Abstract
Persistent infection is a characteristic feature of babesiosis, a worldwide, emerging tick-borne disease caused by members of the genus Babesia. Persistence of Babesia infection in reservoir hosts increases the probability of survival and transmission of these pathogens. Laboratory tools to detect Babesia in red blood cells include microscopic detection using peripheral blood smears, nucleic acid detection (polymerase chain reaction and transcription mediated amplification), antigen detection, and antibody detection. Babesia microti, the major cause of human babesiosis, can asymptomatically infect immunocompetent individuals for up to two years. Chronically infected blood donors may transmit the pathogen to another person through blood transfusion. Transfusion-transmitted babesiosis causes severe complications and death in about a fifth of cases. Immunocompromised patients, including those with asplenia, HIV/AIDS, malignancy, or on immunosuppressive drugs, often experience severe disease that may relapse up to two years later despite anti-Babesia therapy. Persistent Babesia infection is promoted by Babesia immune evasive strategies and impaired host immune mechanisms. The health burden of persistent and recrudescent babesiosis can be minimized by development of novel therapeutic measures, such as new anti-parasitic drugs or drug combinations, improved anti-parasitic drug duration strategies, or immunoglobulin preparations; and novel preventive approaches, including early detection methods, tick-avoidance, and blood donor screening.
Keywords:
Babesia; Babesia microti; persistence; recurrence; Plasmodia; malaria; spleen; blood transfusion 1. Introduction
Babesia are intraerythrocytic protozoa in the same Apicomplexa phylum as Plasmodia. They are transmitted worldwide by hard-bodied ticks and infect a wide variety of wild and domestic animals. Several Babesia species have been found to infect humans, the most important of which is Babesia microti, which is endemic in the Northeastern and northern Midwestern United States [1]. The number of cases and geographic range of B. microti have increased over the past two decades in endemic areas. About 2000 cases of B. microti are reported each year but epidemiologic studies suggest that the actual number of cases is much greater [1,2,3]. B. microti also can be transmitted through blood transfusion, organ transplantation, and perinatally [1,4]. It causes a malaria-like illness that is fatal in about 20% of immunocompromised hosts and those who acquire the infection through blood transfusion.
Persistent infection is a characteristic feature of babesiosis and malaria, the two primary intraerythrocytic protozoal diseases of humans [5,6,7,8,9]. Both depend on an arthropod vector to transmit infection from other humans (Plasmodia) or animal hosts (Babesia). Persistence of infection in the reservoir host increases the probability of transmission and survival of these pathogens [6]. Chronic malaria infection has long been recognized. Recrudescence of Plasmodium vivax and Plasmodium ovale infections have been reported more than two and four years after initial infection, respectively [8]. Human babesiosis also has been documented to persist and recrudesce. Among immunocompetent hosts, Babesia microti parasitemia (DNA) has been detected for more than a year in patients treated with a standard course of antibiotic therapy and more than two years in untreated individuals [10,11]. Immunocompromised patients can experience persistent B. microti parasitemia and relapsing symptoms for more than two years despite antimicrobial therapy [12,13]. Both Plasmodia and Babesia reside within red blood cells, which are somewhat impervious to immune attack. Furthermore, P. ovale and P. vivax also sequester within liver cells during the hypnozoite stage of the life cycle. In this paper, we will focus on persistence of B. microti infection, the most common cause of babesiosis in humans. We will examine laboratory tools that have been used to document persistence of Babesia infection (including blood smear, PCR, animal inoculation, and antibody), asymptomatic and symptomatic persistence of infection following tick-transmitted infection, asymptomatic persistence of infection in blood donors, and mechanisms of Babesia persistence.
2. Babesia microti Detection Tools
The diagnosis of babesiosis should be considered in anyone who resides in or travels to a Babesia endemic area or has received a blood transfusion within the previous six months and has typical clinical symptoms, such as fever, fatigue, malaise, weakness, chills, sweats, and headache. The diagnosis is confirmed through identification of Babesia on microscopic examination of Wright or Giemsa-stained thin blood-film or detection of Babesia nucleic acid using such methods as polymerase chain reaction (PCR) (Figure 1) [1,14,15]. Babesia and Plasmodium falciparum are morphologically similar on microscopic examination. Features that help to discriminate between the two include the lack of hemozoin pigment deposits and the presence of tetrad or “Maltese cross” forms in Babesia-infected erythrocytes. The latter are rarely seen but when identified are pathognomonic for Babesia infection. The sensitivity of blood-film microscopy for Babesia detection is about 85%, while specificity approaches 100% [15,16]. Review of multiple thick and thin-blood films increases sensitivity of microscopic detection. Microscopy is suboptimal for the detection of low-level parasitemia as occurs both in early and long-term chronic infection and is therefore not considered an effective tool for epidemiological and surveillance purposes.
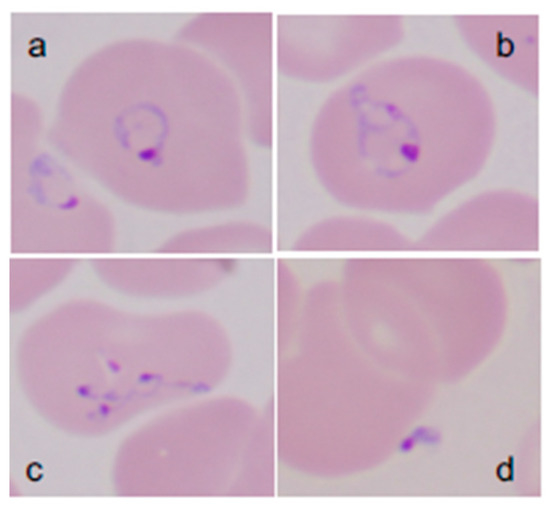
Figure 1.
Giemsa-stained thin blood films showing Babesia microti parasites.B. microti are obligate parasites of erythrocytes. Trophozoites may appear as ring forms (A) or as ameboid forms (B). Merozoites can be arranged in tetrads and are pathognomonic (C). Extracellular parasites can be noted, particularly when the parasitemia level is high (D). (Adapted from [1]).
