Home-Based Virtual Reality Exercise and Resistance Training for Enhanced Cardiorespiratory Fitness in Community-Dwelling Older People with Sarcopenia: A Randomized, Double-Blind Controlled Trial
Abstract
1. Introduction
2. Subjects and Methods
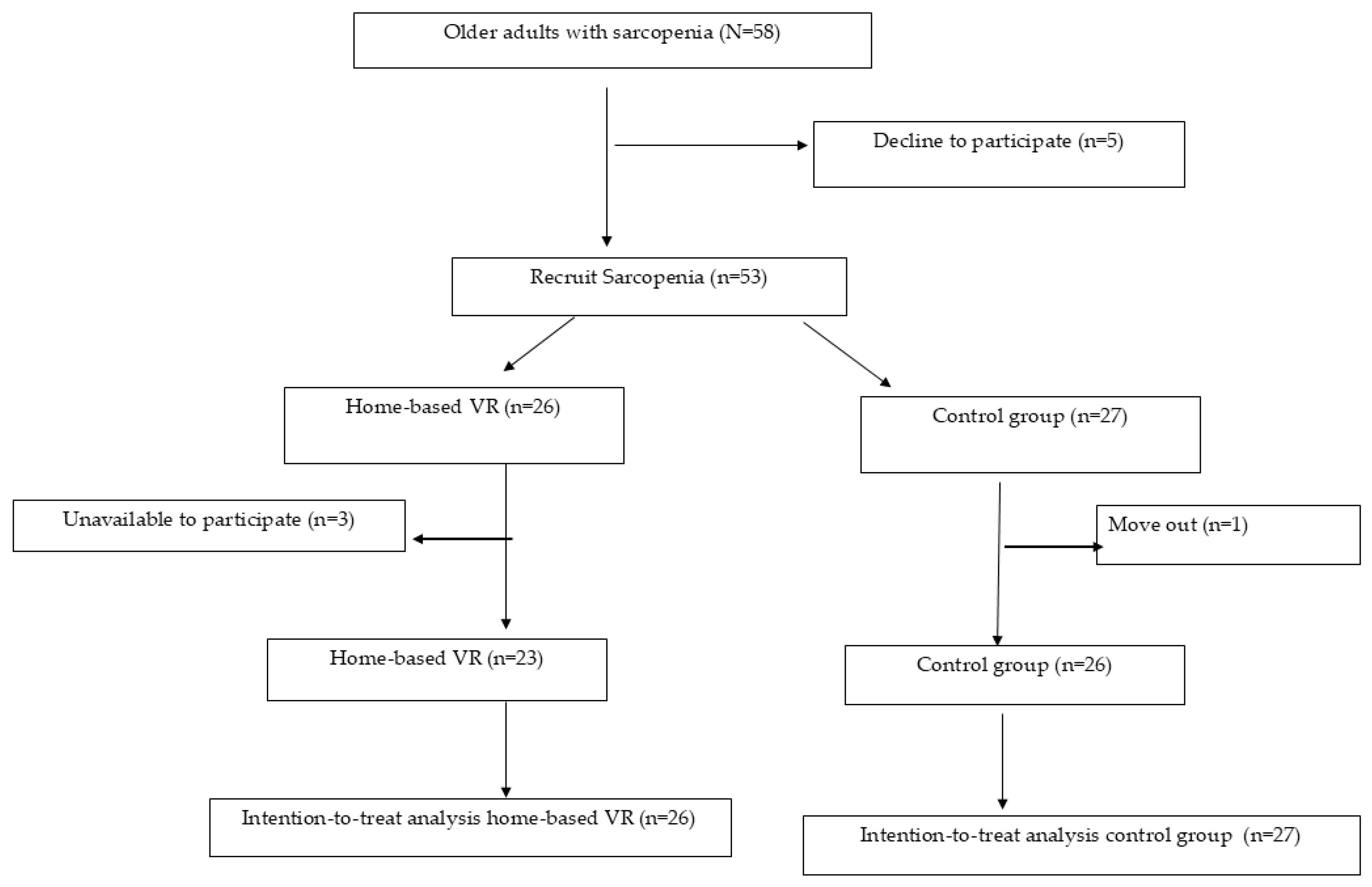
2.1. Participants
2.2. Intervention Program
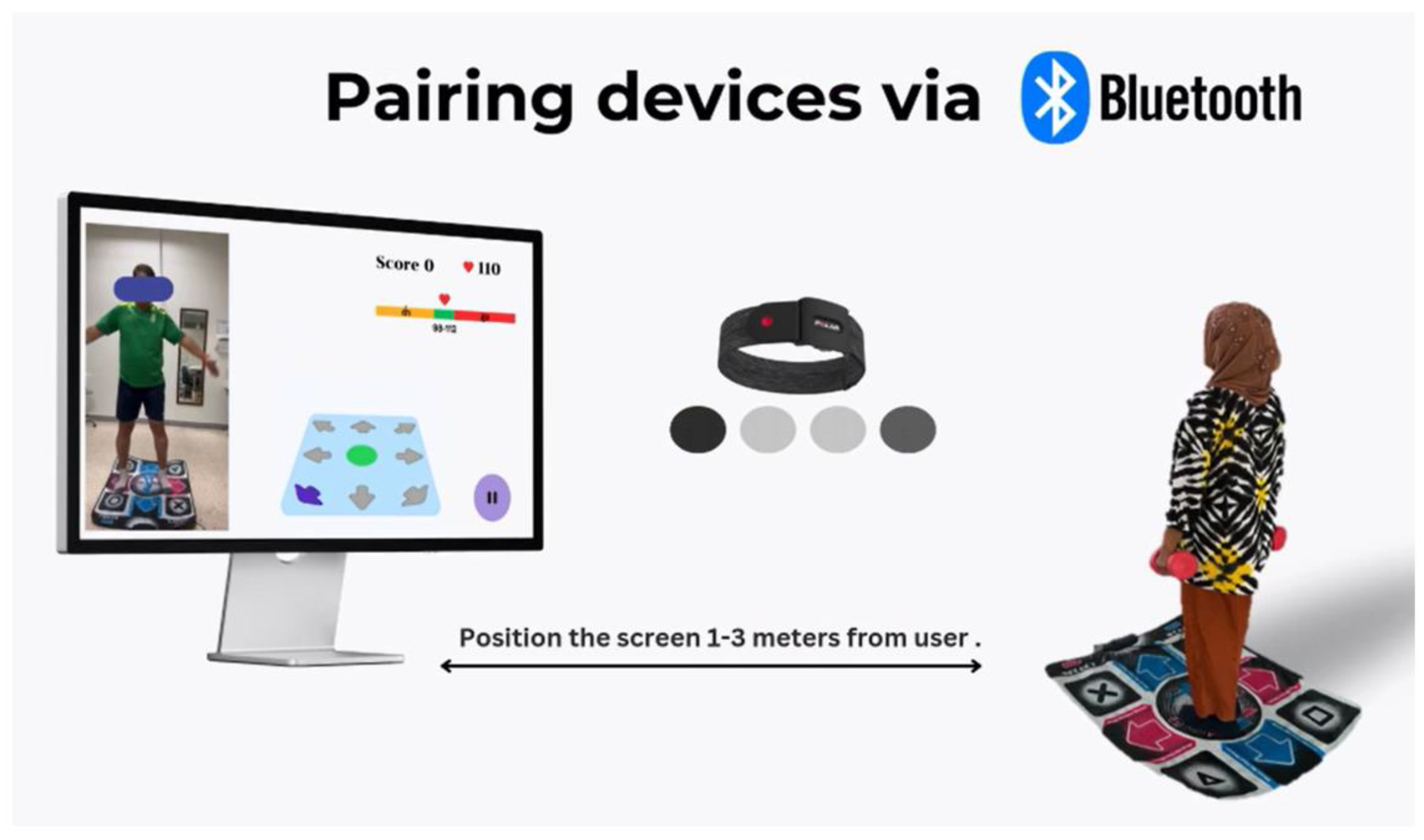
- MiniPC Android board, a board used to install the software
- Wireless Dance Mats Pad (OSTENT USB Non-Slip Dancing Step Dance Mat Pad Blanket, Mainland China; size: 930 × 830 × 80 mm)
- Revolution Non-Slip Footprint Mat connected to a PC through USB
- Air Mouse G10S (wireless 2.4 G): remote control
- Screen with HDMI capability (TV/Computer/Notebook screen size > 15 in) to show the VR coach and monitor heart rate on the screen.
