Exosomal miR-92a Concentration in the Serum of Shift Workers
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjetct Enrollment
2.2. Clinical Parameters Collection
2.3. Determination of Serum Exosomal miR-92a
2.3.1. MiRNAs Extraction
2.3.2. Reverse Transcription
2.3.3. Relative qRT-PCR
2.4. Statistical Analysis
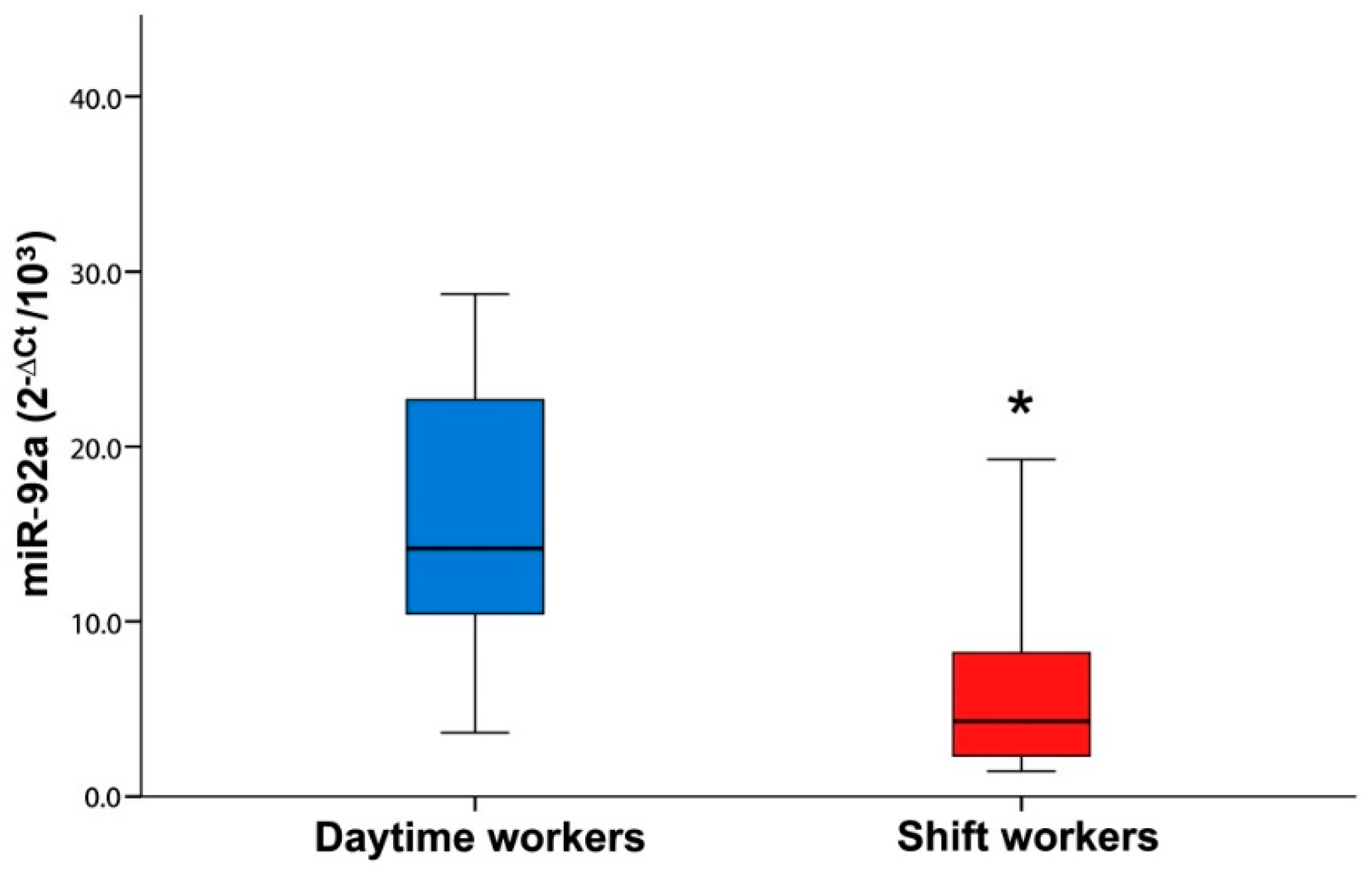
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Boivin, D.B.; Boudreau, P. Impacts of shift work on sleep and circadian rhythms. Pathol. Biol. 2014, 62, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Copertaro, A.; Bracci, M. Working against the biological clock: A review for the occupational physician. Ind. Health 2019, 57, 557–569. [Google Scholar] [CrossRef] [PubMed]
- Engin, A. Circadian rhythms in diet-induced obesity. Adv. Exp. Med. Biol. 2017, 960, 19–52. [Google Scholar] [PubMed]
- McHill, A.W.; Wright, K.P., Jr. Role of sleep and circadian disruption on energy expenditure and in metabolic predisposition to human obesity and metabolic disease. Obes. Rev. 2017, 18 (Suppl.S1), 15–24. [Google Scholar] [CrossRef]
- Bracci, M.; Copertaro, A.; Ciarapica, V.; Barbaresi, M.; Esposito, S.; Albanesi, A.; Valentino, M.; Ledda, C.; Rapisarda, V.; Santarelli, L. Nocturnin gene diurnal variation in healthy volunteers and expression levels in shift workers. BioMed Res. Int. 2019, 2019, 7582734. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.C.; Hoe, V.C.W.; Darus, A.; Bhoo-Pathy, N. Association between night-shift work, sleep quality and metabolic syndrome. Occup. Environ. Med. 2018, 75, 716–723. [Google Scholar] [CrossRef]
- Wang, F.; Zhang, L.; Zhang, Y.; Zhang, B.; He, Y.; Xie, S.; Li, M.; Miao, X.; Chan, E.Y.; Tang, J.L.; et al. Meta-analysis on night shift work and risk of metabolic syndrome. Obes. Rev. 2014, 15, 709–720. [Google Scholar] [CrossRef]
- Esquirol, Y.; Perret, B.; Ruidavets, J.B.; Marquie, J.C.; Dienne, E.; Niezborala, M.; Ferrieres, J. Shift work and cardiovascular risk factors: New knowledge from the past decade. Arch. Cardiovasc.Dis. 2011, 104, 636–668. [Google Scholar] [CrossRef]
- Puttonen, S.; Harma, M.; Hublin, C. Shift work and cardiovascular disease—Pathways from circadian stress to morbidity. Scand. J. Work Environ. Health 2010, 36, 96–108. [Google Scholar] [CrossRef]
- Roskoden, F.C.; Kruger, J.; Vogt, L.J.; Gartner, S.; Hannich, H.J.; Steveling, A.; Lerch, M.M.; Aghdassi, A.A. Physical activity, energy expenditure, nutritional habits, quality of sleep and stress levels in shift-working health care personnel. PLoS ONE 2017, 12, e0169983. [Google Scholar] [CrossRef]
- Cypess, A.M.; Lehman, S.; Williams, G.; Tal, I.; Rodman, D.; Goldfine, A.B.; Kuo, F.C.; Palmer, E.L.; Tseng, Y.H.; Doria, A.; et al. Identification and importance of brown adipose tissue in adult humans. N. Engl. J. Med. 2009, 360, 1509–1517. [Google Scholar] [CrossRef] [PubMed]
- van Marken Lichtenbelt, W.D.; Vanhommerig, J.W.; Smulders, N.M.; Drossaerts, J.M.; Kemerink, G.J.; Bouvy, N.D.; Schrauwen, P.; Teule, G.J. Cold-activated brown adipose tissue in healthy men. N. Engl. J. Med. 2009, 360, 1500–1508. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, K.A.; Lidell, M.E.; Orava, J.; Heglind, M.; Westergren, R.; Niemi, T.; Taittonen, M.; Laine, J.; Savisto, N.J.; Enerback, S.; et al. Functional brown adipose tissue in healthy adults. N. Engl. J. Med. 2009, 360, 1518–1525. [Google Scholar] [CrossRef] [PubMed]
