Microbiological Air Quality in Heating, Ventilation and Air Conditioning Systems of Surgical and Intensive Care Areas: The Application of a Disinfection Procedure for Dehumidification Devices
Abstract
1. Introduction
2. Results
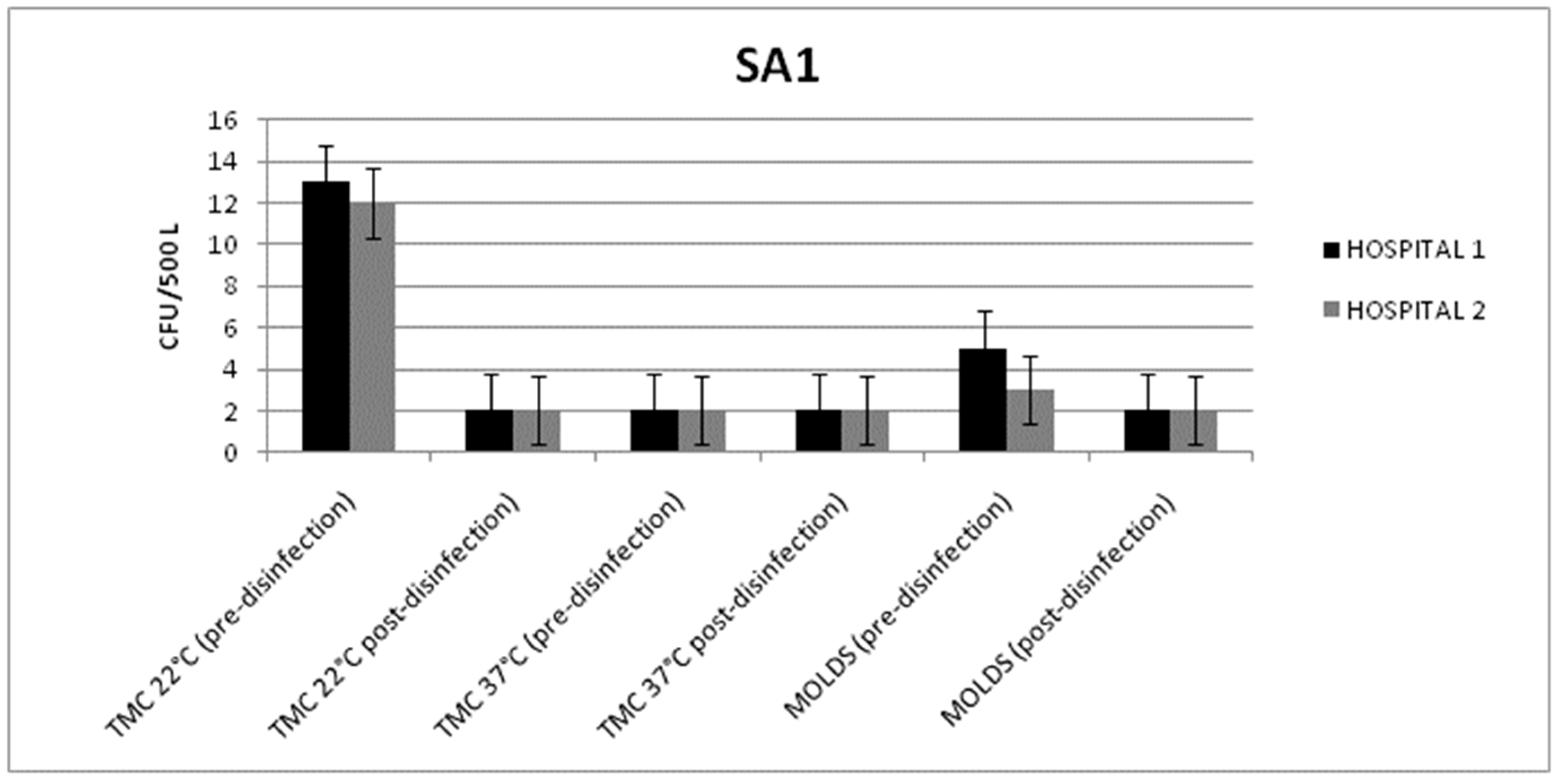
2.1. HVAC Systems in Surgical Area 1 (SA1)
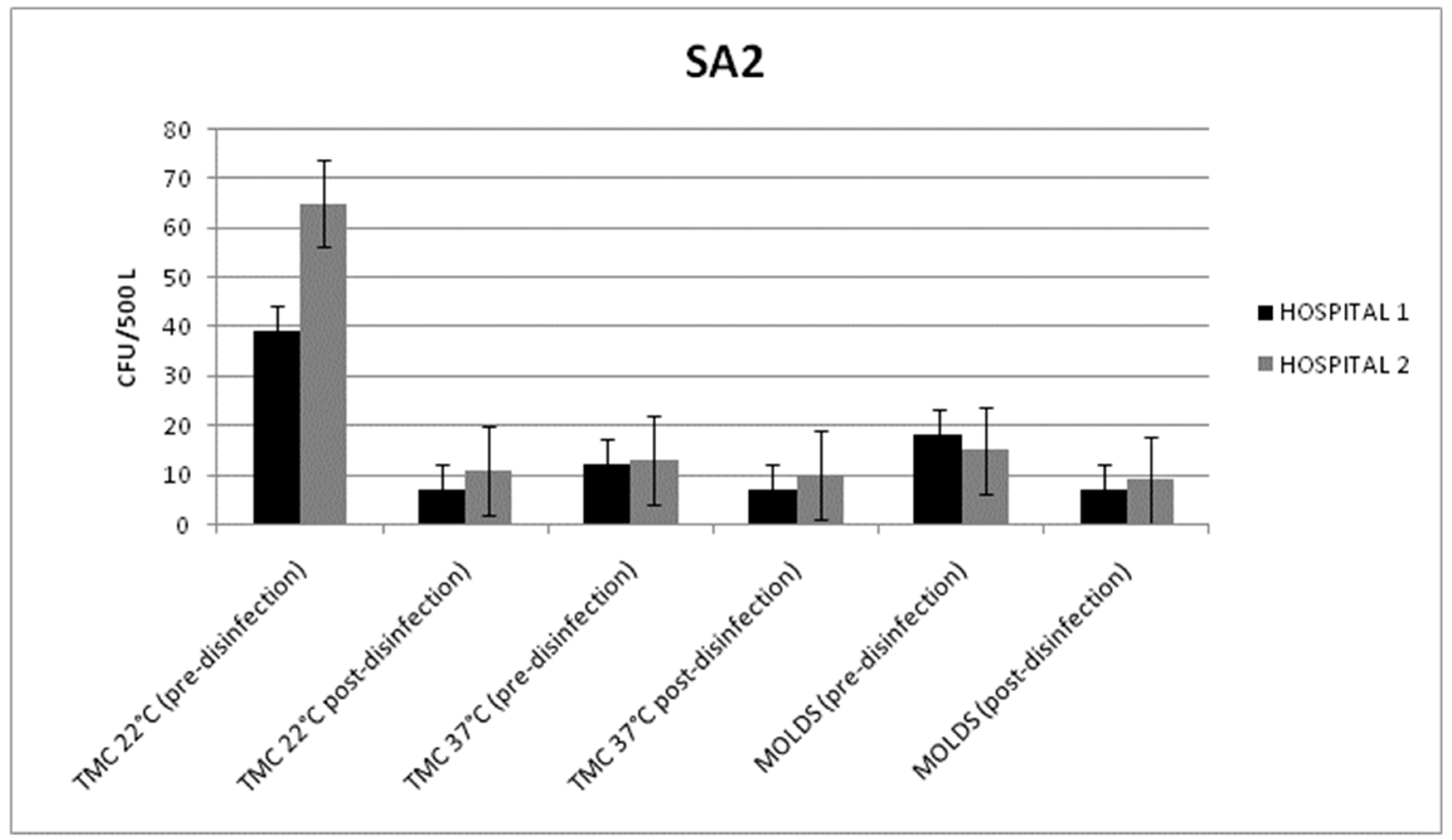
2.2. HVAC Systems in Surgical Area (SA2)