- Polar Verity Sense OH1 (Optical Heart Rate Sensor: Polar Electro, Kempele, Finland)
- ANT+™: Armband (Cochrane, AB, Canada), connected through Bluetooth to monitor heart rate in real-time while exercising within a suitable range with the user-specific exercise program.
2.3. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Ageing and Health. 2024. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 3 March 2025).
- Jubrias, S.A.; Odderson, I.R.; Esselman, P.C.; Conley, K.E. Decline in isokinetic force with age: Muscle cross-sectional area and specific force. Pflug. Arch. 1997, 434, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Keller, K.; Engelhardt, M. Strength and muscle mass loss with aging process. Age Strength loss. Muscles Ligaments Tendons J. 2014, 3, 346–350. [Google Scholar] [CrossRef]
- Yuenyongchaiwat, K.; Akekawatchai, C. Prevalence and incidence of sarcopenia and low physical activity among community-dwelling older Thai people: A preliminary prospective cohort study 2-year follow-up. PeerJ 2022, 10, e13320. [Google Scholar] [CrossRef]
- Yuenyongchaiwat, K.; Boonsinsukh, R. Sarcopenia and Its Relationships with Depression, Cognition, and Physical Activity in Thai Community-Dwelling Older Adults. Curr. Gerontol. Geriatr. Res. 2020, 2020, 8041489. [Google Scholar] [CrossRef] [PubMed]
- El-Sebaie, M.; Elwakil, W. Biomarkers of sarcopenia: An unmet need. Egypt. Rheumatol. Rehabil. 2023, 50, 45. [Google Scholar] [CrossRef]
- Boontanom, N.; Kooncumchoo, P.; Yuenyongchaiwat, K. Cardiorespiratory Performance, Physical Activity, and Depression in Thai Older Adults with Sarcopenia and No Sarcopenia: A Matched Case-Control Study. Int. J. Environ. Res. Public Health 2024, 21, 724. [Google Scholar] [CrossRef]
- Lu, L.; Mao, L.; Feng, Y.; Ainsworth, B.E.; Liu, Y.; Chen, N. Effects of different exercise training modes on muscle strength and physical performance in older people with sarcopenia: A systematic review and meta-analysis. BMC Geriatr. 2021, 21, 708. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Shi, Q.; Nong, K.; Li, S.; Yue, J.; Huang, J.; Dong, B.; Beauchamp, M.; Hao, Q. Exercise for sarcopenia in older people: A systematic review and network meta-analysis. J. Cachexia Sarcopenia Muscle 2023, 14, 1199–1211. [Google Scholar] [CrossRef]
- Boileau, R.A.; McAuley, E.; Demetriou, D.; Devabhaktuni, N.K.; Dykstra, G.L.; Katula, J.; Nelson, J.; Pascale, A.; Pena, M.; Talbot, H.-M. Aerobic Exercise Training and Cardiorespiratory Fitness in Older Adults: A Randomized Control Trial. J. Aging Phys. Act. 1999, 7, 374–383. [Google Scholar] [CrossRef]
- Peterson, M.D.; Rhea, M.R.; Sen, A.; Gordon, P.M. Resistance exercise for muscular strength in older adults: A meta-analysis. Ageing Res. Rev. 2010, 9, 226–237. [Google Scholar] [CrossRef]
