Outcomes of Treatment of Eyelids and Third Eyelid Tumours in Dogs Using High-Frequency Radiowave Surgery
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
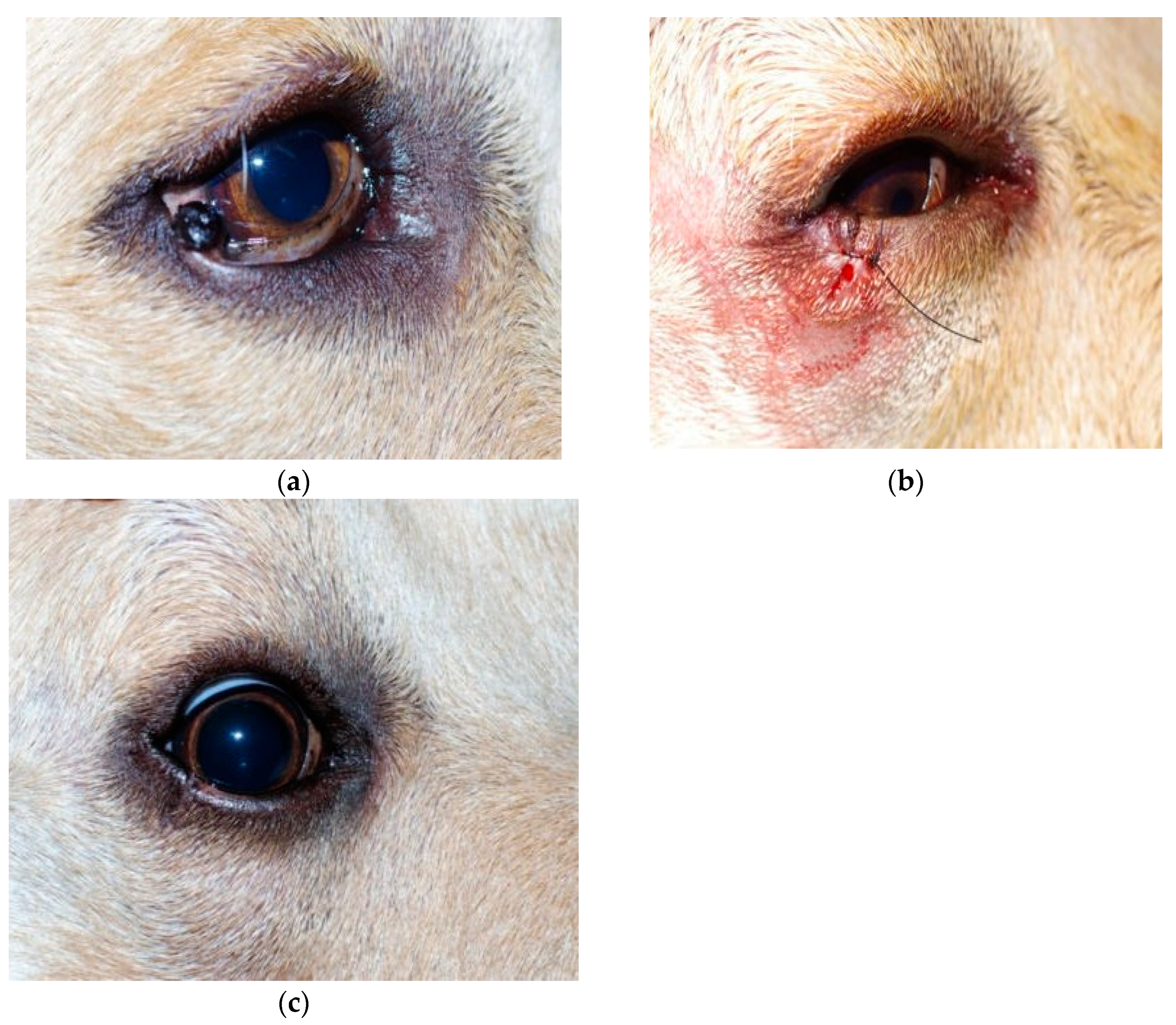
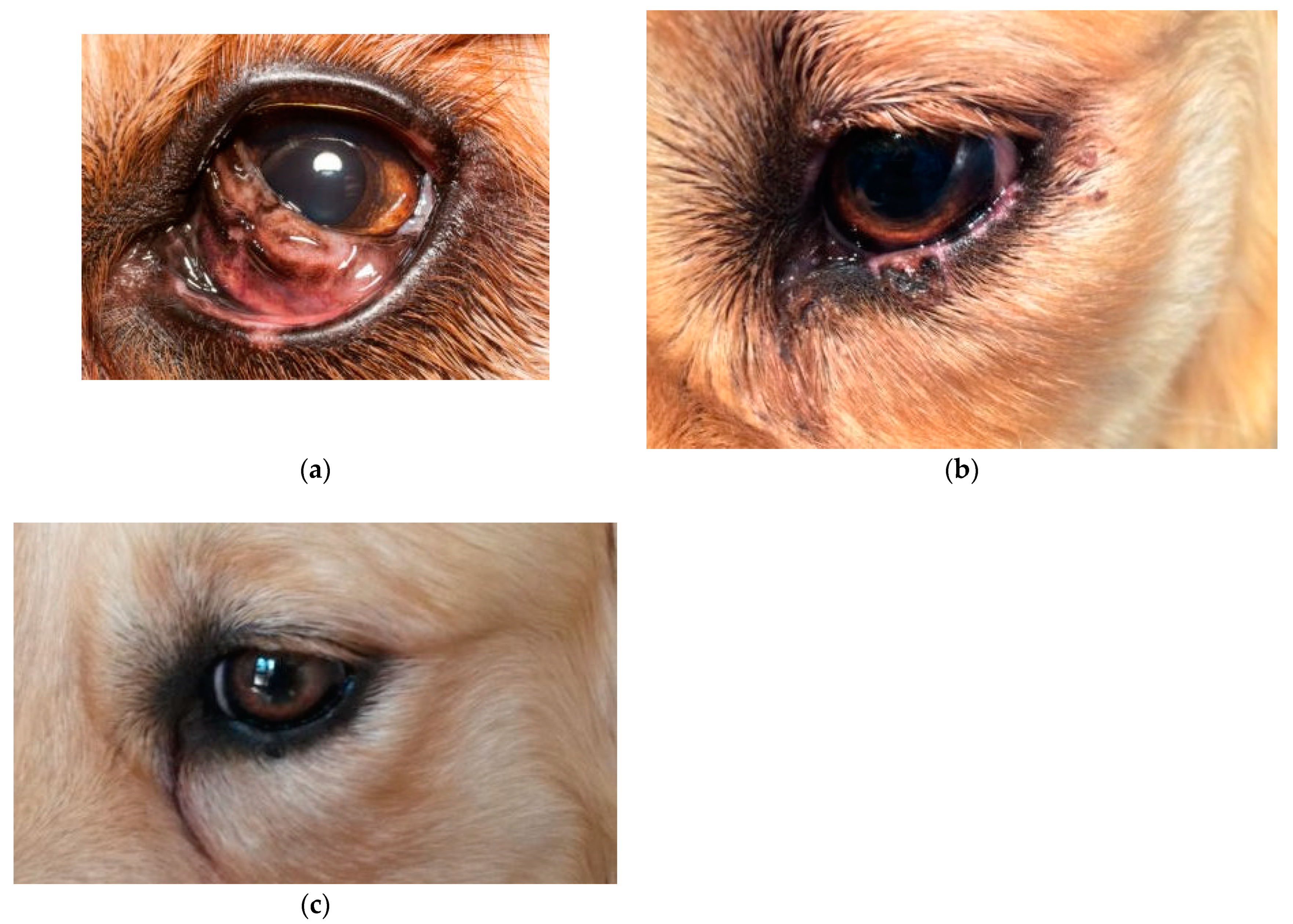
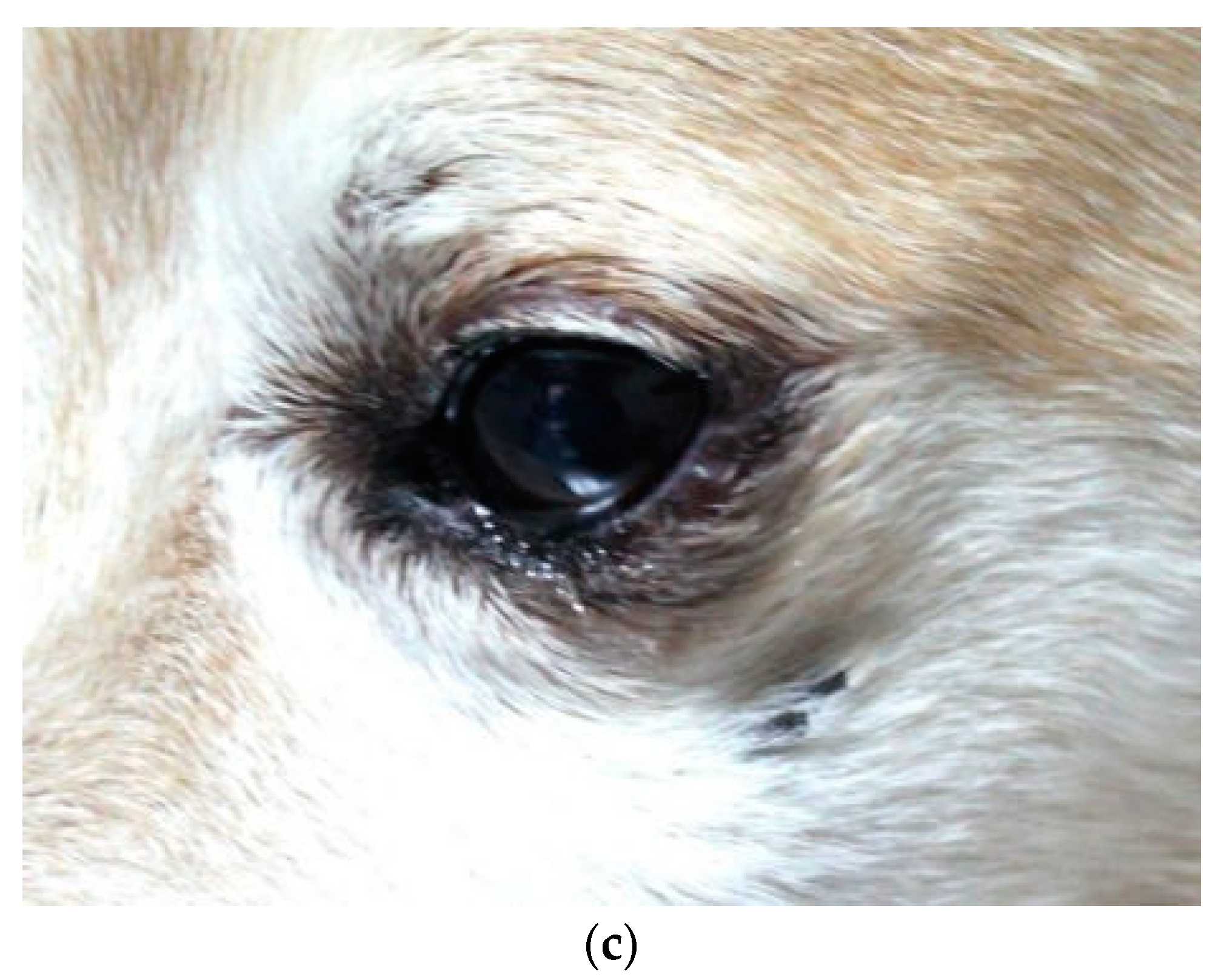
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stades, F.C.; van der Woerdt, A. Veterinary Ophthalmology; Chapter 14; Gelatt, K.N., Gilger, B.C., Kern, T.J., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2013; pp. 832–893. [Google Scholar]
- Hendrix, D.V.H. Veterinary Ophthalmology; Chapter 17; Gelatt, K.N., Gilger, B.C., Kern, T.J., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2013; pp. 945–975. [Google Scholar]
- Aquino, S.M. Management of Eyelid Neoplasms in the Dog and Cat. Clin. Tech. Small Anim. Pract. 2007, 22, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Gelatt, K.N. Diseases and Surgery of the Canine Eyelids. In Essentials of Veterinary Opththalmology; Gelatt, K.N., Ed.; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2000; pp. 47–72. [Google Scholar]
- Raus, P.P.M.; Verhaert, P.D.E.M. Radiofrequency surgery: 3500 years old and still young. Orbit 2018, 37, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Hema, D.; Prasanna, J.S. Radiosurgery in periodontics: Have we forgotten it? J. Indian Soc. Periodontol. 2021, 25, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Maness, W.L.; Roeber, F.W.; Clark, R.E.; Cataldo, E.; Riis, D.; Haddad, A.W. Histologic evaluation of electrosurgery with varying frequency and waveform. J. Prosthet. Dent. 1978, 40, 304–308. [Google Scholar] [CrossRef] [PubMed]
- Bridenstine, J. Use of Ultra-High Frequency Electrosurgery (Radiosurgery) for Cosmetic Surgical Procedures. Dermatol. Surg. 1998, 24, 397–400. [Google Scholar] [CrossRef]
- Suh, J.S.; Choi, S. The Effect of Conjunctivochalasis Surgery Using a High-Frequency Radio-Wave Electrosurgical Unit. J. Korean Ophthalmol. Soc. 2012, 53, 1571–1576. [Google Scholar] [CrossRef] [Green Version]
