Dry Needling in Overhead Athletes with Myofascial Shoulder Pain: A Systematic Review
Abstract
1. Introduction
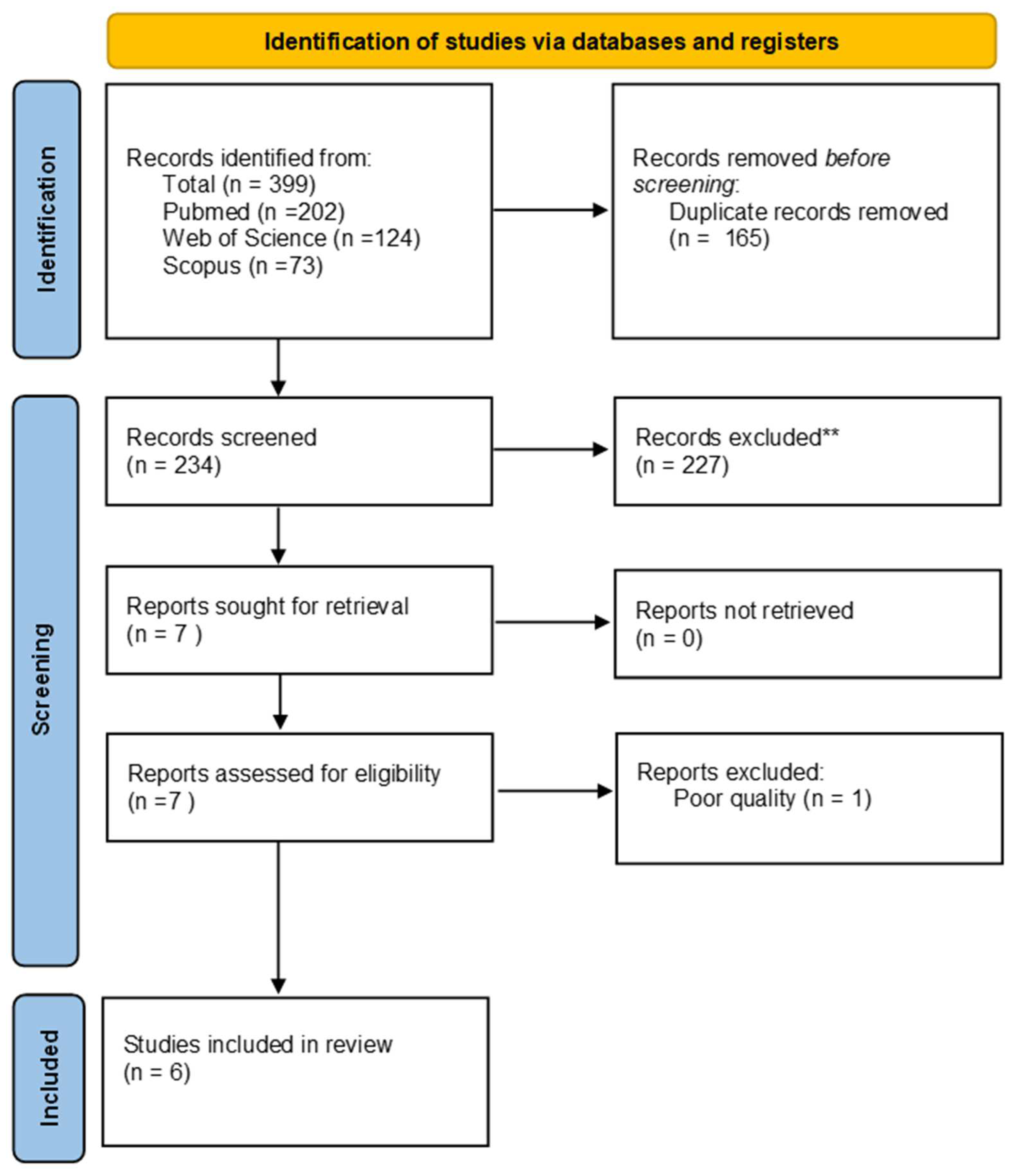
2. Materials and Methods
2.1. Search Strategy
2.2. Selection of Articles
2.3. Data Extraction
2.4. Quality Assessment
3. Results
3.1. Evidence Synthesis
3.2. Synthesis of the Results
3.3. Intervention Protocol
3.4. Outcome Measures
3.4.1. Pain
3.4.2. PPT and Disability
3.4.3. ROM and Isometric Strength
3.4.4. Shoulder Function
3.4.5. Stiffness and Tone
3.4.6. Risk of Bias
3.4.7. Study Limitations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Urwin, M.; Symmons, D.; Allison, T.; Brammah, T.; Busby, H.; Roxby, M.; Simmons, A.; Williams, G. Estimating the Burden of Musculoskeletal Disorders in the Community: The Comparative Prevalence of Symptoms at Different Anatomical Sites, and the Relation to Social Deprivation. Ann. Rheum. Dis. 1998, 57, 649–655. [Google Scholar] [CrossRef]
- Schwank, A.; Blazey, P.; Asker, M.; Møller, M.; Hägglund, M.; Gard, S.; Skazalski, C.; Haugsbø Andersson, S.; Horsley, I.; Whiteley, R.; et al. 2022 Bern Consensus Statement on Shoulder Injury Prevention, Rehabilitation, and Return to Sport for Athletes at All Participation Levels. J. Orthop. Sports Phys. Ther. 2022, 52, 11–28. [Google Scholar] [CrossRef]
- Hoppe, M.W.; Brochhagen, J.; Tischer, T.; Beitzel, K.; Seil, R.; Grim, C. Risk Factors and Prevention Strategies for Shoulder Injuries in Overhead Sports: An Updated Systematic Review. J. Exp. Orthop. 2022, 9, 78. [Google Scholar] [CrossRef] [PubMed]
- Sciascia, A.D. Rehabilitation of the Painful Shoulder. J. Shoulder Elb. Surg. 2023, 33, 494–506. [Google Scholar] [CrossRef] [PubMed]
- Demeco, A.; de Sire, A.; Marotta, N.; Spanò, R.; Lippi, L.; Palumbo, A.; Iona, T.; Gramigna, V.; Palermi, S.; Leigheb, M.; et al. Match Analysis, Physical Training, Risk of Injury and Rehabilitation in Padel: Overview of the Literature. Int. J. Environ. Res. Public Health 2022, 19, 4153. [Google Scholar] [CrossRef] [PubMed]
- Fahlström, M.; Yeap, J.S.; Alfredson, H.; Söderman, K. Shoulder Pain—A Common Problem in World-Class Badminton Players. Scand. J. Med. Sci. Sports 2006, 16, 168–173. [Google Scholar] [CrossRef]
- Clarsen, B.; Bahr, R.; Heymans, M.W.; Engedahl, M.; Midtsundstad, G.; Rosenlund, L.; Thorsen, G.; Myklebust, G. The Prevalence and Impact of Overuse Injuries in Five Norwegian Sports: Application of a New Surveillance Method. Scand. J. Med. Sci. Sports 2015, 25, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Matsuura, T.; Suzue, N.; Iwame, T.; Arisawa, K.; Fukuta, S.; Sairyo, K. Epidemiology of Shoulder and Elbow Pain in Youth Baseball Players. Phys. Sport. 2016, 44, 97–100. [Google Scholar] [CrossRef] [PubMed]
- De Sire, A.; Demeco, A.; Frizziero, A.; Marotta, N.; Spanò, R.; Carozzo, S.; Costantino, C.; Ammendolia, A. Risk of Injury and Kinematic Assessment of the Shoulder Biomechanics during Strokes in Padel Players: A Cross-Sectional Study. J. Sports Med. Phys. Fitness 2024, 64, 383–391. [Google Scholar] [CrossRef]
