Fifteen Years of Emergency Visits for Whiplash Injuries: Impact of COVID-19 and Campaign to Reduce Minor Injury Admission
Abstract
1. Introduction
2. Materials and Methods
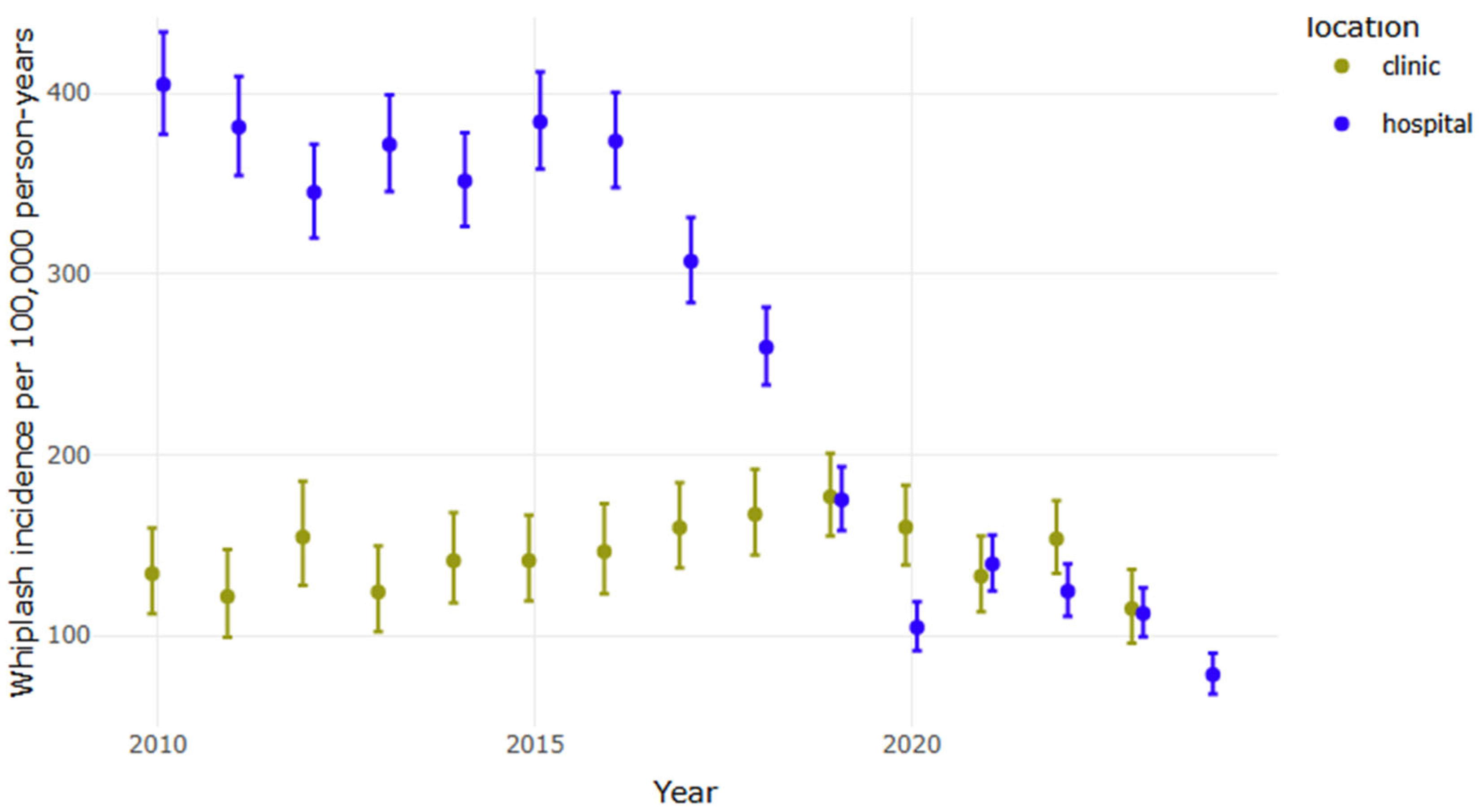
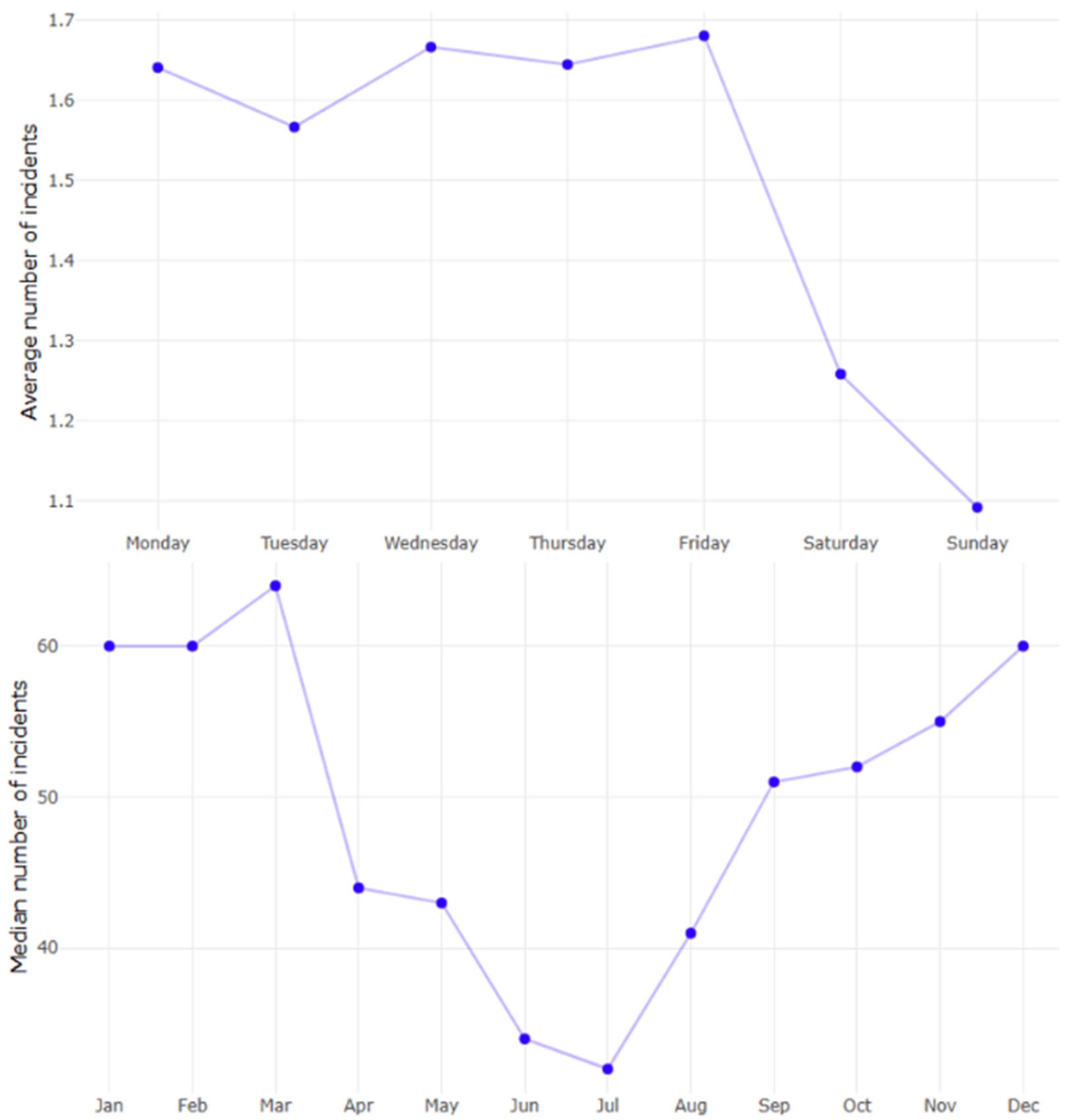
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

Appendix B
| AGE | Sex | No. of Injuries | Person-Years | Incidence 1 |
|---|---|---|---|---|
| 0 | female | 0 | 20,996.0 | 0 |
| 0 | male | 0 | 22,419.0 | 0 |
| 1 | female | 0 | 20,945.0 | 0 |
| 1 | male | 0 | 22,264.5 | 0 |
| 2 | female | 0 | 21,103.0 | 0 |
| 2 | male | 0 | 22,285.5 | 0 |
| 3 | female | 0 | 21,030.0 | 0 |
| 3 | male | 0 | 22,186.0 | 0 |
| 4 | female | 0 | 21,015.5 | 0 |
| 4 | male | 0 | 21,976.0 | 0 |
| 5 | female | 0 | 20,936.0 | 0 |
| 5 | male | 0 | 21,908.0 | 0 |
| 6 | female | 1 | 20,899.0 | 5 |
| 6 | male | 1 | 21,874.0 | 5 |
| 7 | female | 0 | 20,957.0 | 0 |
| 7 | male | 0 | 21,779.0 | 0 |
| 8 | female | 1 | 20,979.5 | 5 |
| 8 | male | 0 | 21,672.5 | 0 |
| 9 | female | 3 | 21,059.5 | 14 |
| 9 | male | 0 | 21,703.0 | 0 |