- Niamtu, J. Radiowave Surgery versus CO2 Laser for Upper Blepharoplasty Incision: Which Modality Produces the Most Aesthetic Incision? Dermatol. Surg. 2008, 34, 912–921. [Google Scholar] [CrossRef]
- Eshraghi, B.; Torabi, H.R.; Kasaie, A.; Rajabi, M.T. The Use of a Radiofrequency Unit for Excisional Biopsy of Eyelid Papillo—Mas. Ophthalmic Plast. Reconstr. Surg. 2010, 26, 448–449. [Google Scholar] [CrossRef]
- Youm, D.J.; Kim, J.M.; Choi, C.Y. Simple Surgical Approach with High-Frequency Radio-Wave Electrosurgery for Conjunctivochalasis. Ophthalmology 2010, 117, 2129–2133. [Google Scholar] [CrossRef]
- Choi, S.M.; Jin, K.H.; Kim, T.G. Successful treatment of conjunctival lymphangiectasia accompanied by corneal dellen using a high-frequency radiowave electrosurgical device. Indian J. Ophthalmol. 2019, 67, 409–411. [Google Scholar]
- Bellows, J. Laser and Radiosurgery in Veterinary Dentistry. Vet. Clin. N. Am. Small Anim. Pract. 2013, 43, 651–668. [Google Scholar] [CrossRef] [PubMed]
- Elkins, A.D. Soft palate resection in brachycephalic dogs. Vet. Forum 2005, 22, 43–46. [Google Scholar]
- Miller, W.W. Using High-Frequency Radio Wave Technology in Veterinary Surgery. Vet. Med. 2004, 99, 796–804. [Google Scholar]
- Fucci, V.; Elkins, A.D. Electrosurgery: Principles and guidelines in veterinary medicine. Compend. Contin. Educ. Pract. Vet. 1991, 13, 407–414. [Google Scholar]
- Hernandez-Divers, S.J. Radiosurgery and Laser in Zoological Practice: Separating Fact from Fiction. J. Exot. Pet. Med. 2008, 17, 165–174. [Google Scholar] [CrossRef]
- Altman, R.B. Radiosurgery. Semin. Avian Exot. Pet Med. 2000, 9, 180–183. [Google Scholar] [CrossRef]
- Roberts, S.M.; Severin, G.A.; Lavach, J.D. Prevalence and treatment of palpebral neoplasms in the dog: 200 cases (1975–1983). J. Am. Vet. Med. Assoc. 1986, 189, 1355–1359. [Google Scholar]
- Wang, S.-L.; Dawson, C.; Wei, L.-N.; Lin, C.-T. The investigation of histopathology and locations of excised eyelid masses in dogs. Vet. Rec. Open 2019, 6, e000344. [Google Scholar] [CrossRef] [Green Version]