- Bahr, R.; Reeser, J.C. Injuries among World-Class Professional Beach Volleyball Players: The Fédération Internationale de Volleyball Beach Volleyball Injury Study. Am. J. Sports Med. 2003, 31, 119–125. [Google Scholar] [CrossRef]
- Moller, M.; Attermann, J.; Myklebust, G.; Wedderkopp, N. Injury Risk in Danish Youth and Senior Elite Handball Using a New SMS Text Messages Approach. Br. J. Sports Med. 2012, 46, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Verhagen, E.A.L.M.; Van der Beek, A.J.; Bouter, L.M.; Bahr, R.M.; Van Mechelen, W. A One Season Prospective Cohort Study of Volleyball Injuries. Br. J. Sports Med. 2004, 38, 477–481. [Google Scholar] [CrossRef] [PubMed]
- Mohseni-Bandpei, M.A.; Keshavarz, R.; Minoonejhad, H.; Mohsenifar, H.; Shakeri, H. Shoulder Pain in Iranian Elite Athletes: The Prevalence and Risk Factors. J. Manip. Physiol. Ther. 2012, 35, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Lo, Y.P.; Hsu, Y.C.; Chan, K.M. Epidemiology of Shoulder Impingement in Upper Arm Sports Events. Br. J. Sports Med. 1990, 24, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Bakshi, N.; Freehill, M.T. The Overhead Athletes Shoulder. Sports Med. Arthrosc. Rev. 2018, 26, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Kamali, F.; Sinaei, E.; Morovati, M. Comparison of Upper Trapezius and Infraspinatus Myofascial Trigger Point Therapy by Dry Needling in Overhead Athletes With Unilateral Shoulder Impingement Syndrome. J. Sport. Rehabil. 2019, 28, 243–249. [Google Scholar] [CrossRef]
- Ceballos-Laita, L.; Medrano-de-la-Fuente, R.; Estébanez-De-Miguel, E.; Moreno-Cerviño, J.; Mingo-Gómez, M.T.; Hernando-Garijo, I.; Jiménez-Del-Barrio, S. Effects of Dry Needling in Teres Major Muscle in Elite Handball Athletes. A Randomised Controlled Trial. J. Clin. Med. 2021, 10, 4260. [Google Scholar] [CrossRef] [PubMed]
- Simons, D.G. Review of Enigmatic MTrPs as a Common Cause of Enigmatic Musculoskeletal Pain and Dysfunction. J. Electromyogr. Kinesiol. 2004, 14, 95–107. [Google Scholar] [CrossRef]
- Fleisig, G.S.; Andrews, J.R.; Dillman, C.J.; Escamilla, R.F. Kinetics of Baseball Pitching with Implications about Injury Mechanisms. Am. J. Sports Med. 1995, 23, 233–239. [Google Scholar] [CrossRef]
- De Sire, A.; Demeco, A.; Marotta, N.; Spanò, R.; Curci, C.; Farì, G.; Fortunato, F.; Iona, T.; Lippi, L.; Paolucci, T.; et al. Neuromuscular Impairment of Knee Stabilizer Muscles in a COVID-19 Cluster of Female Volleyball Players: Which Role for Rehabilitation in the Post-COVID-19 Return-to-Play? Appl. Sci. 2022, 12, 557. [Google Scholar] [CrossRef]