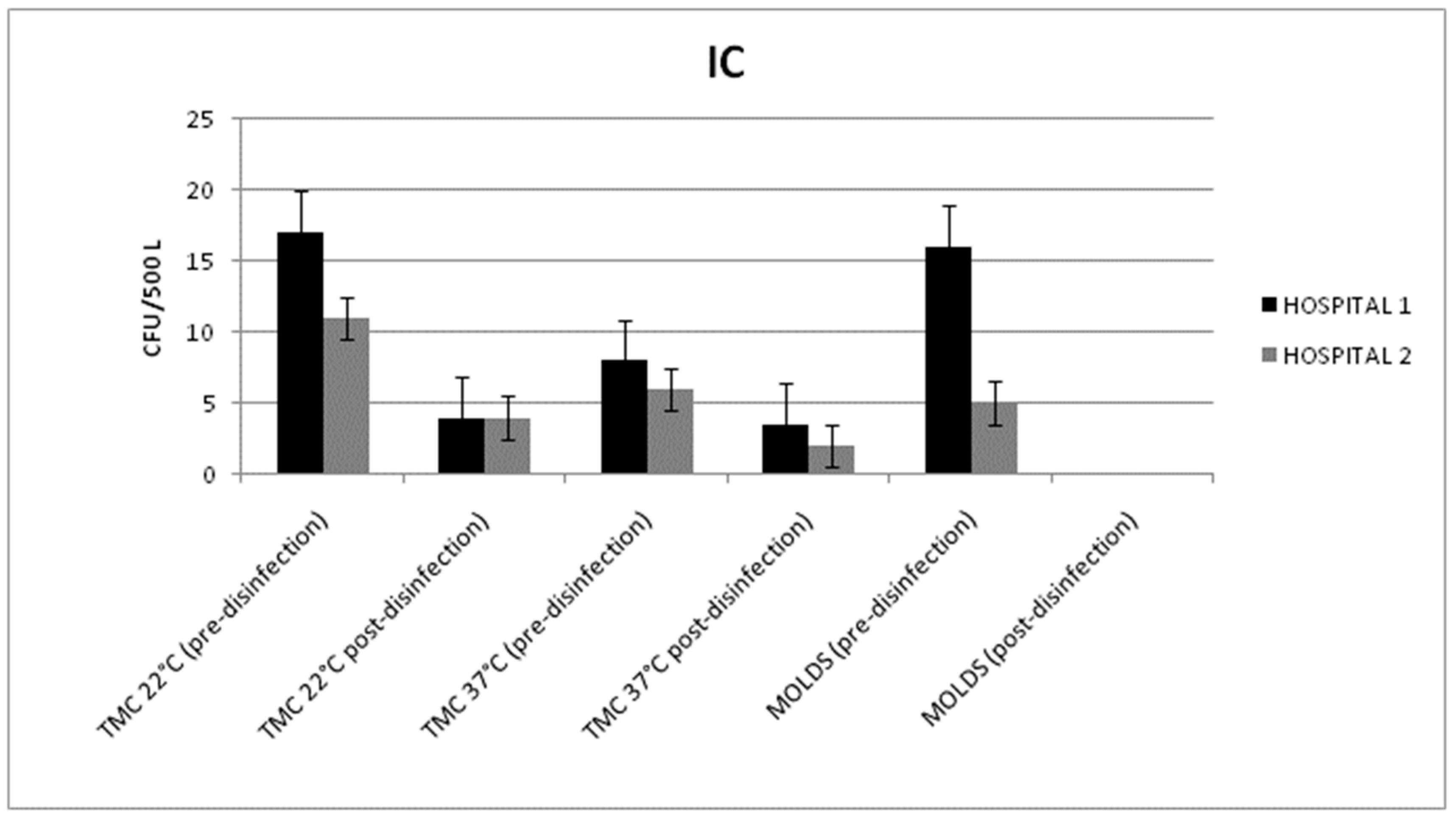
2.3. HVAC Systems in the Intensive Care (IC) Unit
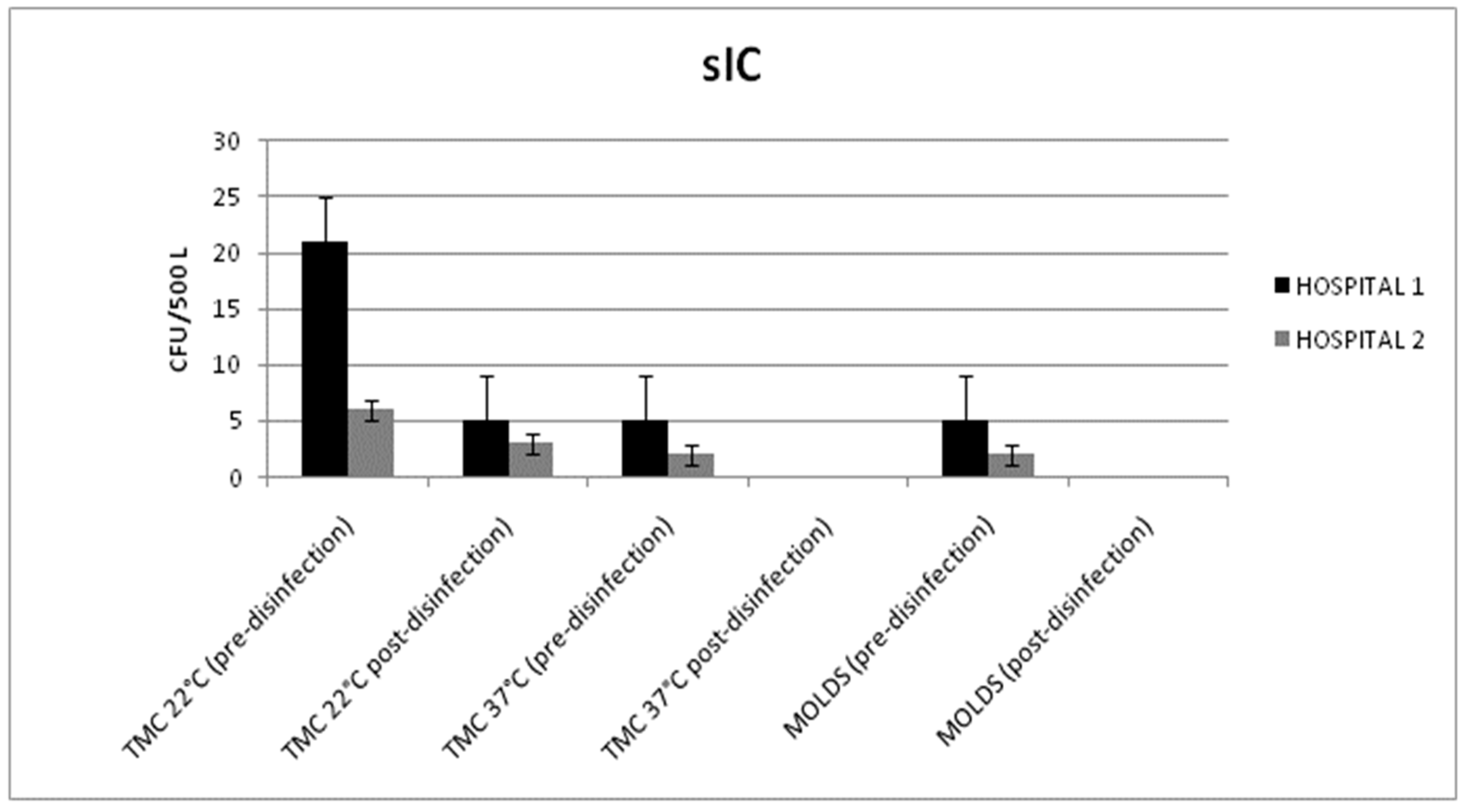
2.4. HVAC Systems in the Sub-Intensive (sIC) Unit
3. Discussion
4. Materials and Methods
Hospital Settings
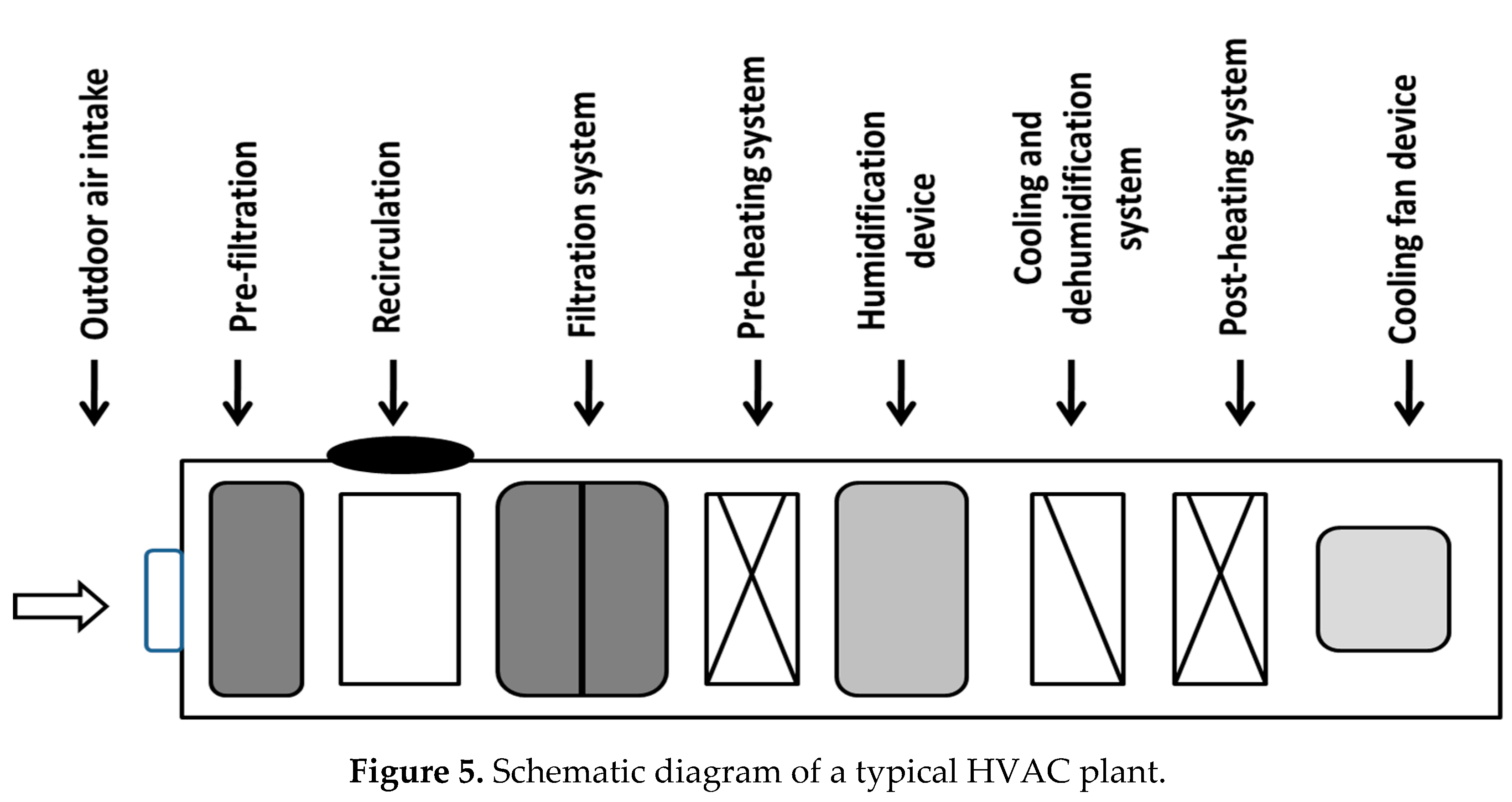
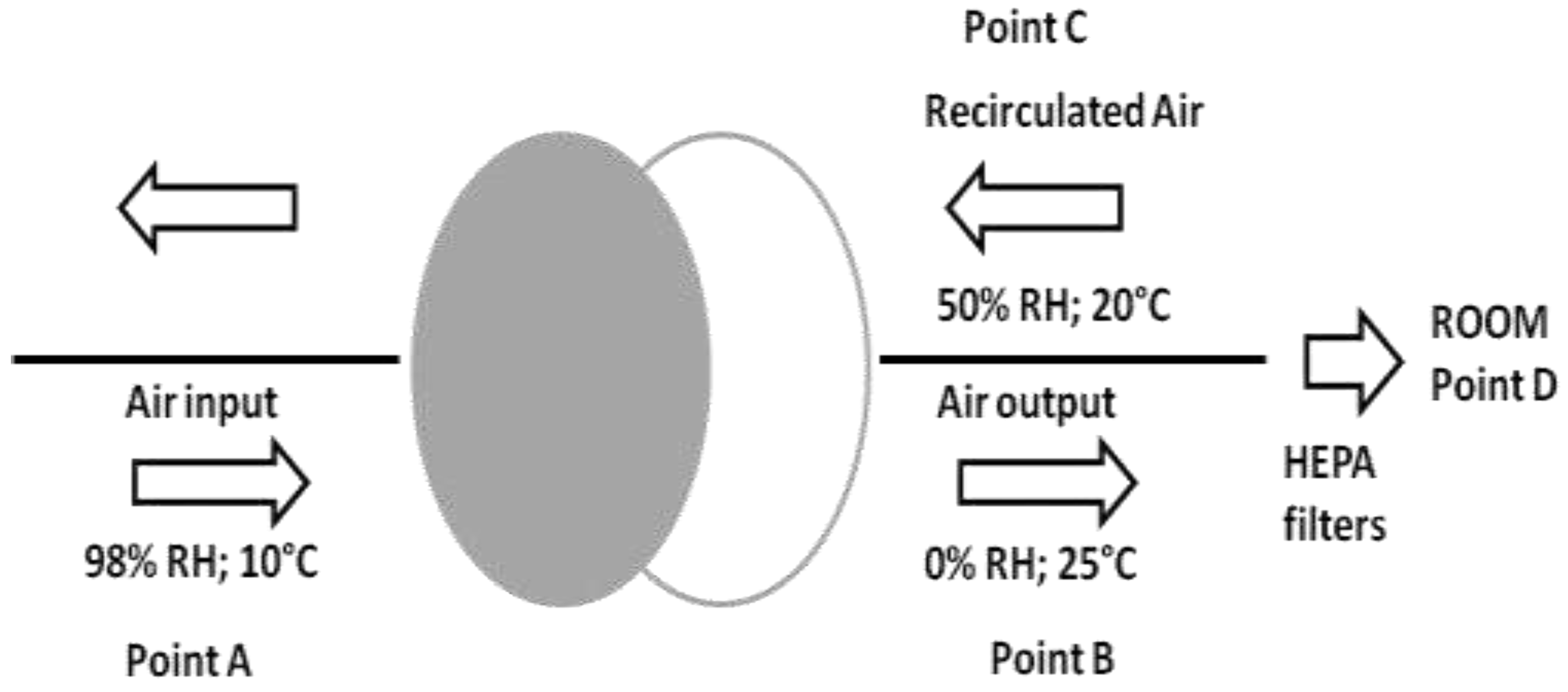
HVAC Systems
Air and Surface Sampling
HVAC System Disinfection
Statistical Analysis
