Concurrent Validity of Digital Measures of Psychological Dimensions Associated with Suicidality Using AuxiliApp
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Sample Size and Power Analysis
2.3. Ethical Considerations
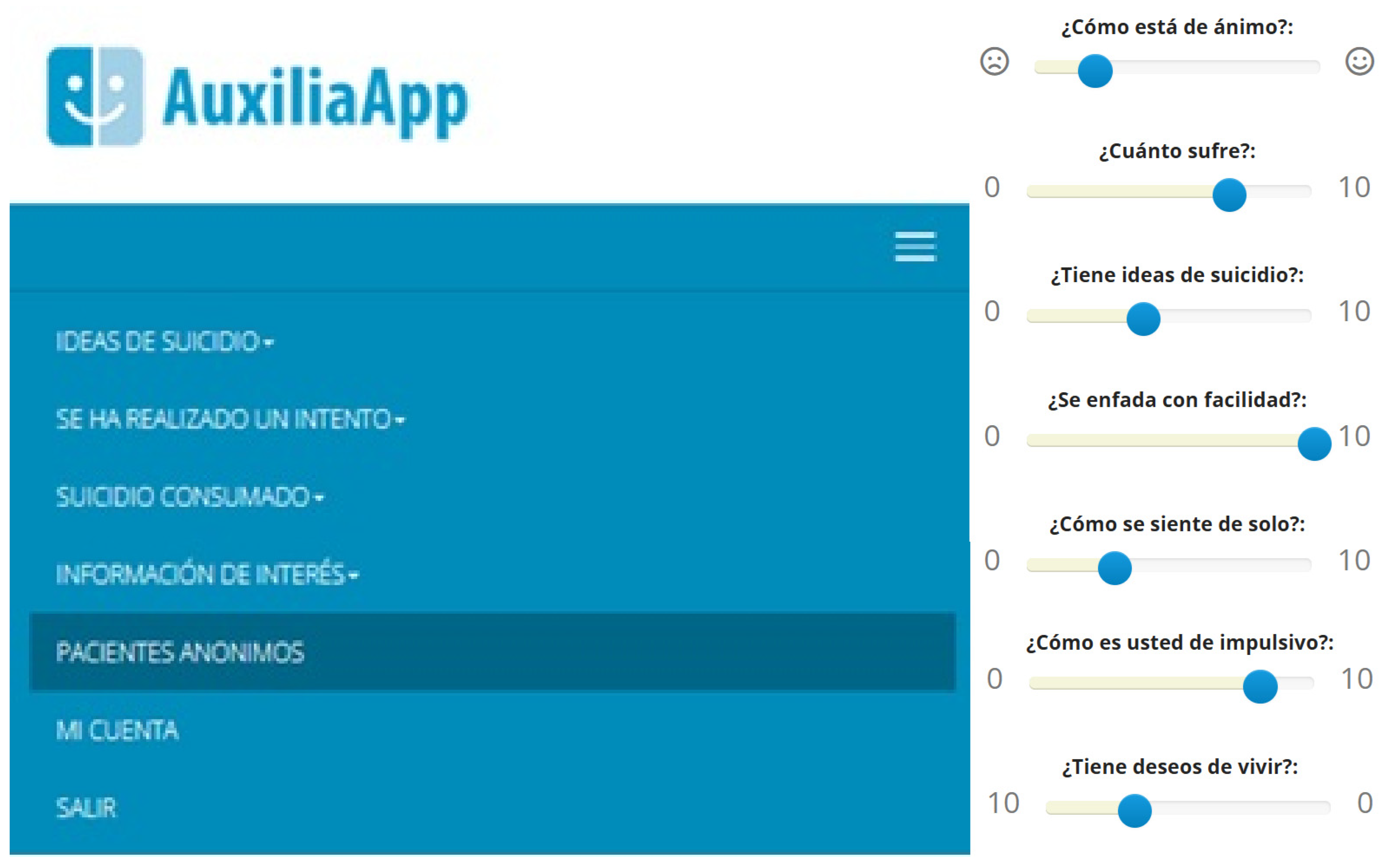
2.4. Procedure
2.5. Instruments
- Beck Depression Inventory-II (BDI-II): Assesses the severity of depressive symptoms (A. T. Beck et al., 1960; Spanish adaptation by Sanz et al., 2003, which reported an excellent internal consistency of α = 0.89 in the general population). The scale consists of 21 items rated on a 4-point scale from 0 to 3, covering emotional, cognitive, and somatic aspects of depression, such as hopelessness, guilt, and physical discomfort.
- Psychache Scale: Measures psychological pain using 13 items rated on a 5-point Likert scale (Holden et al., 2001; Spanish adaptation by Ordóñez-Carrasco et al., 2022, which reported an excellent internal consistency of α = 0.90). Higher scores indicate greater levels of psychological distress.
- Paykel Suicide Scale (PSS): Assesses the severity and frequency of suicidal ideation. For this study, we utilized a Spanish adaptation for adolescents (Fonseca-Pedrero et al., 2018; see also Baños-Chaparro & Ramos-Vera, 2020, who reported an excellent internal consistency of α = 0.94 in a Peruvian adolescent sample).
- State-Trait Anger Expression Inventory-2 (STAXI-2): Evaluates the experience, expression, and control of anger (Spielberger et al., 1983; Spanish adaptation by Miguel-Tobal et al., 2001). The scale comprises several subscales, including State Anger, Trait Anger, Anger Expression-Out, Anger Expression-In, Anger Control-Out, and Anger Control-In. Psychometric studies of its Spanish version have demonstrated good internal consistency, with Cronbach’s alpha values ranging from 0.70 to 0.90 for its various subscales (e.g., García-Batista et al., 2018).