- Krehbiel, J.D.; Langham, R.F. Eyelid neoplasms of dogs. Am. J. Vet. Res. 1975, 36, 115–119. [Google Scholar]
- Scott, E.M.; Miller, P.E. Tumors of the Eye and Ocular Adnexa. In Clinical Small Animal Internal Medicine; Bruyette, D.S., Bex-field, N., Chretin, J.D., Kidd, L., Kube, S., Langston, C., Owen, T.J., Oyama, M.A., Peterson, N., Reiter, L.V., et al., Eds.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2020; pp. 1261–1271. [Google Scholar]
- Goldschmidt, M.H.; Goldschmidt, K.H. Epithelial and Melanocytic Tumors of the Skin. In Tumors in Domestic Animals, 5th ed.; Meuten, D.J., Ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2016; pp. 88–141. [Google Scholar]
- Westermayer, H.D.; Hendrix, D.V.H. Basic Ophthalmic Surgical Procedures. In Veterinary Surgery Small Animals; Tobias, K.M., Johnson, S.A., Eds.; Elsevier Saunders: London, UK, 2013; pp. 2091–2119. [Google Scholar]
- Dubielzig, R.R. Tumors of the eye. In Tumors in Domestic Animals, 5th ed.; Meuten, D.J., Ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2016; pp. 892–922. [Google Scholar]
- Stades, F.C.; Van der Woerdt, A. Canine Eyelids: Disease and Surgery. In Essentials of Veterinary Ophthalmology; Gelatt, K.N., Plummer, C.E., Eds.; Wiley Blackwell: Hoboken, NJ, USA, 2022; pp. 240–279. [Google Scholar]
- Labelle, A.L.; Labelle, P. Canine ocular neoplasia: A review. Vet. Ophthalmol. 2013, 16, 3–14. [Google Scholar] [CrossRef]
- Muñoz-Duque, J.D.; Ramírez-Rojas, M.C.; Duque-Arias, S.; Correa-Valencia, N.M. Eye-related neoplasms in dogs: A retrospective study. Rev. Colomb. Cienc. Pecu. 2019, 32, 298–311. [Google Scholar] [CrossRef]
- Mould, J.R.B.; Petersen-Jones, S.M.; Peruccio, C.; Ratto, A.; Sassani, J.W.; Harbour, J.W. Uveal melanocytic tumors. In Ocular Tumors in Animals and Humans; Peiffer, R.L., Jr., Simons, K.B., Eds.; Iowa State Press: Ames, IA, USA, 2002; pp. 225–282. [Google Scholar]
