Clinical Impact of Admission Day on Outcomes in Acutely Decompensated Aortic Stenosis: A Nationwide Analysis
Abstract
1. Introduction
2. Materials and Methods
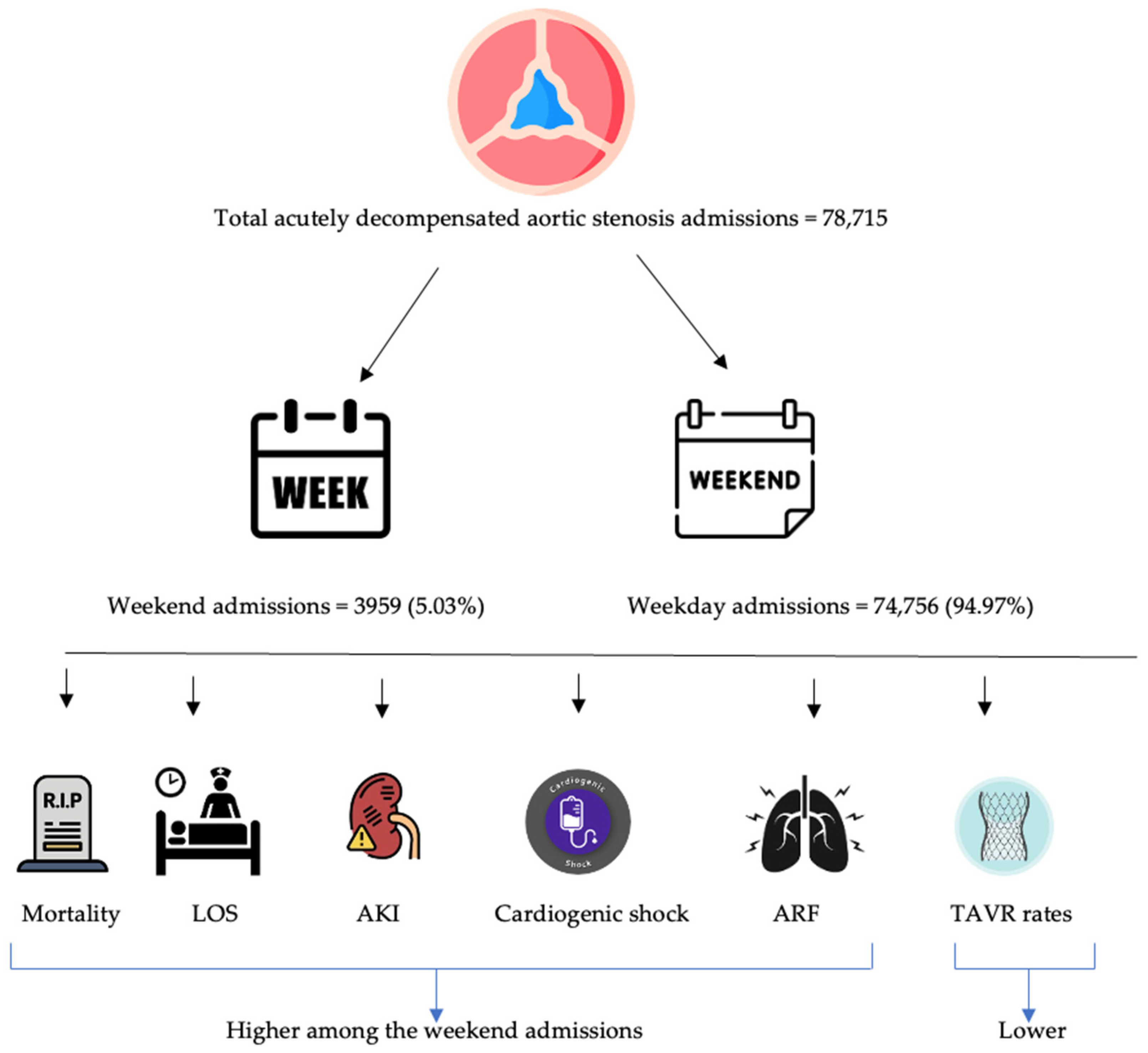
3. Results
3.1. Patient Characteristics
3.2. Primary Outcome: Mortality
3.3. Secondary Outcomes
3.3.1. Resource Utilization: Length of Stay and Hospital Charges
3.3.2. Complications
3.3.3. Rates of Transcatheter Aortic Valve Replacement (TAVR) During the Hospitalization
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- D’Arcy, J.L.; Coffey, S.; Loudon, M.A.; Kennedy, A.; Pearson-Stuttard, J.; Birks, J.; Frangou, E.; Farmer, A.J.; Mant, D.; Wilson, J.; et al. Large-scale community echocardiographic screening reveals a major burden of undiagnosed valvular heart disease in older people: The OxVALVE Population Cohort Study. Eur. Heart J. 2016, 37, 3515–3522. [Google Scholar] [CrossRef] [PubMed]
- Osnabrugge, R.L.; Mylotte, D.; Head, S.J.; Van Mieghem, N.M.; Nkomo, V.T.; LeReun, C.M.; Bogers, A.J.; Piazza, N.; Kappetein, A.P. Aortic stenosis in the elderly: Disease prevalence and number of candidates for transcatheter aortic valve replacement: A meta-analysis and modeling study. J. Am. Coll. Cardiol. 2013, 62, 1002–1012. [Google Scholar] [CrossRef] [PubMed]
- Généreux, P.; Stone, G.W.; O’gara, P.T.; Marquis-Gravel, G.; Redfors, B.; Giustino, G.; Pibarot, P.; Bax, J.J.; Bonow, R.O.; Leon, M.B. Natural History, Diagnostic Approaches, and Therapeutic Strategies for Patients with Asymptomatic Severe Aortic Stenosis. J. Am. Coll. Cardiol. 2016, 67, 2263–2288. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, R.A.; Otto, C.M.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P., III; Fleisher, L.A.; Jneid, H.; Mack, M.J.; McLeod, C.J.; O’Gara, P.T.; et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients with Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2017, 70, 252–289. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Baumann, P.; Manthey, J.; Hoffmann, M.; Schuler, G.; Mehmel, H.C.; Schmitz, W.; Kübler, W. The effect of aortic valve replacement on survival. Circulation 1982, 66, 1105–1110. [Google Scholar] [CrossRef] [PubMed]
- Horinouchi, H.; Nagai, T.; Ohno, Y.; Miyamoto, J.; Murakami, T.; Kamioka, N.; Yoshioka, K.; Ikari, Y. Short-term Outcomes of Urgent Transcatheter Aortic Valve Replacement in Symptomatic Aortic Stenosis That Requires Emergency Hospital Admission. Intern. Med. 2023, 62, 2457–2463. [Google Scholar] [CrossRef] [PubMed]