- UCLA Loneliness Scale: Designed to assess perceived loneliness and social isolation. It contains 20 items rated on a 4-point scale, with higher scores indicating more frequent experiences of loneliness (Russell, 1996; Spanish adaptation by Vázquez Morejón & Jiménez García-Bóveda, 1994; see also Velarde-Mayol et al., 2016) has shown high reliability, with an excellent internal consistency of α = 0.90.
- Barratt Impulsiveness Scale (BIS): A widely used self-report measure of impulsivity (Patton et al., 1995). For this study, the Spanish adaptation for adolescents (Martínez-Loredo et al., 2015) was utilized, which has demonstrated good psychometric properties, including excellent internal consistency for the total scale (α = 0.89) and good consistency for its subscales (Attentional Impulsivity: α = 0.70; Non-planning Impulsivity: α = 0.81; Motor Impulsivity: α = 0.79).
- Reasons for Living Inventory (RFL): Measures an individual’s perceived reasons for not committing suicide (Linehan et al., 1983). The Spanish adaptation (Oquendo et al., 2000) has shown excellent internal consistency, with a Cronbach’s alpha of α = 0.94 for the total scale, and values ranging from 0.70 to 0.89 for its various subscales (Survival and Coping Beliefs, Responsibility to Family, Child Concerns, Fear of Suicide, Fear of Social Disapproval, and Moral/Religious Objections).
2.6. Statistical Analysis
3. Results
4. Discussion
Future Directions
5. Conclusions
6. Strengths and Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BDI-II | Beck Depression Inventory-II |
| BIS | Barratt Impulsiveness Scale |
| CC BY | Creative Commons Attribution license |
| COVID-19 | Coronavirus Disease 2019 |
| GHQ-12 | General Health Questionnaire-12 |
| IDS-C | Inventory of Depressive Symptomatology—Clinician-rated |
| INE | Instituto Nacional de Estadística |
| mHealth | Mobile Health (salud móvil) |
| NT | New technologies |
| PANSS | Positive and Negative Syndrome Scale |
| PHQ-9 | Patient Health Questionnaire-9 |
| QISD-SR 16 | Questionnaire for Impulsive and Self-Destructive Behaviors—Self-Report, 16 items |
| RFL | Reasons for Living Inventory |
| SPSS | Statistical Package for the Social Sciences |
| STAXI-2 | State-Trait Anger Expression Inventory-2 |
| UCLA | University of California, Los Angeles (en “UCLA Loneliness Scale”) |
| VAS | Visual Analog Scale |
| VI-PPITUS | VI Plan Propio de Investigación y Transferencia de la Universidad de Sevilla |
| WHO | World Health Organization |
References
- Alasaarela, L., Hakko, H., Riala, K., & Riipinen, P. (2017). Association of self-reported impulsivity to nonsuicidal self-injury, suicidality, and mortality in adolescent psychiatric inpatients. Journal of Nervous and Mental Disease, 205(5), 340–345. [Google Scholar] [CrossRef]
- Alemu, Y., Chen, H., Duan, C., Caulley, D., Arriaga, R. I., & Sezgin, E. (2023). Detecting Clinically Relevant Emotional Distress and Functional Impairment in Children and Adolescents: Protocol for an Automated Speech Analysis Algorithm Development Study. JMIR Research Protocols, 12, e46970. [Google Scholar] [CrossRef] [PubMed]
- Alfonsson, S., Maathz, P., & Hursti, T. (2014). Interformat reliability of digital psychiatric self-report questionnaires: A systematic review. Journal of Medical Internet Research, 16(12), e268. [Google Scholar] [CrossRef] [PubMed]
- Areán, P., Pratap, A., Hsin, H., Huppert, T. K., E Hendricks, K., Heagerty, P. J., Cohen, T., Bagge, C., & Comtois, K. A. (2021). Perceived utility and characterization of personal google search histories to detect data patterns proximal to a suicide attempt in individuals who previously attempted suicide: Pilot cohort study. Journal of Medical Internet Research, 23(5), e27918. [Google Scholar] [CrossRef] [PubMed]
- Arsenault-Lapierre, G., Kim, C. D., & Turecki, G. (2004). Psychiatric diagnoses in 3275 suicides: A meta-analysis. BMC Psychiatry, 4, 37. [Google Scholar] [CrossRef]
- Auerbach, R. P., Stewart, J. G., & Johnson, S. L. (2017). Impulsivity and suicidality in adolescents inpatients. Journal of Abnormal Child Psychology, 45(1), 91–103. [Google Scholar] [CrossRef]
- Baños-Chaparro, J., & Ramos-Vera, C. (2020). Validez e invarianza según sexo y edad de la Escala Paykel de Ideación Suicida en adolescentes peruanos. Interacciones, 6(1), e225. [Google Scholar] [CrossRef]
- Barrigón, M. L., Rico-Romano, A. M., Ruiz-Gomez, M., Delgado-Gomez, D., Barahona, I., Aroca, F., & Baca-García, E. (2017). Estudio comparativo de los formatos en lápiz y papel y electrónicos de los cuestionarios GHQ-12, WHO-5 y PHQ-9. Revista de Psiquiatría y Salud Mental, 10(3), 160–167. [Google Scholar] [CrossRef]
- Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., & Erbaugh, J. (1960). An inventory for measuring depression. Archives of General Psychiatry, 4(6), 561–571. [Google Scholar] [CrossRef]
