Postextraction Ridge Width Alterations Following Socket Seal Surgery—A Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Case Selection
2.2. Photographic Documentation
2.3. Surgical Technique
2.4. Measurements of the Alveolar Ridge Contour Changes
2.5. Soft Tissue Contour Analysis at 6 Months
2.6. Evaluation of the Soft Tissue Grafts at 1 week
- Group 1.
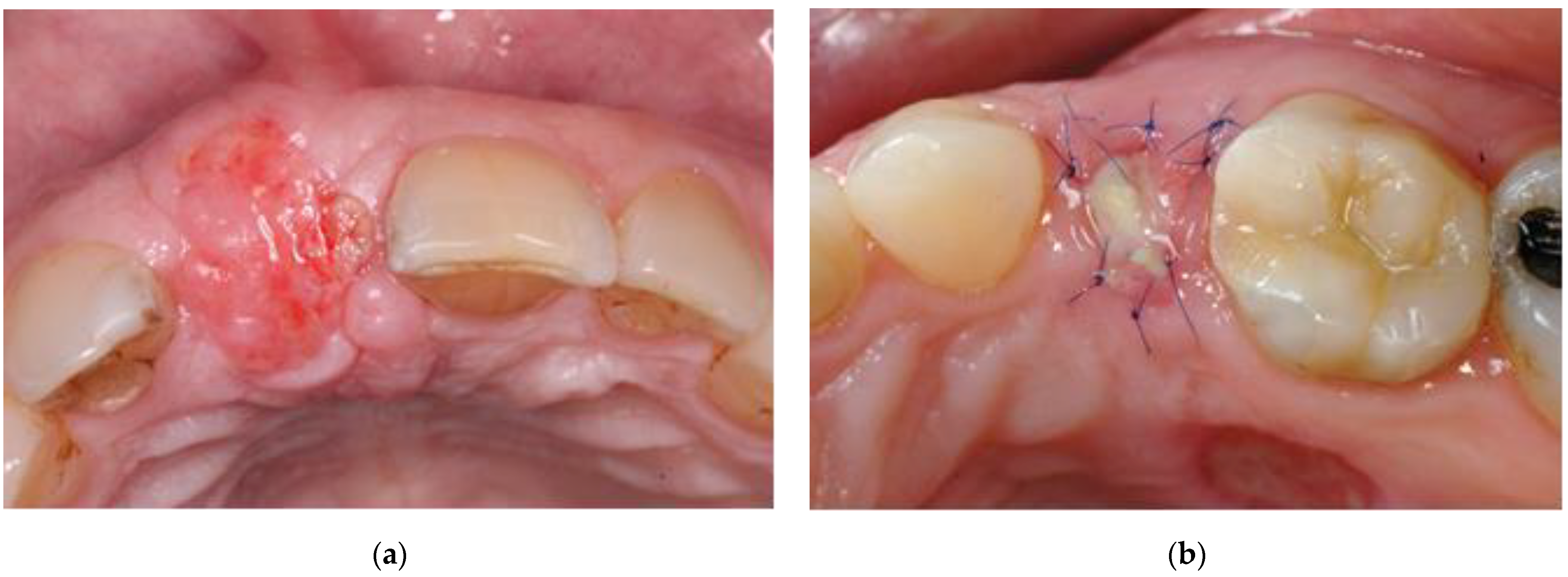
- Vital: reddish tissue color indicating the graft has integration of blood supply (Figure 2a).
- Group 2.
- Partially vital: part of the graft presented signs of vitality (as mentioned above) and another part showed signs of necrosis, i.e., amorphous white material (Figure 2b).
- Group 3.
- Necrotic: the graft was exfoliating or had a yellow-grayish color indicating lack of blood supply.
