Establishment of a New Biomechanical Measurement Method for Surface Deformation of Bone by Force Application via Dental Implants—A Pilot Study
Featured Application
Abstract
1. Introduction
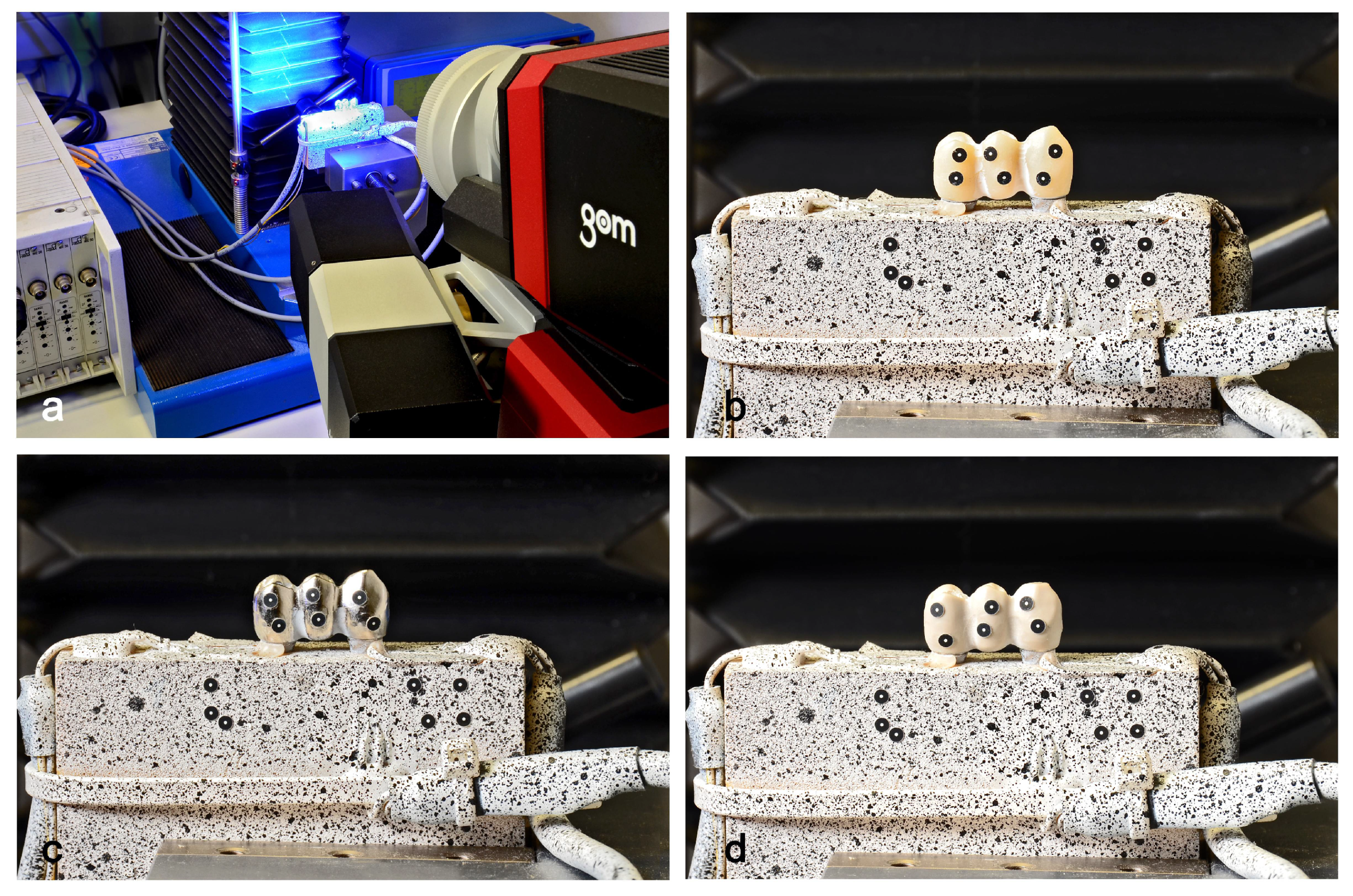
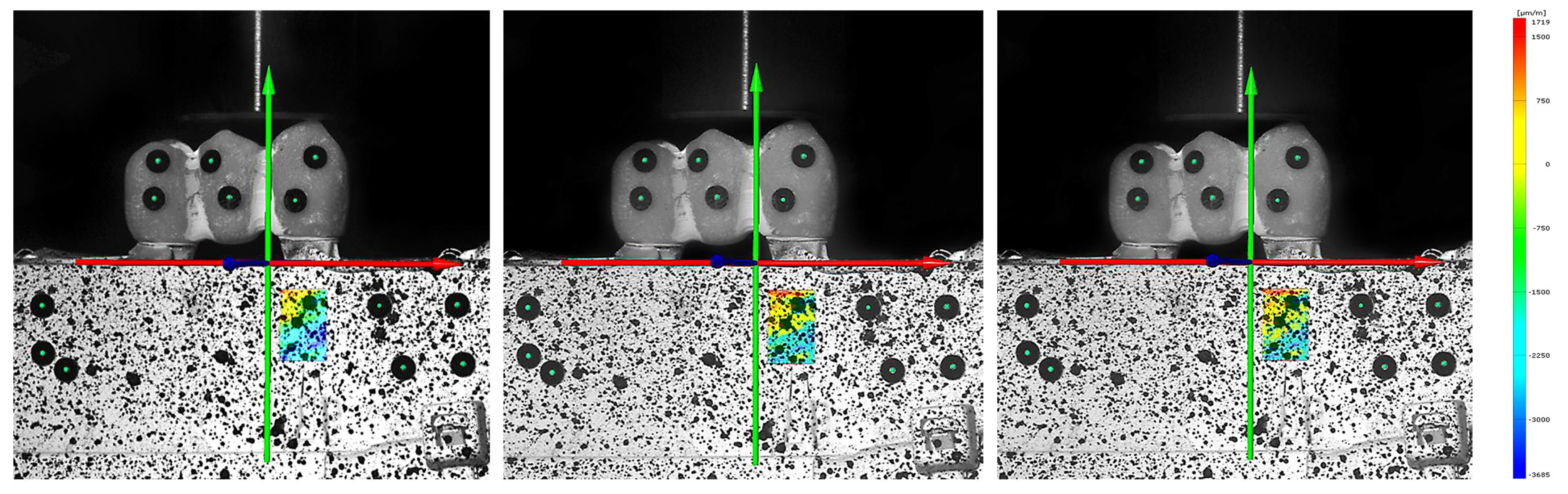
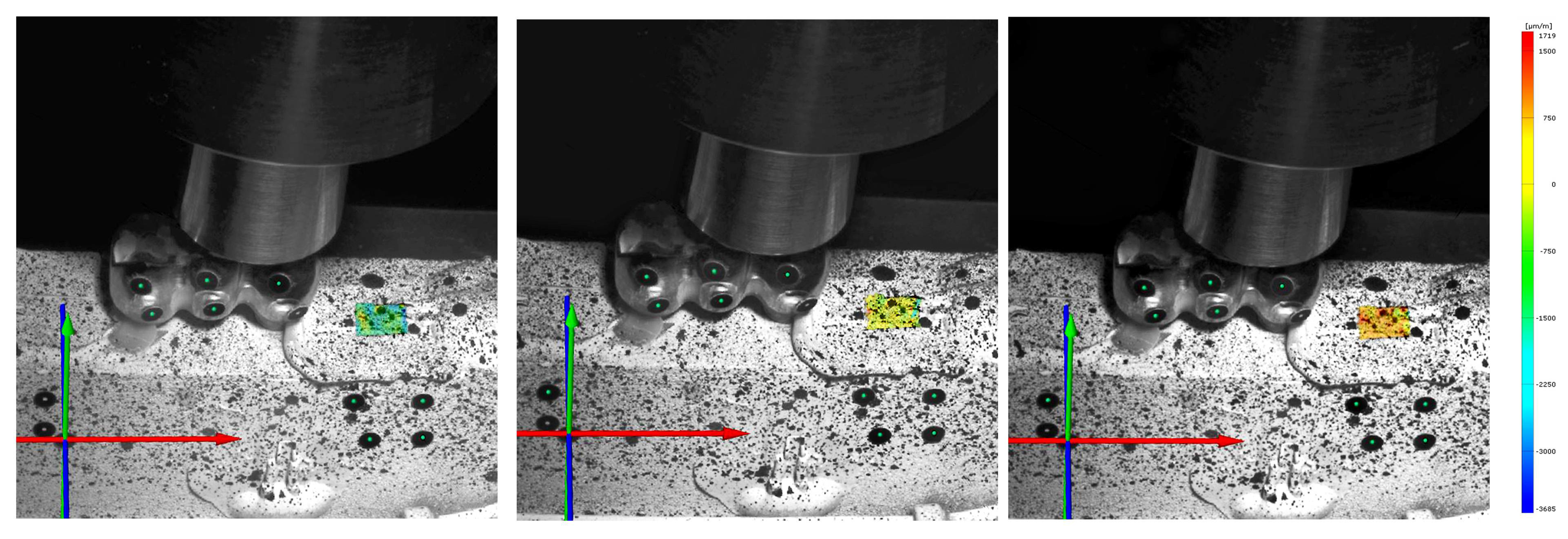
2. Materials and Methods
2.1. Calculation of the Strain ɛ for the Quarter-Bridge Circuit
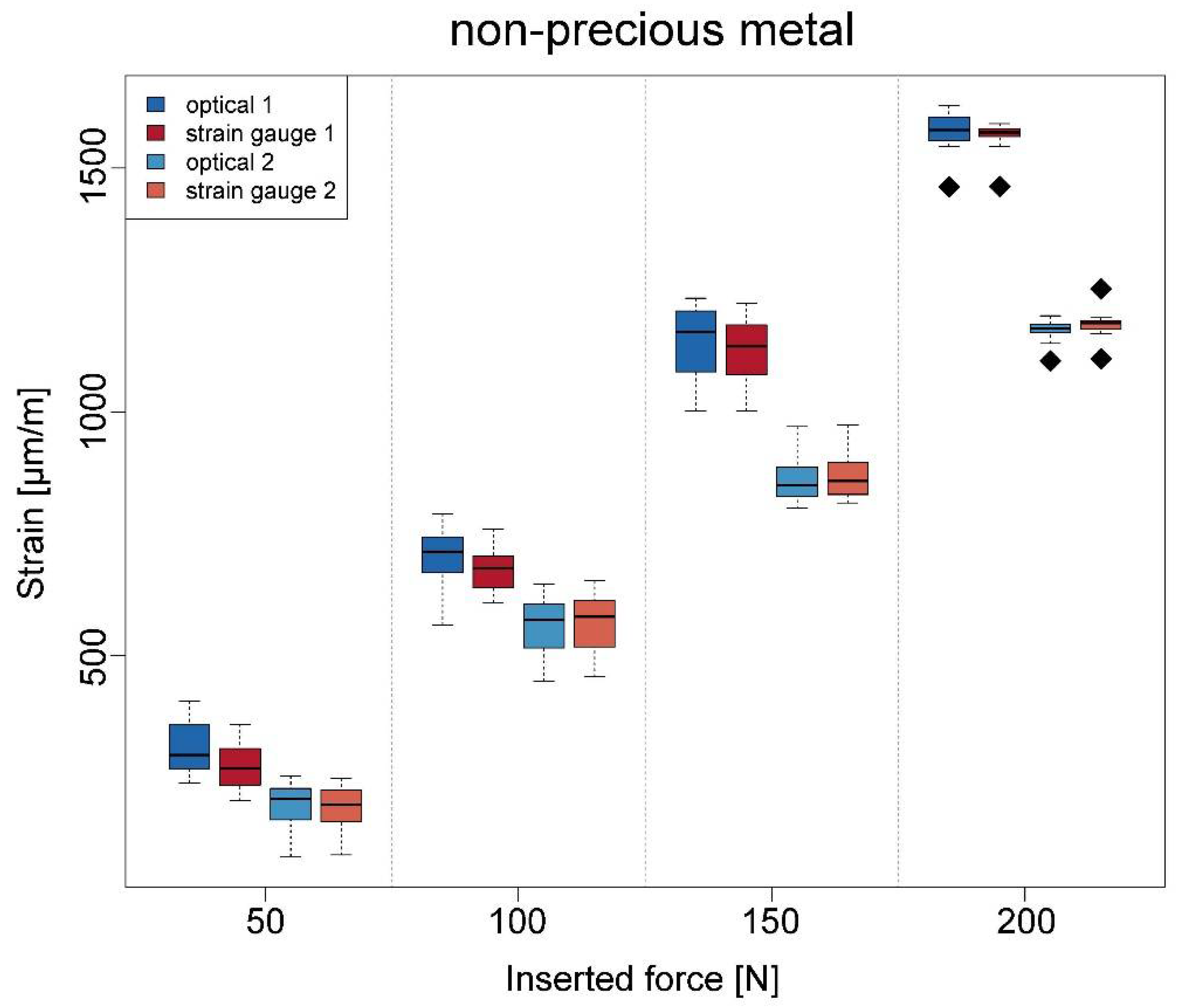
2.2. Results
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cehreli, M.C.; Iplikcioglu, H.; Bilir, O.G. The influence of the location of load transfer on strains around implants supporting four unit cement-retained fixed prostheses: In vitro evaluation of axial versus off-set loading. J. Oral Rehabil. 2002, 29, 394–400. [Google Scholar] [CrossRef]
- Frost, H.M. Wolff’s Law and bone’s structural adaptations to mechanical usage: An overview for clinicians. Angle Orthod. 1994, 64, 175–188. [Google Scholar] [PubMed]
- Wiskott, H.W.; Belser, U.C. Lack of integration of smooth titanium surfaces: A working hypothesis based on strains generated in the surrounding bone. Clin. Oral Implant. Res. 1999, 10, 429–444. [Google Scholar] [CrossRef]
- Frost, H.M. A 2003 update of bone physiology and Wolff’s Law for clinicians. Angle Orthod. 2004, 74, 3–15. [Google Scholar]
- de Vasconcellos, L.; G.Nishioka, R.S.; de Vasconcellos, L.M.; Balducci, I.; Kojima, A.N. Microstrain around dental implants supporting fixed partial prostheses under axial and non-axial loading conditions, in vitro strain gauge analysis. J. Craniofac. Surg. 2013, 24, e546–e551. [Google Scholar] [CrossRef] [PubMed]
- Nishioka, L.N.; Abreu, C.W.; de Vasconcellos, L.G.; Balducci, I. Machined and plastic copings in three-element prostheses with different types of implant-abutment joints: A strain gauge comparative analysis. J. Appl. Oral Sci. 2010, 18, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Kheiralla, L.S.; Younis, J.F. Peri-implant biomechanical responses to standard. short-wide. and mini implants supporting single crowns under axial and off-axial loading (an in vitro study). J. Oral Implantol. 2014, 40, 42–52. [Google Scholar] [CrossRef]