- Yoneshiro, T.; Matsushita, M.; Nakae, S.; Kameya, T.; Sugie, H.; Tanaka, S.; Saito, M. Brown adipose tissue is involved in the seasonal variation of cold-induced thermogenesis in humans. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2016, 310, R999–R1009. [Google Scholar] [CrossRef] [PubMed]
- Giordano, A.; Frontini, A.; Cinti, S. Convertible visceral fat as a therapeutic target to curb obesity. Nat. Rev. Drug Discov. 2016, 15, 405–424. [Google Scholar] [CrossRef] [PubMed]
- Cinti, S. Adipose organ development and remodeling. Compr. Physiol. 2018, 8, 1357–1431. [Google Scholar] [PubMed]
- Cinti, S. Ucp1 protein: The molecular hub of adipose organ plasticity. Biochimie 2017, 134, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Fenzl, A.; Kiefer, F.W. Brown adipose tissue and thermogenesis. Horm. Mol. Biol. Clin. Investig. 2014, 19, 25–37. [Google Scholar] [CrossRef]
- Kiefer, F.W. The significance of beige and brown fat in humans. Endocr. Connect. 2017, 6, R70–R79. [Google Scholar] [CrossRef]
- Trajkovski, M.; Lodish, H. MicroRNA networks regulate development of brown adipocytes. Trends Endocrinol. Metab. 2013, 24, 442–450. [Google Scholar] [CrossRef]
- Bartelt, A.; Bruns, O.T.; Reimer, R.; Hohenberg, H.; Ittrich, H.; Peldschus, K.; Kaul, M.G.; Tromsdorf, U.I.; Weller, H.; Waurisch, C.; et al. Brown adipose tissue activity controls triglyceride clearance. Nat. Med. 2011, 17, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Zhang, M.; Xu, M.; Gu, W.; Xi, Y.; Qi, L.; Li, B.; Wang, W. Brown adipose tissue activation is inversely related to central obesity and metabolic parameters in adult human. PLoS ONE 2015, 10, e0123795. [Google Scholar] [CrossRef] [PubMed]
- Cinti, S. Anatomy and physiology of the nutritional system. Mol. Asp. Med. 2019, 68, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Cereijo, R.; Taxeras, S.D.; Piquer-Garcia, I.; Pellitero, S.; Martinez, E.; Tarasco, J.; Moreno, P.; Balibrea, J.; Puig-Domingo, M.; Jimenez-Pavon, D.; et al. Elevated levels of circulating miR-92a are associated with impaired glucose homeostasis in patients with obesity and correlate with metabolic status after bariatric surgery. Obes. Surg. 2019. [Google Scholar] [CrossRef] [PubMed]
- Saito, M.; Okamatsu-Ogura, Y.; Matsushita, M.; Watanabe, K.; Yoneshiro, T.; Nio-Kobayashi, J.; Iwanaga, T.; Miyagawa, M.; Kameya, T.; Nakada, K.; et al. High incidence of metabolically active brown adipose tissue in healthy adult humans: Effects of cold exposure and adiposity. Diabetes 2009, 58, 1526–1531. [Google Scholar] [CrossRef] [PubMed]
- Mello, C.C.; Conte, D., Jr. Revealing the world of RNA interference. Nature 2004, 431, 338–342. [Google Scholar] [CrossRef]
- Pfeifer, A.; Lehmann, H. Pharmacological potential of RNAi—Focus on miRNA. Pharmacol. Ther. 2010, 126, 217–227. [Google Scholar] [CrossRef]
- Meister, G.; Tuschl, T. Mechanisms of gene silencing by double-stranded RNA. Nature 2004, 431, 343–349. [Google Scholar] [CrossRef]