| 10 | female | 2 | 21,059.0 | 9 |
| 10 | male | 0 | 21,723.5 | 0 |
| 11 | female | 0 | 20,933.0 | 0 |
| 11 | male | 1 | 21,621.0 | 5 |
| 12 | female | 1 | 20,821.5 | 5 |
| 12 | male | 2 | 21,588.0 | 9 |
| 13 | female | 1 | 20,775.5 | 5 |
| 13 | male | 1 | 21,562.5 | 5 |
| 14 | female | 0 | 20,657.5 | 0 |
| 14 | male | 1 | 21,390.5 | 5 |
| 15 | female | 1 | 20,447.5 | 5 |
| 15 | male | 3 | 21,266.5 | 14 |
| 16 | female | 4 | 20,456.5 | 20 |
| 16 | male | 0 | 21,292.0 | 0 |
| 17 | female | 18 | 20,515.5 | 88 |
| 17 | male | 8 | 21,330.5 | 38 |
| 18 | female | 261 | 20,673.0 | 1263 |
| 18 | male | 134 | 21,472.5 | 624 |
| 19 | female | 240 | 21,101.0 | 1137 |
| 19 | male | 133 | 21,850.0 | 609 |
| 20 | female | 236 | 21,586.0 | 1093 |
| 20 | male | 147 | 22,392.5 | 656 |
| 21 | female | 222 | 22,071.5 | 1006 |
| 21 | male | 133 | 22,900.0 | 581 |
| 22 | female | 167 | 22,545.0 | 741 |
| 22 | male | 124 | 23,396.5 | 530 |
| 23 | female | 196 | 22,978.0 | 853 |
| 23 | male | 133 | 23,901.5 | 556 |
| 24 | female | 169 | 23,316.5 | 725 |