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Pasquarella, C.; Pitzurra, O.; Herren, T.; Poletti, L.; Savino, A. Lack of influence of body exhaust gowns on aerobic bacterial surface counts in a mixed-ventilation operating theatre. A study of 62 hip arthroplasties. J. Hosp. Infect. 2003, 54, 2–9. [Google Scholar] [CrossRef]
- Totaro, M.; Porretta, A.; Canale, A.; Filippetti, E.; Tulipani, A.; Quattrone, F.; Giorgi, S.; Costa, A.L.; Valentini, P.; Casini, B.; et al. Preliminary study of the air quality in operating rooms: Do textiles have a role? J. Hosp. Infect. 2018, 99, 306–308. [Google Scholar] [CrossRef] [PubMed]
- Stocks, G.W.; O’Connor, D.P.; Self, S.D.; Marcek, G.A.; Thompson, B.L. Directed air flow to reduce airborne particulate and bacterial contamination in the surgical field during total hip arthroplasty. J. Arthroplast. 2011, 26, 771–776. [Google Scholar] [CrossRef] [PubMed]
- Cristina, M.L.; Spagnolo, A.M.; Sartini, M.; Sartini, M.; Panatto, D.; Gasparini, R.; Ottria, G.; Perdelli, F. Can particulate air sampling predict microbial load in operating theatres for arthroplasty? PLoS ONE 2012, 7, e52809. [Google Scholar] [CrossRef] [PubMed]
- Anderson, D.J.; Podgorny, K.; Berríos-Torres, S.I.; Bratzler, D.W.; Dellinger, E.P.; Greene, L.; Nyquist, A.C.; Saiman, L.; Yokoe, D.S.; Maragakis, L.L.; et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect. Control Hosp. Epidemiol. 2014, 35, S66–S88. [Google Scholar] [CrossRef]
- Istituto Superiore per la Prevenzione e la Sicurezza del Lavoro. Linee Guida Sugli Standard di Sicurezza e di Igiene del Lavoro nel Reparto Operatorio; ISPESL: Rome, Italy, 2009; pp. 1–56.