- Smart, T.F.F.; Doleman, B.; Hatt, J.; Paul, M.; Toft, S.; Lund, J.N.; E Phillips, B. The role of resistance exercise training for improving cardiorespiratory fitness in healthy older adults: A systematic review and meta-analysis. Age Ageing 2022, 51, afac143. [Google Scholar] [CrossRef]
- Collado-Mateo, D.; Lavín-Pérez, A.; Peñacoba, C.; Del Coso, J.; Leyton-Román, M.; Luque-Casado, A.; Gasque, P.; Fernández-Del-Olmo, M.; Amado-Alonso, D. Key Factors Associated with Adherence to Physical Exercise in Patients with Chronic Diseases and Older Adults: An Umbrella Review. Int. J. Environ. Res. Public Health 2021, 18, 2023. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Zhang, H.; Wang, H.Y.; Liu, L.F.; Zhang, X.G. Barriers and facilitators to older adult participation in intergenerational physical activity program: A systematic review. Aging Clin. Exp. Res. 2024, 36, 39. [Google Scholar] [CrossRef]
- Xu, L.; Li, F.; Zhou, C.; Li, J.; Hong, C.; Tong, Q. The effect of mobile applications for improving adherence in cardiac rehabilitation: A systematic review and meta-analysis. BMC Cardiovasc. Disord. 2019, 19, 166. [Google Scholar] [CrossRef] [PubMed]
- Song, X.; Ali, N.M.; Mhd Salim, M.H.; Rezaldi, M.Y. A Literature Review of Virtual Reality Exergames for Older Adults: Enhancing Physical, Cognitive, and Social Health. Appl. Sci. 2025, 15, 351. [Google Scholar] [CrossRef]
- Liu, W.; Zeng, N.; Pope, Z.C.; McDonough, D.J.; Gao, Z. Acute Effects of Immersive Virtual Reality Exercise on Young Adults’ Situational Motivation. J. Clin. Med. 2019, 8, 1947. [Google Scholar] [CrossRef]
- Chen, G.-B.; Lin, C.-W.; Huang, H.-Y.; Wu, Y.-J.; Su, H.-T.; Sun, S.-F.; Tuan, S.-H. Using Virtual Reality-Based Rehabilitation in Sarcopenic Older Adults in Rural Health Care Facilities-A Quasi-Experimental Study. J. Aging Phys. Act. 2021, 29, 866–877. [Google Scholar] [CrossRef]
- Lee, Y.H.; Lin, C.H.; Wu, W.R.; Chiu, H.Y.; Huang, H.C. Virtual reality exercise programs ameliorate frailty and fall risks in older adults: A meta-analysis. J. Am. Geriatr. Soc. 2023, 71, 2946–2955. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.-K.; Woo, J.; Assantachai, P.; Auyeung, T.-W.; Chou, M.-Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e2. [Google Scholar] [CrossRef]
- Hemrungrojn, S.; Tangwongchai, S.; Charoenboon, T.; Panasawat, M.; Supasitthumrong, T.; Chaipresertsud, P.; Maleevach, P.; Likitjaroen, Y.; Phanthumchinda, K.; Maes, M. Use of the Montreal Cognitive Assessment Thai Version to Discriminate Amnestic Mild Cognitive Impairment from Alzheimer’s Disease and Healthy Controls: Machine Learning Results. Dement. Geriatr. Cogn. Disord. 2021, 50, 183–194. [Google Scholar] [CrossRef]
- Nambi, G.; Abdelbasset, W.K.; Alrawaili, S.M.; Elsayed, S.H.; Verma, A.; Vellaiyan, A.; Eid, M.M.; Aldhafian, O.R.; Bin Nwihadh, N.; Saleh, A.K. Comparative effectiveness study of low versus high-intensity aerobic training with resistance training in community-dwelling older men with post-COVID 19 sarcopenia: A randomized controlled trial. Clin. Rehabil. 2022, 36, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Umakanth, S.; Girish, N. A review of the components of exercise prescription for sarcopenic older adults. Eur. Geriatr. Med. 2022, 13, 1245–1280. [Google Scholar] [CrossRef]
