Do Obese Children Achieve Maximal Heart Rate during Treadmill Running?
Abstract
1. Introduction
2. Methods
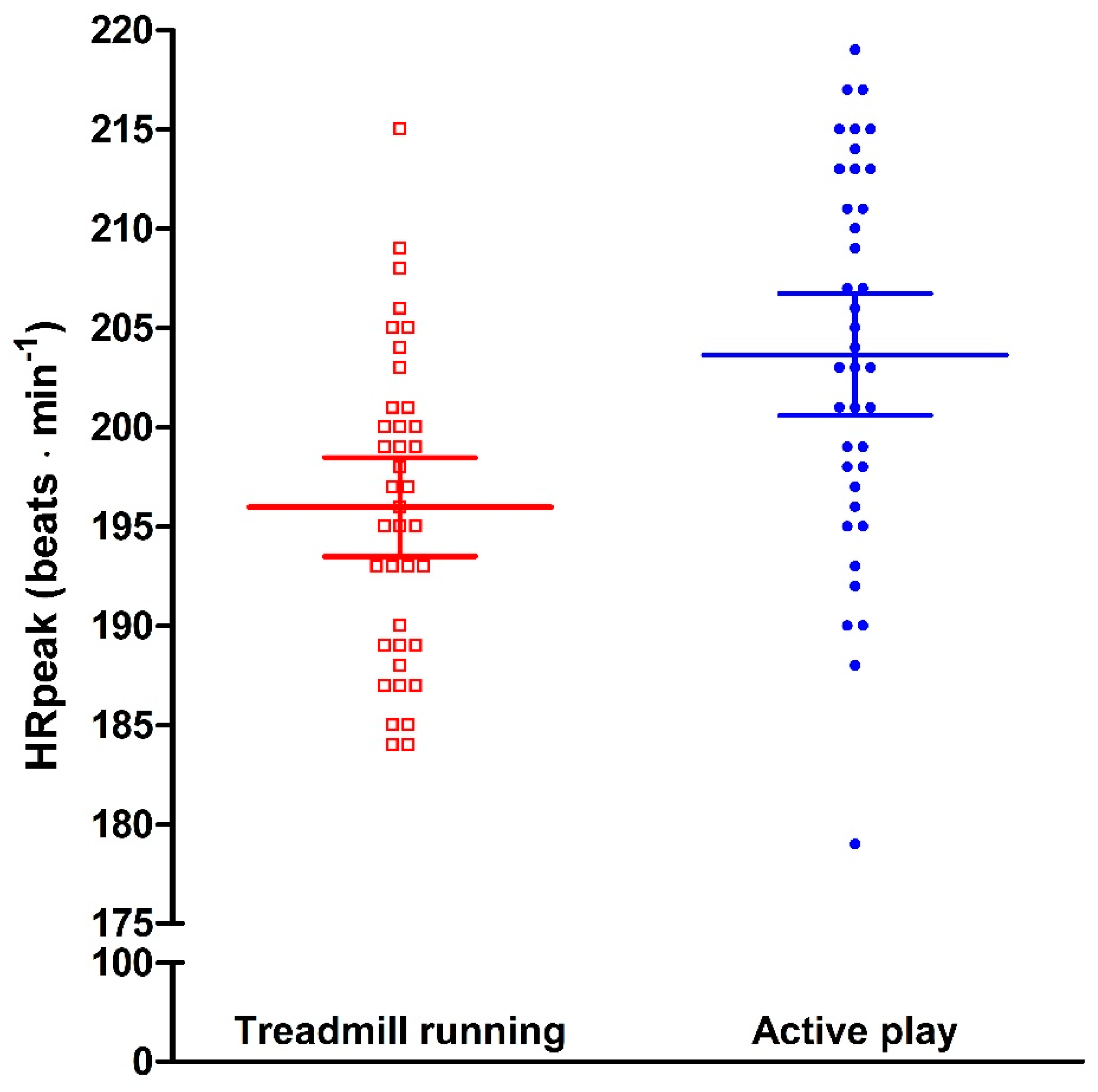
3. Results
4. Discussion
5. Conclusions
6. Practical Implications
- How to report and interpret exercise intensity seems important in training programs for obese children and adolescents.
- The type of exercise as well as setting may influence exercise intensity.
- Active play may result in higher exercise intensity compared to treadmill running in obese children and adolescents.