- Wilcock, B.P.; Peiffer, J.R. Morphology and behavior of primary ocular melanomas in 91 dogs. Vet. Pathol. 1986, 23, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Nishiya, A.T.; Massoco, C.O.; Felizzola, C.R.; Perlmann, E.; Batschinski, K.; Tedardi, M.V.; Garcia, J.S.; Mandonca, P.P.; Teixeira, T.F.; Zaidan Dagli, M.L. Comparative aspects of canine melanoma. Vet. Sci. 2016, 3, 7. [Google Scholar] [CrossRef] [Green Version]
- Yu-Speight, A.; Cho, J.; Fossum, T.W. Surgery of the eye. In Small Animal Surgery, 5th ed.; Fossum, T.W., Ed.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 266–301. [Google Scholar]
- Older, J.J. The Value of Radiosurgery in Oculoplastics. Ophthalmic Plast. Reconstr. Surg. 2002, 18, 214–218. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Lee, S.; Suh, E. Removal of Conjunctival Cyst with High-Frequency Radio-Wave Electrosurgery. Can. J. Ophthalmol. 2015, 50, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Hodshon, R.T.; Sura, P.A.; Schumacher, J.P.; Steeil, J.C.; Newkirk, K.M. Comparison of first-intention healing of carbon dioxide laser, 4.0-MHz radiosurgery, and scalpel incisions in ball pythons (Python regius). Am. J. Vet. Res. 2013, 74, 499–508. [Google Scholar] [CrossRef] [PubMed]
- Silverman, E.B.; Read, R.W.; Boyle, C.R.; Cooper, R.; Miller, W.W.; McLaughlin Ron, M. Histologic Comparison of Canine Skin Biopsies Collected Using Monopolar Electrosurgery, CO2 Laser, Radiowave Radiosurgery, Skin Biopsy Punch, and Scalpel. Vet. Surg. 2007, 36, 50–56. [Google Scholar] [CrossRef]
- Olivar, A.C.; Forouhar, F.A.; Gillies, C.G.; Servanski, D.R. Transmission electron microscopy: Evaluation of damage in human oviducts caused by different surgical instruments. Ann. Clin. Lab. Sci. 1999, 29, 281–285. [Google Scholar]
- Turner, R.J.; Cohen, R.A.; Voet, R.L.; Stephens, S.R.; Weinstein, S.A. Analysis of tissue margins of cone biopsy specimens obtained with “cold knife”, CO2 and Nd:YAG lasers and a radiofrequency surgical unit. J. Reprod. Med. 1992, 37, 607–610. [Google Scholar]
- Hurwitz, J.J.; Johnson, D.; Howarth, D.; Molgat, Y.M. Experimental Treatment of Eyelashes with High-Frequency Radio Wave Electrosurgery. Can. J. Ophthalmol. 1993, 28, 62–64. [Google Scholar]