2.7. Statistical Analysis
3. Results
3.1. Postextraction Ridge Width Alterations at 6 Months
3.2. Assessment of Soft Tissue Contour at 6 Months
3.3. Evaluation of the Soft Tissue Grafts at 1 Week
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Amler, M.H.; Johnson, P.L.; Salman, I. Histological and histochemical investigation of human alveolar socket healing in undisturbed extraction wounds. J. Am. Dent. Assoc. 1960, 61, 32–44. [Google Scholar] [CrossRef] [PubMed]
- Pietrokovski, J.; Massler, M. Alveolar ridge resorption following tooth extraction. J. Prosthet. Dent. 1967, 17, 21–27. [Google Scholar] [CrossRef]
- Schropp, L.; Wenzel, A.; Kostopoulos, L.; Karring, T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int. J. Periodontics Restor. Dent. 2003, 23, 313–323. [Google Scholar]
- Araujo, M.G.; Lindhe, J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J. Clin. Periodontol. 2005, 32, 212–218. [Google Scholar] [CrossRef]
- Fickl, S.; Zuhr, O.; Wachtel, H.; Kebschull, M.; Hürzeler, M.B. Hard tissue alterations after socket preservation with additional buccal overbuilding: A study in the beagle dog. J. Clin. Periodontol. 2009, 36, 898–904. [Google Scholar] [CrossRef]
- Tan, W.L.; Wong, T.L.T.; Wong, M.C.M.; Lang, N.P. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin. Oral Implant. Res. 2012, 23, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Van Der Weijden, F.; Dell’Acqua, F.; Slot, D.E. Alveolar bone dimensional changes of post-extraction sockets in humans: A systematic review. J. Clin. Periodontol. 2009, 36, 1048–1058. [Google Scholar] [CrossRef]
- Araujo, M.G.; Sukekava, F.; Wennstrom, J.L.; Lindhe, J. Ridge alterations following implant placement in fresh extraction sockets: An experimental study in the dog. J. Clin. Periodontol. 2005, 32, 645–652. [Google Scholar] [CrossRef]
- Avila-Ortiz, G.; Chambrone, L.; Vignoletti, F. Effect of alveolar ridge preservation interventions following tooth extraction: A systematic review and meta-analysis. J. Clin. Periodontol. 2019, 46, 195–223. [Google Scholar] [CrossRef]
- Jung, R.E.; Ioannidis, A.; Hämmerle, C.H.F.; Thoma, D.S. Alveolar ridge preservation in the esthetic zone. Periodontol. 2000 2018, 77, 165–175. [Google Scholar] [CrossRef]
- Lekovic, V.; Kenney, E.B.; Weinlaender, M.; Han, T.; Klokkevold, P.; Nedic, M.; Orsini, M. A Bone Regenerative Approach to Alveolar Ridge Maintenance Following Tooth Extraction. Rep. 10 Cases 1997, 68, 563–570. [Google Scholar] [CrossRef]
- Iasella, J.M.; Greenwell, H.; Miller, R.L.; Hill, M.; Drisko, C.; Bohra, A.A.; Scheetz, J.P. Ridge Preservation with Freeze-Dried Bone Allograft and a Collagen Membrane Compared to Extraction Alone for Implant Site Development: A Clinical and Histologic Study in Humans. J. Periodontol. 2003, 74, 990–999. [Google Scholar] [CrossRef] [PubMed]
- Artzi, Z.; Nemcovsky, C.E. The Application of Deproteinized Bovine Bone Mineral for Ridge Preservation Prior to Implantation. Clinical and Histological Observations in a Case Report. J. Periodontol. 1998, 69, 1062–1067. [Google Scholar] [CrossRef] [PubMed]
- Carmagnola, D.; Adriaens, P.; Berglundh, T. Healing of human extraction sockets filled with Bio-OssR. Clin. Oral Implant. Res. 2003, 14, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Brugnami, F.; Caiazzo, A. Efficacy evaluation of a new buccal bone plate preservation technique: A pilot study. Int. J. Periodontics Restor. Dent. 2011, 31, 67–73. [Google Scholar]