Author Contributions
Funding
Conflicts of Interest
References
- Oude, L.H.; Baur, L.; Jansen, H.; Shrewsbury, V.A.; O’Malley, C.; Stolk, R.P.; Summerbell, C.D. Interventions for treating obesity in children. Cochrane Database Syst. Rev. 2009, CD001872. [Google Scholar]
- DiNubile, N.A. Youth fitness—Problems and solutions. Prev. Med. 1993, 22, 589–594. [Google Scholar] [CrossRef] [PubMed]
- Berntsen, S.; Mowinckel, P.; Carlsen, K.H.; Lodrup Carlsen, K.C.; Pollestad Kolsgaard, M.L.; Joner, G.; Anderssen, S.A. Obese children playing towards an active lifestyle. Int. J. Pediatr. Obes. 2010, 5, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Speiser, P.W.; Rudolf, M.C.; Anhalt, H.; Camacho-Hubner, C.; Chiarelli, F.; Eliakim, A.; Freemark, M.; Gruters, A.; Hershkovitz, E.; Iughetti, L.; et al. Childhood obesity. J. Clin. Endocrinol. Metab. 2005, 90, 1871–1887. [Google Scholar] [CrossRef] [PubMed]
- Mann, T.; Lamberts, R.P.; Lambert, M.I. Methods of prescribing relative exercise intensity: Physiological and practical considerations. Sports Med. 2013, 43, 613–625. [Google Scholar] [CrossRef] [PubMed]
- Braaksma, P.; Stuive, I.; Garst, R.M.E.; Wesselink, C.F.; van der Sluis, C.K.; Dekker, R.; Schoemaker, M.M. Characteristics of physical activity interventions and effects on cardiorespiratory fitness in children aged 6–12 years—A systematic review. J. Sci. Med. Sport 2018, 21, 296–306. [Google Scholar] [CrossRef] [PubMed]
- American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2005. [Google Scholar]
- Fox, S.M., III; Naughton, J.P.; Haskell, W.L. Physical activity and the prevention of coronary heart disease. Ann. Clin. Res. 1971, 3, 404–432. [Google Scholar] [CrossRef]
- Tanaka, H.; Monahan, K.D.; Seals, D.R. Age-predicted maximal heart rate revisited. J. Am. Coll. Cardiol. 2001, 37, 153–156. [Google Scholar] [CrossRef]
- Fernhall, B.; McCubbin, J.A.; Pitetti, K.H.; Rintala, P.; Rimmer, J.H.; Millar, A.L.; De Silva, A. Prediction of maximal heart rate in individuals with mental retardation. Med. Sci. Sports Exerc. 2001, 33, 1655–1660. [Google Scholar] [CrossRef]
- Machado, F.A.; Denadai, B.S. Validity of maximum heart rate prediction equations for children and adolescents. Arq. Bras. Cardiol. 2011, 97, 136–140. [Google Scholar] [CrossRef]
- Mahon, A.D.; Marjerrison, A.D.; Lee, J.D.; Woodruff, M.E.; Hanna, L.E. Evaluating the prediction of maximal heart rate in children and adolescents. Res. Q. Exerc. Sport 2010, 81, 466–471. [Google Scholar] [CrossRef]
- Washington, R.L.; Bricker, J.T.; Alpert, B.S.; Daniels, S.R.; Deckelbaum, R.J.; Fisher, E.A.; Gidding, S.S.; Isabel-Jones, J.; Kavey, R.E.; Marx, G.R.; et al. Guidelines for exercise testing in the pediatric age group. From the Committee on Atherosclerosis and Hypertension in Children, Council on Cardiovascular Disease in the Young, the American Heart Association. Circulation 1994, 90, 2166–2179. [Google Scholar] [CrossRef] [PubMed]
- Naughton, G.A.; Carlson, J.S.; Greene, D.A. A challenge to fitness testing in primary schools. J. Sci. Med. Sport 2006, 9, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Tsigilis, N. The influence of intrinsic motivation on an endurance field test. J. Sports Med. Phys. Fit. 2005, 45, 213–216. [Google Scholar]
- Kolsgaard, M.L.; Andersen, L.F.; Tonstad, S.; Brunborg, C.; Wangensteen, T.; Joner, G. Ethnic differences in metabolic syndrome among overweight and obese children and adolescents: The Oslo Adiposity Intervention Study. Acta Paediatr. 2008, 97, 1557–1563. [Google Scholar] [CrossRef]
- Knudtzon, J.; Waaler, P.E.; Skjaerven, R.; Solberg, L.K.; Steen, J. New Norwegian percentage charts for height, weight and head circumference for age groups 0–17 years. Tidsskr. Nor. Laegeforen. 1988, 108, 2125–2135. [Google Scholar] [PubMed]
- Andersen, L.B.; Harro, M.; Sardinha, L.B.; Froberg, K.; Ekelund, U.; Brage, S.; Anderssen, S.A. Physical activity and clustered cardiovascular risk in children: A cross-sectional study (The European Youth Heart Study). Lancet 2006, 368, 299–304. [Google Scholar] [CrossRef]