- Quinn, S.; Olivier, B.; Wood, W.-A. The Short-Term Effects of Trigger Point Therapy, Stretching and Medicine Ball Exercises on Accuracy and Back Swing Hip Turn in Elite, Male Golfers—A Randomised Controlled Trial. Phys. Ther. Sport 2016, 22, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Osborne, N.J.; Gatt, I.T. Management of Shoulder Injuries Using Dry Needling in Elite Volleyball Players. Acupunct. Med. 2010, 28, 42–45. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-del-Barrio, S.; Jiménez-Rejano, J.J.; Rebollo-Salas, M.; Mingo-Gómez, M.T.; Lorenzo-Muñoz, A.; Ceballos-Laita, L. Increased Tone and Stiffness of the Teres Major Muscle in Elite Handball Athletes: A Cross-Sectional Study. Appl. Sci. 2023, 13, 8457. [Google Scholar] [CrossRef]
- Bron, C.; Dommerholt, J.D. Etiology of Myofascial Trigger Points. Curr. Pain. Headache Rep. 2012, 16, 439–444. [Google Scholar] [CrossRef] [PubMed]
- De Sire, A.; Marotta, N.; Agostini, F.; Drago Ferrante, V.; Demeco, A.; Ferrillo, M.; Inzitari, M.T.; Pellegrino, R.; Russo, I.; Ozyemisci Taskiran, O.; et al. A Telerehabilitation Approach to Chronic Facial Paralysis in the COVID-19 Pandemic Scenario: What Role for Electromyography Assessment? J. Pers. Med. 2022, 12, 497. [Google Scholar] [CrossRef] [PubMed]
- Cagnie, B.; Dewitte, V.; Barbe, T.; Timmermans, F.; Delrue, N.; Meeus, M. Physiologic Effects of Dry Needling. Curr. Pain. Headache Rep. 2013, 17, 348. [Google Scholar] [CrossRef]
- Celik, D.; Yeldan, I. The Relationship between Latent Trigger Point and Muscle Strength in Healthy Subjects: A Double-Blind Study. J. Back Musculoskelet. Rehabil. 2011, 24, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Gerwin, R.D. Myofascial Trigger Point Pain Syndromes. Semin. Neurol. 2016, 36, 469–473. [Google Scholar] [CrossRef] [PubMed]
- Kalichman, L.; Vulfsons, S. Dry Needling in the Management of Musculoskeletal Pain. J. Am. Board Fam. Med. 2010, 23, 640–646. [Google Scholar] [CrossRef]
- Jiménez-del-Barrio, S.; Ceballos-Laita, L.; Lorenzo-Muñoz, A.; Mingo-Gómez, M.T.; Rebollo-Salas, M.; Jiménez-Rejano, J.J. Efficacy of Conservative Therapy in Overhead Athletes with Glenohumeral Internal Rotation Deficit: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 12, 4. [Google Scholar] [CrossRef]
- Rodine, R. Trigger Point Dry Needling: An Evidenced and Clinical-Based Approach. J. Can. Chiropr. Assoc. 2015, 59, 84. [Google Scholar]
- Dunning, J.; Butts, R.; Mourad, F.; Young, I.; Flannagan, S.; Perreault, T. Dry Needling: A Literature Review with Implications for Clinical Practice Guidelines. Phys. Ther. Rev. 2014, 19, 252–265. [Google Scholar] [CrossRef] [PubMed]
- Khosrawi, S.; Moghtaderi, A.; Haghighat, S. Acupuncture in Treatment of Carpal Tunnel Syndrome: A Randomized Controlled Trial Study. J. Res. Med. Sci. 2012, 17, 1–7. [Google Scholar] [PubMed]
- Kumnerddee, W.; Kaewtong, A. Efficacy of Acupuncture versus Night Splinting for Carpal Tunnel Syndrome: A Randomized Clinical Trial. J. Med. Assoc. Thail. 2010, 93, 1463–1469. [Google Scholar]