- Clementini, M.; Agostinelli, A.; Castelluzzo, W.; Cugnata, F.; Vignoletti, F.; De Sanctis, M. The effect of immediate implant placement on alveolar ridge preservation compared to spontaneous healing after tooth extraction: Radiographic results of a randomized controlled clinical trial. J. Clin. Periodontol. 2019. [Google Scholar] [CrossRef]
- Canellas, J.; da Costa, R.C.; Breves, R.C.; de Oliveira, G.P.; Figueredo, C.; Fischer, R.G.; Thole, A.A.; Medeiros, P.J.D.; Ritto, F.G. Tomographic and histomorphometric evaluation of socket healing after tooth extraction using leukocyte- and platelet-rich fibrin: A randomized, single-blind, controlled clinical trial. J. Craniomaxillofac Surg 2020, 48, 24–32. [Google Scholar] [CrossRef]
- Bäumer, D.; Zuhr, O.; Rebele, S.; Hürzeler, M. Socket Shield Technique for immediate implant placement—Clinical, radiographic and volumetric data after 5 years. Clin. Oral Implant. Res. 2017, 28, 1450–1458. [Google Scholar] [CrossRef]
- Salama, H.; Salama, M. The role of orthodontic extrusive remodeling in the enhancement of soft and hard tissue profiles prior to implant placement: A systematic approach to the management of extraction site defects. Int. J. Periodontics Restor. Dent. 1993, 13, 312–333. [Google Scholar]
- Fickl, S.; Zuhr, O.; Wachtel, H.; Stappert, C.F.J.; Stein, J.M.; Hürzeler, M.B. Dimensional changes of the alveolar ridge contour after different socket preservation techniques. J. Clin. Periodontol. 2008, 35, 906–913. [Google Scholar] [CrossRef]
- Becker, W.; Becker, B.E. Guided tissue regeneration for implants placed into extraction sockets and for implant dehiscences: Surgical techniques and case report. Int. J. Periodontics Restor. Dent. 1990, 10, 376–391. [Google Scholar]
- Nemcovsky, C.E.; Artzi, Z.; Moses, O. Rotated palatal flap in immediate implant procedures. Clin. Oral Implant. Res. 2000, 11, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Becker, W.; Becker, B.E.; Caffesse, R. A Comparison of Demineralized Freeze-Dried Bone and Autologous Bone to Induce Bone Formation in Human Extraction Sockets. J. Periodontol. 1994, 65, 1128–1133. [Google Scholar] [CrossRef] [PubMed]
- Artzi, Z.; Tal, H.; Dayan, D. Porous Bovine Bone Mineral in Healing of Human Extraction Sockets. Part 1: Histomorphometric Evaluations at 9 Months. J. Periodontol. 2000, 71, 1015–1023. [Google Scholar] [CrossRef]
- Froum, S.; Cho, S.-C.; Rosenberg, E.; Rohrer, M.; Tarnow, D. Histological Comparison of Healing Extraction Sockets Implanted With Bioactive Glass or Demineralized Freeze-Dried Bone Allograft: A Pilot Study. J. Periodontol. 2002, 73, 94–102. [Google Scholar] [CrossRef]
- Serino, G.; Biancu, S.; Iezzi, G.; Piattelli, A. Ridge preservation following tooth extraction using a polylactide and polyglycolide sponge as space filler: A clinical and histological study in humans. Clin. Oral Implant. Res. 2003, 14, 651–658. [Google Scholar] [CrossRef]
- Faria-Almeida, R.; Astramskaite-Januseviciene, I.; Puisys, A.; Correia, F. Extraction Socket Preservation with or without Membranes, Soft Tissue Influence on Post Extraction Alveolar Ridge Preservation: A Systematic Review. J. Oral Maxillofacial Res. 2019, 10. [Google Scholar] [CrossRef]
- Canellas, J.V.D.S.; Medeiros, P.J.D.A.; Figueredo, C.M.D.S.; Fischer, R.G.; Ritto, F.G. Which is the best choice after tooth extraction, immediate implant placement or delayed placement with alveolar ridge preservation? A systematic review and meta-analysis. J. Cranio-Maxillofac. Surg. 2019, 47, 1793–1802. [Google Scholar] [CrossRef]
- Landsberg, C.J.; Bichacho, N. A modified surgical/prosthetic approach for optimal single implant supported crown. Part I--The socket seal surgery. Pract. Periodontics Aesthet Dent. 1994, 6, 11–17, quiz 19. [Google Scholar]
