The Relationship between Self-Compassion and Sleep Quality: An Overview of a Seven-Year German Research Program
Abstract
1. Introduction
- Self-kindness vs. self-judgment. Self-compassionate people react with self-directed empathy and warmth when faced with daily stressors or the sleep problems themselves (instead of harshly criticizing themselves);
- Common humanity vs. isolation. Self-compassionate people cognitively classify their predicament as part of a universal human experience (instead of looking at themselves in isolation from others);
- Mindfulness vs. over-identification. Self-compassionate people pay attention to the suffering they have experienced (instead of avoiding the emotion or being totally carried away by it).
2. Materials and Methods
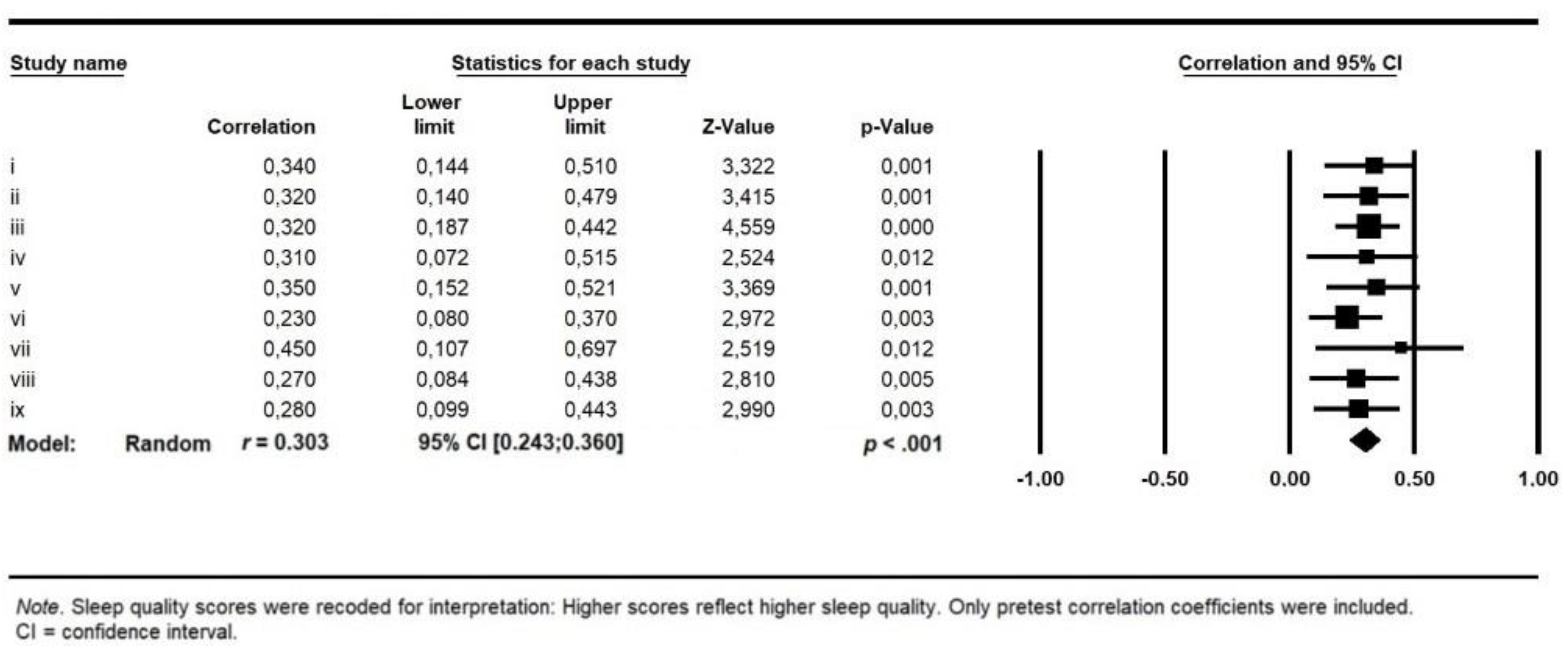
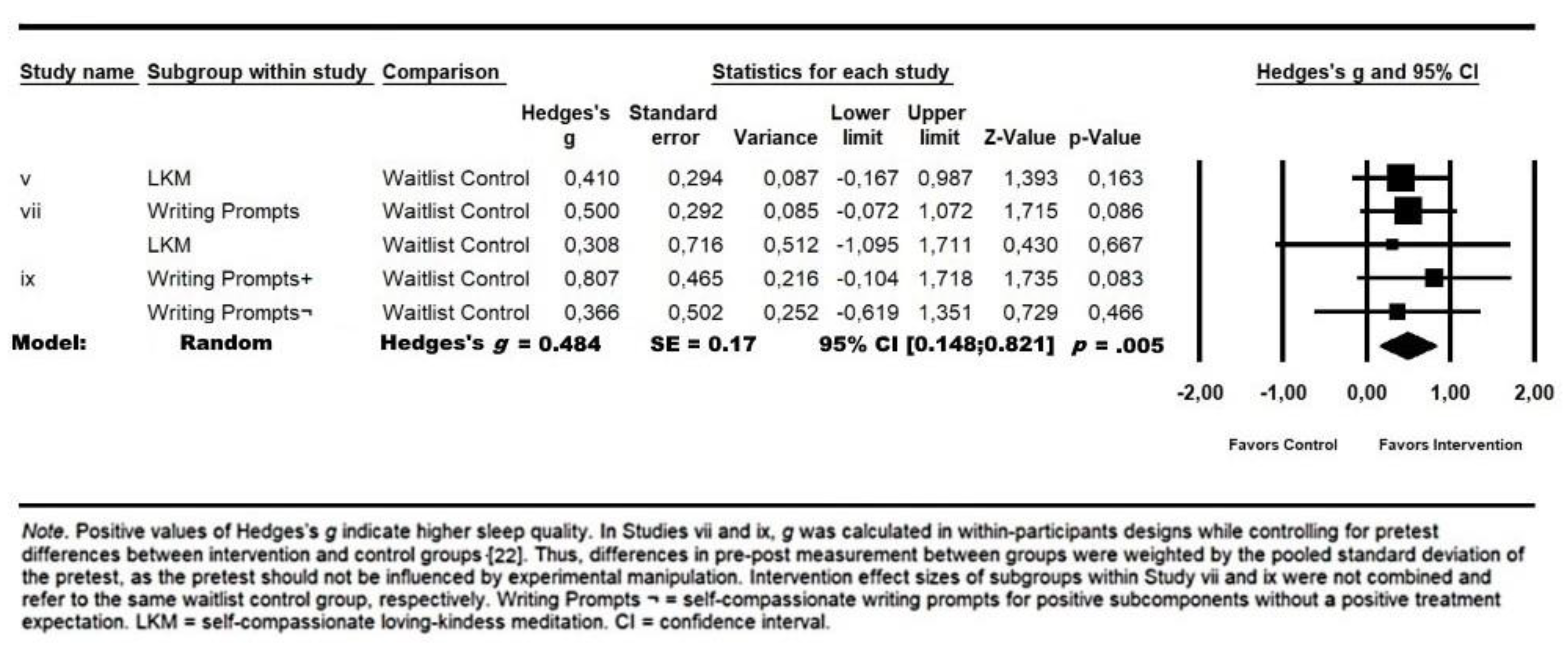
3. Results
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ohayon, M.M. Epidemiology of insomnia: What we know and what we still need to learn. Sleep Med. Rev. 2002, 6, 97–111. [Google Scholar] [CrossRef]
- Drake, C.L.; Roehrs, T.; Roth, T. Insomnia causes, consequences, and therapeutics: An overview. Depress. Anxiety 2003, 18, 163–176. [Google Scholar] [CrossRef]
- Baglioni, C.; Battagliese, G.; Feige, B.; Spiegelhalder, K.; Nissen, C.; Voderholzer, U.; Lombardo, C.; Riemann, D. Insomnia as a predictor of depression. A meta-analytic evaluation of longitudinal epidemiological studies. J. Affect. Disord. 2011, 135, 10–19. [Google Scholar] [CrossRef]
- Swanson, L.M.; Arnedt, J.T.; Rosekind, M.R.; Belenky, G.; Balkin, T.J.; Drake, C. Sleep disorders and work performance: Findings from the 2008 National Sleep Foundation Sleep in America poll. J. Sleep Res. 2011, 20, 487–494. [Google Scholar] [CrossRef]
- Morin, C.M.; Benca, R. Chronic insomnia. Lancet 2012, 379, 1129–1141. [Google Scholar] [CrossRef]
- Katz, D.A.; McHorney, C.A. The relationship between insomnia and health-related quality of life in patients with chronic illness. J. Fam. Pract. 2002, 51, 229–234. [Google Scholar]
- Rosekind, M.R.; Gregory, K.B.; Mallis, M.M.; Brandt, S.L.; Seal, B.; Lerner, D. The cost of poor sleep: Workplace productivity loss and associated costs. J. Occup. Environ. Med. 2010, 52, 91–98. [Google Scholar] [CrossRef]
- Perry, G.S.; Patil, S.P.; Presley-Cantrell, L.R. Raising awareness of sleep as a healthy behavior. Prev. Chronic Dis. 2013, 10, E133. [Google Scholar] [CrossRef] [PubMed]