- Vas, J.; White, A. Evidence from RCTs on Optimal Acupuncture Treatment for Knee Osteoarthritis—An Exploratory Review. Acupunct. Med. 2007, 25, 29–35. [Google Scholar] [CrossRef] [PubMed]
- White, A.; Foster, N.E.; Cummings, M.; Barlas, P. Acupuncture Treatment for Chronic Knee Pain: A Systematic Review. Rheumatology 2007, 46, 384–390. [Google Scholar] [CrossRef] [PubMed]
- Witt, C.M.; Jena, S.; Brinkhaus, B.; Liecker, B.; Wegscheider, K.; Willich, S.N. Acupuncture in Patients with Osteoarthritis of the Knee or Hip: A Randomized, Controlled Trial with an Additional Nonrandomized Arm. Arthritis Rheum. 2006, 54, 3485–3493. [Google Scholar] [CrossRef]
- Green, S.; Buchbinder, R.; Hetrick, S. Acupuncture for Shoulder Pain. Cochrane Database Syst. Rev. 2005, 2, CD005319. [Google Scholar] [CrossRef] [PubMed]
- Tekin, L.; Akarsu, S.; Durmuş, O.; Çakar, E.; Dinçer, Ü.; Kıralp, M.Z. The Effect of Dry Needling in the Treatment of Myofascial Pain Syndrome: A Randomized Double-Blinded Placebo-Controlled Trial. Clin. Rheumatol. 2013, 32, 309–315. [Google Scholar] [CrossRef]
- DiLorenzo, L.; Traballesi, M.; Morelli, D.; Pompa, A.; Brunelli, S.; Buzzi, M.G.; Formisano, R. Hemiparetic Shoulder Pain Syndrome Treated with Deep Dry Needling During Early Rehabilitation: A Prospective, Open-Label, Randomized Investigation. J. Musculoskelet. Pain 2004, 12, 25–34. [Google Scholar] [CrossRef]
- De Sire, A.; Moggio, L.; Demeco, A.; Fortunato, F.; Spanò, R.; Aiello, V.; Marotta, N.; Ammendolia, A. Efficacy of Rehabilitative Techniques in Reducing Hemiplegic Shoulder Pain in Stroke: Systematic Review and Meta-Analysis. Ann. Phys. Rehabil. Med. 2022, 65, 101602. [Google Scholar] [CrossRef] [PubMed]
- Chys, M.; De Meulemeester, K.; De Greef, I.; Murillo, C.; Kindt, W.; Kouzouz, Y.; Lescroart, B.; Cagnie, B. Clinical Effectiveness of Dry Needling in Patients with Musculoskeletal Pain-An Umbrella Review. J. Clin. Med. 2023, 12, 1205. [Google Scholar] [CrossRef] [PubMed]
- Marotta, N.; de Sire, A.; Calafiore, D.; Agostini, F.; Lippi, L.; Curci, C.; Ferraro, F.; Bernetti, A.; Invernizzi, M.; Ammendolia, A. Impact of COVID-19 Era on the Anterior Cruciate Ligament Injury Rehabilitation: A Scoping Review. J. Clin. Med. 2023, 12, 5655. [Google Scholar] [CrossRef] [PubMed]
- Hong, C.Z. Lidocaine Injection versus Dry Needling to Myofascial Trigger Point. The Importance of the Local Twitch Response. Am. J. Phys. Med. Rehabil. 1994, 73, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Cummings, T.M.; White, A.R. Needling Therapies in the Management of Myofascial Trigger Point Pain: A Systematic Review. Arch. Phys. Med. Rehabil. 2001, 82, 986–992. [Google Scholar] [CrossRef] [PubMed]