- Rong, X.; Jia, L.; Hong, L.; Pan, L.; Xue, X.; Zhang, C.; Lu, J.; Jin, Z.; Qiu, H.; Wu, R.; et al. Serum mir-92a-3p as a new potential biomarker for diagnosis of Kawasaki disease with coronary artery lesions. J. Cardiovasc. Transl. Res. 2017, 10, 1–8. [Google Scholar] [CrossRef]
- Raposo, G.; Stoorvogel, W. Extracellular vesicles: Exosomes, microvesicles, and friends. J. Cell Biol. 2013, 200, 373–383. [Google Scholar] [CrossRef]
- Yamamoto, T.; Kosaka, N.; Ochiya, T. Latest advances in extracellular vesicles: From bench to bedside. Sci. Technol. Adv. Mater. 2019, 20, 746–757. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Yu, F.; Ding, H.; Wang, Y.; Li, P.; Wang, K. Emerging function and clinical values of exosomal micrornas in cancer. Mol. Ther. Nucleic. Acids 2019, 16, 791–804. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Li, S.; Li, L.; Li, M.; Guo, C.; Yao, J.; Mi, S. Exosome and exosomal microRNA: Trafficking, sorting, and function. Genom. Proteom. Bioinform. 2015, 13, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, P.S.; Parkin, R.K.; Kroh, E.M.; Fritz, B.R.; Wyman, S.K.; Pogosova-Agadjanyan, E.L.; Peterson, A.; Noteboom, J.; O’Briant, K.C.; Allen, A.; et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc. Natl. Acad. Sci. USA 2008, 105, 10513–10518. [Google Scholar] [CrossRef] [PubMed]
- Huang, W. MicroRNAs: Biomarkers, diagnostics, and therapeutics. Methods Mol. Biol. 2017, 1617, 57–67. [Google Scholar] [PubMed]
- Engin, A.B. MicroRNA and adipogenesis. Adv. Exp. Med. Biol. 2017, 960, 489–509. [Google Scholar] [CrossRef] [PubMed]
- Loh, W.P.; Yang, Y.; Lam, K.P. MiR-92a enhances recombinant protein productivity in CHO cells by increasing intracellular cholesterol levels. Biotechnol. J. 2017, 12, 1600488. [Google Scholar] [CrossRef]
- Huang, Y.; Tang, S.; Ji-Yan, C.; Huang, C.; Li, J.; Cai, A.P.; Feng, Y.Q. Circulating miR-92a expression level in patients with essential hypertension: A potential marker of atherosclerosis. J. Hum. Hypertens. 2017, 31, 200–205. [Google Scholar] [CrossRef]
- Chen, Y.; Buyel, J.J.; Hanssen, M.J.; Siegel, F.; Pan, R.; Naumann, J.; Schell, M.; van der Lans, A.; Schlein, C.; Froehlich, H.; et al. Exosomal microrna miR-92a concentration in serum reflects human brown fat activity. Nat. Commun. 2016, 7, 11420. [Google Scholar] [CrossRef]
- Horne, J.A.; Ostberg, O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int. J. Chronobiol. 1976, 4, 97–110. [Google Scholar] [PubMed]
- Bracci, M.; Ciarapica, V.; Zabaleta, M.E.; Tartaglione, M.F.; Pirozzi, S.; Giuliani, L.; Piva, F.; Valentino, M.; Ledda, C.; Rapisarda, V.; et al. BRCA1 and BRCA2 gene expression: Diurnal variability and influence of shift work. Cancers 2019, 11, 1146. [Google Scholar] [CrossRef] [PubMed]
- Randler, C.; Engelke, J. Gender differences in chronotype diminish with age: A meta-analysis based on morningness/chronotype questionnaires. Chronobiol. Int. 2019, 36, 888–905. [Google Scholar] [CrossRef] [PubMed]
- Razavi, P.; Devore, E.E.; Bajaj, A.; Lockley, S.W.; Figueiro, M.G.; Ricchiuti, V.; Gauderman, W.J.; Hankinson, S.E.; Willett, W.C.; Schernhammer, E.S. Shift work, chronotype, and melatonin rhythm in nurses. Cancer Epidemiol.Biomark. Prev. 2019, 28, 1177–1186. [Google Scholar] [CrossRef] [PubMed]