- Beck, T., Brown, G., Berchick, J., Stewart, L., Steer, A., Ed, D., & Ph, D. (1990). Relationship between hopelessness and ultimate suicide: A replication with psychiatric outpatients. American Journal of Psychiatry, 147, 190–195. [Google Scholar] [CrossRef]
- Bobes, J., González, M. P., Saiz, P. A., & Bousoño, M. (1996). Índice europeo de severidad de la adicción: EuropASI. Versión española. Actas de la IV Reunión Interregional de Psiquiatría, 1996, 201–218. [Google Scholar]
- Bobes García, J., Badia Llach, X., Luque, A., García, M., González Rodríguez, M. P., Dal-Ré Saavedra, R., & Grupo de Validación en Español de Cuestionarios de Evaluación de la Fobia Social. (1999). Validación de las versiones en español de los cuestionarios liebowitz social anxiety scale, social anxiety and distress scale y sheehan disability inventory para la evaluación de la fobia social. Medicina Clínica, 112(14), 530–538. [Google Scholar]
- Caro-Cañizares, I., Brenlla, M., Carballo, J., Santos, M., Guija, J., & Giner, L. (2024). Suicidal behaviour and stressful life events: The Mediating role of the impulsivity-aggression-hostility triad through psychological autopsy. Psicothema, 36(4), 380–388. [Google Scholar] [CrossRef]
- Chamorro, J., Bernardi, S., Potenza, M. N., Grant, J. E., Marsh, R., Wang, S., & Blanco, C. (2012). Impulsivity in the general population: A national study. Journal of Psychiatric Research, 46(8), 994–1001. [Google Scholar] [CrossRef]
- Chen, J. I., Osman, A., Freedenthal, S. L., & Gutierrez, P. M. (2020). An examination of the psychometric properties of the reasons for living inventory within a male veteran clinical sample. Archives of Suicide Research, 24(Suppl. S1), 204–230. [Google Scholar] [CrossRef]
- Cohen, J., Cohen, P., West, S. G., & Aiken, L. S. (2003). Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed.). Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Cole, A. B., Littlefield, A. K., Gauthier, J. M., & Bagge, C. L. (2019). Impulsivity facets and perceived likelihood of future suicide attempt among patients who recently attempted suicide. Journal of Affective Disorders, 257, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Costanza, A., Rothen, S., Achab, S., Thorens, G., Baertschi, M., Weber, K., Canuto, A., Richard-Lepouriel, H., Perroud, N., & Zullino, D. (2020). Impulsivity and impulsivity-related endophenotypes in suicidal patients with substance use disorders: An exploratory study. International Journal of Mental Health and Addiction, 19, 1729–1744. [Google Scholar] [CrossRef]
- Critchfield, K. L., Levy, K. N., & Clarkin, J. F. (2004). The relationship between impulsivity, aggression, and impulsive-aggression in borderline personality disorder: An empirical analysis of self-report measures. Journal of Personality Disorders, 18(6), 555–570. [Google Scholar] [CrossRef]
- Dalca, I. M., McGirr, A., Renaud, J., & Turecki, G. (2013). Gender-specific suicide risk factors: A case-control study of individuals with major depressive disorder. Journal of Clinical Psychiatry, 74(12), 1209–1215. [Google Scholar] [CrossRef]
- Daniel, S. S., Goldston, D. B., Erkanli, A., Franklin, J. C., & Mayfield, A. M. (2009). Trait anger, anger expression, and suicide attempts among adolescents and young adults: A prospective study. Journal of Clinical Child and Adolescent Psychology, 38(5), 661–671. [Google Scholar] [CrossRef]
- Dillon, K. H., Van Voorhees, E. E., Dennis, P. A., Glenn, J. J., Wilks, C. R., Morland, L. A., Beckham, J. C., & Elbogen, E. B. (2020). Anger mediates the relationship between posttraumatic stress disorder and suicidal ideation in veterans. Journal of Affective Disorders, 269, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Dubé, J. P., Smith, M. M., Sherry, S. B., Hewitt, P. L., & Stewart, S. H. (2021). Suicide behaviors during the COVID-19 pandemic: A meta-analysis of 54 studies. Psychiatry Research, 301, 113998. [Google Scholar] [CrossRef] [PubMed]
- Ernst, M., Klein, E. M., Beutel, M. E., & Brähler, E. (2021). Gender-specific associations of loneliness and suicidal ideation in a representative population sample: Young, lonely men are particularly at risk. Journal of Affective Disorders, 294, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Esposito, C., Spirito, A., Boergers, J., & Donaldson, D. (2003). Affective, behavioral, and cognitive functioning in adolescents with multiple suicide attempts. Suicide and Life-Threatening Behavior, 33(4), 389–399. [Google Scholar] [CrossRef]
- Evren, C., Cinar, O., Evren, B., & Celik, S. (2011). History of suicide attempt in male substance-dependent inpatients and relationship to borderline personality features, anger, hostility and aggression. Psychiatry Research, 190(1), 126–131. [Google Scholar] [CrossRef]
- Faurholt-Jepsen, M., Munkholm, K., Frost, M., Bardram, J. E., & Kessing, L. V. (2016). Electronic self-monitoring of mood using IT platforms in adult patients with bipolar disorder: A systematic review of the validity and evidence. BMC Psychiatry, 16(1), 7. [Google Scholar] [CrossRef]