- Matricciani, L.; Olds, T.; Petkov, J. In search of lost sleep: Secular trends in the sleep time of school-aged children and adolescents. Sleep Med. Rev. 2012, 16, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; Taggart, F.M.; Kandala, N.B.; Currie, A.; Peile, E.; Stranges, S.; Miller, M.A. Meta-analysis of short sleep duration and obesity in children and adults. Sleep 2008, 31, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Qaseem, A.; Kansagara, D.; Forciea, M.A.; Cooke, M.; Denberg, T.D. Management of chronic insomnia disorder in adults: A clinical practice guideline from the American College of Physicians. Ann. Intern. Med. 2016, 165, 125. [Google Scholar] [CrossRef] [PubMed]
- Riemann, D.; Perlis, M.L. The treatments of chronic insomnia. A review of benzodiazepine receptor agonists and psychological and behavioral therapies. Sleep Med. Rev. 2009, 13, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Van Straten, A.; van der Zweerde, T.; Kleiboer, A.; Cuijpers, P.; Morin, C.; Lancee, J. Cognitive and behavioral therapies in the treatment of insomnia: A meta-analysis. Sleep Med. Rev. 2018, 38, 3–16. [Google Scholar] [CrossRef] [PubMed]
- DAK-Gesundheit. Beiträge zur Gesundheitsökonomie und Versorgungsforschung (Band 28); Health Economics and Health Services Research; GER: Storm, Germany, 2017; Volume 28. [Google Scholar]
- Chevalier, H.; Los, F.; Boichut, D.; Bianchi, M.; Nutt, D.J.; Hajak, G.; Hetta, J.; Hoffmann, G.; Crowe, C. Evaluation of severe insomnia in the general population: Results of a European multinational survey. J. Psychopharmacol. 1999, 13, 21–24. [Google Scholar] [CrossRef]
- Espie, C.A.; Inglis, S.J.; Tessier, S.; Harvey, L. The clinical effectiveness of cognitive behaviour therapy for chronic insomnia: Implementation and evaluation of a sleep clinic in general medical practice. Behav. Res. Ther. 2001, 39, 45–60. [Google Scholar] [CrossRef]
- Janson, C.; Lindberg, E.; Gislason, T.; Elmasry, A.; Boman, G. Insomnia in men—A 10-year prospective population based study. Sleep 2001, 24, 425–430. [Google Scholar] [CrossRef]
- Ancoli-Israel, S.; Roth, T. Characteristics of insomnia in the United States: Results of the 1991 National Sleep Foundation Survey. I. Sleep 1999, 22, 347–353. [Google Scholar]
- Gong, H.; Ni, C.X.; Liu, Y.Z.; Zhang, Y.; Su, W.J.; Lian, Y.J.; Peng, W.; Jiang, C.L. Mindfulness meditation for insomnia: A meta-analysis of randomized controlled trials. J. Psychosom. Res. 2016, 89, 1–6. [Google Scholar] [CrossRef]