- American College of Sports Medicine. The American College of Sports Medicine (ACSM) ’s Guidelines for Exercise Testing and Prescription (American College of Sports Medicine), 10th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2018. [Google Scholar]
- American Thoracic Society/European Respiratory Society. ATS/ERS Statement on respiratory muscle testing. Am. J. Respir. Crit. Care Med. 2002, 166, 518–624. [Google Scholar] [CrossRef]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the Six-Minute Walk Test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef]
- Cho, H.E. Understanding Changes in the Respiratory System with Ageing. Ann. Cardiopulm. Rehabil. 2023, 3, 27–34. [Google Scholar] [CrossRef]
- Sato, S.; Miyazaki, S.; Tamaki, A.; Yoshimura, Y.; Arai, H.; Fujiwara, D.; Katsura, H.; Kawagoshi, A.; Kozu, R.; Maeda, K.; et al. Respiratory sarcopenia: A position paper by four professional organizations. Geriatr. Gerontol. Int. 2023, 23, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Elliott, J.E.; Greising, S.M.; Mantilla, C.B.; Sieck, G.C. Functional impact of sarcopenia in respiratory muscles. Respir. Physiol. Neurobiol. 2016, 226, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Pessoa, M.F.; Brandão, D.C.; de Sá, R.B.; Barcelar, J.d.M.; Rocha, T.D.d.S.; de Souza, H.C.M.; de Andrade, A.D. Vibrating Platform Training Improves Respiratory Muscle Strength, Quality of Life, and Inspiratory Capacity in the Elderly Adults: A Randomized Controlled Trial. J. Gerontol. A Biol. Sci. Med. Sci. 2017, 72, 683–688. [Google Scholar] [CrossRef]
- Yuenyongchaiwat, K.; Akekawatchai, C. Beneficial effects of walking-based home program for improving cardio-respiratory performance and physical activity in sarcopenic older people: A randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2022, 58, 838–844. [Google Scholar] [CrossRef]
- Cebrià IIranzo, M.À.; Balasch-Bernat, M.; Tortosa-Chuliá, M.Á.; Balasch-Parisi, S. Effects of Resistance Training of Peripheral Muscles Versus Respiratory Muscles in Older Adults with Sarcopenia Who are Institutionalized: A Randomized Controlled Trial. J. Aging Phys. Act. 2018, 26, 637–646. [Google Scholar] [CrossRef]
- Salepçi, B.; Güngör, G.A.; Parmaksız, E.T.; Fidan, A.; Kıral, N.; Cömert, S.S.; Doğan, C. Expiratory and Inspiratory Muscle Functions in Obstructive Sleep Apnea Syndrome. J. Turk. Sleep Med. 2016, 3, 65–68. [Google Scholar] [CrossRef]