- Lee, J.H.; Frias, V.; Lee, K.W.; Wright, R.F. Effect of implant size and shape on implant success rates: A literature review. J. Prosthet. Dent. 2005, 94, 377–381. [Google Scholar] [CrossRef]
- Peixoto, H.E.; Bordin, D.; Del Bel Cury, A.A.; da Silva, W.J.; Faot, F. The role of prosthetic abutment material on the stress distribution in a maxillary single implant-supported fixed prosthesis. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 65, 90–96. [Google Scholar] [CrossRef]
- Takahashi, J.M.; Dayrell, A.C.; Consani, R.L.; de Arruda Nóbilo, M.A.; Henriques, G.E.; Mesquita, M.F. Stress evaluation of implant-abutment connections under different loading conditions: A 3D finite element study. J. Oral Implantol. 2015, 41, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Srirekha, A.; Bashetty, K. Infinite to finite: An overview of finite element analysis. Indian J. Dent. Res. 2010, 21, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Geng, J.P.; Tan, K.B.; Liu, G.R. Application of finite element analysis in implant dentistry: A review of the literature. J. Prosthet. Dent. 2001, 85, 585–598. [Google Scholar] [CrossRef] [PubMed]
- Reddy, M.S.; Sundram, R.; Abdemagyd, H.A.E. Application of Finite Element Model in Implant Dentistry: A Systematic Review. J. Pharm. Bioallied Sci. 2019, 11 (Suppl. 2), S85–S91. [Google Scholar] [CrossRef] [PubMed]
- Pesqueira, A.A.; Goiato, M.C.; Filho, H.G.; Monteiro, D.R.; Santos, D.M.; Haddad, M.F.; Pellizzer, E.P. Use of stress analysis methods to evaluate the biomechanics of oral rehabilitation with implants. J. Oral Implantol. 2014, 40, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Omori, M.; Sato, Y.; Kitagawa, N.; Shimura, Y.; Ito, M. A biomechanical investigation of mandibular molar implants: Reproducibility and validity of a finite element analysis model. Int. J. Implant. Dent. 2015, 1, 10. [Google Scholar] [CrossRef]
