Evaluating the Utility of UV Lamps to Mitigate the Spread of Pathogens in the ICU
Abstract
Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Site and Design
2.2. UV Light Installation and UV Treatment Protocol
2.3. Mosaic Virus Transfer
2.4. Viral Swabs and Processing
2.5. Device Touch and Cycle Analysis
2.6. Statistical Analysis
3. Results
Mosaic Virus Transfer
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Center for Disease Control (CDC). Healthcare-Associated Infection (HAI). April 2012. Available online: www.cdc.gov/hai/ (accessed on 15 January 2020).
- Scott, R.D. The Direct Medical Costs of Healthcare-Associated Infections in U.S. Hospital and the Benefits of Prevention; National Center for Preparedness, Detection, and Control of Infectious Diseases: Atlanta, GR, USA, 2009. [Google Scholar]
- Graves, N.; Weinhold, D.; Tong, E.; Birrell, F.; Doidge, S.; Ramritu, P.; Halton, K.; Lairson, D.R.; Whitby, M. Effect of healthcare-acquired infection on length of hospital stay and cost. Infect. Control Hosp. Epidemiol. 2007, 28, 280–292. [Google Scholar] [CrossRef] [PubMed]
- Brun-Buisson, C.; Roudot-Thoraval, F.; Girou, E.; Grenier-Sennelier, C.; Durand-Zaleski, I. The costs of septic syndromes in the intensive care unit and influence of hospital-acquired sepsis. Intensive Care Med. 2003, 29, 1464–1471. [Google Scholar] [CrossRef] [PubMed]
- Zimlichman, E.; Henderson, D.; Tamir, O.; Franz, C.; Song, P.X.K.; Yamin, C.K.; Keohane, C.A.; Denham, C.R.; Bates, D.W. Health care-associated infections: A meta-analysis of costs and financial impact on the us health care system. JAMA Intern. Med. 2013, 173, 2039–2046. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health & Human Services Centers for Disease Control and Prevention. Vital Signs: Central Line-Associated Blood Stream Infections—United States, 2001, 2008, and 2009. MMWR 2011, 60, 243–248. [Google Scholar]
- Donskey, C.J. Beyond High-Touch Surfaces: Portable Equipment and Floors as Potential Sources of Transfer of Health Care–Associated Pathogens. Am. J. Infect. Control 2019, 47. [Google Scholar] [CrossRef]
- Mcdonald, L.C.; Gerding, D.N.; Johnson, S.; Bakken, J.S.; Carroll, K.C.; Coffin, S.E.; Dubberke, E.R.; Garey, K.W.; Gould, C.V.; Kelly, C.P.; et al. Clinical Practice Guidelines for Clostridium Difficile Infection in Adults and Children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin. Infect. Dis. 2018, 66, 987–994. [Google Scholar] [CrossRef]