- Khoury, B.; Lecomte, T.; Fortin, G.; Masse, M.; Therien, P.; Bouchard, V.; Chapleau, M.A.; Paquin, K.; Hofmann, S.G. Mindfulness-based therapy: A comprehensive meta-analysis. Clin. Psychol. Rev. 2013, 33, 763–771. [Google Scholar] [CrossRef]
- Virgili, M. Mindfulness-based interventions reduce psychological distress in working adults. A meta-analysis of intervention studies. Mindfulness 2015, 6, 326–337. [Google Scholar] [CrossRef]
- Klatt, M.; Norre, C.; Reader, B.; Yodice, L.; White, S. Mindfulness in Motion. A Mindfulness-Based Intervention to Reduce Stress and Enhance Quality of Sleep in Scandinavian Employees. Mindfulness 2016, 8, 481–488. [Google Scholar] [CrossRef]
- Neff, K.D. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self Identity 2003, 2, 85–101. [Google Scholar] [CrossRef]
- Allen, A.B.; Leary, M.R. Self-Compassion, stress, and coping. Soc. Personal. Psychol. Compass 2010, 4, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Inwood, E.; Ferrari, M. Mechanisms of change in the relationship between self-compassion, emotion regulation, and mental health: A systematic review. Appl. Psychol. Health Well Being 2018, 10, 215–235. [Google Scholar] [CrossRef] [PubMed]
- Fredrickson, B.L. The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. Am. Psychol. 2001, 56, 218–226. [Google Scholar] [CrossRef]
- Gilbert, P. Compassion as a social mentality: An evolutionary approach. In Compassion; Routledge: London, UK, 2017; pp. 31–68. [Google Scholar]
- Rockliff, H.; Gilbert, P.; McEwan, K.; Lightman, S.; Glover, D. A pilot exploration of heart rate variability and salivary cortisol responses to compassion-focused imagery. Clin. Neuropsychiatry 2008, 5, 132–139. [Google Scholar]
- Harvey, A.G. A cognitive model of insomnia. Behav. Res. Ther. 2002, 40, 869–893. [Google Scholar] [CrossRef]
- Calkins, A.; Hearon, B.; Capozzoli, M.; Otto, M. Psychosocial predictors of sleep dysfunction: The role of anxiety sensitivity, dysfunctional beliefs, and neuroticism. Behav. Sleep Med. 2013, 11, 133–143. [Google Scholar] [CrossRef]
- Kemper, K.J.; Mo, X.; Khayat, R. Are mindfulness and self-compassion associated with sleep and resilience in health professionals? J. Altern. Complement. Med. 2015, 21, 496–503. [Google Scholar] [CrossRef]
- Sirois, F.M.; Kitner, R.; Hirsch, J.K. Self-compassion 2015, affect, and health-promoting behaviors. Health Psychol. 2015, 34, 661. [Google Scholar] [CrossRef]