- Ekelund, U.; Sardinha, L.B.; Anderssen, S.A.; Harro, M.; Franks, P.W.; Brage, S.; Cooper, A.R.; Andersen, L.B.; Riddoch, C.; Froberg, K. Associations between objectively assessed physical activity and indicators of body fatness in 9- to 10-y-old European children: A population-based study from 4 distinct regions in Europe (the European Youth Heart Study). Am. J. Clin. Nutr. 2004, 80, 584–590. [Google Scholar] [CrossRef]
- Borg, G. Perceived exertion as an indicator of somatic stress. Scand. J. Rehabil. Med. 1970, 2, 92–98. [Google Scholar]
- Shephard, R.J.; Allen, C.; Bar-Or, O.; Davies, C.T.; Degre, S.; Hedman, R.; Ishii, K.; Kaneko, M.; LaCour, J.R.; di Prampero, P.E.; et al. The working capacity of Toronto schoolchildren. I. Can. Med. Assoc. J. 1969, 100, 560–566. [Google Scholar]
- Lambrick, D.; Jakeman, J.; Grigg, R.; Kaufmann, S.; Faulkner, J. The efficacy of a discontinuous graded exercise test in measuring peak oxygen uptake in children aged 8 to 10 years. Biol. Sport 2017, 34, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Aras, S. Free play in early childhood education: A phenomenological study. Early Child. Dev. Care 2016, 186, 1173–1184. [Google Scholar] [CrossRef]
- Wilmore, J.H.; Constable, S.H.; Stanforth, P.R.; Tasao, W.Y.; Rotkis, T.C.; Paicius, R.M.; Mattern, C.M.; Ewy, G.A. Prevalence of coronary heart disease risk factors in 13-to 15-year-old boys. J. Cardiac. Rehabil. 1982, 2, 223–233. [Google Scholar]
- Hermansen, L.; Oseid, S. Direct and indirect estimation of maximal oxygen uptake in pre-pubertal boys. Acta Paediatr. Scand. Suppl. 1971, 217, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, S.J.; Weiss, R.; Adams, F.H. A comparison of the maximal endurance of normal children and patients with congenital cardiac disease. J. Pediatr. 1966, 69, 46–55. [Google Scholar] [CrossRef]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P.; American College of Sports Medicine. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [PubMed]
- Epstein, L.H.; Paluch, R.A.; Kalakanis, L.E.; Goldfield, G.S.; Cerny, F.J.; Roemmich, J.N. How much activity do youth get? A quantitative review of heart-rate measured activity. Pediatrics 2001, 108, E44. [Google Scholar] [CrossRef]
- Hawley, J.A. Adaptations of skeletal muscle to prolonged, intense endurance training. Clin. Exp. Pharmacol. Physiol. 2002, 29, 218–222. [Google Scholar] [CrossRef]
- Ingjer, F.; Stromme, S.B. Effects of active, passive or no warm-up on the physiological response to heavy exercise. Eur. J. Appl. Physiol. Occup. Physiol. 1979, 40, 273–282. [Google Scholar] [CrossRef]
| Girls (n = 21) | Boys (n = 18) | P-value ** | |
|---|---|---|---|
| Age (years) | 12 (2) | 13 (2) | 0.10 |
| Body mass (kg) | 70 (19) | 75 (17) | 0.15 |
| Height (cm) | 154 (10) | 161 (10) | 0.01 |
| Percentage of body fat (%) | 49 (5) | 45 (6) | 0.03 |
| MVPA (min·day−1) | 43 (14) | 81 (22) | <0.01 |
| Girls (n = 21) | Boys (n = 18) | P-value ** | |
|---|---|---|---|
| Peak (1∙min−1) | 82.4 (25.0) | 87.0 (20.1) | 0.55 |
| Peak RER | 1.06 (0.07) | 1.00 (0.09) | 0.04 |
| Peak RPE | 18 (2) | 18 (1) | 0.74 |
| Peak HR (beats∙min−1) | 195 (8) | 197 (7) | 0.58 |
| Speed at termination (km∙t−1) | 7.4 (0.6) | 7.2 (0.6) | 0.23 |
| Inclination at termination (%) | 7.1 (1.6) | 6.7 (2.1) | 0.51 |
| peak (ml∙kg−1∙min−1) | 33.5 (5.1) | 34.7 (7.1) | 0.53 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berntsen, S.; Edvardsen, E.; Gerbi, S.; Kolsgaard, M.L.; Anderssen, S.A. Do Obese Children Achieve Maximal Heart Rate during Treadmill Running? Sports 2019, 7, 26. https://doi.org/10.3390/sports7010026
Berntsen S, Edvardsen E, Gerbi S, Kolsgaard ML, Anderssen SA. Do Obese Children Achieve Maximal Heart Rate during Treadmill Running? Sports. 2019; 7(1):26. https://doi.org/10.3390/sports7010026
Chicago/Turabian StyleBerntsen, Sveinung, Elisabeth Edvardsen, Shlomi Gerbi, Magnhild L. Kolsgaard, and Sigmund A. Anderssen. 2019. "Do Obese Children Achieve Maximal Heart Rate during Treadmill Running?" Sports 7, no. 1: 26. https://doi.org/10.3390/sports7010026
APA StyleBerntsen, S., Edvardsen, E., Gerbi, S., Kolsgaard, M. L., & Anderssen, S. A. (2019). Do Obese Children Achieve Maximal Heart Rate during Treadmill Running? Sports, 7(1), 26. https://doi.org/10.3390/sports7010026




