–Global Digital Insights. Available online: https://datareportal.com/global-digital-overview (accessed on 26 September 2021).
- Colorafi, K. Connected health: A review of the literature. Mhealth 2016, 2, 13. [Google Scholar] [CrossRef][Green Version]
- Macridis, S.; Johnston, N.; Johnson, S.; Vallance, J.K. Consumer physical activity tracking device ownership and use among a population-based sample of adults. PLoS ONE 2018, 13, e0189298. [Google Scholar] [CrossRef] [PubMed]
- Gualtieri, L.; Rosenbluth, S.; Phillips, J. Can a Free Wearable Activity Tracker Change Behavior? The Impact of Trackers on Adults in a Physician-Led Wellness Group. JMIR Res. Protoc. 2016, 5, e237. [Google Scholar] [CrossRef] [PubMed]
- Shemilt, I.; Hollands, G.J.; Marteau, T.M.; Nakamura, R.; Jebb, S.A.; Kelly, M.P.; Suhrcke, M.; Ogilvie, D. Economic instruments for population diet and physical activity behaviour change: A systematic scoping review. PLoS ONE 2013, 8, e75070. [Google Scholar] [CrossRef] [PubMed]
- Jacob, S.; Lawarée, J. The adoption of contact tracing applications of COVID-19 by European governments. Policy Des. Pract. 2021, 4, 44–58. [Google Scholar]
| Authors, Year | Subjects Countries | Study Design Study Period | Wearable Activity Trackers | Results |
|---|---|---|---|---|
| Sun et al., 2020 [20] | 1062 patients with major depressive disorder or multiple sclerosis in Italy, Spain, Denmark, the United Kingdom, and Netherlands Age: No description BMI: No description | Prospective cohort study a part of the RADAR-CNS studies Between 1 February 2019 and 5 July 2020 | Smartphone Fitbit | Daily step count↓ in young subjects Heart rate↓ Time spent on social media↑ Sleep duration↑ |
| Kańtoch E and Kańtoch A, 2021 [22] | 5 adult volunteers (2 men and 3 women, 2 subjects with history of cardiovascular diseases) Poland Age: 57 ± 22.38 years BMI: 27.80 ± 2.95 kg/m2 | Retrospective observational study Between 22 January 2019 and 30 April 2020 | Fitbit Versa smartwatch | Daily step count↓ Resting heart rate↓ Sleep duration→ |
| Mishra et al., 2021 [23] | 10 community-dwelling older adults (6 men and 4 women) United States Age: 77.3 ± 1.9 years BMI: 27.5 ± 1.6 kg/m2 | Prospective observational study Between January-March 2020 and March–September 2020 | ActivePERS/PAMSys pendant | Daily step count↓ Standing%↓ Walking%↓ Sitting%↑ Sleep quality→ |
| Woodruff et al., 2021 [24] | 121 subjects (23 men, 96 women, 1 cisgender, and 1 unknown) Canada Age: 36.2 ± 13.12 years BMI: No description | Prospective observational study Between March 2020 and April 2020 | Various activity trackers, e.g., Apple Watch, Fitbit, Samsung, and Garmin | Daily step count↓ Sedentary time↑ |
| Ong et al., 2021 [26] | 1824 city-dwelling, working adults (883 men and 941 women) Singapore Age: 30.94 ± 4.62 years BMI: No description | Prospective cohort study Between 2 January 2020 and 27 April 2020 | Fitbit | Daily step count↓ Time spent on moderate-to-vigorous activity↓ Resting heart rate↓ Sleep duration↑ Sleep efficiency→ |
| Pépin et al., 2020 [27] | Approximately 742,000 individuals using wearable activity trackers (proportion of women: 37.8%) Australia, Canada, China, France, Germany, Ireland, Italy, Japan, Netherlands, Singapore, Switzerland, United Kingdom, and United States Age: 35–46 years BMI: No description | Retrospective observational study Between 1 December 2019 and 13 April 2020 | Withings | The number of steps↓ in countries with lockdown The number of steps↑ in Sweden without lockdown |
| Capodilupo and Miller, 2021 [28] | 5436 individuals using a wearable activity tracker (3900 men and 1536 women) United States Age: 40.25 ± 11.33 years BMI: No description | Retrospective observational study Between 1 January 2020 and 15 May 2020 | WHOOP strap | Exercise frequency↑ in all subjects Exercise frequency↓ in subjects aged 18–25 years Resting heart rate↓ Heart rate variability↑ Sleep duration↑ |
| Zinner et al., 2020 [29] | 14 highly trained athletes (6 men and 8 women) Germany Age: 17.1 ± 1.9 years BMI: 22.9 ± 1.4 kg/m2 | Retrospective observational study During 4 weeks prior to and after the social distancing and lockdown on 23 March 2020 | Polar M430 | Training time↓ Time spent on light- and moderate-intensity physical activity↓ Sitting time↓ Time spent lying down↑ |
| Taylor et al., 2021 [30] | 311 patients with heart failure (240 men and 71 women) United Kingdom Age: 68.8 years BMI: <18.5 kg/m2 (0.7%), 18.5–24.9 kg/m2 (22.3%), 25–29.9 kg/m2 (32.8%), >30 (44.3%) | Prospective observational study During 4 weeks preceding and following the lockdown on 23 March 2020 | Triage HF | Daily physical activity↓ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hamasaki, H. Daily Physical Activity and Sleep Measured by Wearable Activity Trackers during the Coronavirus Disease 2019 Pandemic: A Lesson for Preventing Physical Inactivity during Future Pandemics. Appl. Sci. 2021, 11, 9956. https://doi.org/10.3390/app11219956
Hamasaki H. Daily Physical Activity and Sleep Measured by Wearable Activity Trackers during the Coronavirus Disease 2019 Pandemic: A Lesson for Preventing Physical Inactivity during Future Pandemics. Applied Sciences. 2021; 11(21):9956. https://doi.org/10.3390/app11219956
Chicago/Turabian StyleHamasaki, Hidetaka. 2021. "Daily Physical Activity and Sleep Measured by Wearable Activity Trackers during the Coronavirus Disease 2019 Pandemic: A Lesson for Preventing Physical Inactivity during Future Pandemics" Applied Sciences 11, no. 21: 9956. https://doi.org/10.3390/app11219956
APA StyleHamasaki, H. (2021). Daily Physical Activity and Sleep Measured by Wearable Activity Trackers during the Coronavirus Disease 2019 Pandemic: A Lesson for Preventing Physical Inactivity during Future Pandemics. Applied Sciences, 11(21), 9956. https://doi.org/10.3390/app11219956