Nucleic acid detection offers a better correlate of active infection. Nucleic acid detection based tests (NAT), such as polymerase chain reaction (PCR) and transcription-mediated amplification (TMA), more effectively identify low-level infections than other laboratory tests [15,16,17,18,19]. The molecular methods for Babesia detection generally rely on amplification of the 18S gene, which encodes the small subunit ribosomal RNA gene. Publication of the full B. microti genome in 2012 has enabled identification of higher copy number detection targets, allowing the routine detection of less than 10 B. microti parasites per ml of blood [18,20]. Additional technological advances such as sample concentration, high copy detection targets such as BMN multigene family members, and bead-based target capture may further enhance the sensitivity of NAT assays [21,22]. Detection of Babesia antigen(s) offers additional markers of active infection. Efforts should be made to identify excreted/secreted B. microti antigen to develop high throughput detection assays for diagnostic and donor screening purposes [18,22]. Inoculation of patient blood into small mammals such as hamsters, gerbils, or SCID mice for detection of Babesia is less sensitive than PCR and impractical but is useful for investigation of rare variants/strains of Babesia and for blood donor studies [15].
Antibodies are the most reliable marker of past exposure to the Babesia parasite. The indirect fluorescent antibody (IFA) assay is the most commonly used Babesia antibody test, which utilizes the whole parasite as an antigen source [15,23]. The CDC defines a Babesia laboratory supportive antibody test result as an IFA total immunoglobulin or IgG antibody titer of ≥1:256 (or ≥1:64 in epidemiologically linked blood donors or recipients) [24]. An enzyme-linked immunosorbent assay (ELISA) test also has been developed for detection of antibodies to the immunodominant B. microti antigens BMN-9 and BMN-17 [25]. A commercial ELISA based on the synthetic peptides representing these antigens was used for screening blood donors for anti-B. microti antibodies in investigational studies [26,27]. Recent advances, which include genomics-based approaches for antigen discovery, bead particle-based antigen multiplexing, and application of nanotechnology, are all anticipated to improve the sensitivity of Babesia antibody-based assays [28,29]. A major limitation of antibody-based assays is that a single antibody result fails to distinguish between present (active) and past (resolved) infection, although a B. microti IgG antibody titer of ≥1:1024 or the presence of IgM antibody suggest recent infection [30,31]. A four-fold rise in Babesia antibody confirms recent infection but is impractical because convalescent sera must be obtained at least two to three weeks after sera is first obtained during acute illness (acute sera). Identification of antigens that could distinguish between active and resolved infections would greatly enhance the utility of antibody-based assays for Babesia diagnosis.
3. Persistent Babesia microti Infection in Immunocompetent and Immunocompromised Hosts
Persistent Babesia infection was first reported in an immunocompetent 59-year-old woman who contracted the infection on Nantucket, Massachusetts [32]. She experienced Babesia symptoms for three weeks and B. microti parasites continued to be detected on blood smear for more than four months after symptoms resolved. The first prospective study of persistent babesiosis was carried out in 46 residents of southern New England [10]. Blood samples were obtained from patients during acute infection and every three months thereafter for amplification of B. microti DNA using PCR. Asymptomatic parasitemia was shown to last more than a year in a few patients, despite treatment with clindamycin and quinine. Asymptomatic infection persisted even longer in a group of patients who had mild or subclinical B. microti infection and were not treated because of concern about side effects of clindamycin and quinine. One untreated patient had persistence of infection and recrudescence of symptoms 27 months after diagnosis [6]. Similar results were noted in another study of 56 asymptomatically infected blood donors (Figure 2) [11].
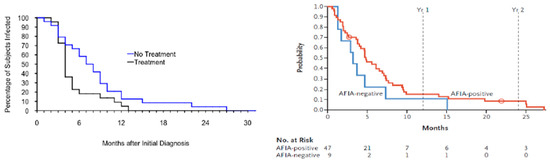
Figure 2.
Persistence of B. microti infection.Left panel. Persistence of Babesia microti DNA in humans following acute babesiosis. Blood samples from patients experiencing acute babesiosis were tested for B. microti DNA using PCR every three months following the onset of infection until DNA was no longer detectable. Panel shows the Kaplan–Meier estimate of the survival function modeling the time to the first PCR-negative follow-up sample among study subjects with B. microti infection (adapted from [10]). Right panel. This panel shows the Kaplan–Meier estimate of the survival function modeling the time to the first PCR-negative follow-up sample in blood donors whose samples were PCR positive for B. microti on the index blood donation sample. The results of two groups are shown, those that were Babesia antibody positive as determined by AFIA (semi-automated arrayed fluorescent immunoassay) and those who were Babesia antibody negative (adapted from [11]).
Prolonged Babesia disease has been described in immunocompromised hosts, with relapsing symptoms lasting up to nine months and parasitemia continuing for more than a year [33,34,35,36]. These patients were markedly immunocompromised given underlying diagnoses that included HIV/AIDS, malignancy, and asplenia. A retrospective case series of consecutively enrolled babesiosis patients who failed to respond to standard anti-Babesia antibiotic therapy also demonstrated that patients with these immunosuppressive conditions experienced persistent and relapsing babesiosis [12]. Interestingly, 10 of the 14 patients in this series suffered from B cell lymphoma and had been treated with Rituximab, an anti-B cell monoclonal antibody. These data suggest that an impaired anti-Babesia antibody response, in the context of generalized immunosuppression, prevents clearance of B. microti infection. Long term antibiotic therapy of at least six weeks, rather than the standard 7 to 10 days, was required to resolve infection in these severely immunocompromised patients [12]. Severe and persistent B. microti infection also has been associated with advanced age in a mouse model and in humans [1,36,37].
4. Persistent Babesia microti infection in Asymptomatic Immune-Intact Blood Donors
Babesia can be transmitted through blood transfusion and has long been recognized as a leading infectious risk to the blood supply in the United States, particularly in parts of the Northeast and Upper Midwestern states where B. microti is endemic [38]. To date over 200 cases of transfusion-transmitted babesiosis (TTB) have been described [39], the overwhelming majority of which have been caused by B. microti [4]. In addition, rare cases of TTB have been attributed to other species (e.g., Babesia duncani) [40] and variant Babesia strains [41]. While Babesia species are globally ubiquitous, findings from the few studies outside of the US that have investigated blood donors have failed to match the scale encountered here [1,42,43,44].