- Ferrando, L., Bobes, J., Gibert, M., Soto, M., & Soto, O. (1998). M.I.N.I. mini international neuropsychiatric interview. Versión en español 5.0.0.DSM-IV. Instituto IAP. [Google Scholar]
- Fonseca-Pedrero, E., Inchausti, F., Pérez-Gutiérrez, L., Aritio Solana, R., Ortuño-Sierra, J., Sánchez-García, M. A., Lucas-Molina, B., Domínguez, C., Foncea, D., Espinosa, V., Gorría, A., Urbiola-Merina, E., Fernández, M., Merina Díaz, C., Gutiérrez, C., Aures, M., Campos, M. S., & Pérez de Albéniz Iturriaga, A. (2018). Ideación suicida en una muestra representativa de adolescentes españoles. Revista de Psiquiatría y Salud Mental, 11(2), 76–85. [Google Scholar] [CrossRef]
- García-Batista, Z. E., Guerra-Peña, K., Cano-Vindel, A., Herrera-Martínez, S. X., Flores-Kanter, P. E., & Medrano, L. A. (2018). Evidencias de validez y fiabilidad de las Puntuaciones del STAXI-2 para población general y hospitalaria: Estudio con una muestra de adultos de República Dominicana. Suma Psicológica, 25(1), 21–29. [Google Scholar] [CrossRef]
- Giegling, I., Olgiati, P., Hartmann, A., Calati, R., Möller, H., Rujescu, D., & Serretti, A. (2009). Personality and attempted suicide. Analysis of anger, aggression and impulsivity. Journal of Psychiatric Research, 43(16), 1262–1271. [Google Scholar] [CrossRef]
- Green, K. L., Brown, G. K., Jager-Hyman, S., Cha, J., Steer, R. A., & Beck, A. T. (2015). The predictive validity of the beck depression inventory suicide item. The Journal of Clinical Psychiatry, 76(12), 1683–1686. [Google Scholar] [CrossRef]
- Grupo Español de Trabajo para la Evaluación por Estrés Postraumático. (2000). Evaluación de las propiedades psicométricas de la versión española de cinco cuestionarios para la evaluación del trastorno de estrés postraumático. Actas Españolas de Psiquiatría, 28(4), 207–218. [Google Scholar]
- Guilford, J. P. (1956). Fundamental statistics in psychology and education (3rd ed.). McGraw-Hill. [Google Scholar]
- Gwaltney, C. J., Shields, A. L., & Shiffman, S. (2008). Equivalence of electronic and paper-and-pencil administration of patient-reported outcome measures: A meta-analytic review. Value in Health, 11(2), 322–333. [Google Scholar] [CrossRef]
- Hamza, C. A., & Willoughby, T. (2019). Impulsivity and nonsuicidal self-injury: A longitudinal examination among emerging adults. Journal of Adolescence, 75, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Hamza, C. A., Willoughby, T., & Heffer, T. (2015). Impulsivity and nonsuicidal self-injury: A review and meta-analysis. Clinical Psychology Review, 38, 13–24. [Google Scholar] [CrossRef]
- Harriss, L., & Hawton, K. (2005). Suicidal intent in deliberate self-harm and the risk of suicide: The predictive power of the suicide intent scale. Journal of Affective Disorders, 86(2–3), 225–233. [Google Scholar] [CrossRef]
- Hawkins, K. A., Hames, J. L., Ribeiro, J. D., Silva, C., Joiner, T. E., & Cougle, J. R. (2014). An examination of the relationship between anger and suicide risk through the lens of the interpersonal theory of suicide. Journal of Psychiatric Research, 50(1), 59–65. [Google Scholar] [CrossRef] [PubMed]
- Heidari, P., Broadbear, J. H., Brown, R., Dharwadkar, N. P., & Rao, S. (2023). Mental health support for and telehealth use by Australians living with borderline personality disorder during the onset of the COVID-19 pandemic: A national study. Digital Health, 9, 20552076231169824. [Google Scholar] [CrossRef]
- Herpertz, S., Steinmeyer, S. M., Marx, D., Oidtmann, A., & Sass, H. (1995). The significance of aggression and impulsivitiy for self-mutilative behavior. Pharmacopsychiatry, 28(Suppl. S2), 64–72. [Google Scholar] [CrossRef]
- Hilty, D. M., Armstrong, C. M., A Smout, S., Crawford, A., Maheu, M. M., Drude, K. P., Chan, S., Yellowlees, P. M., & Krupinski, E. A. (2022). Findings and guidelines on provider technology, fatigue, and well-being: Scoping review. Journal of Medical Internet Research, 24(5), e34451. [Google Scholar] [CrossRef]
- Holden, R. R., Mehta, K., Cunningham, E. J., & McLeod, L. D. (2001). Development and preliminary validation of a scale of psychache. Canadian Journal of Behavioural Science, 33(4), 224–232. [Google Scholar] [CrossRef]
- Horesh, N., Rolnick, T., Iancu, I., Dannon, P., Lepkifker, E., Apter, A., & Kotler, M. (1997). Anger, impulsivity and suicide risk. Psychotherapy and Psychosomatics, 66(2), 92–96. [Google Scholar] [CrossRef] [PubMed]
- John, A., Eyles, E., Webb, R. T., Okolie, C., Schmidt, L., Arensman, E., Hawton, K., O’Connor, R. C., Kapur, N., Moran, P., O’Neill, S., McGuinness, L. A., Olorisade, B. K., Dekel, D., Macleod-Hall, C., Cheng, H. Y., Higgins, J. P. T., & Gunnell, D. (2021). The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: Update of living systematic review. F1000Research, 9, 1–44. [Google Scholar] [CrossRef] [PubMed]