- Woo, K.I.; Choi, C.Y. High-Frequency Radiowave Electrosurgery for Persistent Conjunctival Chemosis Following Cosmetic Blepharoplasty. Plast. Reconstr. Surg. 2014, 133, 1336–1342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahn, J.M.; Choi, C.Y.; Seo, K.Y. Surgical Approach with High-Frequency Radiowave Electrosurgery for Superior Limbic Keratoconjunctivitis. Cornea 2014, 33, 210–214. [Google Scholar] [CrossRef] [PubMed]
- Moore, C.P.; Constantinescu, G.M. Surgery of Adnexa. Vet. Clin. N. Am. Small Anim. Pract. 1997, 11, 543–602. [Google Scholar] [CrossRef] [PubMed]
- Shenoda, Y.; Ward, M.P.; McKeegan, D.; Fawcett, A. “The Cone of Shame”: Welfare Implications of Elizabethan Collar Use on Dogs and Cats as Reported by Their Owners. Animals 2020, 10, 333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pigatto, J.A.T.; Albuquerque, L.D.; Voll, J.; Driemeier, D. Hemangiosarcoma of the Third Eyelid in a Dog. Acta Sci. Veteinariae 2015, 43, 91. [Google Scholar]
- Dees, D.D.; Schobert, C.S.; Dubielzig, R.R.; Stein, T.J. Third eyelid gland neoplasms of dogs and cats: A retrospective histopathologic study of 145 cases. Vet. Ophthalmol. 2016, 19, 138–143. [Google Scholar] [CrossRef]
- Saito, A.; Izumisawa, Y.; Yamashita, K.; Kotani, T. The effect of third eyelid gland removal on the ocular surface of dogs. Vet. Ophthalmol. 2001, 4, 13–18. [Google Scholar] [CrossRef]
- Saito, A.; Watanabe, Y.; Kotani, T. Morphologic changes of the anterior corneal epithelium cause by third eyelid removal in dogs. Vet. Ophthalmol. 2004, 7, 113–119. [Google Scholar] [CrossRef]
- Dees, D.D.; Knollinger, A.M.; MacLaren, N.E. Carbon dioxide (CO2) laser third eyelid excision: Surgical description and report of 7 cases. Vet. Ophthalmol. 2015, 18, 381–384. [Google Scholar] [CrossRef]
- Bussieres, M.; Krohne, S.G.; Stiles, J.; Townsend, W.M. The Use of Carbon Dioxide Laser for the Ablation of Meibomian Gland Adenomas in Dogs. J. Am. Anim. Hosp. Assoc. 2005, 41, 227–234. [Google Scholar] [CrossRef]