- Taillard, J.; Philip, P.; Chastang, J.F.; Bioulac, B. Validation of Horne and Ostberg morningness-eveningness questionnaire in a middle-aged population of French workers. J. Biol. Rhythms 2004, 19, 76–86. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef]
- Vignatelli, L.; Plazzi, G.; Barbato, A.; Ferini-Strambi, L.; Manni, R.; Pompei, F.; D’Alessandro, R. Italian version of the Epworth sleepiness scale: External validity. Neurol. Sci 2003, 23, 295–300. [Google Scholar] [CrossRef]
- Durnin, J.V.; Womersley, J. Body fat assessed from total body density and its estimation from skinfold thickness: Measurements on 481 men and women aged from 16 to 72 years. Br. J. Nutr. 1974, 32, 77–97. [Google Scholar] [CrossRef]
- Salvini, S.; Gnagnarella, P.; Parpinel, M.T.; Boyle, P.; Decarli, A.; Ferraroni, M.; Giacosa, A.; La Vecchia, C.; Negri, E.; Franceschi, S. The food composition database for an italian food frequency questionnaire. J. Food Compos. Anal. 1996, 9, 57–71. [Google Scholar] [CrossRef]
- Manns, P.J.; Haennel, R.G. Sensewear armband and stroke: Validity of energy expenditure and step count measurement during walking. Stroke Res. Treat. 2012, 2012, 247165. [Google Scholar] [CrossRef]
- Tomasetti, M.; Staffolani, S.; Nocchi, L.; Neuzil, J.; Strafella, E.; Manzella, N.; Mariotti, L.; Bracci, M.; Valentino, M.; Amati, M.; et al. Clinical significance of circulating miR-126 quantification in malignant mesothelioma patients. Clin. Biochem. 2012, 45, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Schmittgen, T.D.; Livak, K.J. Analyzing real-time PCR data by the comparative C(T) method. Nat. Protoc. 2008, 3, 1101–1108. [Google Scholar] [CrossRef] [PubMed]
- Sourvinou, I.S.; Markou, A.; Lianidou, E.S. Quantification of circulating miRNAs in plasma: Effect of preanalytical and analytical parameters on their isolation and stability. J. Mol. Diagn. 2013, 15, 827–834. [Google Scholar] [CrossRef] [PubMed]
- Ledda, C.; Cina, D.; Matera, S.; Mucci, N.; Bracci, M.; Rapisarda, V. High HOMA-IR index in healthcare shift workers. Medicina 2019, 55, 186. [Google Scholar] [CrossRef] [PubMed]
- Strohmaier, S.; Devore, E.E.; Zhang, Y.; Schernhammer, E.S. A review of data of findings on night shift work and the development of DM and CVD events: A synthesis of the proposed molecular mechanisms. Curr. Diab. Rep. 2018, 18, 132. [Google Scholar] [CrossRef]
- Vetter, C.; Dashti, H.S.; Lane, J.M.; Anderson, S.G.; Schernhammer, E.S.; Rutter, M.K.; Saxena, R.; Scheer, F. Night shift work, genetic risk, and type 2 diabetes in the UK Biobank. Diabetes Care 2018, 41, 762–769. [Google Scholar] [CrossRef]
- Kolbe, I.; Oster, H. Chronodisruption, metabolic homeostasis, and the regulation of inflammation in adipose tissues. Yale J. Biol. Med. 2019, 92, 317–325. [Google Scholar] [PubMed]
- Copertaro, A.; Bracci, M.; Barbaresi, M.; Santarelli, L. Role of waist circumference in the diagnosis of metabolic syndrome and assessment of cardiovascular risk in shift workers. Med. Lav. 2008, 99, 444–453. [Google Scholar] [PubMed]
- Copertaro, A.; Bracci, M.; Barbaresi, M.; Santarelli, L. Assessment of cardiovascular risk in shift healthcare workers. Eur. J. Cardiovasc. Prev. Rehabil. 2008, 15, 224–229. [Google Scholar] [CrossRef]