- Abdelaziz, M.; Khogali, S.; Cotton, J.M.; Meralgia, A.; Matuszewski, M.; Luckraz, H. Transcatheter aortic valve implantation in decompensated aortic stenosis within the same hospital admission: Early clinical experience. Open Heart 2018, 5, e000827. [Google Scholar] [CrossRef] [PubMed]
- Antia, A.; Ndukauba, C.; Pius, R.; Gbegbaje, O.; Ong, K. Impact of day of admission on in-hospital outcomes of cardiogenic shock. Curr. Probl. Cardiol. 2024, 49, 102140. [Google Scholar] [CrossRef] [PubMed]
- Altujjar, M.; Khokher, W.; Sajdeya, O.; Hennessey, K.C.; Henkin, S.; Andrus, B.W.; Taub, C.C. Weekend effect on patients presenting with cardiac arrest: A nationwide analysis. J. Am. Coll. Cardiol. 2022, 79, 1040. [Google Scholar] [CrossRef]
- Mounsey, L.A.; Chang, P.P.; Sueta, C.A.; Matsushita, K.; Russell, S.D.; Caughey, M.C. In-Hospital and Postdischarge Mortality Among Patients with Acute Decompensated Heart Failure Hospitalizations Ending on the Weekend Versus Weekday: The ARIC Study Community Surveillance. J. Am. Heart Association. Cardiovasc. Cerebrovasc. Dis. 2019, 8, e011631. [Google Scholar] [CrossRef] [PubMed]
- Bell, C.M.; Redelmeier, D.A. Mortality among Patients Admitted to Hospitals on Weekends as Compared with Weekdays. N. Engl. J. Med. 2001, 345, 663–668. [Google Scholar] [CrossRef] [PubMed]
- Horwich, T.B.; Hernandez, A.F.; Liang, L.; Albert, N.M.; LaBresh, K.A.; Yancy, C.W.; Fonarow, G.C. Weekend hospital admission and discharge for heart failure: Association with quality of care and clinical outcomes. Am. Heart J. 2009, 158, 451–458. [Google Scholar] [CrossRef]
- Khoshchehreh, M.; Groves, E.M.; Tehrani, D.; Amin, A.; Patel, P.M.; Malik, S. Changes in mortality on weekend versus weekday admissions for Acute Coronary Syndrome in the United States over the past decade. Int. J. Cardiol. 2016, 210, 164–172. [Google Scholar] [CrossRef] [PubMed]
- Pauls, L.A.; Johnson-Paben, R.; McGready, J.; Murphy, J.D.; Pronovost, P.J.; Wu, C.L. The Weekend Effect in Hospitalized Patients: A Meta-Analysis. J. Hosp. Med. 2017, 12, 760–766. [Google Scholar] [CrossRef] [PubMed]
- Lindman, B.R.; Bonow, R.O.; Otto, C.M. Current management of calcific aortic stenosis. Circ. Res. 2013, 113, 223–237. [Google Scholar] [CrossRef] [PubMed]
- Ye, J.; Soon, J.L.; Webb, J. Aortic valve replacement vs. transcatheter aortic valve implantation: Patient selection. Ann. Cardiothorac. Surg. 2012, 1, 194–199. [Google Scholar] [CrossRef] [PubMed]
