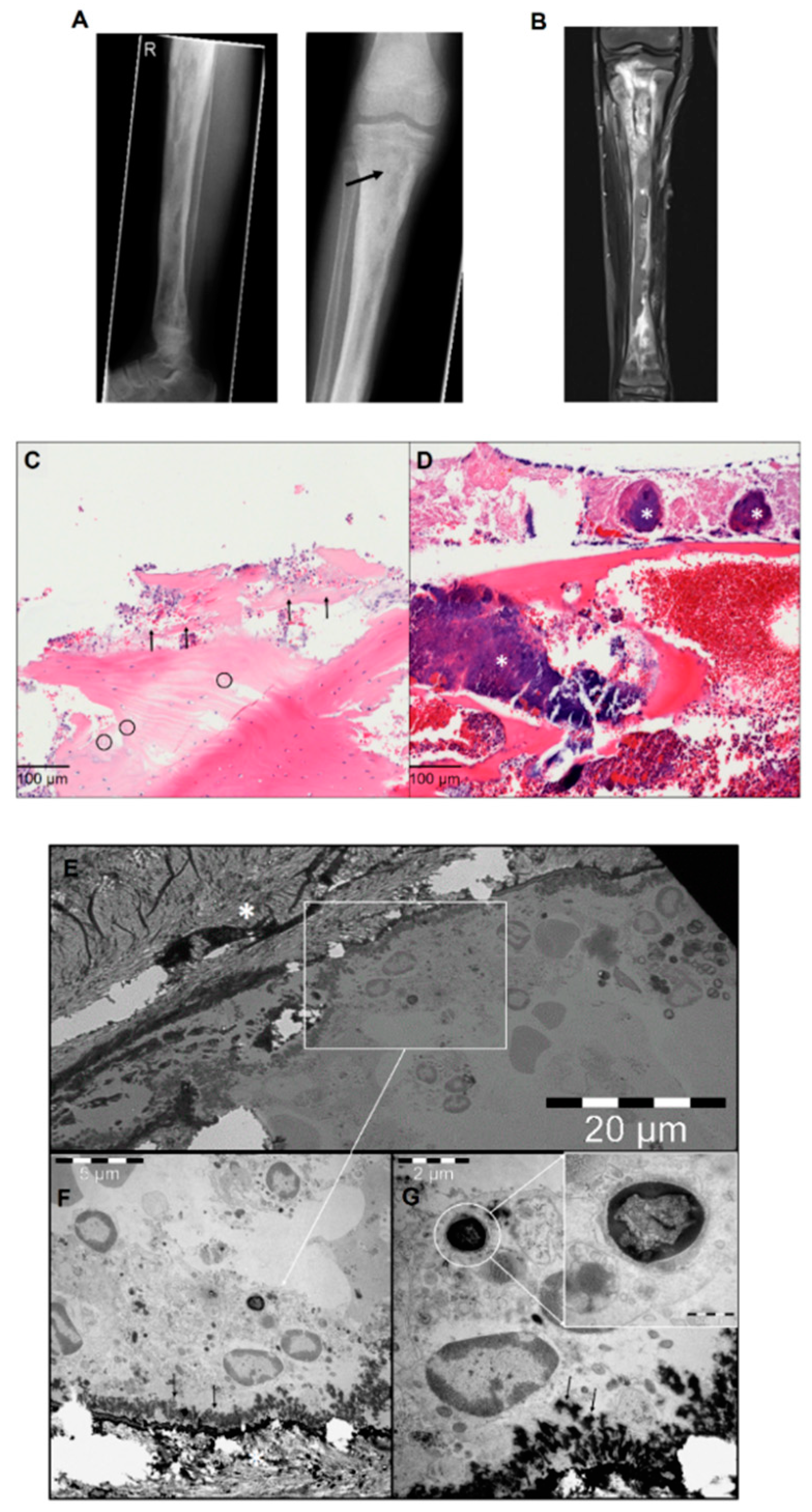
Intracellular S. aureus in Osteoblasts in a Clinical Sample from a Patient with Chronic Osteomyelitis—A Case Report
Abstract
:1. Introduction
2. Case Presentation
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Walter, N.; Baertl, S.; Alt, V.; Rupp, M. What is the burden of osteomyelitis in Germany? An analysis of inpatient data from 2008 through 2018. BMC Infect. Dis. 2021, 21, 550. [Google Scholar] [CrossRef] [PubMed]
- Urish, K.L.; Cassat, J.E. Staphylococcus aureus Osteomyelitis: Bone, Bugs, and Surgery. Infect. Immun. 2020, 88, e00932-19. [Google Scholar] [CrossRef] [PubMed]
- Costerton, J.W.; Stewart, P.; Greenberg, E. Bacterial Biofilms: A Common Cause of Persistent Infections. Science 1999, 284, 1318–1322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Josse, J.; Velard, F.; Gangloff, S.C. Staphylococcus aureus vs. Osteoblast: Relationship and Consequences in Osteomyelitis. Front. Cell. Infect. Microbiol. 2015, 5, 85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stracquadanio, S.; Musso, N.; Costantino, A.; Lazzaro, L.M.; Stefani, S.; Bongiorno, D. Staphylococcus aureus Internalization in Osteoblast Cells: Mechanisms, Interactions and Biochemical Processes. What Did We Learn from Experimental Models? Pathogens 2021, 10, 239. [Google Scholar] [CrossRef]
- Valour, F.; Rasigade, J.-P.; Trouillet-Assant, S.; Gagnaire, J.; Bouaziz, A.; Karsenty, J.; Lacour, C.; Bes, M.; Lustig, S.; Bénet, T.; et al. Delta-toxin production deficiency in Staphylococcus aureus: A diagnostic marker of bone and joint infection chronicity linked with osteoblast invasion and biofilm formation. Clin. Microbiol. Infect. 2015, 21, 568.e1–568.e11. [Google Scholar] [CrossRef] [Green Version]
- Kalinka, J.; Hachmeister, M.; Geraci, J.; Sordelli, D.O.; Hansen, U.; Niemann, S.; Oetermann, S.; Peters, G.; Löffler, B.; Tuchscherr, L. Staphylococcus aureus isolates from chronic osteomyelitis are characterized by high host cell invasion and intracellular adaptation, but still induce inflammation. Int. J. Med. Microbiol. 2014, 304, 1038–1049. [Google Scholar] [CrossRef] [PubMed]