- Peplonska, B.; Bukowska, A.; Sobala, W. Association of rotating night shift work with BMI and abdominal obesity among nurses and midwives. PLoS ONE 2015, 10, e0133761. [Google Scholar] [CrossRef]
- Thosar, S.S.; Butler, M.P.; Shea, S.A. Role of the circadian system in cardiovascular disease. J. Clin. Investig. 2018, 128, 2157–2167. [Google Scholar] [CrossRef] [PubMed]
- Torquati, L.; Mielke, G.I.; Brown, W.J.; Kolbe-Alexander, T. Shift work and the risk of cardiovascular disease. A systematic review and meta-analysis including dose-response relationship. Scand. J. Work Environ. Health 2018, 44, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Rosa, D.; Terzoni, S.; Dellafiore, F.; Destrebecq, A. Systematic review of shift work and nurses’ health. Occup. Med. 2019, 69, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Roomi, M.A.; Mohammadnezhad, M. Prevalence of metabolic syndrome among apparently healthy workforce. J. Ayub Med. Coll. Abbottabad 2019, 31, 252–254. [Google Scholar] [PubMed]
- Croce, N.; Bracci, M.; Ceccarelli, G.; Barbadoro, P.; Prospero, E.; Santarellia, L. Body mass index in shift workers: Relation to diet and physical activity. G. Ital. Med. Lav. Ergon. 2007, 29, 488–489. [Google Scholar] [PubMed]
- Proper, K.I.; van de Langenberg, D.; Rodenburg, W.; Vermeulen, R.C.H.; van der Beek, A.J.; van Steeg, H.; van Kerkhof, L.W.M. The relationship between shift work and metabolic risk factors: A systematic review of longitudinal studies. Am. J. Prev. Med. 2016, 50, e147–e157. [Google Scholar] [CrossRef] [PubMed]
- Barbadoro, P.; Santarelli, L.; Croce, N.; Bracci, M.; Vincitorio, D.; Prospero, E.; Minelli, A. Rotating shift-work as an independent risk factor for overweight italian workers: A cross-sectional study. PLoS ONE 2013, 8, e63289. [Google Scholar] [CrossRef]
- Hulsegge, G.; Gupta, N.; Holtermann, A.; Jorgensen, M.B.; Proper, K.I.; van der Beek, A.J. Shift workers have similar leisure-time physical activity levels as day workers but are more sedentary at work. Scand. J. Work Environ. Health 2017, 43, 127–135. [Google Scholar] [CrossRef]
- Loef, B.; Hulsegge, G.; Wendel-Vos, G.C.; Verschuren, W.M.; Vermeulen, R.C.; Bakker, M.F.; van der Beek, A.J.; Proper, K.I. Non-occupational physical activity levels of shift workers compared with non-shift workers. Occup. Environ. Med. 2017, 74, 328–335. [Google Scholar] [CrossRef]
- Kooijman, S.; van den Berg, R.; Ramkisoensing, A.; Boon, M.R.; Kuipers, E.N.; Loef, M.; Zonneveld, T.C.; Lucassen, E.A.; Sips, H.C.; Chatzispyrou, I.A.; et al. Prolonged daily light exposure increases body fat mass through attenuation of brown adipose tissue activity. Proc. Natl. Acad. Sci. USA 2015, 112, 6748–6753. [Google Scholar] [CrossRef]
- Ishii, N.; Iwata, T.; Dakeishi, M.; Murata, K. Effects of shift work on autonomic and neuromotor functions in female nurses. J. Occup. Health 2004, 46, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Bartness, T.J.; Vaughan, C.H.; Song, C.K. Sympathetic and sensory innervation of brown adipose tissue. Int. J. Obes. 2010, 34 (Suppl. S1), S36–S42. [Google Scholar] [CrossRef]