- Wakabayashi, N.; Ona, M.; Suzuki, T.; Igarashi, Y. Nonlinear finite element analyses: Advances and challenges in dental applications. J. Dent. 2008, 36, 463–471. [Google Scholar] [CrossRef]
- Ishikawa, Y.; Komada, W.; Inagaki, T.; Nemoto, R.; Omori, S.; Miura, H. The effects of post and core material combination on the surface strain of the 4-unit zirconia fixed partial denture margins. Dent. Mater. J. 2017, 36, 798–808. [Google Scholar] [CrossRef][Green Version]
- Karl, M.; Wichmann, M.G.; Winter, W.; Graef, F.; Taylor, T.D.; Heckmann, S.M. Influence of fixation mode and superstructure span upon strain development of implant fixed partial dentures. J. Prosthodont. 2008, 17, 3–8. [Google Scholar] [CrossRef]
- Shimura, Y.; Sato, Y.; Kitagawa, N.; Omori, M. Biomechanical effects of offset placement of dental implants in the edentulous posterior mandible. Int. J. Implant. Dent. 2016, 2, 17. [Google Scholar] [CrossRef]
- Grassi, L.; Isaksson, H. Extracting accurate strain measurements in bone mechanics: A critical review of current methods. J. Mech. Behav. Biomed. Mater. 2015, 50, 43–54. [Google Scholar] [CrossRef]
- Clelland, N.L.; Gilat, A.; McGlumphy, E.A.; Brantley, W.A. A photoelastic and strain gauge analysis of angled abutments for an implant system. Int. J. Oral Maxillofac. Implants 1993, 8, 541–548. [Google Scholar] [PubMed]
- Duyck, J.; Van Oosterwyck, H.; De Cooman, M.; Puers, R.; Vander Sloten, J.; Naert, I. Three-dimensional force measurements on oral implants: A methodological study. J. Oral Rehabil. 2000, 27, 744–753. [Google Scholar] [CrossRef] [PubMed]
- Nishioka, R.S.; de Vasconcellos, L.G.; de Melo Nishioka, G.N. Comparative strain gauge analysis of external and internal hexagon. Morse taper. and influence of straight and offset implant configuration. Implant Dent. 2011, 20, e24–e32. [Google Scholar] [CrossRef]