Babesia is transmissible through any red blood cell containing blood product, including packed red blood cells (RBCs), whole blood, and whole blood-derived platelets [4,45]. Findings from a murine model suggest that as few as 10 to 100 RBCs are needed to establish host infection [46]. Transfusion recipients are at high risk for severe or complicated disease. For one, there is overrepresentation of vulnerable patient subsets among transfusion recipients such as those at extremes of age, those with asplenia, or those who have just undergone surgery. Furthermore, the primary indication for red blood cell transfusions is anemia, which exacerbates underlying disease and compounds the risk of complications. Such is reflected by the high fatality rate of TTB (19%) [4].
Unlike natural (i.e., tick-borne) acquisition, TTB is not strictly seasonal. Prolonged storage of blood components enables transfusion of parasitemic blood long after blood donation. In addition, the incubation period for development of symptoms after transfusion is as long as six months. TTB is also not geographically bound, given that blood donors from non-endemic areas may travel to endemic areas where they can acquire the infection through tick bite, return to the non-endemic area and donate infectious blood. Finally, blood that is collected in endemic states is frequently shipped to states that are not considered high risk for babesiosis, also accounting for cases of TTB in non-endemic states [47,48,49].
The risk of TTB is greatly increased by persistent asymptomatic parasitemia in blood donors [11,50,51,52]. Blood donors are an invaluable resource to study the kinetics of Babesia infection in healthy individuals. The donation process itself selects for asymptomatic individuals. Those with high parasitemia would be expected to manifest symptoms, and either self-defer from blood donation or be deemed ineligible given detectable fever, low hemoglobin and/or abnormal vital signs that would likely be detected during pre-donation screening. Historically, individuals who reported a history of babesiosis were permanently deferred from blood donation, further emphasizing that donors are typically unaware of prior and/or ongoing Babesia infection at the time of donation.
Recognition of risk to the US blood supply spurred a series of studies to characterize the burden and immunopathogenesis of Babesia in blood donors. These studies revealed a high B. microti seroprevalence in endemic areas (up to 2.5% in parts of Connecticut) with molecular (PCR) evidence of infection in up to a half of seropositive donors [3,19].
About a fifth (21%) of 84 seropositive blood donors (IFA titers ≥64), who were followed for up to three years in Connecticut and Massachusetts were found to be parasitemic [50]. Over the course of follow-up, protracted low-level parasitemia was variably and intermittently detectable. One subject was found to be parasitemic on initial screening and then again 13 months later, as shown by hamster inoculation. Those who were parasitemic were similar with respect to demographic and geographic characteristics to those who were not, but displayed higher Babesia IFA antibody titers in aggregate (median IFA titer ≥256 vs. ≥64).
Development of blood donor screening assays, which began in the mid-to-late 2000s, largely through partnerships between small businesses and the major blood collection agencies in the US, expanded testing capacity and further enabled the study of Babesia kinetics in the donor population. In one study over a two-year period (June 2012–September 2014), a total of 89,153 blood-donation samples were tested with a semi-automated arrayed fluorescent immunoassay (AFIA), together with a PCR assay. A total of 335 (0.38%) samples were shown to be seroreactive by AFIA, 67 (20%) of which were also PCR positive [52] (Figure 1). Furthermore, 1 per 9906 screened samples was seronegative but PCR positive. Approximately a third of the red blood cell samples from PCR positive or high-titer AFIA seroreactive donations resulted in infection following inoculation into hamsters. After a year of follow-up, DNA persistence based on PCR was noted in 14% of the donors. In contrast, 92% of donors displayed evidence of antibody persistence.
During validation studies of a new B. microti enzyme-linked immunoassay (ELISA) in 15,000 blood donors, the investigators reported 1.08% seroreactivity in those residing in a highly endemic area (Long Island, NY) [22]. In a subsequent study in which blood donors were prospectively tested, seroreactivity in donors from moderately to highly Babesia-endemic counties of New York was considerably lower (0.28%, 38/13,757) [23]. A subset (37/60) of seroreactive donors were prospectively followed for at least 12 months following donation, 20 of 37 (54%) completed the 12-month follow-up visit of whom 15 (75%) were still seroreactive [19]. Nine donors were identified as being PCR-positive during index screening. Of the five donors who participated in the follow-up study, three were PCR positive at six months, and two remained positive at final follow-up at 12 months (378- and 404-day post-index donation). Seropositive donors were questioned whether they had experienced symptoms or signs of Babesia infection in the three months prior to donation. Few reported symptoms or signs that were consistent with babesiosis.
In 2019, the US Federal Drug Administration (FDA) published a guidance for industry that included a non-binding recommendation to perform regional nucleic acid testing (NAT) in 15 high-risk states using licensed assays [53]. At the time of the recommendation, NAT (PCR and transcription mediated amplification) assays had already been licensed for donor screening. NAT has shown high sensitivity and specificity with limits of detection for Babesia as low as two to three parasites/mL [54]. The guidance also allows for requalification of those donors who are deferred for a history of babesiosis or positive Babesia test result after two years of negative testing. Experimental molecular [17,18] and commercial antibody-based assays [55] have also been developed that could have utility in donor screening.
In summary, studies of transfusion-transmitted babesiosis highlight persistence of B. microti infection with few discernible clinical effects in infected blood donors. Asymptomatic, intermittent and low-level parasitemia can occasionally persist for more than two years.
5. Mechanisms of Babesia Persistence
Currently there is a limited understanding of the immune mechanisms that mitigate the severity and duration of Babesia infection, however, existing data indicate that innate and adaptive immune mechanisms are able to clear the infection without antimicrobial therapy in the majority of immune competent individuals [10,11,36]. A putative immunological model can be deduced from human and animal studies, and from a review of the large body of work on malaria immunology.