- Hu, Y.; Wang, Y.; Sun, Y.; Arteta-Garcia, J.; Purol, S. Diary study: The protective role of self-compassion on stress-related poor sleep quality. Mindfulness 2018, 9, 1931–1940. [Google Scholar] [CrossRef]
- Zessin, U.; Dickhäuser, O.; Garbade, S. The relationship between self-compassion and well-being: A meta-analysis. Appl. Psychol. Health Well Being 2015, 7, 340–364. [Google Scholar] [CrossRef] [PubMed]
- MacBeth, A.; Gumley, A. Exploring compassion: A meta-analysis of the association between self-compassion and psychopathology. Clin. Psychol. Rev. 2002, 32, 545–552. [Google Scholar] [CrossRef] [PubMed]
- Butz, S.; Stahlberg, D. Can self-compassion improve sleep quality via reduced rumination? Self Identity 2018, 17, 666–686. [Google Scholar] [CrossRef]
- Goh, J.X.; Hall, J.A.; Rosenthal, R. Mini meta-analysis of your own studies: Some arguments on why and a primer on how. Soc. Personal. Psychol. Compass 2016, 10, 535–549. [Google Scholar] [CrossRef]
- Neff, K.D. The development and validation of a scale to measure self-compassion. Self Identity 2003, 2, 223–250. [Google Scholar] [CrossRef]
- Raes, F.; Pommier, E.; Neff, K.D.; van Gucht, D. Construction and factorial validation of a short form of the self-compassion scale. Clin. Psychol. Psychother. Int. J. Theory Pract. 2011, 18, 250–255. [Google Scholar] [CrossRef]
- Hupfeld, J.; Ruffieux, N. Validierung einer deutschen Version der Self-Compassion Scale (SCS-D). [Validation of a German version of the Self-Compassion Scale (SCS-D)]. Z. Für Klin. Psychol. Und Psychother. 2011, 40, 115–123. [Google Scholar] [CrossRef]
- Galante, J.; Galante, I.; Bekkers, M.J.; Gallacher, J. Effect of kindness-based meditation on health and well-being. A systematic review and meta-analysis. J. Consult. Clin. Psychol. 2014, 82, 1101–1114. [Google Scholar] [CrossRef]
- Leary, M.R.; Tate, E.B.; Adams, C.E.; Allen, A.; Hancock, J. Self-compassion and reactions to unpleasant self-relevant events. The implications of treating oneself kindly. J. Personal. Soc. Psychol. 2007, 92, 887–904. [Google Scholar] [CrossRef]
- Jenkins, C.D.; Stanton, B.A.; Niemcryk, S.J.; Rose, R.M. A scale for the estimation of sleep problems in clinical research. J. Clin. Epidemiol. 1988, 41, 313–321. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index. A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Morris, S.B. Estimating effects sizes from pretest-posttest control group designs. Organ. Res. Methods 2008, 11, 364–386. [Google Scholar] [CrossRef]