- Roule, V.; Rebouh, I.; Lemaitre, A.; Sabatier, R.; Blanchart, K.; Briet, C.; Bignon, M.; Beygui, F. Impact of wait times on late postprocedural mortality after successful transcatheter aortic valve replacement. Sci. Rep. 2022, 12, 5967. [Google Scholar] [CrossRef] [PubMed]
- Ascandar, N.; Williamson, C.; Bakhtiyar, S.S.; Chervu, N.; Benharash, P. TCT-454 Impact of Weekend Admission on Outcomes After Nonelective TAVR. JACC 2022, 80 (Suppl. 12), B183. [Google Scholar] [CrossRef]
- Ryan, K.; Levit, K.; Davis, P.H. Characteristics of Weekday and Weekend Hospital Admissions. 2010 Mar. In Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2006; Statistical Brief #87. Available online: https://www.ncbi.nlm.nih.gov/books/NBK53602/ (accessed on 24 September 2024).
- Camiat, F.; Restrepo, M.I.; Chauny, J.-M.; Lahrichi, N.; Rousseau, L.-M. Productivity-driven physician scheduling in emergency departments. Health Syst. 2019, 10, 104–117. [Google Scholar] [CrossRef] [PubMed]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.-M.; Sundararajan, V. Updating and Validating the Charlson Comorbidity Index and Score for Risk Adjustment in Hospital Discharge Abstracts Using Data From 6 Countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef] [PubMed]

| Weekend Admission | Weekday Admission | p Value * | |
|---|---|---|---|
| Patient characteristics | |||
| No. (%) of patients | 3959 (5.03) | 74756 (94.97) | |
| Age (mean) | 78.13 ± 0.36 | 77.93 ± 0.09 | 0.59 |
| Female gender (%) | 46.52 | 42.62 | 0.03 |
| Race (%) | <0.01 | ||
| Caucasian | 78.41 | 86.98 | |
| African American | 7.02 | 4.27 | |
| Hispanic | 8.58 | 4.97 | |
| Asian or Pacific islander | 2.86 | 1.42 | |
| Native American | 0.65 | 0.26 | |
| Others | 2.47 | 2.1 | |
| Median Income in patients Zip code (%) | 0.09 | ||
| USD 1–USD 47,999 | 26 | 22.01 | |
| USD 48,000–USD 60,999 | 25.36 | 27.46 | |
| USD 61,000–81,999 | 25.1 | 25.62 | |
| ≥USD 82,000 | 23.54 | 24.92 | |
| Charlson comorbidity index (%) | <0.01 | ||
| 0 | 5.82 | 8.89 | |
| 1 | 14.29 | 21.05 | |
| 2 | 19.22 | 20.35 | |
| 3 or more | 60.68 | 49.71 |
| Weekend Admission | Weekday Admission | p Value * | |
|---|---|---|---|
| Hospital Region | 0.21 | ||
| Northeast | 21.74 | 22.09 | |
| Midwest | 19.34 | 22.82 | |
| South | 38.18 | 34.99 | |
| West | 20.73 | 20.1 | |
| Hospital Bed size (%) | 0.01 | ||