The initial immunological barrier that Babesia encounter after transmission to a human host is the spleen. Individuals who lack a spleen and become infected with Babesia generally experience severe infection, which is associated with a high fatality rate [1,5,10,56,57,58]. Many of the earliest reported cases of babesiosis involved asplenic individuals because the severity of those infections prompted a comprehensive diagnostic evaluation. This led to the discovery of Babesia parasites during microscopic evaluation of thin blood smears. Dr. Jane Deforges wrote an editorial in 1957 after cases were first described on Nantucket Island (babesiosis was initially known as Nantucket fever), suggesting that those who were asplenic should avoid travel to the Island [59]. Today this admonition would need to include large areas of the Northeast and northern Midwest. Numerous subsequent reports, including both human and animal studies, have demonstrated that the spleen plays a crucial role in the immune response to Babesia infection [1,5,57,58,60,61]. After Babesia parasites are introduced into the bloodstream following a tick bite, they enter the spleen through the splenic artery, course through the white pulp and empty into the marginal zone blood vessels or the vascular tufts and sinuses in the red pulp (Figure 3). The marginal zone contains macrophages and neutrophils that recognize and ingest Babesia-infected red blood cells and circulating Babesia parasites. In the red pulp, Babesia-infected red blood cells are captured in sieve-like slits in the sinuses as they return to the main circulation and are ingested by macrophages [1,5]. The white pulp of the spleen contains T cells that produce cytokines such as gamma interferon (IFNγ), which enhance macrophage destruction of Babesia and activate B cells to secrete Babesia-specific antibody.
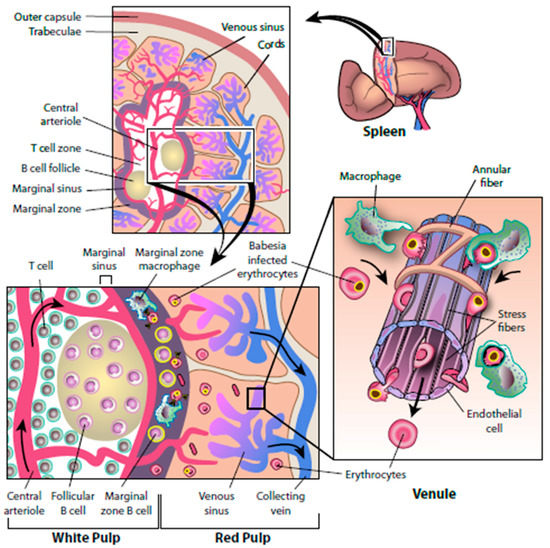
Figure 3.
The splenic response to Babesia infection. The following composite model is based on studies of Babesia infection in natural vertebrate hosts and animal models. The spleen is a heavily vascularized organ (top left panel) that consists of red-pulp zones and white pulp zones surrounded by a trabecula and an outer capsule. A circulating erythrocyte travels through the spleen approximately once every 20 min. Erythrocytes enter the spleen by means of the trabecular artery and flow into central arteries and follicular arterioles to reach the marginal sinus of the white pulp. Once in the adjacent marginal zone, Babesia-infected erythrocytes are ingested and destroyed by resident dendritic cells and macrophages. Marginal-zone macrophages do not express major histocompatibility complex (MHC) class II molecules but shed pathogen-degradation products that are picked up by marginal-zone B cells. Activated marginal-zone B cells and dendritic cells move to the T-cell zones, where they present antigen to T cells. Activated T cells migrate to the edge of the follicles and engage B cells, causing them to activate and eventually differentiate into antibody-secreting cells. Opsonization of Babesia-infected erythrocytes by antibody promotes their clearance by phagocytes. Activated T cells also produce interferon-γ, the prototypic cytokine that helps macrophages kill ingested pathogens. Blood may bypass the white pulp and reach the red pulp directly. In the splenic cords of the red pulp, blood cells slowly flow between reticular fibers and are sensed by resident macrophages. Babesia-infected erythrocytes squeeze with difficulty through the apertures of the endothelium lining and are ingested by resident macrophages of the cords. Stress fibers that run longitudinally at the base of the endothelial cell lining and connect to annular fibers can contract and loosen, thereby regulating the flow and size of erythrocytes that reach the venous sinuses. Blood cells that access the venous sinuses flow into venules and eventually reach the collecting vein. (Adapted from [1]).
As with other aspects of Babesia immunity, much can be deduced from studies of malaria immunity. Antibody has been shown to be crucial in reducing malaria parasite load, thereby limiting the severity of disease and helping to prevent subsequent malarial infection. There are thousands of malaria strains so that sterilizing immunity can be achieved against a specific strain but not all strains [7]. Partial immunity from cross-reacting antibody can limit the severity of infection of most malaria strains. People living in malaria-endemic areas generally experience multiple malarial infections, but the disease becomes less severe over time. There is good evidence that antibody is also important in limiting and clearing Babesia infection, at least in immunocompromised individuals [12,34]. Patients with B cell lymphoma and/or Rituximab therapy have impaired antibody responses and were found to have a prolonged relapsing clinical course despite antimicrobial therapy [12,62]. Antibody clears infection through neutralization by blocking pathogen entry into red blood cells, enhances opsonization of parasites by macrophages and neutrophils, eradicates pathogens through antibody-dependent cytotoxicity by natural killer cells, and activates complement.
Babesia parasites employ a number of evasive measures to avoid an immune attack, which leads to persistent B. microti infection, even when immune function is intact [6]. For one, the invasion of red blood cells limits pathogen exposure. Secondly, expression of Plasmodia and Babesia-induced adhesion molecules on the red blood cell surface have been identified that cause adherence of parasite-infected erythrocytes to vascular endothelium [5,6,63]. As a result, parasites can complete their entire life cycle and invade other erythrocytes without ever circulating through the spleen. The importance of this mechanism is emphasized by the production of antibody against these adherence proteins, which block their action. Great variability exists among the genes that encode these proteins. Antibody directed against one type of adherence protein may be ineffective in blocking a second type of adherence protein. Parasite-induced adherence proteins have been identified for several Babesia species, including Babesia bovis in cattle, although they have yet to be demonstrated for B. microti [6,63,64]. Babesia also can develop resistance to antiparasitic drugs, including the two standard combinations of atovaquone and azithromycin and clindamycin and quinine. The molecular origin of B. microti resistance to atovaquone and to azithromycin have been identified as genetic mutations in certain Babesia strains, which alter the microbial protein targets of the drugs These targets are the cytochrome b protein in the Babesia mitochondrial electron transport chain for atovaquone and the apicoplast protein, which inhibits protein translation in this organelle for azithromycin. Atovaquone and azithromycin cannot effectively bind and inhibit the growth of these strains [65,66].