- Andreani, V.; Guandalini, A.; D’Anna, N.; Giudice, C.; Corvi, R.; di Girolamo, N.; Sapienza, J.S. The Combined Use of Surgical Debulking and Diode Laser Photocoagulation for Limbal Melanoma Treatment: A Retrospective Study of 21 Dogs. Vet. Ophthalmol. 2017, 20, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Zibura, A.E.; Henriksen, M.d.L.; Rendahl, A.; Lim, C.C.; Reilly, C. Retrospective Evaluation of Canine Palpebral Masses Treated with Debulking and Cryotherapy: 46 Cases. Vet. Ophthalmol. 2019, 22, 256–264. [Google Scholar] [CrossRef] [PubMed]



| Breed | Sex | Age | Localization of the Tumor | Type of Tumor | Duration of Surgery | Bleeding Degree |
|---|---|---|---|---|---|---|
| Alaskan Malamute | F | 7 | Lower left eyelid | Meibomian gland adenoma | 8 | Absent |
| Beagle | M | 7 | Lower left eyelid | Meibomian gland epithelioma | 7 | Absent |
| Beagle | F | 2 | Upper right eyelid | Histiocytoma | 7 | Absent |
| Boxer | M | 8 | Upper right eyelid | Papilloma | 7 | Absent |
| Boxer | M | 6 | Upper right eyelid | Meibomian gland adenoma | 5 | Absent |
| Breton | F | 8 | Lower left eyelid | Papilloma | 4 | Absent |
| Cocker Spaniel | F | 7 | Upper right eyelid | Meibomian gland adenoma | 6 | Absent |
| Cocker Spaniel | M | 8 | Upper right eyelid | Meibomian gland adenoma | 6 | Absent |
| Dachshund | M | 5 | Upper left eyelid | Meibomian gland adenoma | 6 | Mild |
| Dalmatian | M | 3 | Upper left eyelid | Histiocytoma | 6 | Absent |
| Dobermann | M | 7 | Upper left eyelid | Papilloma | 5 | Absent |
| Dogue de Bordeaux | M | 3 | Lower right eyelid | Histiocytoma | 7 | Absent |
| English Setter | F | 7 | Upper right eyelid | Meibomian gland adenoma | 5 | Absent |
| English Setter | M | 6 | Upper right eyelid | Papilloma | 6 | Mild |
| German Shepherd | M | 10 | Lower left eyelid | Meibomian gland epithelioma | 5 | Absent |
| German Shepherd | M | 6 | Upper left eyelid | Meibomian gland adenoma | 5 | Absent |
| Golden Retriever | M | 4 | Left third eyelid | Melanocytoma | 6 | Absent |
| Golden Retriever | F | 7 | Upper right eyelid | Meibomian gland adenoma | 5 | Absent |