- Epprecht, A.; Zeltner, M.; Benic, G.; Özcan, M. A strain gauge analysis comparing 4-unit veneered zirconium dioxide implant-borne fixed dental prosthesis on engaging and non-engaging abutments before and after torque application. Clin. Exp. Dent. Res. 2018, 4, 13–18. [Google Scholar] [CrossRef]
- Karl, M.; Wichmann, M.G.; Heckmann, S.M.; Krafft, T. Strain development in 3-unit implant-supported CAD/CAM restorations. Int. J. Oral Maxillofac. Implants. 2008, 23, 648–652. [Google Scholar]
- Karl, M.; Holst, S. Strain development of screw-retained implant-supported fixed restorations: Procera implant bridge versus conventionally cast restorations. Int. J. Prosthodont. 2012, 25, 166–169. [Google Scholar]
- Asvanund, P. A strain gauge analysis comparing external and internal implant-abutment connections. Implant Dent. 2014, 23, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Cozzolino, F.; Apicella, D.; Wang, G.; Apicella, A.; Sorrentino, R. Implant-to-bone force transmission: A pilot study for in vivo strain gauge measurement technique. J. Mech. Behav. Biomed. Mater. 2019, 90, 173–181. [Google Scholar] [CrossRef]
- Crawshaw, A.H.; Hastings, G.W.; Dove, J. The implanted electrical resistance strain gauge: In vitro studies on data integrity. J. Med. Eng. Technol. 1991, 15, 72–77. [Google Scholar] [CrossRef]
- Wang, W.; Liu, H.; Huang, R.; Zhao, Y.; Huang, C.; Guo, S.; Shan, Y.; Li, L. Thermal Expansion and Magnetostriction Measurements at Cryogenic Temperature Using the Strain Gauge Method. Front. Chem. 2018, 6, 72. [Google Scholar] [CrossRef]
- Chengqun, G.; Legtenberg, R.; Tilmans, H.A.C.; Fluitman, J.H.J.; Elwenspoek, M. Nonlinearity and hysteresis of resonant strain gauges. J. Microelectromechan. Syst. 1998, 7, 122–127. [Google Scholar] [CrossRef]