- Tough, E.A.; White, A.R.; Cummings, T.M.; Richards, S.H.; Campbell, J.L. Acupuncture and Dry Needling in the Management of Myofascial Trigger Point Pain: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Eur. J. Pain 2009, 13, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Kietrys, D.M.; Palombaro, K.M.; Azzaretto, E.; Hubler, R.; Schaller, B.; Schlussel, J.M.; Tucker, M. Effectiveness of Dry Needling for Upper-Quarter Myofascial Pain: A Systematic Review and Meta-Analysis. J. Orthop. Sports Phys. Ther. 2013, 43, 620–634. [Google Scholar] [CrossRef] [PubMed]
- Furlan, A.D.; van Tulder, M.W.; Cherkin, D.C.; Tsukayama, H.; Lao, L.; Koes, B.W.; Berman, B.M. Acupuncture and Dry-Needling for Low Back Pain. Cochrane Database Syst. Rev. 2005, 1, CD001351. [Google Scholar] [CrossRef] [PubMed]
- Abbaszadeh-Amirdehi, M.; Ansari, N.N.; Naghdi, S.; Olyaei, G.; Nourbakhsh, M.R. Therapeutic Effects of Dry Needling in Patients with Upper Trapezius Myofascial Trigger Points. Acupunct. Med. 2017, 35, 85–92. [Google Scholar] [CrossRef]
- Thompson, R.; Prosell, M.; Timpka, T. Elite Athletes’ Experiences of Musculoskeletal Pain Management Using Neuroanatomical Dry Needling: A Qualitative Study in Swedish Track and Field. J. Sci. Med. Sport 2021, 24, 46–51. [Google Scholar] [CrossRef]
- Fleckenstein, J.; Banzer, W. A Review of Hands-on Based Conservative Treatments on Pain in Recreational and Elite Athletes. Sci. Sports 2019, 34, E77–E100. [Google Scholar] [CrossRef]
- Janowski, J.A.; Phelan-Smith, D.M.L.; Kroat Brady, M.N.; Michels, K.L.; Timm, A.H.; Boucher, N.M.; Casteen, K.D.; Village, D.; Sleeper, M.D. Acute Effects of Dry Needling on Myofascial Trigger Points in the Triceps Surae of Ballet Dancers: A Pilot Randomized Controlled Trial. Int. J. Sports Phys. Ther. 2021, 16, 418–430. [Google Scholar] [CrossRef] [PubMed]
- Jayaseelan, D.J.; Moats, N.; Ricardo, C.R. Rehabilitation of Proximal Hamstring Tendinopathy Utilizing Eccentric Training, Lumbopelvic Stabilization, and Trigger Point Dry Needling: 2 Case Reports. J. Orthop. Sports Phys. Ther. 2014, 44, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Roccuzzo, A.; Molinero-Mourelle, P.; Ferrillo, M.; Cobo-Vázquez, C.; Sanchez-Labrador, L.; Ammendolia, A.; Migliario, M.; de Sire, A. Type I Collagen-Based Devices to Treat Nerve Injuries after Oral Surgery Procedures. A Systematic Review. Appl. Sci. 2021, 11, 3927. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Kheradmandi, A.; Kamali, F.; Ebrahimian, M.; Abbasi, L. Comparison between Dry Needling plus Manual Therapy with Manual Therapy Alone on Pain and Function in Overhead Athletes with Scapular Dyskinesia: A Randomized Clinical Trial. J. Bodyw. Mov. Ther. 2021, 26, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Javed, M.A.; Saleem, S.; Hassan Raza, M.K. Management of Muscle Trigger Points Causing Subacromial Pain Using Dry Needling Technique—A Case Report. J. Pak. Med. Assoc. 2020, 70, 2270–2272. [Google Scholar] [CrossRef] [PubMed]