| Labrador Retriever | F | 6 | Lower right eyelid | Meibomian gland adenoma | 7 | Absent |
| Maltese | M | 11 | Lower left eyelid | Meibomian gland adenoma | 6 | Absent |
| Maremma Shepherd | F | 6 | Lower right eyelid | Meibomian gland adenoma | 7 | Absent |
| Mixed | M | 9 | Upper right eyelid | Meibomian gland epithelioma | 8 | Mild |
| Mixed | F | 8 | Upper right eyelid | Meibomian gland adenoma | 6 | Absent |
| Mixed | F | 5 | Upper right eyelid | Meibomian gland adenoma | 8 | Absent |
| Mixed | M | 12 | Upper left eyelid | Meibomian gland adenoma | 7 | Absent |
| Mixed | M | 10 | Lower right eyelid | Meibomian gland adenoma | 5 | Absent |
| Mixed | M | 10 | Upper right eyelid | Meibomian gland adenoma | 7 | Absent |
| Mixed | M | 10 | Upper left eyelid | Meibomian gland adenoma | 7 | Mild |
| Mixed | F | 10 | Upper right eyelid | Meibomian gland adenoma | 6 | Absent |
| Mixed | F | 9 | Lower right eyelid | Papilloma | 7 | Absent |
| Mixed | M | 7 | Lower right eyelid | Papilloma | 9 | Absent |
| Pekinese | M | 8 | Upper left eyelid | Meibomian gland adenoma | 5 | Absent |
| Pinscher | F | 8 | Lower right eyelid | Meibomian gland adenoma | 5 | Absent |
| Pitbull | M | 7 | Lower left eyelid | Meibomian gland adenoma | 7 | Mild |
| Pitbull | F | 8 | Upper right eyelid | Papilloma | 8 | Absent |
| Poodle | F | 8 | Lower left eyelid | Meibomian gland adenoma | 6 | Absent |
| Poodle | F | 11 | Lower left eyelid | Papilloma | 8 | Absent |
| Saint Bernard | M | 5 | Lower left eyelid | Meibomian gland adenoma | 6 | Absent |
| Siberian Husky | M | 8 | Upper right eyelid | Meibomian gland epithelioma | 8 | Absent |
| Springer Spaniel | M | 6 | Lower right eyelid | Papilloma | 7 | Absent |
| Yorkshire | F | 10 | Upper left eyelid | Meibomian gland adenoma | 7 | Absent |
| Yorkshire | M | 8 | Lower left eyelid | Papilloma | 6 | Absent |
| Yorkshire | M | 7 | Upper left eyelid | Meibomian gland epithelioma | 9 | Absent |
| Breed | Sex | Age | Localization of the Tumour | Type of Tumour | Duration of Surgery | Bleeding Degree |
|---|---|---|---|---|---|---|