- Sztefek, P.; Vanleene, M.; Olsson, R.; Collinson, R.; Pitsillides, A.A.; Shefelbine, S. Using digital image correlation to determine bone surface strains during loading and after adaptation of the mouse tibia. J. Biomech. 2010, 43, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Peterka, J.; Buranský, I. Using Aramis for Measurement of Deformation of Thin-Walled Parts during Milling; Research Papers; Faculty of Materials Science and Technology Slovak University of Technology: Trnava, Slovakia, 2011; Volume 18, pp. 45–50. [Google Scholar]
- Sojic, L.T.; Milic Lemic, A.; Tanasic, I.; Mitrovic, N.; Milosevic, M.; Petrovic, A. Compressive strains and displacement in a partially dentate lower jaw rehabilitated with two different treatment modalities. Gerodontology 2012, 29, e851–e857. [Google Scholar] [CrossRef] [PubMed]
- Bol, M.; Leichsenring, K.; Weichert, C.; Sturmat, M.; Schenk, P.; Blickhan, R.; Siebert, T. Three-dimensional surface geometries of the rabbit soleus muscle during contraction: Input for biomechanical modelling and its validation. Biomech. Model Mechanobiol. 2013, 12, 1205–1220. [Google Scholar] [CrossRef]
- Goellner, M.; Berthold, C.; Holst, S.; Petschelt, A.; Wichmann, M.; Schmitt, J. Influence of attachment and bone loss on the mobility of incisors and canine teeth. Acta. Odontol. Scand. 2013, 71, 656–663. [Google Scholar] [CrossRef]
- Goellner, M.; Berthold, C.; Holst, S.; Wichmann, M.; Schmitt, J. Correlations between photogrammetric measurements of tooth mobility and the Periotest method. Acta Odontol. Scand. 2012, 70, 27–35. [Google Scholar] [CrossRef]
- Miletic, V.; Peric, D.; Milosevic, M.; Manojlovic, D.; Mitrovic, N. Local deformation fields and marginal integrity of sculptable bulk-fill. low-shrinkage and conventional composites. Dent. Mater. 2016, 32, 1441–1451. [Google Scholar] [CrossRef] [PubMed]