- Ceballos-Laita, L.; Jiménez-Rejano, J.J.; Rebollo-Salas, M.; Mingo-Gómez, M.T.; Hernández-Lázaro, H.; Jiménez-del-Barrio, S. Dry Needling versus Diacutaneous Fibrolysis for the Treatment of the Mechanical Properties of the Teres Major Muscle: A Randomized Clinical Trial. Appl. Sci. 2023, 13, 10995. [Google Scholar] [CrossRef]
- Demeco, A.; de Sire, A.; Marotta, N.; Palumbo, A.; Fragomeni, G.; Gramigna, V.; Pellegrino, R.; Moggio, L.; Petraroli, A.; Iona, T.; et al. Effectiveness of Rehabilitation through Kinematic Analysis of Upper Limb Functioning in Wheelchair Basketball Athletes: A Pilot Study. Appl. Sci. 2022, 12, 2929. [Google Scholar] [CrossRef]
- Keller, R.A.; De Giacomo, A.F.; Neumann, J.A.; Limpisvasti, O.; Tibone, J.E. Glenohumeral Internal Rotation Deficit and Risk of Upper Extremity Injury in Overhead Athletes: A Meta-Analysis and Systematic Review. Sports Health 2018, 10, 125–132. [Google Scholar] [CrossRef]
- Cools, A.M.J.; Vanderstukken, F.; Vereecken, F.; Duprez, M.; Heyman, K.; Goethals, N.; Johansson, F. Eccentric and Isometric Shoulder Rotator Cuff Strength Testing Using a Hand-Held Dynamometer: Reference Values for Overhead Athletes. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 3838–3847. [Google Scholar] [CrossRef] [PubMed]
- Moradi, M.; Hadadnezhad, M.; Letafatkar, A.; Khosrokiani, Z.; Baker, J.S. Efficacy of Throwing Exercise with TheraBand in Male Volleyball Players with Shoulder Internal Rotation Deficit: A Randomized Controlled Trial. BMC Musculoskelet. Disord. 2020, 21, 376. [Google Scholar] [CrossRef] [PubMed]
- Baraja-Vegas, L.; Martin-Rodriguez, S.; Piqueras-Sanchiz, F.; Martin-Ruiz, J.; Yeste Fabregat, M.; Florencio, L.L.; Fernandez-de-las-Penas, C. Electromyographic Activity Evolution of Local Twitch Responses During Dry Needling of Latent Trigger Points in the Gastrocnemius Muscle: A Cross-Sectional Study. Pain Med. 2020, 21, 1224–1229. [Google Scholar] [CrossRef] [PubMed]
- Mason, J.S.; Crowell, M.; Dolbeer, J.; Morris, J.; Terry, A.; Koppenhaver, S.; Goss, D.L. The effectiveness of dry needling and stretching vs. Stretching alone on hamstring flexibility in patients with knee pain: A randomized controlled trial. Int. J. Sports Phys. Ther. 2016, 11, 672–683. [Google Scholar] [PubMed]
- Schneider, E.; Moore, E.S.; Stanborough, R.; Slaven, E. Effects of Trigger Point Dry Needling on Strength Measurements and Activation Levels of the Gluteus Medius: A Quasi-Experimental Randomized Control Study. Int. J. Sports Phys. Ther. 2022, 17, 1404–1416. [Google Scholar] [CrossRef]
- Haser, C.; Stöggl, T.; Kriner, M.; Mikoleit, J.; Wolfahrt, B.; Scherr, J.; Halle, M.; Pfab, F. Effect of Dry Needling on Thigh Muscle Strength and Hip Flexion in Elite Soccer Players. Med. Sci. Sports Exerc. 2017, 49, 378. [Google Scholar] [CrossRef] [PubMed]
- Bazzaz-Yamchi, M.; Naghdi, S.; Nakhostin-Ansari, A.; Hadizadeh, M.; Ansari, N.N.; Moghimi, E.; Hasson, S. Acute and Short-Term Effects of Dry Needling in Patients with Chronic Nonspecific Low Back Pain and Hamstring Tightness: A Pilot Study. Sci. World J. 2021, 2021, 7259956. [Google Scholar] [CrossRef]