- Killgore, W. D., Cloonan, S. A., Taylor, E. C., Miller, M. A., & Dailey, N. S. (2020). Three months of loneliness during the COVID-19 lockdown. Psychiatry Research, 293, 1–2. [Google Scholar] [CrossRef]
- Kotler, M., Iancu, I., Efroni, R., & Amir, M. (2001). Anger, impulsivity, social support, and suicide risk in patients with posttraumatic stress disorder. The Journal of Nervous and Mental Disease, 189(3), 162–167. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y., Gilbert, J., Waldman, L., Zarate, C., & Ballard, E. (2024). Potential association between suicide risk, aggression, impulsivity, and the somatosensory system. Social Cognitive and Affective Neuroscience, 19(1), 7. [Google Scholar] [CrossRef]
- Lin, L., & Zhang, J. (2017). Impulsivity, mental disorder, and suicide in rural China. Archives of Suicide Research, 21(1), 73–82. [Google Scholar] [CrossRef]
- Lindsay, J. A. B., McGowan, N. M., Henning, T., Harriss, E., & Saunders, K. E. A. (2024). Digital interventions for symptoms of borderline personality disorder: Systematic review and meta-analysis. Journal of Medical Internet Research, 26, e54941. [Google Scholar] [CrossRef]
- Linehan, M. M., Goodstein, J. L., Nielsen, S. L., & Chiles, J. A. (1983). Reasons for staying alive when you are thinking of killing yourself: The brief reasons for living inventory. Journal of Consulting and Clinical Psychology, 51(2), 276–286. [Google Scholar] [CrossRef]
- Liu, R., Trout, Z., Hernandez, E., Cheek, S., & Gerlus, N. (2017). A behavioral and cognitive neuroscience perspective on impulsivity, suicide, and non-suicidal self-injury: Meta-analysis and recommendations for future research. Neuroscience & Biobehavioral Reviews, 83, 440–450. [Google Scholar]
- Maino, M. d. l. P., Morales, S., Echávarri, O., Barros, J., García, A., Moya, C., Szmulewicz, T., Fischman, R., Núñez, C., & Tomicic, A. (2019). Suicide risk configuration system in a clustered clinical sample: A generalized linear model obtained through the LASSO technique. Revista Brasileira de Psiquiatria, 41(2), 112–121. [Google Scholar] [CrossRef]
- Marciano, L., & Saboor, S. (2023). Reinventing mental health care in youth through mobile approaches: Current status and future steps. Frontiers in Psychology, 14, 1126015. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Loredo, V., Fernández-Hermida, J. R., Fernández-Artamendi, S., Carballo, J. L., & García-Rodríguez, O. (2015). Spanish adaptation and validation of the Barratt Impulsiveness Scale for early adolescents (BIS-11-A). International Journal of Clinical and Health Psychology, 15(3), 274–282. [Google Scholar] [CrossRef]
- Melia, R., Francis, K., Hickey, E., Bogue, J., Duggan, J., O’Sullivan, M., & Young, K. (2020). Mobile health technology interventions for suicide prevention: Systematic review. JMIR MHealth and UHealth, 8(1), e12516. [Google Scholar] [CrossRef] [PubMed]
- Mercer, D., Douglass, A. B., & Links, P. S. (2009). Meta-analyses of mood stabilizers, antidepressants and antipsychotics in the treatment of borderline personality disorder: Effectiveness for depression and anger symptoms. Journal of Personality Disorders, 23(2), 156–174. [Google Scholar] [CrossRef]
- Miguel-Tobal, J., Cano-Vindel, A., Casado-Morales, M., & Spielberger, C. (2001). Inventario de expresión de la Ira estado-rasgo, S.T.A.X.I.-2./state-trait anger expression inventory. STAXI-2. TEA Ediciones. [Google Scholar]
- Moore, F., Allott, C., & O’Connor, R. (2023). Impulsivity, aggression, and impulsive aggression in suicidality. Personality and Individual Differences, 202, 111971. [Google Scholar] [CrossRef]
- Moynihan, R., Sanders, S., Michaleff, Z. A., Scott, A. M., Clark, J., To, E. J., Jones, M., Kitchener, E., Fox, M., Johansson, M., Lang, E., Duggan, A., Scott, I., & Albarqouni, L. (2021). Impact of COVID-19 pandemic on utilisation of healthcare services: A systematic review. BMJ Open, 11(3), e045343. [Google Scholar] [CrossRef] [PubMed]
- Neelam, K., Duddu, V., Anyim, N., Neelam, J., & Lewis, S. (2021). Pandemics and pre-existing mental illness: A systematic review and meta-analysis. Brain, Behavior, and Immunity—Health, 10, 100177. [Google Scholar] [CrossRef]
- Nock, M. K., Green, J. G., Hwang, I., McLaughlin, K. A., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C. (2013). Prevalence, correlates and treatments of lifetime suicidal behavior among adolescents: Results from the national comorbidity survey replication—Adolescente supplement (NCS-A). JAMA Psychiatry, 70(3), 300–310. [Google Scholar] [CrossRef]
- Olié, E., Dubois, J., Benramdane, M., Guillaume, S., & Courtet, P. (2021). Psychological state of a sample of patients with mood disorders during the first French COVID-19 lockdown. Scientific Reports, 11(1), 23711. [Google Scholar] [CrossRef]
- Oquendo, M. A., Cia, E., Graver, R., Mora, M., Montalvan, V., & Mann, J. (2000). Spanish adaptation of the reasons for living inventory. Hispanic Journal of Behavioral Sciences, 22(3), 369–381. [Google Scholar] [CrossRef]