- Messina, G.; Quercioli, C.; Burgassi, S.; Nisticò, F.; Lupoli, A.; Nante, N. How many bacteria live on the keyboard of your computer? Am. J. Infect. Control 2011, 39, 616–618. [Google Scholar] [CrossRef]
- Boyce, J.M.; Potter-Bynoe, G.; Chenevert, C.; King, T. Environmental contamination due to methicillin-resistant Staphylococcus aureus: Possible infection control implications. Infect. Control Hosp. Epid. 1997, 18, 622–627. [Google Scholar] [CrossRef]
- Ray, A.; Hoyen, C.; Taub, T.F.; Eckstein, E.C.; Donskey, C.J. Nosocomial transfer of vancomycin-resistant enterococci from surfaces. JAMA 2002, 287, 1400–1401. [Google Scholar] [CrossRef]
- Hayden, M.K.; Bonten, M.J.; Blom, D.; Lyle, E.A.; De Vijver, D.A.; Weinstein, R.A. Reduction in acquisition of vancomycin-resistant enterococcus after enforcement of routine environmental cleaning measures. Clin. Infect. Dis. 2006, 42, 1552–1560. [Google Scholar] [CrossRef]
- Rutala, W.A.; Gergen, M.F.; Weber, D.J. Room Decontamination with UV Radiation. Infect. Control Hosp. Epidemiol. 2010, 31, 1025–1029. [Google Scholar] [CrossRef] [PubMed]
- Levin, J.; Riley, L.S.; Parrish, C.; English, D.; Ahn, S. The effect of portable pulsed xenon ultraviolet light after terminal cleaning on hospital-associated clostridium difficile infection in a community hospital. Am. J. Infect. Control 2013, 41, 746–748. [Google Scholar] [CrossRef] [PubMed]
- Vermeulen, N.; Keeler, W.; Nandakumar, K.; Leung, K.T. The Bactericidal Effect of Ultraviolet and Visible Light on Escherichia Coli. Biotechnol. Bioeng. 2007, 99, 550–556. [Google Scholar] [CrossRef] [PubMed]
- Cutler, T.D.; Zimmerman, J.J. Ultraviolet irradiation and the mechanisms underlying its inactivation of infectious agents. Anim. Health Res. Rev. 2011, 12, 15–23. [Google Scholar] [CrossRef]
- Messina, G.; Fattorini, M.; Nante, N.; Rosadini, D.; Serafini, A.; Tani, M.; Cevenini, G. Time Effectiveness of Ultraviolet C Light (UVC) Emitted by Light Emitting Diodes (LEDs) in Reducing Stethoscope Contamination. Int. J. Environ. Res. Public Health 2016, 13, 940. [Google Scholar] [CrossRef]
- Gostine, A.; Gostine, D.; Donohue, C.; Carlstrom, L. Evaluating the effectiveness of ultraviolet-c lamps for reducing keyboard contamination in the intensive care unit: A longitudinal analysis. Am. J. Infect. Control 2016, 44, 1089–1094. [Google Scholar] [CrossRef][Green Version]
- Nerandzic, M.M.; Cadnum, J.L.; Pultz, M.J.; Donskey, C.J. Evaluation of an Automated Ultraviolet Radiation Device for Decontamination of Clostridium Difficile and Other Healthcare-Associated Pathogens in Hospital Rooms. BMC Infect. Dis. 2010, 10. [Google Scholar] [CrossRef]