- Neff, K.D.; Germer, C.K. A pilot study and randomized controlled trial of the mindful self-compassion program. J. Clin. Psychol. 2013, 69, 28–44. [Google Scholar] [CrossRef]
- Tang, N.K.; Fiecas, M.; Afolalu, E.F.; Wolke, D. Changes in sleep duration, quality, and medication use are prospectively associated with health and well-being: Analysis of the UK household longitudinal study. Sleep 2017, 40, 1–10. [Google Scholar] [CrossRef]
- Goodman, R.J.; Quaglia, J.T.; Brown, K.W. Burning issues in dispositional mindfulness research. In Handbook of Mindfulness and Self-Regulation (S. 67–80); Springer: Heidelberg, Germany, 2015. [Google Scholar] [CrossRef]
- Gordon, A.M.; Mendes, W.B.; Prather, A.A. The social side of sleep: Elucidating the links between sleep and social processes. Curr. Dir. Psychol. Sci. 2017, 26, 470–475. [Google Scholar] [CrossRef]
- Littner, M.; Kushida, C.A.; Anderson, W.M.; Bailey, D.; Berry, R.B.; Davila, D.G.; Hirshkowitz, M.; Kapen, S.; Kramer, M.; Loube, D.; et al. Practice parameters for the role of actigraphy in the study of sleep and circadian rhythms: An update for 2002. Sleep 2003, 26, 337–341. [Google Scholar] [CrossRef]
- Coates, T.J.; Killen, J.D.; George, J.; Marchini, E.; Silverman, S.; Thoresen, C. Estimating sleep parameters: A multitrait-multimethod analysis. J. Consult. Clin. Psychol. 1982, 50, 345–352. [Google Scholar] [CrossRef]
- Muris, P.; Otgaar, H.; Petrocchi, N. Protection as the mirror image of psychopathology. Further critical notes on the self-compassion scale. Mindfulness 2016, 7, 787–790. [Google Scholar] [CrossRef]
- Braver, S.L.; Thoemmes, F.J.; Rosenthal, R. Continuously cumulating meta-analysis and replicability. Perspect. Psychol. Sci. 2014, 9, 333–342. [Google Scholar] [CrossRef] [PubMed]
| First Author and Year | Notation | Publication Status | Sample (N) | Mean Age (SD) | Gender (% Female) | Design | Scales/Interventions Used |
|---|---|---|---|---|---|---|---|
| Kombeiz and Stahlberg (2012) | i | Unpublished diploma thesis | University: students and community (N = 91) | 27.08 (7.94) | 77.2% | Correlational | SCS [12]; Sleep Quality Index [17] |
| Popova, et al. (2014) | ii | Unpublished diploma thesis | University: students and community (N = 109) | 25.90 (6.19) | 69.2% | Correlational; diary study (one week) | SCS [12]; Sleep Quality Index [17] |