- Ordóñez-Carrasco, J. L., Cuadrado Guirado, I., & Rojas Tejada, A. (2022). Escala de dolor psicológico: Adaptación de la Psychache Scale al español en jóvenes adultos. Revista de Psiquiatría y Salud Mental, 15(3), 196–204. [Google Scholar] [CrossRef]
- Ornell, F., Borelli, W. V., Benzano, D., Schuch, J. B., Moura, H. F., Sordi, A. O., Kessler, F. H. P., Scherer, J. N., & von Diemen, L. (2021). The next pandemic: Impact of COVID-19 in mental healthcare assistance in a nationwide epidemiological study. The Lancet Regional Health—Americas, 4, 100061. [Google Scholar] [CrossRef] [PubMed]
- Painuly, N., Sharan, P., & Mattoo, S. K. (2007). Antecedents, concomitants and consequences of anger attacks in depression. Psychiatry Research, 153(1), 39–45. [Google Scholar] [CrossRef]
- Palmier-Claus, J. E., Ainsworth, J., Machin, M., Barrowclough, C., Dunn, G., Barkus, E., Rogers, A., Wykes, T., Kapur, S., Buchan, I., Salter, E., & Lewis, S. W. (2012). The feasibility and validity of ambulatory self-report of psychotic symptoms using a smartphone software application. BMC Psychiatry, 12(1), 172. [Google Scholar] [CrossRef] [PubMed]
- Park, Y. J., Ryu, H., Han, K. S., Kwon, J. H., Kim, H. K., Kang, H. C., Yoon, J. W., Cheon, S. H., & Shin, H. (2010). Anger, anger expression, and suicidal ideation in Korean adolescents. Archives of Psychiatric Nursing, 24(3), 168–177. [Google Scholar] [CrossRef] [PubMed]
- Patten, S. B., Kutcher, S., Streiner, D., Gratzer, D., Kurdyak, P., & Yatham, L. (2021). Population mental health and COVID-19: Why do we know so little? Canadian Journal of Psychiatry, 66(9), 782–784. [Google Scholar] [CrossRef]
- Patton, J. H., Stanford, M. S., & Barratt, E. S. (1995). Factor structure of the Barratt impulsiveness scale. Journal of Clinical Psychology, 51(6), 768–774. [Google Scholar] [CrossRef]
- Paz García-Portilla, M., Alejandra Sáiz, P., Díaz-Mesa, E. M., Fonseca, E., Arrojo, M., Sierra, P., Sarramea, F., Sánchez, E., Manuel Goikolea, J., Balanzá, V., Benabarre, A., & Bobes, J. (2009). Psychometric performance of the Oviedo sleep questionnaire in patients with severe mental disorder. Revista de Psiquiatría y Salud Mental (English Edition), 2(4), 169–177. [Google Scholar] [CrossRef]
- Reger, M. A., Stanley, I. H., & Joiner, T. E. (2020). Suicide mortality and coronavirus disease 2019—A perfect storm. JAMA Psychiatry, 77(11), 1093–1094. [Google Scholar] [CrossRef]
- Rogers, M. L., Kelliher-Rabon, J., Hagan, C. R., Hirsch, J. K., & Joiner, T. E. (2017). Negative emotions in veterans relate to suicide risk through feelings of perceived burdensomeness and thwarted belongingness. Journal of Affective Disorders, 208, 15–21. [Google Scholar] [CrossRef]
- Roster, C. A., Lucianetti, L., & Albaum, G. (2015). Exploring slider vs. categorical response formats in web-based surveys. Journal of Research Practice, 11(1), 1. [Google Scholar]
- Rozek, D. C., Crawford, J. N., LoSavio, S. T., Myers, U. S., Dabovich, P., Warnecke, A., Smith, N. B., & Bryan, C. J. (2021). The protective role of reasons for living on suicidal cognitions for military affiliated individuals with a positive PTSD screen in primary care settings. Journal of Affective Disorders, 292, 424–429. [Google Scholar] [CrossRef] [PubMed]
- Rueda-Jaimes, G. E., Castro-Rueda, V. A., Rangel-Martínez-Villalba, A. M., Moreno-Quijano, C., Martinez-Salazar, G. A., & Camacho, P. A. (2018). Validation of the beck hopelessness scale in patients with suicide risk. Revista de Psiquiatría y Salud Mental, 11(2), 86–93. [Google Scholar] [CrossRef]
- Russell, D. (1996). UCLA loneliness scale (version 3): Reliability, validity and factor structure. Journal of Personality Assessment, 66(42), 3–4. [Google Scholar] [CrossRef]
- Rutherford, C., Costa, D., Mercieca-Bebber, R., Rice, H., Gabb, L., & King, M. (2016). Mode of administration does not cause bias in patient-reported outcome results: A meta-analysis. Quality of Life Research, 25(3), 559–574. [Google Scholar] [CrossRef] [PubMed]
- Santomauro, D. F., Mantilla Herrera, A. M., Shadid, J., Zheng, P., Ashbaugh, C., Pigott, D. M., Abbafati, C., Adolph, C., Amlag, J. O., Aravkin, A. Y., Bang-Jensen, B. L., Bertolacci, G. J., Bloom, S. S., Castellano, R., Castro, E., Chakrabarti, S., Chattopadhyay, J., Cogen, R. M., Collins, J. K., … Ferrari, A. J. (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet, 398(10312), 1700–1712. [Google Scholar] [CrossRef] [PubMed]
- Sanz, J., Perdigón, A. L., & Vázquez, C. (2003). Adaptación española del Inventario para la Depresión de Beck-II (BDI-II): 2. Propiedades psicométricas en población general. Clínica y Salud, 14(3), 249–280. [Google Scholar]
- Sánchez-Teruel, D., Robles-Bello, M. A., & Camacho-Conde, J. A. (2020). Validity of the Spanish version of the herth hope index and the beck hopelessness scale in people who have attempted suicide. Actas Españolas de Psiquiatría, 48(4), 163–168. [Google Scholar]