Cytokines are another immune component that is thought to play an important role in protecting against Babesia infection. They are small signaling molecules of critical importance in normal immune function and other biological processes [67]. Hundreds of different cytokines are secreted by immune and non-immune cells. Cytokines can stimulate or inhibit cell differentiation and proliferation, cell activation, cell migration, and cell survival. Proinflammatory cytokine release helps activate the immune response to eradicate Babesia [68,69]. An impaired cytokine response would likely facilitate persistence of B. microti infection, although there is no data to support this possibility. Paradoxically, an excessive cytokine response is thought to enhance disease and contribute to complications and death [5,69,70]. A good example is the apparent cytokine-induced pulmonary edema and death following B. duncani infection in hamsters. B.duncani infected hamsters uniformly have elevated lung concentrations of TNFα and IFNγ. In contrast, B. microti infection elicits a mild clinical response in hamsters, and pulmonary TNFα and IFNγ are not upregulated. Further studies of the role of cytokines in the persistence of Babesia infections in humans are needed.
6. Conclusions
- Persistence of Babesia infection in mammalian hosts is an important characteristic of these parasites that maximizes the probability of transmission between vector and host.
- Asymptomatic persistence of Babesia infection in blood donors increases the probability of transmission to blood transfusion recipients.
- Persistent asymptomatic Babesia infection in blood donors is being addressed through implementation of blood donor screening.
- Symptomatic persistence of Babesia infection in immunocompromised hosts increases the probability of disease complications and death.
- The health burden of persistent and recrudescent babesiosis can be minimized by development of novel therapeutic measures, such as new antiparasitic drugs or drug combinations, improved antiparasitic drug duration strategies, or immunoglobulin preparations; and novel preventive approaches, including early detection methods, tick-avoidance, and blood donor screening.
Author Contributions
Each author has made substantial contributions to the design of the work and has helped draft the work and substantively revised it, and has approved the submitted version (and the version substantially edited by journal staff that involves the author’s contribution to the study), and agrees to be personally accountable for the author’s own contributions and for ensuring that questions related to the accuracy or integrity of any part of the work.
Funding
This research was funded by the Gordon and Llura Gund Foundation
Acknowledgments
We thank Wendy Hill for help with the illustrations and Francesica Tizzard with technical assistance.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Vannier, E.; Krause, P.J. Human Babesiosis. N. Engl. J. Med. 2012, 66, 2397–2407. [Google Scholar] [CrossRef] [PubMed]
- Krause, P.J.; McKay, K.; Gadbaw, J.; Christianson, D.; Closter, L.; Lepore, T.; Telford, S.R., 3rd; Sikand, V.; Ryan, R.; Persing, D.; et al. Increasing health burden of human babesiosis in endemic sites. Am. J. Trop. Med. Hyg. 2003, 68, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Leiby, D.A.; Chung, A.P.; Gill, J.E.; Houghton, R.L.; Persing, D.H.; Badon, S.; Cable, R.G. Demonstrable parasitemia among Connecticut blood donors with antibodies to Babesia microti. Transfusion 2005, 45, 1804–1810. [Google Scholar] [CrossRef] [PubMed]
- Herwaldt, B.L.; Linden, J.V.; Bosserman, E.; Young, C.; Olkowska, D.; Wilson, M. Transfusion-associated babesiosis in the United States: A description of cases. Ann Intern Med. 2011, 155, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Krause, P.J.; Daily, J.; Telford, S.R.; Vannier, E.; Lantos, P.; Spielman, A. Shared features in the pathobiology of babesiosis and malaria. Trends Parasitol. 2007, 23, 605–610. [Google Scholar] [CrossRef] [PubMed]
- Allred, D.R. Babesiosis: Persistence in the face of adversity. Trends Parasitol. 2003, 19, 51–55. [Google Scholar] [CrossRef]
- White, N.J. Determinants of relapse periodicity in Plasmodium vivax malaria. Malar. J. 2011, 10, 297. [Google Scholar] [CrossRef]
- Trager, W.; Most, H. A long-delayed primary attack of Ovale malaria. Am. J. Trop. Med. Hyg. 1963, 12, 837–839. [Google Scholar] [CrossRef]
- Suarez, C.E.; Alzan, H.F.; Silva, M.G.; Rathinasamy, V.; Poole, W.A.; Cooke, B.M. Unravelling the cellular and molecular pathogenesis of bovine babesiosis: Is the sky the limit? Int. J. Parasitol. 2019, 49, 183–197. [Google Scholar] [CrossRef]
- Krause, P.J.; Spielman, A.; Telford, S.; Sikand, V.J.; McKay, K.; Christianson, D.; Pollack, R.; Brassard, P.; Magera, J.; Ryan, R.; et al. Persistent parasitemia following acute babesiosis. N. Engl. J. Med. 1998, 339, 160–165. [Google Scholar] [CrossRef]
- Moritz, E.; Winton, C.S.; Tonnetti, L.; Townsend, R.L.; Berardi, V.P.; Hewins, M.E.; Weeks, K.E.; Dodd, R.Y.; Stramer, S.L. Screening for Babesia microti in the US blood supply. N. Engl. J. Med. 2016, 375, 2236–2245. [Google Scholar] [CrossRef] [PubMed]
- Krause, P.J.; Gewurz, B.E.; Hill, D.; Marty, F.M.; Vannier, E.; Foppa, I.M.; Furman, R.R.; Neuhaus, E.; Skowron, G.; Gupta, S.; et al. Persistent and relapsing babesiosis in immunocompromised patients. Clin. Infect. Dis. 2008, 46, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Raffalli, J.; Wormser, G.P. Persistence of babesiosis for >2 years in a patient on Rituximab for rheumatoid arthritis. Diag. Microbiol. Infect. Dis. 2016, 85, 231–232. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention, DPDx- Laboratory Identification of Parasites of Public Health Concern. Available online: https://www.cdc.gov/dpdx/babesiosis/index.html (accessed on 12 July 2019).