| Stahlberg et al. (2016) | iii | Unpublished research project | University: students and community (N = 192) | 27.00 (NR) | 76.0% | Correlational | SCS [12]; Sleep Quality Index [17] |
| Butz and Stahlberg (2016) I | iv | Published Butz and Stahlberg (2018) | University: students (N = 65) | 21.41 (5.65) | 75.0% | Quasi-experimental (randomized order) | SCS-SF [13]; ISI [19] |
| Butz and Stahlberg (2016) II | v | Published Butz and Stahlberg (2018) | University: students (N = 88) | 22.59 (3.43) | 54.5% | Experimental; one-time intervention vs. waitlist | SCS [12]; Sleep Quality Index [17]/20min LKM vs. writing prompts |
| Tartter and Butz (2016) | vi | Unpublished bachelor’s thesis | University: students and community (N = 164) | 27.50 (11.51) | 68.0% | Correlational | SCS-SF [13]; Sleep Quality Index [17] |
| Butz and Stahlberg (2017) | vii | Published Butz and Stahlberg (2018) | Clinical: major depression episode (N = 30) | 42.45 (11.54) | 50.0% | Experimental; Pre–post intervention (20min 1 session, 5min 4 sessions) vs. waitlist | SCS-SF [13]; ISI [19]/20min LKM; 5min SC-break |
| Kuhn and Butz (2017) | viii | Unpublished bachelor’s thesis | University: students and community (N = 106) | 40.00 (NR) | 66.0% | Correlational | SCS-SF [13]; PSQI [18] |
| Butz and Stahlberg (2018) | ix | Published in partial fulfillment of the requirements for the degree of Doctor of Social Sciences | University: students (N = 111) | 21.24 (3.18) | 88.3% | Experimental; pre–post intervention (20min 1 session, 5min 6 sessions) vs. Waitlist | SCS [12]; Sleep Quality Index [17]/20min writing prompts; 5min SC-break |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Butz, S.; Stahlberg, D. The Relationship between Self-Compassion and Sleep Quality: An Overview of a Seven-Year German Research Program. Behav. Sci. 2020, 10, 64. https://doi.org/10.3390/bs10030064
Butz S, Stahlberg D. The Relationship between Self-Compassion and Sleep Quality: An Overview of a Seven-Year German Research Program. Behavioral Sciences. 2020; 10(3):64. https://doi.org/10.3390/bs10030064
Chicago/Turabian StyleButz, Sebastian, and Dagmar Stahlberg. 2020. "The Relationship between Self-Compassion and Sleep Quality: An Overview of a Seven-Year German Research Program" Behavioral Sciences 10, no. 3: 64. https://doi.org/10.3390/bs10030064
APA StyleButz, S., & Stahlberg, D. (2020). The Relationship between Self-Compassion and Sleep Quality: An Overview of a Seven-Year German Research Program. Behavioral Sciences, 10(3), 64. https://doi.org/10.3390/bs10030064