- Flor-Rufino, C.; Pérez-Ros, P.; Martínez-Arnau, F.M. Influence of physical exercise on respiratory muscle function in older adults: A systematic review and meta-analysis. Geriatr. Nurs. 2024, 57, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-J.; Lim, O.-B.; Cynn, H.-S.; Yi, C.-H. Differential increase in the thickness of abdominal muscles during different squat exercises in college athletes. Isokinet. Exerc. Sci. 2017, 25, 193–200. [Google Scholar] [CrossRef]
- Qaisar, R.; Bhaskaran, S.; Van Remmen, H. Muscle fiber type diversification during exercise and regeneration. Free Radic. Biol. Med. 2016, 98, 56–67. [Google Scholar] [CrossRef]
- Kim, S.H.; Shin, M.J.; Lee, J.M.; Huh, S.; Shin, Y.B. Effects of a new respiratory muscle training device in community-dwelling elderly men: An open-label, randomized, non-inferiority trial. BMC Geriatr. 2022, 22, 155. [Google Scholar] [CrossRef]
- Kono, Y.; Izawa, H.; Aoyagi, Y.; Ishikawa, A.; Sugiura, T.; Mori, E.; Ueda, S.; Fujiwara, W.; Hayashi, M.; Saitoh, E. The difference in determinant factor of six-minute walking distance between sarcopenic and non-sarcopenic elderly patients with heart failure. J. Cardiol. 2020, 75, 42–46. [Google Scholar] [CrossRef]
- Kwok, B.C.; Pua, Y.H.; Mamun, K.; Wong, W.P. The minimal clinically important difference of six-minute walk in Asian older adults. BMC Geriatr. 2013, 13, 23. [Google Scholar] [CrossRef]
- Barajas-Galindo, D.E.; González Arnáiz, E.; Ferrero Vicente, P.; Ballesteros-Pomar, M.D. Effects of physical exercise in sarcopenia. A systematic review. Endocrinol. Diabetes Nutr. (Engl. Ed.) 2021, 68, 159–169. [Google Scholar] [CrossRef]
- Brightwell, C.R.; Markofski, M.M.; Moro, T.; Fry, C.S.; Porter, C.; Volpi, E.; Rasmussen, B.B. Moderate-intensity aerobic exercise improves skeletal muscle quality in older adults. Moderate-intensity aerobic exercise improves skeletal muscle quality in older adults. Transl. Sports Med. 2019, 2, 109–119. [Google Scholar] [CrossRef]
- Coelho-Júnior, H.J.; Calvani, R.; Picca, A.; Tosato, M.; Landi, F.; Marzetti, E. Engagement in Aerobic Exercise Is Associated with a Reduced Prevalence of Sarcopenia and Severe Sarcopenia in Italian Older Adults. J. Pers. Med. 2023, 13, 655. [Google Scholar] [CrossRef]
- Yoo, S.-Z.; No, M.-H.; Heo, J.-W.; Park, D.-H.; Kang, J.-H.; Kim, S.H.; Kwak, H.-B. Role of exercise in age-related sarcopenia. J. Exerc. Rehabil. 2018, 14, 551–558. [Google Scholar] [CrossRef] [PubMed]
| Virtual Reality Group (n = 26) | Control Group (n = 27) | x2 | p-Value | |
|---|---|---|---|---|
| Sex | 0.092 (1) | 0.761 | ||
| Male (%) | 4 (44.44) | 5 (55.56) | ||
| Female (%) | 22 (50.00) | 22 (50.00) | ||
| Diabetic mellitus (%) | 12 (66.67) | 6 (33.33) | 3.382 | 0.066 |
| Hypertension (%) | 15 (60.00) | 10 (40.00) | 2.268 | 0.132 |
| Dyslipidemia (%) | 3 (50.00) | 3 (50.00) | 0.002 | 0.961 |
| Heart disease (%) | 1 (20.00) | 4 (80.00) | 1.865 | 0.172 |
| Mean ± SD | Mean ± SD | t (test) | p-Value | |
| Age (years) | 69.23 ± 4.79 | 71.15 ± 5.94 | −1.290 | 0.203 |
| Maximal inspiratory pressure (cmH2O) | 45.27 ± 21.06 | 51.93 ± 24.09 | −1.069 | 0.290 |