- Lee, P.; Bova, R.; Schofield, L.; Bryant, W.; Dieckmann, W.; Slattery, A.; Govendir, M.A.; Emmett, L.; Greenfield, J.R. Brown adipose tissue exhibits a glucose-responsive thermogenic biorhythm in humans. Cell Metab. 2016, 23, 602–609. [Google Scholar] [CrossRef]
- Onder, Y.; Green, C.B. Rhythms of metabolism in adipose tissue and mitochondria. Neurobiol. Sleep Circadian Rhythms 2018, 4, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Bracci, M.; Ciarapica, V.; Copertaro, A.; Barbaresi, M.; Manzella, N.; Tomasetti, M.; Gaetani, S.; Monaco, F.; Amati, M.; Valentino, M.; et al. Peripheral skin temperature and circadian biological clock in shift nurses after a day off. Int. J. Mol. Sci. 2016, 17, 623. [Google Scholar] [CrossRef] [PubMed]
- Giral, H.; Kratzer, A.; Landmesser, U. MicroRNAs in lipid metabolism and atherosclerosis. Best Pract. Res. Clin. Endocrinol. Metab. 2016, 30, 665–676. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Guan, X.; Sun, Y.; Mi, J.; Shu, X.; Liu, F.; Li, C. MiR-92a family and their target genes in tumorigenesis and metastasis. Exp. Cell Res. 2014, 323, 1–6. [Google Scholar] [CrossRef] [PubMed]
- MiRTargetLink Human. Available online: https://ccb-web.cs.uni-saarland.de/mirtargetlink/ (accessed on 26 December 2019).
- Chou, C.H.; Chang, N.W.; Shrestha, S.; Hsu, S.D.; Lin, Y.L.; Lee, W.H.; Yang, C.D.; Hong, H.C.; Wei, T.Y.; Tu, S.J.; et al. MiRTarBase 2016: Updates to the experimentally validated miRNA-target interactions database. Nucleic Acids Res. 2016, 44, D239–D247. [Google Scholar] [CrossRef] [PubMed]
- Hamberg, M.; Backes, C.; Fehlmann, T.; Hart, M.; Meder, B.; Meese, E.; Keller, A. MiRTargetLink--miRNAs, genes and interaction networks. Int. J. Mol. Sci. 2016, 17, 564. [Google Scholar] [CrossRef]
- Manni, I.; Artuso, S.; Careccia, S.; Rizzo, M.G.; Baserga, R.; Piaggio, G.; Sacchi, A. The microRNA miR-92 increases proliferation of myeloid cells and by targeting p63 modulates the abundance of its isoforms. FASEB J. 2009, 23, 3957–3966. [Google Scholar] [CrossRef]
- Wegrzyn, L.R.; Tamimi, R.M.; Rosner, B.A.; Brown, S.B.; Stevens, R.G.; Eliassen, A.H.; Laden, F.; Willett, W.C.; Hankinson, S.E.; Schernhammer, E.S. Rotating night-shift work and the risk of breast cancer in the nurses’ health studies. Am. J. Epidemiol. 2017, 186, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Ward, E.M.; Germolec, D.; Kogevinas, M.; McCormick, D.; Vermeulen, R.; Anisimov, V.N.; Aronson, K.J.; Bhatti, P.; Cocco, P.; Costa, G.; et al. Carcinogenicity of night shift work. Lancet Oncol. 2019, 20, 1058–1059. [Google Scholar] [CrossRef]
- Hansen, J. Night shift work and risk of breast cancer. Curr. Environ. Health Rep. 2017, 4, 325–339. [Google Scholar] [CrossRef] [PubMed]
- Lunn, R.M.; Blask, D.E.; Coogan, A.N.; Figueiro, M.G.; Gorman, M.R.; Hall, J.E.; Hansen, J.; Nelson, R.J.; Panda, S.; Smolensky, M.H.; et al. Health consequences of electric lighting practices in the modern world: A report on the national toxicology program’s workshop on shift work at night, artificial light at night, and circadian disruption. Sci. Total Environ. 2017, 607–608, 1073–1084. [Google Scholar] [CrossRef] [PubMed]