- Krause, P.J.; Telford, S.; Spielman, A.; Ryan, R.; Magera, J.; Rajan, T.V.; Christianson, D.; Alberghini, T.V.; Bow, L.; Persing, D. Comparison of PCR with blood smear and small animal inoculation for diagnosis of Babesia microti parasitemia. J. Clin. Microbiol. 1996, 34, 2791–2794. [Google Scholar] [PubMed]
- Wang, G.; Villafuerte, P.; Zhuge, J.; Visintainer, P.; Wormser, G.P. Comparison of a quantitative PCR assay with peripheral blood smear examination for detection and quantitation of Babesia microti infection in humans. Diagn. Microbiol. Infect. Dis. 2015, 82, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Bloch, E.M.; Lee, T.H.; Krause, P.J.; Telford, S.R., 3rd; Montalvo, L.; Chafets, D.; Usmani-Brown, S.; Lepore, T.J.; Busch, M.P. Development of a real-time polymerase chain reaction assay for sensitive detection and quantitation of Babesia microti infection. Transfusion 2013, 53, 2299–2306. [Google Scholar] [PubMed]
- Grabias, B.; Clement, J.; Krause, P.J.; Lepore, T.; Kumar, S. Superior real-time polymerase chain reaction detection of Babesia microti parasites in whole blood utilizing high-copy BMN antigens as amplification targets. Transfusion 2018, 58, 1924–1932. [Google Scholar] [CrossRef]
- Johnson, S.T.; Van Tassell, E.R.; Tonnetti, L.; Cable, R.G.; Berardi, V.P.; Leiby, D.A. Babesia microti real-time polymerase chain reaction testing of Connecticut blood donors: Potential implications for screening algorithms. Transfusion 2013. [Google Scholar] [CrossRef]
- Cornillot, E.; Hadj-Kaddour, K.; Dassouli, A.; Noel, B.; Ranwez, V.; Vacherie, B.; Augagneur, Y.; Brès, V.; Duclos, A.; Randazzo, S.; et al. Sequencing of the smallest Apicomplexan genome from the human pathogen Babesia microti. Nucleic Acids Res. 2012, 40, 9102–9114. [Google Scholar] [CrossRef]
- Thekkiniath, J.; Mootien, S.; Lawres, L.; Perrin, B.A.; Gewirtz, M.; Krause, P.J.; Williams, S.; Doggett, J.S.; Ledizet, M.; Ben Mamoun, C. BmGPAC, an antigen capture assay for detection of active Babesia microti infection. J Clin Microbiol. 2018, 25, 56. [Google Scholar] [CrossRef]
- Elton, C.M.; Rodriguez, M.; Ben Mamoun, C.; Lobo, C.A.; Wright, G.J. A library of recombinant Babesia microti cell surface and secreted proteins for diagnostics discovery and reverse vaccinology. Int. J. Parasitol. 2019, 49, 115–125. [Google Scholar] [CrossRef] [PubMed]
- Krause, P.J.; Telford, S.; Ryan, R.; Conrad, P.A.; Conrad, M.; Wilson, M.; Thomford, J.W.; Spielman, A. Diagnosis of babesiosis: Evaluation of a serologic test for the detection of Babesia microti antibody. J. Inf. Dis. 1994, 169, 923–926. [Google Scholar] [CrossRef] [PubMed]
- Gray, E.B.; Herwaldt, B.L. Babesiosis Surveillance—United States, 2011–2015. MMWR Surveill Summ 2019, 68, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Priest, J.W.; Moss, D.M.; Won, K.; Todd, C.W.; Henderson, L.; Jones, C.C.; Wilson, M. Multiplex assay detection of immunoglobulin G antibodies that recognize Babesia microti antigens. Clin. Vacc. Immunol. 2012, 19, 1539–1548. [Google Scholar] [CrossRef] [PubMed]
- Levin, A.E.; Williamson, P.C.; Erwin, J.L.; Cyrus, S.; Bloch, E.M.; Shaz, B.H.; Kessler, D.; Telford, S.R., 3rd; Krause, P.J.; Wormser, G.P.; et al. Determination of Babesia microti seroprevalence in blood donor populations using an investigational enzyme immunoassay. Transfusion 2014, 54, 2237–2244. [Google Scholar] [CrossRef] [PubMed]
- Levin, A.E.; Williamson, P.C.; Bloch, E.M.; Clifford, J.; Cyrus, S.; Shaz, B.H.; Kessler, D.; Gorlin, J.; Erwin, J.L.; Krueger, N.X.; et al. Serologic screening of United States blood donors for Babesia microti using an investigational enzyme immunoassay. Transfusion 2016, 56, 1866–1874. [Google Scholar] [CrossRef] [PubMed]
- Hockman, D.; Dong, M.; Zheng, H.; Kumar, S.; Huff, M.D.; Grigorenko, E.; Beanan, M.; Duncan, R. Comparison of multiplex PCR hybridization-based and singleplex real-time PCR-based assays for detection of low prevalence pathogens in spiked samples. J. Microbiol. Methods 2017, 132, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Magni, R.; Luchini, A.; Liotta, L.; Molestina, R.E. Analysis of the Babesia microti proteome in infected red blood cells by a combination of nanotechnology and mass spectrometry. Int. J. Parasitol. 2019, 49, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Ruebush, T.K.; Chisholm, E.S.; Sulzer, A.J.; Healy, G.R. Development and persistence of antibody in persons infected with Babesia microti. Am. J. Trop. Med. Hyg. 1981, 30, 291–292. [Google Scholar] [CrossRef]
- Krause, P.J.; Ryan, R.; Telford, S.; Persing, D.; Spielman, A. Efficacy of an IgM serodiagnostic test for the rapid diagnosis of acute babesiosis. J. Clin. Microbiol. 1996, 34, 2014–2016. [Google Scholar]
- Western, K.A.; Benson, G.D.; Gleason, N.N.; Healy, G.R.; Schultz, M.G. Babesiosis in a Massachusetts resident. N. Engl. J. Med. 1970, 283, 854–856. [Google Scholar] [CrossRef] [PubMed]
- Falagas, M.E.; Klempner, M.S. Babesiosis in patients with AIDS: A chronic infection presenting as fever of unknown origin. Clin. Infect. Dis. 1996, 22, 809–812. [Google Scholar] [CrossRef] [PubMed]