| Small | 14.03 | 9.51 | |
| Medium | 24.65 | 23.53 | |
| Large | 61.31 | 66.96 | |
| Hospital Location (%) | 0.12 | ||
| Rural | 3.79 | 2.25 | |
| Urban | 96.21 | 97.75 | |
| Hospital Teaching (%) | 0.01 | ||
| Non-teaching (%) | 16.31 | 12.66 | |
| Teaching (%) | 83.69 | 87.34 | |
| Insurance type (%) | <0.01 | ||
| Medicaid | 83.38 | 87.93 | |
| Medicare | 4.16 | 1.6 | |
| Private | 10.13 | 9.9 | |
| Uninsured | 2.34 | 0.58 |
| Outcomes | Weekend (%) (aOR; 95% CI) | Weekday (%) | p Value |
|---|---|---|---|
| a. Primary Outcome | |||
| Mortality | 3.67 (2.23, 1.49–3.35) | 1.51 (ref) | <0.001 * |
| b. Secondary Outcomes | |||
| Cardiac arrest | 1.52 (1.75; 0.96–3.20) | 0.82 (ref) | 0.07 |
| Cardiogenic shock | 4.68 (2.76; 1.94–3.92) | 1.53 (ref) | <0.001 * |
| Acute kidney injury | 23.26 (2.48; 2.29–3.39) | 8.84 (ref) | <0.001 * |
| Acute respiratory failure | 17.7 (3.27; 2.63–4.06) | 5.54 (ref) | <0.001 * |
| TAVR | 33.25 (0.11; 0.09–0.14) | 52.14 (ref) | <0.001 * |
| Valvuloplasty | 5.44 (1.39; 0.96–1.81) | 3.96 (ref) | 0.09 |
| Outcomes | Weekend (Mean) 95% CI | Weekday (Mean) 95% CI | p Value |
|---|---|---|---|
| b. Secondary Outcomes | |||
| Length of stay (days) | 6.98 (6.49–7.47) | 3.80 (3.69–3.91) | <0.001 * |
| Hospitalization charges (USD) | 168,594.2 (153,019.2–184,169.3) | 200,608 (192,446.3–208,769.6) | 0.23 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bansal, N.; Kwak, E.S.; Alqadi, M.; Qiu, S.; Assaly, R. Clinical Impact of Admission Day on Outcomes in Acutely Decompensated Aortic Stenosis: A Nationwide Analysis. J. Pers. Med. 2024, 14, 1118. https://doi.org/10.3390/jpm14121118
Bansal N, Kwak ES, Alqadi M, Qiu S, Assaly R. Clinical Impact of Admission Day on Outcomes in Acutely Decompensated Aortic Stenosis: A Nationwide Analysis. Journal of Personalized Medicine. 2024; 14(12):1118. https://doi.org/10.3390/jpm14121118
Chicago/Turabian StyleBansal, Nahush, Eun Seo Kwak, Mohammad Alqadi, Shuhao Qiu, and Ragheb Assaly. 2024. "Clinical Impact of Admission Day on Outcomes in Acutely Decompensated Aortic Stenosis: A Nationwide Analysis" Journal of Personalized Medicine 14, no. 12: 1118. https://doi.org/10.3390/jpm14121118
APA StyleBansal, N., Kwak, E. S., Alqadi, M., Qiu, S., & Assaly, R. (2024). Clinical Impact of Admission Day on Outcomes in Acutely Decompensated Aortic Stenosis: A Nationwide Analysis. Journal of Personalized Medicine, 14(12), 1118. https://doi.org/10.3390/jpm14121118