- Minesaki, Y.; Murahara, S.; Kajihara, Y.; Takenouchi, Y.; Tanaka, T.; Suzuki, S.; Minami, H. Effect of metal conditioner on bonding of porcelain to cobalt-chromium alloy. J. Adv. Prosthodont. 2016, 8, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Skirbutis, G.; Dzingutė, A.; Masiliūnaitė, V.; Šulcaitė, G.; Žilinskas, J. PEEK polymer’s properties and its use in prosthodontics. A review. Stomatologija 2018, 20, 54–58. [Google Scholar] [PubMed]
- Zhang, Y.; Kelly, J.R. Dental Ceramics for Restoration and Metal Veneering. Dent. Clin. N. Am. 2017, 61, 797–819. [Google Scholar] [CrossRef]
- Huang, L.; Korhonen, R.K.; Turunen, M.J.; Finnilä, M.A.J. Experimental mechanical strain measurement of tissues. PeerJ 2019, 7, e6545. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Liu, H.; Huang, R.; Zhao, Y.; Huang, C.; Guo, S.; Shan, Y.; Li, L. Whole Field Strain Measurement on Complex Surfaces by Digital Speckle Pattern Interferometry. Mater. Eval. 2008, 66, 507–512. [Google Scholar] [PubMed]
- Abreu, C.W.; Nishioka, R.S.; Balducci, I.; Consani, R.L. Straight and offset implant placement under axial and nonaxial loads in implant-supported prostheses: Strain gauge analysis. J. Prosthodont. 2012, 21, 535–539. [Google Scholar] [CrossRef]
- Asundi, A.; Kishen, A. A strain gauge and photoelastic analysis of in vivo strain and in vitro stress distribution in human dental supporting structures. Arch. Oral Biol. 2000, 45, 543–550. [Google Scholar] [CrossRef]
- Zhang, D.; Arola, D.D. Applications of digital image correlation to biological tissues. J. Biomed. Opt. 2004, 9, 691–699. [Google Scholar] [CrossRef]
- Heary, R.F.; Parvathreddy, N.; Sampath, S.; Agarwal, N. Elastic modulus in the selection of interbody implants. J. Spine Surg. 2017, 3, 163–167. [Google Scholar] [CrossRef]
- Skalak, R. Biomechanical considerations in osseointegrated prostheses. J. Prosthet. Dent. 1983, 49, 843–848. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]

| Strain Gauge 1 (µm/m) | Strain Gauge 2 (µm/m) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Material | Load | Method | Mean | SD | Min. | Max. | Mean | SD | Min. | Max. |