- Albin, S.R.; Koppenhaver, S.L.; MacDonald, C.W.; Capoccia, S.; Ngo, D.; Phippen, S.; Pineda, R.; Wendlandt, A.; Hoffman, L.R. The Effect of Dry Needling on Gastrocnemius Muscle Stiffness and Strength in Participants with Latent Trigger Points. J. Electromyogr. Kinesiol. 2020, 55, 102479. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Huang, Q.-M.; Liu, Q.-G.; Ye, G.; Bo, C.-Z.; Chen, M.-J.; Li, P. Effectiveness of Dry Needling for Myofascial Trigger Points Associated with Neck and Shoulder Pain: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2015, 96, 944–955. [Google Scholar] [CrossRef]
- Lee, S.-H.; Chen, C.-C.; Lee, C.-S.; Lin, T.-C.; Chan, R.-C. Effects of Needle Electrical Intramuscular Stimulation on Shoulder and Cervical Myofascial Pain Syndrome and Microcirculation. J. Chin. Med. Assoc. 2008, 71, 200–206. [Google Scholar] [CrossRef]
- Baraja-Vegas, L.; Martín-Rodríguez, S.; Piqueras-Sanchiz, F.; Faundez-Aguilera, J.; Bautista, I.J.; Barrios, C.; Garcia-Escudero, M.; Fernández-de-Las-Peñas, C. Localization of Muscle Edema and Changes on Muscle Contractility After Dry Needling of Latent Trigger Points in the Gastrocnemius Muscle. Pain Med. 2019, 20, 1387–1394. [Google Scholar] [CrossRef] [PubMed]
- Lundberg, T.R.; Howatson, G. Analgesic and Anti-Inflammatory Drugs in Sports: Implications for Exercise Performance and Training Adaptations. Scand. J. Med. Sci. Sports 2018, 28, 2252–2262. [Google Scholar] [CrossRef] [PubMed]
- Holgado, D.; Hopker, J.; Sanabria, D.; Zabala, M. Analgesics and Sport Performance: Beyond the Pain-Modulating Effects. PM&R 2018, 10, 72–82. [Google Scholar] [CrossRef] [PubMed]
| PubMed ((dry needling) OR (dny)) AND ((sport) OR (overhead athletes)) AND ((pain) OR (trigger point)) Scopus TITLE-ABS-KEY (“dry needling” OR “dny”) AND (“sport” OR “overhead athletes”) AND (“pain”OR “ trigger point”) Web of Science (“dry needling” OR “dny”) AND (“sport” OR “overhead athletes”) AND (“pain”OR “ trigger point”) |
| Author | Design | Patients | Inclusion Criteria | TG | CG | Outcome | Main Finding |
|---|---|---|---|---|---|---|---|
| Kheradmandi et al., [56], 2021 | RCT | N = 40 15 M/25 F Age: 18–45 y.o. DNY group = 32.2 ± 8.35 y.o.; Control group = 31.80 ± 6.85 y.o. |
| Scapular mobilization at 3 sets of 10 repetitions with a 30 s rest between each set + DNY Three sessions for each patient with the interval of every three days | Only MT | NRS; DASH; PPT; SD | Reduction in pain (p < 0.001) and disability (p = 0.02) with significant improvement in scapular dyskinesia in treatment group (p = 0.02). PPT significantly increased in the control group (p = 0.004). No adverse effects reported by the participants during this study. |
| Ceballos et al. [17], 2021 | RCT | N = 30 M; Age: 22.39 ± 3.73 y.o. DNY group = 22.47 ± 3.04 y.o.; Control group = 22.31 ± 4.37 y.o. |