- Schäfer, S. K., von Boros, L., Schaubruch, L. M., Kunzler, A. M., Lindner, S., Koehler, F., Werner, T., Zappalà, F., Helmreich, I., Wessa, M., Lieb, K., & Tüscher, O. (2024). Digital interventions to promote psychological resilience: A systematic review and meta-analysis. Npj Digital Medicine, 7, 1–12. [Google Scholar] [CrossRef]
- Simeon, D., Stanley, B., Frances, A., Mann, J. J., Winchel, R., & Stanley, M. (1992). Self-mutilation in personality disorders: Psychological and biological correlates. American Journal of Psychiatry, 149, 221–226. [Google Scholar] [CrossRef]
- Spielberger, C. D., Gorsuch, R. L., Lushene, R. E., Vagg, P. R., & Jacobs, G. A. (1983). Manual for the state-trait anxiety inventory (form Y). Consulting Psychologists Press. [Google Scholar]
- Stefansson, J., Nordström, P., & Jokinen, J. (2012). Suicide intent scale in the prediction of suicide. Journal of Affective Disorders, 136(1–2), 167–171. [Google Scholar] [CrossRef]
- Stringer, B., Van Meijel, B., Eikelenbooma, M., Koekkoek, B., Licht, C. M. M., Ad Kerkhof, J. E. M., Penninx, B. W. J. H., & Beekman, A. T. E. (2013). Recurrent suicide attempts in patients with depressive and anxiety disorders: The role of borderline personality traits. Journal of Affective Disorders, 151(1), 23–30. [Google Scholar] [CrossRef]
- Sueki, H. (2022). Relationship between beck hopelessness scale and suicidal ideation: A short-term longitudinal study. Death Studies, 46(2), 467–472. [Google Scholar] [CrossRef]
- Sun, L., Li, H., Zhang, J., & Wu, Q. (2015). Psychological strains and suicide intent: Results from a psychological autopsy study with Chinese rural young suicides. International Journal of Social Psychiatry, 61(7), 677–683. [Google Scholar] [CrossRef]
- Swann, A., Lijffijt, M., O’Brien, B., & Mathew, S. (2020). Impulsivity and suicidal behavior. In Recent advances in research on impulsivity and impulsive behaviors. Current Topics in Behavioral Neurosciences. Springer. [Google Scholar] [CrossRef]
- Torous, J., & Roberts, L. W. (2017). The ethical use of mobile health technology in clinical psychiatry. Journal of Nervous and Mental Disease, 205(1), 4–8. [Google Scholar] [CrossRef]
- Troister, T., D’Agata, M. T., & Holden, R. R. (2015). Suicide risk screening: Comparing the beck depression inventory-II, beck hopelessness scale, and psychache scale in undergraduates. Psychological Assessment, 27(4), 1500–1506. [Google Scholar] [CrossRef]
- Troister, T., & Holden, R. R. (2012). A two-year prospective study of psychache and its relationship to suicidality among high-risk undergraduates. Journal of Clinical Psychology, 68(9), 1019–1027. [Google Scholar] [CrossRef]
- Troister, T., & Holden, R. R. (2013). Factorial differentiation among depression, hopelessness, and psychache in statistically predicting suicidality. Measurement and Evaluation in Counseling and Development, 46(1), 50–63. [Google Scholar] [CrossRef]
- Turecki, G., Brent, D. A., Gunnell, D., O’Connor, R. C., Oquendo, M. A., Pirkis, J., & Stanley, B. H. (2019). Suicide and suicide risk. Nature Reviews Disease Primers, 5(1), 1–12. [Google Scholar] [CrossRef]
- Vázquez Morejón, A. J., & Jiménez García-Bóveda, R. (1994). RULS: Escala de soledad UCLA revisada. Fiabilidad y validez de una versión española. Revista de Psicología de la Salud, 6(1), 46–55. [Google Scholar]
- Velarde-Mayol, C., Fragua-Gil, S., & García-de-Cecilia, J. M. (2016). Validación de la escala de soledad de UCLA y perfil social en la población anciana que vive sola. Medicina de Familia. SEMERGEN, 42(3), 177–183. [Google Scholar] [CrossRef]
- Wang, H., Naghavi, M., Allen, C., Barber, R. M., Carter, A., Casey, D. C., Charlson, F. J., Chen, A. Z., Coates, M. M., Coggeshall, M., Dandona, L., Dicker, D. J., Erskine, H. E., Haagsma, J. A., Fitzmaurice, C., Foreman, K., Forouzanfar, M. H., Fraser, M. S., Fullman, N., … Zuhlke, L. J. (2016). Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the global burden of disease study 2015. The Lancet, 388(10053), 1459–1544. [Google Scholar] [CrossRef] [PubMed]
- Wilks, C. R., Morland, L. A., Dillon, K. H., Mackintosh, M. A., Blakey, S. M., Wagner, H. R., & Elbogen, E. B. (2019). Anger, social support, and suicide risk in U.S. military veterans. Journal of Psychiatric Research, 109, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Winkler, P., Formanek, T., Mlada, K., Kagstrom, A., Mohrova, Z., Mohr, P., & Csemy, L. (2020). Increase in prevalence of current mental disorders in the context of COVID-19: Analysis of repeated nationwide cross-sectional surveys. Epidemiology and Psychiatric Sciences, 29, e173. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. (2021). COVID-19 continues to disrupt essential health services in 90% of countries. Available online: https://www.who.int/news/item/23-04-2021-covid-19-continues-to-disrupt-essential-health-services-in-90-of-countries (accessed on 20 December 2024).