| ceramics | 50 N | Optical | 282.5 | 39.9 | 218 | 355 | 225.4 | 44.6 | 143 | 277 |
| SG | 273.3 | 38.6 | 198 | 348 | 223.7 | 38.4 | 155 | 278 | ||
| 100 N | Optical | 639.7 | 54.6 | 560 | 738 | 571.6 | 62.0 | 471 | 672 | |
| SG | 640 | 51.8 | 562 | 719 | 582.0 | 57.2 | 494 | 686 | ||
| 150 N | Optical | 1078.7 | 50.1 | 986 | 1153 | 910.4 | 60.5 | 804 | 1009 | |
| SG | 1073.9 | 43.6 | 997 | 1172 | 933.9 | 50.7 | 862 | 1014 | ||
| 200 N | Optical | 1544.2 | 36.1 | 1449 | 1598 | 1252.1 | 15.2 | 1221 | 1278 | |
| SG | 1536.5 | 31.7 | 1436 | 1567 | 1259.4 | 10.2 | 1231 | 1273 | ||
| npm | 50 N | Optical | 312.3 | 54.9 | 239 | 406 | 195.1 | 47.5 | 88 | 253 |
| SG | 271.1 | 48.2 | 202 | 359 | 187.9 | 46.6 | 91 | 248 | ||
| 100 N | Optical | 703.5 | 60.6 | 563 | 791 | 556.8 | 60.2 | 448 | 647 | |
| SG | 674.8 | 42.6 | 609 | 760 | 564.4 | 59.2 | 457 | 653 | ||
| 150 N | Optical | 1143.3 | 75.6 | 1002 | 1233 | 861.9 | 46.3 | 802 | 970 | |
| SG | 119.6 | 69.3 | 1002 | 1223 | 867.1 | 47.3 | 813 | 973 | ||
| 200 N | Optical | 1575.7 | 41.2 | 1461 | 1628 | 1168.1 | 22.7 | 1104 | 1197 | |
| SG | 1564.9 | 31.4 | 1462 | 1591 | 1178.8 | 28.7 | 1109 | 1252 | ||
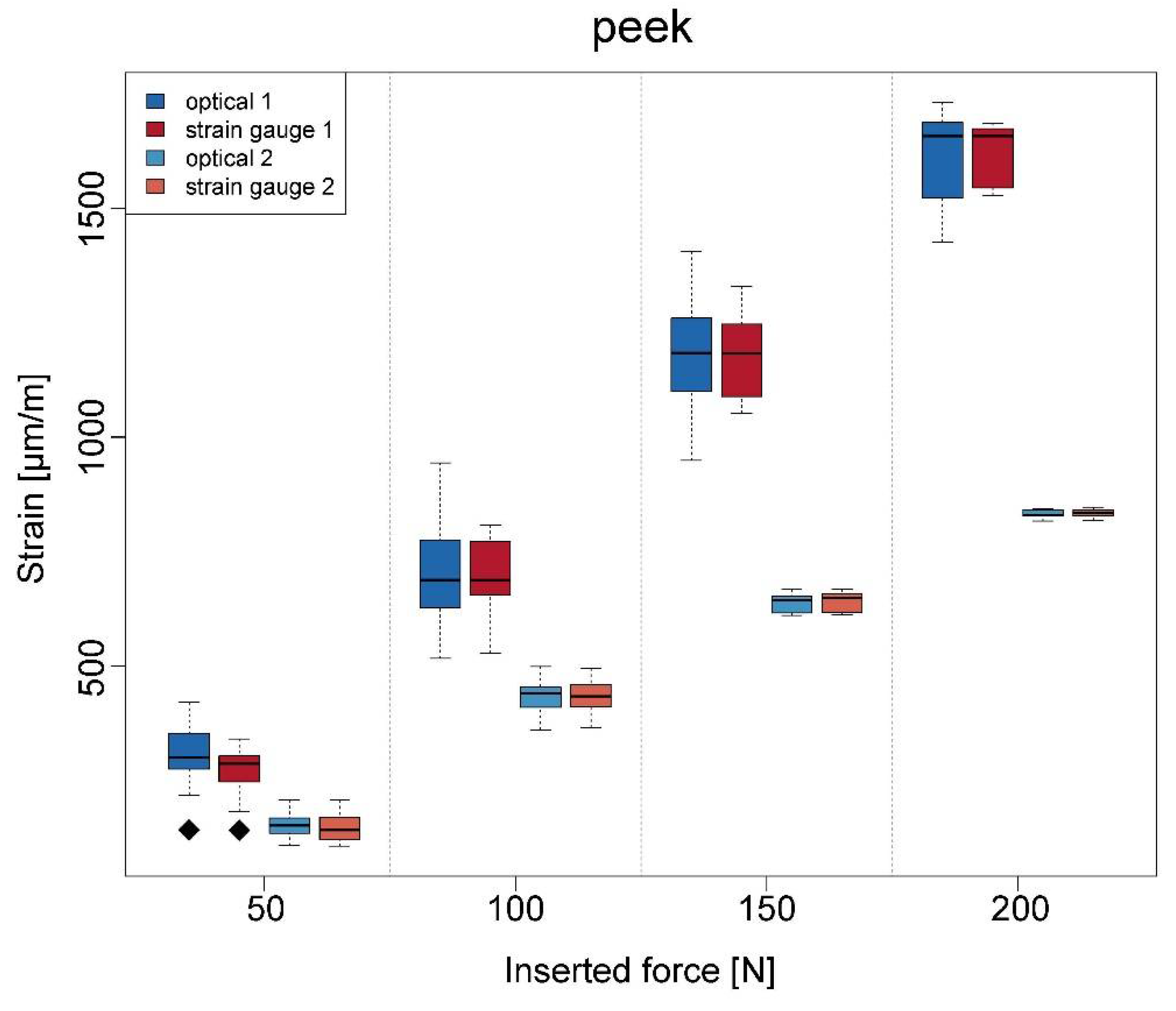
| PEEK | 50 N | Optical | 304.4 | 74.7 | 142 | 421 | 152.2 | 27.7 | 108 | 208 |
| SG | 272.5 | 55.1 | 142 | 341 | 147.7 | 31.4 | 107 | 207 | ||
| 100 N | Optical | 697.7 | 109.2 | 517 | 994 | 434.5 | 39.8 | 361 | 499 | |
| SG | 698.0 | 85.3 | 529 | 808 | 434.1 | 36.5 | 366 | 495 | ||
| 150 N | Optical | 1170.3 | 124.4 | 949 | 1405 | 639.1 | 20.5 | 611 | 667 | |
| SG | 1176.9 | 92.5 | 1052 | 1329 | 641.7 | 20.5 | 612 | 668 | ||
| 200 N | Optical | 1613.5 | 104.5 | 1426 | 1731 | 832.5 | 8.4 | 817 | 843 | |
| SG | 1616.9 | 67 | 528 | 1686 | 834.3 | 8.2 | 818 | 847 | ||
| Material | Ceramics | npm | PEEK | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Load | 50 N | 100 N | 150 N | 200 N | 50 N | 100 N | 150 N | 200 N | 50 N | 100 N | 150 N | 200 N |