| German Shepherd | M | 6 | Lower left eyelid | Melanoma | 7 | Absent |
| Golden Retriever | M | 6 | Lower left eyelid | Melanoma | 6 | Absent |
| Labrador Retriever | F | 7 | Left third eyelid | Pleomorphic carcinoma | 6 | Mild |
| Labrador Retriever | M | 4 | Lower right eyelid | Melanoma | 7 | Absent |
| Mixed | M | 10 | Left third eyelid | Ductal carcinoma | 8 | Absent |
| Mixed | F | 10 | Upper right eyelid | Meibomian gland adenocarcinoma | 6 | Mild |
| Mixed | M | 8 | Right third eyelid | Pleomorphic carcinoma | 7 | Mild |
| Rottweiler | M | 5 | Lower right eyelid | Melanoma | 7 | Absent |
| Yorkshire | F | 6 | Upper left eyelid | Meibomian gland adenocarcinoma | 6 | Mild |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Navas, L.; Di Palma, C.; Pasolini, M.P.; Montano, C.; de Chiara, M.; Lamagna, F.; Uccello, V.; Micieli, F.; Amalfitano, C.; Paciello, O.; et al. Outcomes of Treatment of Eyelids and Third Eyelid Tumours in Dogs Using High-Frequency Radiowave Surgery. Animals 2023, 13, 2105. https://doi.org/10.3390/ani13132105
Navas L, Di Palma C, Pasolini MP, Montano C, de Chiara M, Lamagna F, Uccello V, Micieli F, Amalfitano C, Paciello O, et al. Outcomes of Treatment of Eyelids and Third Eyelid Tumours in Dogs Using High-Frequency Radiowave Surgery. Animals. 2023; 13(13):2105. https://doi.org/10.3390/ani13132105
Chicago/Turabian StyleNavas, Luigi, Cristina Di Palma, Maria Pia Pasolini, Chiara Montano, Mariaelena de Chiara, Francesco Lamagna, Valeria Uccello, Fabiana Micieli, Claudia Amalfitano, Orlando Paciello, and et al. 2023. "Outcomes of Treatment of Eyelids and Third Eyelid Tumours in Dogs Using High-Frequency Radiowave Surgery" Animals 13, no. 13: 2105. https://doi.org/10.3390/ani13132105
APA StyleNavas, L., Di Palma, C., Pasolini, M. P., Montano, C., de Chiara, M., Lamagna, F., Uccello, V., Micieli, F., Amalfitano, C., Paciello, O., & Lamagna, B. (2023). Outcomes of Treatment of Eyelids and Third Eyelid Tumours in Dogs Using High-Frequency Radiowave Surgery. Animals, 13(13), 2105. https://doi.org/10.3390/ani13132105