| DNY teres major | No intervention | NRS; ROM (inclinometer); Isometric strength (hand-held dynamometer); Extensibility (inclinometer) | Improvement in pain. External rotation and internal rotation in the DNY group. |
| Javed et al., [57], 2020 | Case study | N = 1 M Age: 22 y.o. |
| DNY supraspinatus + heating pads to enhance the blood supply of the area and for analgesic effect + Progressive resistance training exercise | None | ROM (goniometer and inclinometer); VAS | Improvement in ROM and pain (VAS). |
| Khamali et al. [16], 2019 | RCT | N = 40; 20 M/20 F; Age: 18–60; 36 ± 16 y.o. |
| DNY ISP | DNY UT | VAS; PPT; Dash | Pain and disability decreased significantly in both groups. Ppt increase only in infraspinatus. |
| Osborne et al. [22], 2010 | Case study | N = 4 F Age: 25 ± 2 y.o. |
| 1 DNY session (subject 2 receive 2 sessions of DNY) + post-training icing, exercises and stretching. | None | ROM (goniometer); McGill Pain Questionnaire; Verbal pain score | Improvement in ROM and functional pain scores. |
| Jiménez-del-Barrio et al. [58], 2023 | RCT | N = 30; 30 M; Age: 25.83 ± 5.39 y.o. |
| 1 DNY session | 1 DF session | ROM (inclinometer); Muscle stiffness | No between-group difference. |
| Article | Criteria for the Quality Scoring | Score | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
| Kheradmandi et al. [56], 2021 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| Ceballos et al. [17], 2021 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| Javed et al. [57], 2020 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 7 |
| Khamali et al. [16], 2019 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 9 |
| Osborne et al. [22], 2010 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 6 |
| Jiménez-del-Barrio et al. [58], 2023 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Demeco, A.; de Sire, A.; Salerno, A.; Marotta, N.; Palermi, S.; Frizziero, A.; Costantino, C. Dry Needling in Overhead Athletes with Myofascial Shoulder Pain: A Systematic Review. Sports 2024, 12, 156. https://doi.org/10.3390/sports12060156
Demeco A, de Sire A, Salerno A, Marotta N, Palermi S, Frizziero A, Costantino C. Dry Needling in Overhead Athletes with Myofascial Shoulder Pain: A Systematic Review. Sports. 2024; 12(6):156. https://doi.org/10.3390/sports12060156
Chicago/Turabian StyleDemeco, Andrea, Alessandro de Sire, Antonello Salerno, Nicola Marotta, Stefano Palermi, Antonio Frizziero, and Cosimo Costantino. 2024. "Dry Needling in Overhead Athletes with Myofascial Shoulder Pain: A Systematic Review" Sports 12, no. 6: 156. https://doi.org/10.3390/sports12060156
APA StyleDemeco, A., de Sire, A., Salerno, A., Marotta, N., Palermi, S., Frizziero, A., & Costantino, C. (2024). Dry Needling in Overhead Athletes with Myofascial Shoulder Pain: A Systematic Review. Sports, 12(6), 156. https://doi.org/10.3390/sports12060156