- Haselbarth, K.; Tenter, A.M.; Brade, V.; Krieger, G.; Hunfeld, K.P. First case of human babesiosis in Germany—Clinical presentation and molecular characterization of the pathogen. Int. J. Med. Microbiol. 2007, 297, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Stowell, C.P.; Gelfand, J.A.; Shepard, J.O.; Kratz, A. Case 17–2007—A 25- year-old woman with relapsing fevers and recent onset of dyspnea. N. Engl. J. Med. 2007, 356, 2313–2319. [Google Scholar] [CrossRef] [PubMed]
- Vannier, E.; Borggraefe, I.; Telford, S.R.; Menon, S.; Brauns, T.; Spielman, A.; Gelfand, J.A.; Wortis, H.H. Age-associated decline in resistance to Babesia microti is genetically determined. J. Infect. Dis. 2004, 189, 1721–1728. [Google Scholar] [CrossRef]
- Mareedu, N.; Schotthoefer, A.M.; Tomkins, J.; Hall, M.C.; Fritsche, T.R.; Frost, H.M. Risk factors for severe infection, hospitalization, and prolonged antimicrobial therapy in patients with babesiosis. Am. J. Trop. Med. Hyg. 2017, 97, 1218–1225. [Google Scholar] [CrossRef] [PubMed]
- Leiby, D.A. Transfusion-transmitted Babesia spp.: bull’s-eye on Babesia microti. Clin. Microbiol. Rev. 2011, 24, 14–28. [Google Scholar] [CrossRef]
- Tonnetti, L.; Townsend, R.L.; Deisting, B.M.; Haynes, J.M.; Dodd, R.Y.; Stramer, S.L. The impact of Babesia microti blood donation screening. Transfusion 2019, 59, 593–600. [Google Scholar] [CrossRef]
- Bloch, E.M.; Herwaldt, B.L.; Leiby, D.A.; Shaieb, A.; Herron, R.M.; Chervenak, M.; Reed, W.; Hunter, R.; Ryals, R.; Hagar, W.; et al. The third described case of transfusion-transmitted Babesia duncani. Transfusion 2012, 52, 1517–1522. [Google Scholar] [CrossRef]
- Burgess, M.J.; Rosenbaum, E.R.; Pritt, B.S.; Haselow, D.T.; Ferren, K.M.; Alzghoul, B.N.; Rico, J.C.; Sloan, L.M.; Ramanan, P.; Purushothaman, R.; et al. Possible transfusion-transmitted Babesia divergens-like/MO-1 infection in an Arkansas patient. Clin. Infect. Dis. 2017, 64, 1622–1625. [Google Scholar] [CrossRef]
- Faddy, H.M.; Rooks, K.M.; Irwin, P.J.; Viennet, E.; Paparini, A.; Seed, C.R.; Stramer, S.L.; Harley, R.J.; Chan, H.T.; Dennington, P.M.; et al. No evidence for widespread Babesia microti transmission in Australia. Transfusion 2019. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, S.F.; Delage, G.; Scalia, V.; Lindsay, R.; Bernier, F.; Dubuc, S.; Germain, M.; Pilot, G.; Yi, Q.L.; Fearon, M.A. Seroprevalence of Babesia microti infection in Canadian blood donors. Transfusion 2016, 56, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Bloch, E.M.; Yang, Y.; He, M.; Tonnetti, L.; Liu, Y.; Wang, J.; Guo, Y.; Li, H.; Leiby, D.A.; Shan, H.; et al. A pilot serosurvey of Babesia microti in Chinese blood donors. Vox Sang. 2018, 113, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Herwaldt, B.L.; Neitzel, D.F.; Gorlin, J.B.; Jensen, K.A.; Perry, E.H.; Peglow, W.R.; Slemenda, S.B.; Won, K.Y.; Nace, E.K.; Pieniazek, N.J.; et al. Transmission of Babesia microti in Minnesota through four blood donations from the same donor over a 6-month period. Transfusion 2002, 42, 1154–1158. [Google Scholar] [CrossRef] [PubMed]
- Bakkour, S.; Chafets, D.M.; Wen, L.; Muench, M.O.; Telford, S.R., 3rd; Erwin, J.L.; Levin, A.E.; Self, D.; Bres, V.; Linnen, J.M.; et al. Minimal infectious dose and dynamics of Babesia microti parasitemia in a murine model. Transfusion 2018, 58, 2903–2910. [Google Scholar] [CrossRef] [PubMed]
- Meissner, E.G.; McGillicuddy, J.W.; Squires, J.; Skipper, D.; Self, S.; Wray, D.; Moritz, E.D.; Stramer, S.L.; Nadig, S. Across state lines: Fulminant Babesia microti infection in a liver transplant recipient. Transpl. Infect. Dis. 2017, 19, e12741. [Google Scholar] [CrossRef] [PubMed]
- Ngo, V.; Civen, R. Babesiosis acquired through blood transfusion, California, USA. Emerg. Infect. Dis. 2009, 15, 785–787. [Google Scholar] [CrossRef] [PubMed]
- Cangelosi, J.J.; Sarvat, B.; Sarria, J.C.; Herwaldt, B.L.; Indrikovs, A.J. Transmission of Babesia microti by blood transfusion in Texas. Vox Sang. 2008, 95, 331–334. [Google Scholar] [CrossRef] [PubMed]
- Leiby, D.A.; Johnson, S.T.; Won, K.Y.; Nace, E.K.; Slemenda, S.B.; Pieniazek, N.J.; Cable, R.G.; Herwaldt, B.L. A longitudinal study of Babesia microti infection in seropositive blood donors. Transfusion 2014, 54, 2217–2225. [Google Scholar] [CrossRef]
- Bloch, E.M.; Levin, A.E.; Williamson, P.C.; Cyrus, S.; Shaz, B.H.; Kessler, D.; Gorlin, J.; Bruhn, R.; Lee, T.H.; Montalvo, L.; et al. A prospective evaluation of chronic Babesia microti infection in seroreactive blood donors. Transfusion 2016, 56, 1875–1882. [Google Scholar] [CrossRef] [PubMed]
- Moritz, E.D.; Winton, C.S.; Johnson, S.T.; Krysztof, D.E.; Townsend, R.L.; Foster, G.A.; Devine, P.; Molloy, P.; Brissette, E.; Berardi, V.P.; et al. Investigational screening for Babesia microti in a large repository of blood donor samples from nonendemic and endemic areas of the United States. Transfusion 2014, 54, 2226–2236. [Google Scholar] [CrossRef]
- FDA. Recommendations for Reducing the Risk of Transfusion-Transmitted Babesiosis; U.S. Department of Health and Human Services: Silver Spring, MD, USA, 2019.