- International Organization for Standardization. ISO 14644-1 Cleanrooms and Associated Controlled Environments—Part 1: Classification of Air Cleanliness by Particle Concentration. International Organization for Standardization: Geneva, Switzerland, 2015; pp. 1–37. [Google Scholar]
- National Air Duct Cleaners Association. The NADCA Standard for Assessment, Cleaning, and Restoration of HVAC Systems; NADCA: Mt. Laurel, NJ, USA, 2013; pp. 1–36. [Google Scholar]
- Associazione Italiana Igienisti Sistemi Aeraulici. Protocollo Operativo AIISA per L’ispezione e la Sanificazione Degli Impianti Aeraulici; AIISA: Rome, Italy, 2013; pp. 1–44. [Google Scholar]
- Garrison, R.A.; Robertson, L.D.; Koehn, R.D.; Wynn, S.R. Effect of heating-ventilation-air conditioning system sanitation on airborne fungal populations in residential environments. Ann. Allergy 1993, 71, 548–556. [Google Scholar] [PubMed]
- Ohsaki, Y.; Koyano, S.; Tachibana, M.; Shibukawa, K.; Kuroki, M.; Yoshida, I.; Ito, Y. Undetected Bacillus pseudo-outbreak after renovation work in a teaching hospital. J. Infect. 2007, 54, 617–622. [Google Scholar] [CrossRef] [PubMed]
- Alsved, M.; Civilis, A.; Ekolind, P.; Tammelin, A.; Andersson, A.E.; Jakobsson, J.; Svensson, T.; Ramstorp, M.; Sadrizadeh, S.; Larsson, P.A.; et al. Temperature-controlled airflow ventilation in operating rooms compared with laminar airflow and turbulent mixed airflow. J. Hosp. Infect. 2018, 98, 181–190. [Google Scholar] [CrossRef]
- World Health Organization. Global Guidelines for the Prevention of Surgical Site Infection; World Health Organization: Geneva, Switzerland, 2016; pp. 1–186. [Google Scholar]
- International Organization for Standardization. ISO 16890-1 Air Filters for General Ventilation—Part 1: Technical Specifications, Requirements and Classification System Based upon Particulate Matter Efficiency (ePM); International Organization for Standardization: Geneva, Switzerland, 2016; pp. 1–27. [Google Scholar]
- Gormley, T.; Markel, T.A.; Jones, H.; Greeley, D.; Ostojic, J.; Clarke, J.H.; Abkowitz, M.; Wagner, J. Cost-benefit analysis of different air change rates in an operating room environment. Am. J. Infect. Control 2017, 45, 1318–1323. [Google Scholar] [CrossRef]
- Memarzadeh, F.; Olmsted, R.N.; Bartley, J.M. Applications of ultraviolet germicidal irradiation disinfection in health care facilities: Effective adjunct, but not stand-alone technology. Am. J. Infect. Control 2010, 38, S13–S24. [Google Scholar] [CrossRef] [PubMed]
- Zimlichman, E.; Henderson, D.; Tamir, O.; Franz, C.; Song, P.; Yamin, C.K.; Keohane, C.; Denham, C.R.; Bates, D.W. Health care-associated infections: A meta-analysis of costs and financial impact on the US health care system. JAMA Intern. Med. 2013, 173, 2039–2046. [Google Scholar] [CrossRef] [PubMed]
- Cubi Montanya, E.; Salom Tormo, J.; Garrido Soriano, N. Indoor environmental quality and infection control in surgery rooms: Code requirements vs performance motivation. HVAC&R Res. 2014, 20, 643–654. [Google Scholar] [CrossRef]
- Perfect, J.R.; Cox, G.M.; Lee, J.Y.; Kauffman, C.A.; de Repentigny, L.; Chapman, S.W.; Morrison, V.A.; Pappas, P.; Hiemenz, J.W.; Stevens, D.A.; et al. The impact of culture isolation of Aspergillus species: A hospital-based survey of aspergillosis. Clin. Infect. Dis. 2001, 33, 1824–1833. [Google Scholar] [CrossRef] [PubMed]
- Plá, M.P.; Berenguer, J.; Arzuaga, J.A.; Bañares, R.; Polo, J.R.; Bouza, E. Surgical wound infection by Aspergillus fumigatus in liver transplant recipients. Diagn. Microbiol. Infect. Dis. 1992, 15, 703–706. [Google Scholar] [CrossRef]
- Lutz, B.D.; Jin, J.; Rinaldi, M.G.; Wickes, B.L.; Huycke, M.M. Outbreak of invasive Aspergillus infection in surgical patients, associated with a contaminated air-handling system. Clin. Infect. Dis. 2003, 37, 786–793. [Google Scholar] [CrossRef] [PubMed]
- Kanamori, H.; Rutala, W.A.; Sickbert-Bennett, E.E.; Weber, D.J. Review of fungal outbreaks and infection prevention in healthcare settings during construction and renovation. Clin. Infect. Dis. 2015, 61, 433–444. [Google Scholar] [CrossRef] [PubMed]