- Zalsman, G., Hawton, K., Wasserman, D., van Heeringen, K., Arensman, E., Sarchiapone, M., Carli, V., Höschl, C., Barzilay, R., Balazs, J., Purebl, G., Kahn, J. P., Sáiz, P. A., Lipsicas, C. B., Bobes, J., Cozman, D., Hegerl, U., & Zohar, J. (2016). Suicide prevention strategies revisited: 10-year systematic review. The Lancet Psychiatry, 3(7), 646–659. [Google Scholar] [CrossRef]
- Zhang, J., & Jia, C. X. (2007). Validating a short version of the suicide intent scale in China. Omega: Journal of Death and Dying, 55(4), 255–265. [Google Scholar] [CrossRef]
| Scale | Slider Question | N | Traditional Format Mean (Min–Max) | Slider Format Mean (Min–Max) | Pearson’s r | p-Value |
|---|---|---|---|---|---|---|
| * Beck Depression Inventory | How is your mood? | 56 | 5.268 (0–32) | 7.197 (0–10) | −0.541 | <0.001 |
| Psychache Scale | How much are you suffering? | 265 | 22.694 (13–64) | 2.385 (0–9) | 0.598 | <0.001 |
| Paykel | Do you have suicidal thoughts? | 223 | 0.973 (0–5) | 0.883 (0–10) | 0.503 | <0.001 |
| STAXI-2—State Anger | Do you feel angry? | 270 | 18.622 (15–50) | 1.541 (0–8) | 0.459 | <0.001 |
| STAXI-2—Trait Anger | Do you get angry easily? | 270 | 21.152 (10–37) | 4.037 (0–10) | 0.558 | <0.001 |
| STAXI-2—Anger Expression-Out | Do you express your anger? | 270 | 12.296 (6–23) | 4.852 (0–10) | 0.292 | <0.001 |
| STAXI-2—Anger Expression-In | Do you keep your anger to yourself? | 270 | 12.456 (6–22) | 3.889 (0–10) | 0.489 | <0.001 |
| STAXI-2—External Anger Control | Do you remain calm? | 270 | 17.900 (6–24) | 5.756 (0–10) | 0.354 | <0.001 |
| STAXI-2—Internal Anger Control | Do you count to ten before expressing your anger? | 270 | 14.463 (6–24) | 3.118 (0–10) | 0.380 | <0.001 |
| UCLA Loneliness Scale | How lonely do you feel? | 249 | 12.076 (0–58) | 2.531 (0–10) | 0.582 | <0.001 |
| * BIS—Cognitive/Attentional | Do you find it easy to concentrate? | 272 | 12.658 (2–28) | 6.224 (0–10) | −0.581 | <0.001 |
| * BIS—Non-Planning | Do you finish what you start? | 272 | 14.158 (2–40) | 7.404 (0–10) | −0.445 | <0.001 |
| BIS—Motor | How impulsive are you? | 272 | 14.856 (2–39) | 5.353 (0–10) | 0.426 | <0.001 |
| * RFL—Survival and Coping | Do you have a desire to live? | 274 | 19.467 (0–118) | 9.310 (0–10) | −0.589 | <0.001 |
| * RFL—Family-Related | Does your family motivate you to live? | 274 | 11.912 (0–50) | 9.164 (0–10) | −0.382 | <0.001 |
| * RFL—Fear of Suicide | Are you afraid of suicide? | 274 | 22.580 (0–35) | 5.967 (0–10) | −0.283 | <0.001 |
| * RFL—Fear of Disapproval | Are you concerned about what people would think if you died by suicide? | 274 | 10.117 (0–15) | 3.817 (0–10) | −0.455 | <0.001 |
| RFL—Moral Objections | Do you think suicide is wrong? | 274 | 13.496 (0–20) | 7.256 (0–10) | −0.359 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sosa, M.Z.P.; de-la-Vega-Sánchez, D.; Sanz-Gómez, S.; Alacreu-Crespo, A.; Moreno-Gea, P.; Saiz, P.A.; Seoane Rey, J.; Giner, J.; Giner, L. Concurrent Validity of Digital Measures of Psychological Dimensions Associated with Suicidality Using AuxiliApp. Behav. Sci. 2025, 15, 868. https://doi.org/10.3390/bs15070868
Sosa MZP, de-la-Vega-Sánchez D, Sanz-Gómez S, Alacreu-Crespo A, Moreno-Gea P, Saiz PA, Seoane Rey J, Giner J, Giner L. Concurrent Validity of Digital Measures of Psychological Dimensions Associated with Suicidality Using AuxiliApp. Behavioral Sciences. 2025; 15(7):868. https://doi.org/10.3390/bs15070868
Chicago/Turabian StyleSosa, Miguel Zacarías Pérez, Diego de-la-Vega-Sánchez, Sergio Sanz-Gómez, Adrián Alacreu-Crespo, Pedro Moreno-Gea, Pilar A. Saiz, Julio Seoane Rey, José Giner, and Lucas Giner. 2025. "Concurrent Validity of Digital Measures of Psychological Dimensions Associated with Suicidality Using AuxiliApp" Behavioral Sciences 15, no. 7: 868. https://doi.org/10.3390/bs15070868
APA StyleSosa, M. Z. P., de-la-Vega-Sánchez, D., Sanz-Gómez, S., Alacreu-Crespo, A., Moreno-Gea, P., Saiz, P. A., Seoane Rey, J., Giner, J., & Giner, L. (2025). Concurrent Validity of Digital Measures of Psychological Dimensions Associated with Suicidality Using AuxiliApp. Behavioral Sciences, 15(7), 868. https://doi.org/10.3390/bs15070868