| Maximal expiratory pressure (cmH2O) | 44.31 ± 15.93 | 47.48 ± 14.58 | −0.757 | 0.453 |
| 6 min walk test (meters) | 334.52 ± 46.96 | 354.48 ± 70.37 | −1.210 | 0.232 |
| Virtual Reality Group (n = 26) | Change Mean ± SE VR vs. Control | Significant Within VR gr | Control Group (n = 27) | Change Mean ± SE | Significant Within CG | p-Value VR vs. Control | Significant Between VR gr and CG | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Test | Post-Test | Pre-Test | Post-Test | |||||||
| MIP (cmH2O) | 45.27 ± 21.06 | 58.23 ± 20.21 | 12.96 ± 1.49 *** | F(1,51) = 75.593, p < 0.001, np2 = 0.597 | 51.93 ± 24.09 | 51.59 ± 23.19 | −0.33 ± 1.46 | F(1,51) = 0.052, p = 0.821, np2 = 0.001 | 0.272 | F(1,51) = 1.231, p = 0.272, np2 = 0.024 |
| MEP (cmH2O) | 44.31 ± 15.93 | 58.04 ± 19.81 | 13.73 ± 1.72 *** | F(1,51) = 63.759, p < 0.001, np2 = 0.556 | 47.48 ± 14.58 | 43.56 ± 12.01 | −3.93 ± 1.69 * | F(1,51) = 5.413, p = 0.024, np2 = 0.096 | 0.002 | F(1,51) = 10.446, p = 0.002, np2 = 0.170 |
| 6MWT (meter) | 334.52 ± 46.96 | 362.84 ± 39.46 | 28.32 ± 3.48 *** | F(1,51) = 66.104, p < 0.001, np2 = 0.564 | 354.48 ± 70.37 | 344.09 ± 39.46 | −10.39 ± 3.42 ** | F(1,51) = 9.238, p = 0.004, np2 = 0.153 | 0.229 | F(1,51) = 1.479, p = 0.229, np2 = 0.028 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chitjamnogchai, C.; Yuenyongchaiwat, K.; Sermsinsaithong, N.; Tavonudomgit, W.; Mahawong, L.; Buranapuntalug, S.; Thanawattano, C. Home-Based Virtual Reality Exercise and Resistance Training for Enhanced Cardiorespiratory Fitness in Community-Dwelling Older People with Sarcopenia: A Randomized, Double-Blind Controlled Trial. Life 2025, 15, 986. https://doi.org/10.3390/life15070986
Chitjamnogchai C, Yuenyongchaiwat K, Sermsinsaithong N, Tavonudomgit W, Mahawong L, Buranapuntalug S, Thanawattano C. Home-Based Virtual Reality Exercise and Resistance Training for Enhanced Cardiorespiratory Fitness in Community-Dwelling Older People with Sarcopenia: A Randomized, Double-Blind Controlled Trial. Life. 2025; 15(7):986. https://doi.org/10.3390/life15070986
Chicago/Turabian StyleChitjamnogchai, Chanakan, Kornanong Yuenyongchaiwat, Natsinee Sermsinsaithong, Wararat Tavonudomgit, Lucksanaporn Mahawong, Sasipa Buranapuntalug, and Chusak Thanawattano. 2025. "Home-Based Virtual Reality Exercise and Resistance Training for Enhanced Cardiorespiratory Fitness in Community-Dwelling Older People with Sarcopenia: A Randomized, Double-Blind Controlled Trial" Life 15, no. 7: 986. https://doi.org/10.3390/life15070986
APA StyleChitjamnogchai, C., Yuenyongchaiwat, K., Sermsinsaithong, N., Tavonudomgit, W., Mahawong, L., Buranapuntalug, S., & Thanawattano, C. (2025). Home-Based Virtual Reality Exercise and Resistance Training for Enhanced Cardiorespiratory Fitness in Community-Dwelling Older People with Sarcopenia: A Randomized, Double-Blind Controlled Trial. Life, 15(7), 986. https://doi.org/10.3390/life15070986