- Jiang, X.; Dai, X.; Goldblatt, S.; Buescher, C.; Cusack, T.M.; Matson, D.O.; Pickering, L.K. Pathogen Transmission in Child Care Settings Studied by Using a Cauliflower Virus DNA as a Surrogate Marker. J. Infect. Dis. 1998, 177, 881–888. [Google Scholar] [CrossRef]
- Decker, B.K.; Palmore, T.N. The Role of Water in Healthcare-Associated Infections. Curr. Opin. Infect. Dis. 2013, 26, 345–351. [Google Scholar] [CrossRef]
- Mehta, Y.; Gupta, A.; Todi, S.; Myatra, S.; Samaddar, D.P.; Patil, V.; Bhattacharya, P.; Ramasubban, S. Guidelines for prevention of hospital acquired infections. Indian J. Crit. Care Med. 2014, 18, 149–163. [Google Scholar] [CrossRef]
- Otter, J.A.; Havill, N.L.; Adams, N.M.T.; Boyce, J.M. Extensive environmental contamination associated with patients with loose stools and methicillin-resistant Staphylococcus aureus colonization of the gastrointestinal tract. In Proceedings of the 16th Annual Scientific Meeting of the Society for Healthcare Epidemiology of America, Chicago, IL, USA, 18–21 March 2006. [Google Scholar]
- Weber, D.J.; Rutala, W.A.; Miller, M.B.; Huslage, K.; Sickbert-Bennett, E. Role of hospital surfaces in the transfer of emerging health care-associated pathogens: Norovirus, Clostridium difficile, and Acinetobacter species. Am. J. Infect. Control 2010, 38, S25–S33. [Google Scholar] [CrossRef] [PubMed]
- Carling, P.C.; Parry, M.F.; von Beheren, S.M. Identifying opportunities to enhance environmental cleaning in 23 acute care hospitals. Infect. Control Hosp. Epidemiol. 2008, 29, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kramer, A.; Schwebke, I.; Kampf, G. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect. Dis. 2006, 6, 130. [Google Scholar] [CrossRef]
- Smith, S.J.; Young, V.; Robertson, C.; Dancer, S.J. Cross-transfer audit of environmental surfaces, clinical equipment and patient: Who touches what? J. Hosp. Infect. 2012, 80, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Dancer, S.J. The role of environmental cleaning in the control of hospital-acquired infection. J. Hosp. Infect. 2009, 73, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Bhalla, A.; Pultz, N.J.; Gries, D.M.; Ray, A.J.; Eckstein, E.C.; Aron, D.C.; Donskey, C.J. Acquisition of nosocomial pathogens on hands after contact with environmental surfaces near hospitalized patients. Infect. Control Hosp. Epidemiol. 2004, 25, 164–167. [Google Scholar] [CrossRef]