- Hamza, T.; Li, B. Differential responses of osteoblasts and macrophages upon Staphylococcus aureus infection. BMC Microbiol. 2014, 14, 207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mannala, G.K.; Koettnitz, J.; Mohamed, W.; Sommer, U.; Lips, K.S.; Spröer, C.; Bunk, B.; Overmann, J.; Hain, T.; Heiss, C.; et al. Whole-genome comparison of high and low virulent Staphylococcus aureus isolates inducing implant-associated bone infections. Int. J. Med. Microbiol. 2018, 308, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, W.; Sommer, U.; Sethi, S.; Domann, E.; Thormann, U.; Schütz, I.; Lips, K.; Chakraborty, T.; Schnettler, R.; Alt, V. Intracellular proliferation of S. aureus in osteoblasts and effects of rifampicin and gentamicin on S. aureus intracellular proliferation and survival. Eur. Cells Mater. 2014, 28, 258–268. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, W.; Domann, E.; Chakraborty, T.; Mannala, G.; Lips, K.S.; Heiss, C.; Schnettler, R.; Alt, V. TLR9 mediates S. aureus killing inside osteoblasts via induction of oxidative stress. BMC Microbiol. 2016, 16, 230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reilly, S.; Hudson, M.; Kellam, J.; Ramp, W. In vivo internalization of Staphylococcus aureus by embryonic chick osteoblasts. Bone 2000, 26, 63–70. [Google Scholar] [CrossRef]
- Bosse, M.J.; Gruber, H.E.; Ramp, W.K. Internalization of Bacteria by Osteoblasts in a Patient with Recurrent, Long-Term Osteomyelitis: A Case Report. JBJS Case Connect. 2005, 87, 1343–1347. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Walter, N.; Mendelsohn, D.; Brochhausen, C.; Rupp, M.; Alt, V. Intracellular S. aureus in Osteoblasts in a Clinical Sample from a Patient with Chronic Osteomyelitis—A Case Report. Pathogens 2021, 10, 1064. https://doi.org/10.3390/pathogens10081064
Walter N, Mendelsohn D, Brochhausen C, Rupp M, Alt V. Intracellular S. aureus in Osteoblasts in a Clinical Sample from a Patient with Chronic Osteomyelitis—A Case Report. Pathogens. 2021; 10(8):1064. https://doi.org/10.3390/pathogens10081064
Chicago/Turabian StyleWalter, Nike, Daniel Mendelsohn, Christoph Brochhausen, Markus Rupp, and Volker Alt. 2021. "Intracellular S. aureus in Osteoblasts in a Clinical Sample from a Patient with Chronic Osteomyelitis—A Case Report" Pathogens 10, no. 8: 1064. https://doi.org/10.3390/pathogens10081064
APA StyleWalter, N., Mendelsohn, D., Brochhausen, C., Rupp, M., & Alt, V. (2021). Intracellular S. aureus in Osteoblasts in a Clinical Sample from a Patient with Chronic Osteomyelitis—A Case Report. Pathogens, 10(8), 1064. https://doi.org/10.3390/pathogens10081064