| ICC | 0.90 | 0.96 | 0.89 | 0.90 | 0.59 | 0.60 | 0.79 | 0.82 | 0.72 | 0.90 | 0.93 | 0.81 |
| p-values | <0.001 | <0.001 | <0.001 | <0.001 | 0.135 | 0.034 | 0.021 | <0.001 | 0.052 | <0.001 | <0.001 | <0.001 |
| Material | Ceramics | npm | PEEK | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Load | 50 N | 100 N | 150 N | 200 N | 50 N | 100 N | 150 N | 200 N | 50 N | 100 N | 150 N | 200 N |
| ICC | 0.83 | 0.89 | 0.72 | 0.52 | 0.98 | 0.99 | 0.98 | 0.33 | 0.75 | 0.98 | 0.98 | 0.88 |
| p-values | <0.001 | <0.001 | 0.007 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matta, R.E.; Riegger, K.; Trägler, H.; Adler, W.; Eitner, S.; Wichmann, M.; Motel, C. Establishment of a New Biomechanical Measurement Method for Surface Deformation of Bone by Force Application via Dental Implants—A Pilot Study. Appl. Sci. 2021, 11, 7568. https://doi.org/10.3390/app11167568
Matta RE, Riegger K, Trägler H, Adler W, Eitner S, Wichmann M, Motel C. Establishment of a New Biomechanical Measurement Method for Surface Deformation of Bone by Force Application via Dental Implants—A Pilot Study. Applied Sciences. 2021; 11(16):7568. https://doi.org/10.3390/app11167568
Chicago/Turabian StyleMatta, Ragai Edward, Katharina Riegger, Horst Trägler, Werner Adler, Stephan Eitner, Manfred Wichmann, and Constantin Motel. 2021. "Establishment of a New Biomechanical Measurement Method for Surface Deformation of Bone by Force Application via Dental Implants—A Pilot Study" Applied Sciences 11, no. 16: 7568. https://doi.org/10.3390/app11167568
APA StyleMatta, R. E., Riegger, K., Trägler, H., Adler, W., Eitner, S., Wichmann, M., & Motel, C. (2021). Establishment of a New Biomechanical Measurement Method for Surface Deformation of Bone by Force Application via Dental Implants—A Pilot Study. Applied Sciences, 11(16), 7568. https://doi.org/10.3390/app11167568