- Landsberg, C.J. Implementing Socket Seal Surgery as a Socket Preservation Technique for Pontic Site Development: Surgical Steps Revisited—A Report of Two Cases. J. Periodontol. 2008, 79, 945–954. [Google Scholar] [CrossRef]
- Jung, R.E.; Siegenthaler, D.W.; Hammerle, C.H. Postextraction tissue management: A soft tissue punch technique. Int. J. Periodontics Restor. Dent. 2004, 24, 545–553. [Google Scholar]
- Fickl, S.; Zuhr, O.; Wachtel, H.; Bolz, W.; Huerzeler, M.B. Hard tissue alterations after socket preservation: An experimental study in the beagle dog. Clin. Oral Implant. Res. 2008, 19, 1111–1118. [Google Scholar] [CrossRef] [PubMed]
- Tal, H. Autogenous masticatory mucosal grafts in extraction socket seal procedures: A comparison between sockets grafted with demineralized freeze-dried bone and deproteinized bovine bone mineral. Clin. Oral Implant. Res. 1999, 10, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-Y.; Kim, Y.-K.; Kim, H.-S.; Yun, P.-Y.; Kim, S.-G.; Choi, Y.-H. Extraction socket sealing using palatal gingival grafts and resorbable collagen membranes. Maxillofac. Plast. Reconstr. Surg. 2017, 39. [Google Scholar] [CrossRef] [PubMed]
- Oghli, A.A.; Steveling, H. Ridge preservation following tooth extraction: A comparison between atraumatic extraction and socket seal surgery. Quintessence Int. 2010, 41, 605–609. [Google Scholar] [PubMed]
- Thoma, D.S.; Bienz, S.P.; Lim, H.C.; Lee, W.Z.; Hämmerle, C.H.F.; Jung, R.E. Explorative randomized controlled study comparing soft tissue thickness, contour changes, and soft tissue handling of two ridge preservation techniques and spontaneous healing two months after tooth extraction. Clin. Oral Implant. Res. 2020, 31, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Rodd, H.D.; Malhotra, R.; O’Brien, C.H.; Elcock, C.; Davidson, L.E.; North, S. Change in supporting tissue following loss of a permanent maxillary incisor in children. Dent. Traumatol. 2007, 23, 328–332. [Google Scholar] [CrossRef]
- Chappuis, V.; Engel, O.; Reyes, M.; Shahim, K.; Nolte, L.P.; Buser, D. Ridge Alterations Post-extraction in the Esthetic Zone. J. Dent. Res. 2013, 92, 195S–201S. [Google Scholar] [CrossRef]
- Sun, M.; Gu, F.; Wang, J.; Zhou, C.; Xia, J.; Qin, H.; Yang, J. Measurement for natural dental neck data of normal adults and its clinical significance on guiding implant restoration. Int. J. Clin. Exp. Med. 2015, 8, 14732–14740. [Google Scholar]
- Watzek, G.; Haider, R.; Mensdorff-Pouilly, N.; Haas, R. Immediate and delayed implantation for complete restoration of the jaw following extraction of all residual teeth: A retrospective study comparing different types of serial immediate implantation. Int. J. Oral Maxillofac Implant. 1995, 10, 561–567. [Google Scholar]
- Slagter, K.W.; Den Hartog, L.; Bakker, N.A.; Vissink, A.; Meijer, H.J.A.; Raghoebar, G.M. Immediate Placement of Dental Implants in the Esthetic Zone: A Systematic Review and Pooled Analysis. J. Periodontol. 2014, 85, e241–e250. [Google Scholar] [CrossRef] [PubMed]
- Discepoli, N.; Vignoletti, F.; Laino, L.; De Sanctis, M.; Muñoz, F.; Sanz, M. Fresh extraction socket: Spontaneous healing vs. immediate implant placement. Clin. Oral Implant. Res. 2015, 26, 1250–1255. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Cortellini, P.; Graziani, F.; Cairo, F.; Lang, N.P.; Abundo, R.; Conforti, G.P.; Marquardt, S.; Rasperini, G.; Silvestri, M.; et al. Immediateversusdelayed implant placement after anterior single tooth extraction: The timing randomized controlled clinical trial. J. Clin. Periodontol. 2017, 44, 215–224. [Google Scholar] [CrossRef] [PubMed]