- Busch, M.P.; Bloch, E.M.; Kleinman, S. Prevention of transfusion-transmitted infections. Blood 2019, 133, 1854–1864. [Google Scholar] [CrossRef] [PubMed]
- Cheng, K.; Coller, K.E.; Marohnic, C.C.; Pfeiffer, Z.A.; Fino, J.R.; Elsing, R.R.; Bergsma, J.; Marcinkus, M.A.; Kar, A.K.; Gumbs, O.H.; et al. Performance evaluation of a prototype architect antibody assay for Babesia microti. J. Clin. Microbiol. 2018, 56. [Google Scholar] [CrossRef]
- Mebius, R.E.; Kraal, G. Structure and function of the spleen. Nat. Rev. Immunol. 2005, 5, 606–616. [Google Scholar] [CrossRef]
- Rosner, F.; Zarrabi, M.H.; Benach, J.L.; Habicht, G.S. Babesiosis in splenectomized adults: Review of 22 reported cases. Am. J. Med. 1984, 76, 696–701. [Google Scholar] [CrossRef]
- Zintl, A.; Mulcahy, G.; Skerrett, H.E.; Taylor, S.M.; Gray, J.S. Babesia divergens, a bovine blood parasite of veterinary and zoonotic importance. Clin. Microbiol. Rev. 2003, 16, 622–636. [Google Scholar] [CrossRef]
- Desforges, J.F.; Quimby, F. Babesia abroad. N. Engl. J. Med. 1976, 295, 103–104. [Google Scholar] [CrossRef] [PubMed]
- Cullen, J.; Levine, J.F. Pathology of experimental Babesia microti infection in the Syrian hamster. Lab. Anim. Sci. 1987, 37, 640–643. [Google Scholar] [PubMed]
- Ruebush, T.K., 2nd; Collins, W.E.; Warren, M. Experimental Babesia microti infections in Macaca mulatta: Recurrent parasitemia before and after splenectomy. Am. J. Trop. Med. Hyg. 1981, 30, 304–307. [Google Scholar] [CrossRef]
- Westra, J.; van Assen, S.; Wilting, K.R.; Land, J.; Horst, G.; de Haan, A.; Bijl, M. Rituximab impairs immunoglobulin (Ig)M and IgG (subclass) responses after influenza vaccination in rheumatoid arthritis patients. Clin. Exp. Immunol. 2014, 178, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Allred, D.R.; Al-Khedery, B. Antigenic variation and cytoadhesion in Babesia bovis and Plasmodium falciparum: Different logics achieve the same goal. Mol. Biochem. Parasitol. 2004, 134, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Clark, I.A.; Budd, A.C.; Hsue, G.; Haymore, B.R.; Joyce, A.J.; Thorner, R.; Krause, P.J. Absence of erythrocyte sequestration in a case of babesiosis in a splenectomized human patient. Malar. J. 2006, 5, 69–71. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Simon, M.S.; Westblade, L.F.; Dziedziech, A.; Visone, J.E.; Furman, R.R.; Jenkins, S.G.; Schuetz, A.N.; Kirkman, L.A. Clinical and molecular evidence of atovaquone and azithromycin resistance in relapsed Babesia microti infection associated with Rituximab and chronic lymphocytic leukemia. Clin. Infect. Dis. 2017, 65, 1222–1225. [Google Scholar] [CrossRef] [PubMed]
- Lemieux, J.E.; Tran, A.D.; Freimark, L.; Schaffner, S.F.; Goethert, H.; Andersen, K.G.; Bazner, S.; Li, A.; McGrath, G.; Sloan, L.; et al. A global map of genetic diversity in Babesia microti reveals strong population structure and identifies variants associated with clinical relapse. Nat. Microbiol. 2016, 1, 16079. [Google Scholar] [CrossRef] [PubMed]
- Sacca, R.; Cuff, C.A.; Ruddle, N.H. Mediators of inflammation. Curr. Opinion. Immunol. 1997, 9, 851–857. [Google Scholar] [CrossRef]
- Shaio, M.; Lin, P.R. A case study of cytokine profiles in acute human babesiosis. Am. J. Trop. Med. Hyg. 1998, 58, 335–337. [Google Scholar] [CrossRef] [PubMed]
- Clark, I.A.; Alleva, L.M.; Mills, A.C.; Cowden, W.B. Pathogenesis of malaria and clinically similar conditions. Clin. Microbiol. Rev. 2004, 17, 509–539. [Google Scholar] [CrossRef]
- Hemmer, R.M.; Ferrick, D.A.; Conrad, P.A. Up-regulation of tumor necrosis factor alpha and interferon-gamma expression in the spleen and lungs of mice infected with the human Babesia isolate WA1. Parasitol. Res. 2000, 86, 121–128. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).