- Dancer, S.J.; White, L.F.; Lamb, J.; Girvan, E.K.; Robertson, C. Measuring the effect of enhanced cleaning in a UK hospital: A prospective cross-over study. BMC Med. 2009, 7, 28. [Google Scholar] [CrossRef]
- Larson, E.; Early, E.; Cloonan, P.; Sugrue, S.; Parides, M.K. An organizational climate intervention associated with increased handwashing and decreased nosocomial infections. Behav. Med. 2000, 26, 14–22. [Google Scholar] [CrossRef]
- Haas, J.P.; Menz, J.; Dusza, S.; Montecalvo, M.A. Implementation and Impact of Ultraviolet Environmental Disinfection in an Acute Care Setting. Am. J. Infect. Control 2014, 42, 586–590. [Google Scholar] [CrossRef]
- Cornell, P.; Herringriffith, D.; Keim, C.; Petschonek, S.; Sanders, A.M.; Dmello, S.K.; Golden, T.W.; Shepherd, G. Transforming nursing workflow, part 1: The chaotic nature of nurse activities. J. Nurs. Adm. 2010, 40, 366–373. [Google Scholar] [CrossRef]
| Device | Average 24-h Touches |
|---|---|
| IV Pump | 48.8 |
| Keyboard | 111.2 |
| Pyxis | 50.5 |
| Ventilator | 28.5 |
| Vitals Monitor | 29.5 |
| Worksurface on Cart | 112.7 |
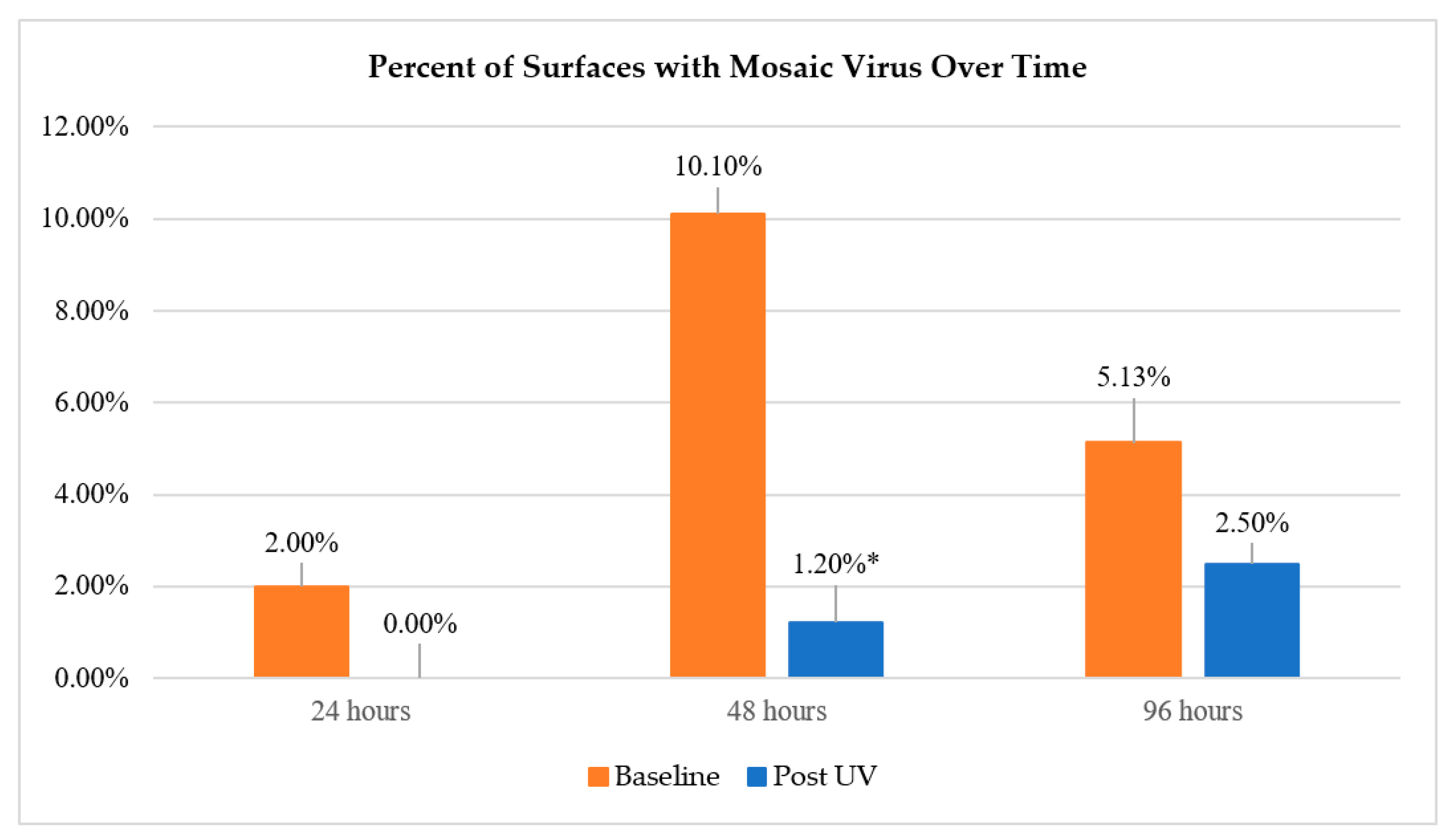
| Hours Post Inoculation | 24 | 48 | 96 |
| Pre-UV Surfaces Positive (Percent) | 2.00% | 10.10% | 5.13% |
| Pre-UV Surfaces Positive (Number) | N = 2 | N = 10 | N = 4 |
| Post-UV Surfaces Positive (Percent) | 0% | 1.20% | 2.50% |
| Post-UV Surfaces Positive (Number) | N = 0 | N = 1 | N = 2 |
| Significance | p = 0.125 | p < 0.0001 | p = 0.688 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gostine, A.; Gostine, D.; Short, J.; Rustagi, A.; Cadnum, J.; Donskey, C.; Angelotti, T. Evaluating the Utility of UV Lamps to Mitigate the Spread of Pathogens in the ICU. Appl. Sci. 2020, 10, 6326. https://doi.org/10.3390/app10186326
Gostine A, Gostine D, Short J, Rustagi A, Cadnum J, Donskey C, Angelotti T. Evaluating the Utility of UV Lamps to Mitigate the Spread of Pathogens in the ICU. Applied Sciences. 2020; 10(18):6326. https://doi.org/10.3390/app10186326
Chicago/Turabian StyleGostine, Andrew, David Gostine, Jack Short, Arjun Rustagi, Jennifer Cadnum, Curtis Donskey, and Tim Angelotti. 2020. "Evaluating the Utility of UV Lamps to Mitigate the Spread of Pathogens in the ICU" Applied Sciences 10, no. 18: 6326. https://doi.org/10.3390/app10186326
APA StyleGostine, A., Gostine, D., Short, J., Rustagi, A., Cadnum, J., Donskey, C., & Angelotti, T. (2020). Evaluating the Utility of UV Lamps to Mitigate the Spread of Pathogens in the ICU. Applied Sciences, 10(18), 6326. https://doi.org/10.3390/app10186326