- Cun, J.; Yang, Q. Bioinformatics-based interaction analysis of miR-92a-3p and key genes in tamoxifen-resistant breast cancer cells. Biomed. Pharmacother. 2018, 107, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Danza, K.; De Summa, S.; Pinto, R.; Pilato, B.; Palumbo, O.; Carella, M.; Popescu, O.; Digennaro, M.; Lacalamita, R.; Tommasi, S. TGFbeta and miRNA regulation in familial and sporadic breast cancer. Oncotarget 2017, 8, 50715–50723. [Google Scholar] [CrossRef]
- Li, M.; Zhou, Y.; Xia, T.; Zhou, X.; Huang, Z.; Zhang, H.; Zhu, W.; Ding, Q.; Wang, S. Circulating microRNAs from the mir-106a-363 cluster on chromosome X as novel diagnostic biomarkers for breast cancer. Breast Cancer Res. Treat. 2018, 170, 257–270. [Google Scholar] [CrossRef]
- Nilsson, S.; Moller, C.; Jirstrom, K.; Lee, A.; Busch, S.; Lamb, R.; Landberg, G. Downregulation of miR-92a is associated with aggressive breast cancer features and increased tumour macrophage infiltration. PLoS ONE 2012, 7, e36051. [Google Scholar] [CrossRef]
- Ou, Z.; Wang, Y.; Chen, J.; Tao, L.; Zuo, L.; Sahasrabudhe, D.; Joseph, J.; Wang, L.; Yeh, S. Estrogen receptor beta promotes bladder cancer growth and invasion via alteration of miR-92a/DAB2IP signals. Exp. Mol. Med. 2018, 50, 152. [Google Scholar] [CrossRef]
- Pillai, M.M.; Gillen, A.E.; Yamamoto, T.M.; Kline, E.; Brown, J.; Flory, K.; Hesselberth, J.R.; Kabos, P. HITS-CLIP reveals key regulators of nuclear receptor signaling in breast cancer. Breast Cancer Res. Treat. 2014, 146, 85–97. [Google Scholar] [CrossRef]
- Si, H.; Sun, X.; Chen, Y.; Cao, Y.; Chen, S.; Wang, H.; Hu, C. Circulating microRNA-92a and microRNA-21 as novel minimally invasive biomarkers for primary breast cancer. J. Cancer Res. Clin. Oncol. 2013, 139, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Al-Nakhle, H.; Burns, P.A.; Cummings, M.; Hanby, A.M.; Hughes, T.A.; Satheesha, S.; Shaaban, A.M.; Smith, L.; Speirs, V. Estrogen receptor {beta}1 expression is regulated by miR-92 in breast cancer. Cancer Res. 2010, 70, 4778–4784. [Google Scholar] [CrossRef] [PubMed]
- Bracci, M.; Copertaro, A.; Manzella, N.; Staffolani, S.; Strafella, E.; Nocchi, L.; Barbaresi, M.; Copertaro, B.; Rapisarda, V.; Valentino, M.; et al. Influence of night-shift and napping at work on urinary melatonin, 17-beta-estradiol and clock gene expression in pre-menopausal nurses. J. Biol. Regul. Homeost. Agents 2013, 27, 267–274. [Google Scholar] [PubMed]
- Bracci, M.; Manzella, N.; Copertaro, A.; Staffolani, S.; Strafella, E.; Barbaresi, M.; Copertaro, B.; Rapisarda, V.; Valentino, M.; Santarelli, L. Rotating-shift nurses after a day off: Peripheral clock gene expression, urinary melatonin, and serum 17-beta-estradiol levels. Scand. J. Work Environ. Health 2014, 40, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Peplonska, B.; Bukowska, A.; Lie, J.A.; Gromadzinska, J.; Zienolddiny, S. Night shift work and other determinants of estradiol, testosterone, and dehydroepiandrosterone sulfate among middle-aged nurses and midwives. Scand. J. Work Environ. Health 2016, 42, 435–446. [Google Scholar] [CrossRef] [PubMed]
- Schernhammer, E.S.; Rosner, B.; Willett, W.C.; Laden, F.; Colditz, G.A.; Hankinson, S.E. Epidemiology of urinary melatonin in women and its relation to other hormones and night work. Cancer Epidemiol. Biomark. Prev. 2004, 13, 936–943. [Google Scholar] [PubMed]
| DT Nurses | SW Nurses | |