- Doll, M.; Preas, M.A.; Johnson, J.K.; Mitchell, C.; Roup, B.; Wilson, L.; Carothers, C.; Nkonge, G.; Leekha, S. A Pseudo-outbreak of Aspergillosis at a Tertiary Care Hospital: Thinking Beyond the Infection Control Risk Assessment. Infect. Control Hosp. Epidemiol. 2017, 38, 115–118. [Google Scholar] [CrossRef]
- Dancer, S.J. The role of environmental cleaning in the control of hospital-acquired infection. J. Hosp. Infect. 2009, 73, 378–385. [Google Scholar] [CrossRef]
- Mitchell, B.G.; Digney, W.; Locket, P.; Dancer, S.J. Controlling methicillin-resistant Staphylococcus aureus (MRSA) in a hospital and the role of hydrogen peroxide decontamination: An interrupted time series analysis. BMJ Open 2014, 4, e004522. [Google Scholar] [CrossRef]
- Block, S.S. Disinfection, Sterilization, and Preservation, 5th ed.; Limpicott Williams & Wilkins: Philadelphia, PA, USA, 2011; pp. 1–1481. [Google Scholar]
- Casini, B.; Aquino, F.; Totaro, M.; Miccoli, M.; Galli, I.; Manfredini, L.; Giustarini, C.; Costa, A.L.; Tuvo, B.; Valentini, P.; et al. Application of Hydrogen Peroxide as an Innovative Method of Treatment for Legionella Control in a Hospital Water Network. Pathogens 2017, 6, 15. [Google Scholar] [CrossRef]
- Dallolio, L.; Raggi, A.; Sanna, T.; Mazzetti, M.; Orsi, A.; Zanni, A.; Farruggia, P.; Leoni, E. Surveillance of Environmental and Procedural Measures of Infection Control in the Operating Theatre Setting. Int. J. Environ. Res. Public Health 2017, 15, 46. [Google Scholar] [CrossRef] [PubMed]
- Caggiano, G.; Napoli, C.; Coretti, C.; Lovero, G.; Scarafile, G.; De Giglio, O.; Montagna, M.T. Mold contamination in a controlled hospital environment: A 3-year surveillance in southern Italy. BMC Infect. Dis. 2014, 14, 595. [Google Scholar] [CrossRef] [PubMed]
| Hospital | Months of Samplings | Hvac Systems | Sampling Conditions | Matrix |
|---|---|---|---|---|
| HOSPITAL 1 | September–December 2016 | SA1 SA2 IC sIC | First sampling with RDW in operation | |
| May–July 2017 | Second sampling with RDW in operation (24 h after the disinfection) | Air and surfaces | ||
| HOSPITAL 2 | April–May 2018 | SA1 SA2 IC sIC | First sampling with RDW in operation | |
| July 2018 | Second sampling with RDW in operation (24 h after the disinfection) | Air and surfaces |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Totaro, M.; Costa, A.L.; Casini, B.; Profeti, S.; Gallo, A.; Frendo, L.; Porretta, A.; Valentini, P.; Privitera, G.; Baggiani, A. Microbiological Air Quality in Heating, Ventilation and Air Conditioning Systems of Surgical and Intensive Care Areas: The Application of a Disinfection Procedure for Dehumidification Devices. Pathogens 2019, 8, 8. https://doi.org/10.3390/pathogens8010008
Totaro M, Costa AL, Casini B, Profeti S, Gallo A, Frendo L, Porretta A, Valentini P, Privitera G, Baggiani A. Microbiological Air Quality in Heating, Ventilation and Air Conditioning Systems of Surgical and Intensive Care Areas: The Application of a Disinfection Procedure for Dehumidification Devices. Pathogens. 2019; 8(1):8. https://doi.org/10.3390/pathogens8010008
Chicago/Turabian StyleTotaro, Michele, Anna Laura Costa, Beatrice Casini, Sara Profeti, Antonio Gallo, Lorenzo Frendo, Andrea Porretta, Paola Valentini, Gaetano Privitera, and Angelo Baggiani. 2019. "Microbiological Air Quality in Heating, Ventilation and Air Conditioning Systems of Surgical and Intensive Care Areas: The Application of a Disinfection Procedure for Dehumidification Devices" Pathogens 8, no. 1: 8. https://doi.org/10.3390/pathogens8010008
APA StyleTotaro, M., Costa, A. L., Casini, B., Profeti, S., Gallo, A., Frendo, L., Porretta, A., Valentini, P., Privitera, G., & Baggiani, A. (2019). Microbiological Air Quality in Heating, Ventilation and Air Conditioning Systems of Surgical and Intensive Care Areas: The Application of a Disinfection Procedure for Dehumidification Devices. Pathogens, 8(1), 8. https://doi.org/10.3390/pathogens8010008