- Tonetti, M.S.; Jung, R.E.; Avila-Ortiz, G.; Blanco, J.; Cosyn, J.; Fickl, S.; Figuero, E.; Goldstein, M.; Graziani, F.; Madianos, P.; et al. Management of the extraction socket and timing of implant placement: Consensus report and clinical recommendations of group 3 of the XV European Workshop in Periodontology. J. Clin. Periodontol. 2019, 46, 183–194. [Google Scholar] [CrossRef] [PubMed]
- Jambhekar, S.; Kernen, F.; Bidra, A.S. Clinical and histologic outcomes of socket grafting after flapless tooth extraction: A systematic review of randomized controlled clinical trials. J. Prosthet. Dent. 2015, 113, 371–382. [Google Scholar] [CrossRef] [PubMed]
- Zitzmann, N.U.; Schärer, P.; Marinello, C.P. Factors influencing the success of GBR. J. Clin. Periodontol. 1999, 26, 673–682. [Google Scholar] [CrossRef] [PubMed]
- Dohan, D.M.; Choukroun, J.; Diss, A.; Dohan, S.L.; Dohan, A.J.J.; Mouhyi, J.; Gogly, B. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part II: Platelet-related biologic features. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2006, 101, e45–e50. [Google Scholar] [CrossRef]
- Areewong, K.; Chantaramungkorn, M.; Khongkhunthian, P. Platelet-rich fibrin to preserve alveolar bone sockets following tooth extraction: A randomized controlled trial. Clin. Implant. Dent. Relat. Res. 2019, 21, 1156–1163. [Google Scholar] [CrossRef]
- Moraschini, V.; Mourão, C.F.D.A.B.; Machado, R.C.D.M.; Nascimento, J.R.B.; Javid, K.; Calasans-Maia, M.D.; Cardarelli, A.; Montemezzi, P.; Calasans-Maia, J.D.A. Does Platelet-Rich Fibrin Decrease Dimensional Changes and Improve Postoperative Comfort in Post-Extraction Sockets? An Overview of Systematic Reviews. Appl. Sci. 2020, 10, 5750. [Google Scholar] [CrossRef]
- Thalmair, T.; Fickl, S.; Schneider, D.; Hinze, M.; Wachtel, H. Dimensional alterations of extraction sites after different alveolar ridge preservation techniques—A volumetric study. J. Clin. Periodontol. 2013, 40, 721–727. [Google Scholar] [CrossRef]

| Location | Number | Mean T6 Width/T0 Width (%) | Mean Change in Width (%) | SD |
|---|---|---|---|---|
| Incisors | 18 | 101.5 | 1.5 | 13.1 |
| Canines | 4 | 83.0 | −17.0 | 2.1 |
| Premolars | 14 | 89.5 | −10.5 | 11.2 |
| Total | 36 | 94.7 | −5.3 | 13.4 |
| Invaginations | |
|---|---|
| Incisors | 1 (5.5%) |
| Canines | 0 (0%) |
| Premolars | 4 (28.5%) |
| Total | 5 (13.9%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Landsberg, C.; Bender, O.; Weinreb, M.; Wigler, R.; Chackartchi, T.; Matalon, S.; Weinberg, E. Postextraction Ridge Width Alterations Following Socket Seal Surgery—A Retrospective Study. Appl. Sci. 2021, 11, 324. https://doi.org/10.3390/app11010324
Landsberg C, Bender O, Weinreb M, Wigler R, Chackartchi T, Matalon S, Weinberg E. Postextraction Ridge Width Alterations Following Socket Seal Surgery—A Retrospective Study. Applied Sciences. 2021; 11(1):324. https://doi.org/10.3390/app11010324
Chicago/Turabian StyleLandsberg, Cobi, Omer Bender, Miron Weinreb, Ronald Wigler, Tali Chackartchi, Shlomo Matalon, and Evgeny Weinberg. 2021. "Postextraction Ridge Width Alterations Following Socket Seal Surgery—A Retrospective Study" Applied Sciences 11, no. 1: 324. https://doi.org/10.3390/app11010324
APA StyleLandsberg, C., Bender, O., Weinreb, M., Wigler, R., Chackartchi, T., Matalon, S., & Weinberg, E. (2021). Postextraction Ridge Width Alterations Following Socket Seal Surgery—A Retrospective Study. Applied Sciences, 11(1), 324. https://doi.org/10.3390/app11010324