|---|---|---|
| Age (years): Median (25th–75th percentile) | 39.0 (37.0–41.5) | 39.0 (35.5–40.5) |
| Job seniority (years): Median (25th–75th percentile) | 14.0 (11.0–18.3) | 13.0 (10.5–16.5) |
| Shift work seniority (years): Median (25th–75th percentile) | - | 13.0 (10.5–16.5) |
| Night worked per month: Median (25th–75th percentile) | - | 6.0 (5.3–6.0) |
| Smokers (%) | 40.0 | 40.0 |
| Alcohol drinkers (%) | 33.3 | 40.0 |
| Subjects taking physical exercise (%) | 46.7 | 60.0 |
| Coffee consumption (cups/day): Median (25th–75th percentile) | 2.0 (1.0–3.0) | 2.0 (1.5–3.0) |
| Chronotype (MEQ score): Median (25th–75th percentile) | 57.5 (52.5–64.0) | 57.0 (51.3–62.0) |
| Sleep quality (PSQI score): Median (25th–75th percentile) | 6.0 (3.0–8.0) | 4.0 (2.5–6.5) |
| Daytime sleepiness (ESS score): Median (25th–75th percentile) | 4.0 (2.3–8.8) | 5.0 (4.0–9.3) |
| DT Nurses | SW Nurses | ||
|---|---|---|---|
| Fasting glycemia (mg/dL) | 89.5 (86.3–96.3) | 83.0 (78.3–91.0) | |
| Total cholesterol (mg/dL) | 206.5 (158.8–225.5) | 186.0 (159.5–196.3) | |
| HDL cholesterol (mg/mL) | 52.5 (40.8–61.5) | 49.0 (41.0–57.5) | |
| Triglicerides (mg/mL) | 70.0 (51.5–106.3) | 67.5 (55.5–114.5) | |
| Systolic pressure (mmHg) | 110.0 (105.0–120.0) | 110 (110–117.5) | |
| Diastolic pressure (mmHg) | 70.0 (60.0–80.0) | 70.0 (65.0–72.5) | |
| BMI (Kg/m2) | 23.6 (21.1–25.7) | 22.5 (21.2–29.7) | |
| Waist circumference (cm) | 90.0 (83.3–99.0) | 87.0 (81.0–103.0) | |
| Skin thickness | Biceps | 11.2 (6.7–11.8) | 11.2 (8.2–15.2) |
| Triceps | 21.2 (17.2–28.0) | 22.2 (20.0–28.8) | |
| Subscapular | 23.0 (17.5–27.8) | 18.8 (13.4–38.4) | |
| Suprailiac | 31.2 (22.4–33.7) | 24.0 (18.4–35.8) | |
| Body fat (%) | 37.5 (34.1–41.9) | 35.9 (32.1–40.1) | |
| DT Nurses | SW Nurses | ||
|---|---|---|---|
| Total Energy intake (Kcal) | 2004 (1712–2272) | 1927 (1850–2112) | |
| Diet composition | Carbohydrates (%) | 55.0 (53.2–55.5) | 55.0 (53.9–55.4) |
| Proteins (%) | 18.4 (17.8–19.4) | 19.0 (18.6–19.6) | |
| Fats (%) | 26.5 (26.1–27.8) | 26.1 (25.8–25.8) | |
| Total energy expenditure (Kcal) | 2179 (1866–2438) | 2225 (1962–2527) | |
| Energy expenditure due to locomotor activity (Kcal) | 874 (694–1484) | 1050 (923–1294) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bracci, M.; Eléxpuru Zabaleta, M.; Tartaglione, M.F.; Ledda, C.; Rapisarda, V.; Santarelli, L. Exosomal miR-92a Concentration in the Serum of Shift Workers. Appl. Sci. 2020, 10, 430. https://doi.org/10.3390/app10020430
Bracci M, Eléxpuru Zabaleta M, Tartaglione MF, Ledda C, Rapisarda V, Santarelli L. Exosomal miR-92a Concentration in the Serum of Shift Workers. Applied Sciences. 2020; 10(2):430. https://doi.org/10.3390/app10020430
Chicago/Turabian StyleBracci, Massimo, Maria Eléxpuru Zabaleta, Maria Fiorella Tartaglione, Caterina Ledda, Venerando Rapisarda, and Lory Santarelli. 2020. "Exosomal miR-92a Concentration in the Serum of Shift Workers" Applied Sciences 10, no. 2: 430. https://doi.org/10.3390/app10020430
APA StyleBracci, M., Eléxpuru Zabaleta, M., Tartaglione, M. F., Ledda, C., Rapisarda, V., & Santarelli, L. (2020). Exosomal miR-92a Concentration in the Serum of Shift Workers. Applied Sciences, 10(2), 430. https://doi.org/10.3390/app10020430