| 24 | male | 131 | 24,213.5 | 541 |
| 25 | female | 151 | 23,755.0 | 636 |
| 25 | male | 101 | 24,590.0 | 411 |
| 26 | female | 155 | 24,154.0 | 642 |
| 26 | male | 110 | 25,212.5 | 436 |
| 27 | female | 141 | 24,476.5 | 576 |
| 27 | male | 116 | 25,797.0 | 450 |
| 28 | female | 148 | 24,685.0 | 600 |
| 28 | male | 121 | 26,260.0 | 461 |
| 29 | female | 152 | 24,793.0 | 613 |
| 29 | male | 83 | 26,678.5 | 311 |
| 30 | female | 129 | 24,447.5 | 528 |
| 30 | male | 89 | 26,432.5 | 337 |
| 31 | female | 131 | 24,201.5 | 541 |
| 31 | male | 103 | 26,249.5 | 392 |
| 32 | female | 137 | 23,817.5 | 575 |
| 32 | male | 103 | 25,710.5 | 401 |
| 33 | female | 113 | 23,432.5 | 482 |
| 33 | male | 94 | 25,293.0 | 372 |
| 34 | female | 103 | 23,167.5 | 445 |
| 34 | male | 77 | 24,820.0 | 310 |
| 35 | female | 108 | 22,805.0 | 474 |
| 35 | male | 75 | 24,376.5 | 308 |
| 36 | female | 86 | 22,517.0 | 382 |
| 36 | male | 110 | 24,026.0 | 458 |
| 37 | female | 101 | 22,468.5 | 450 |
| 37 | male | 79 | 23,743.5 | 333 |
| 38 | female | 75 | 22,433.5 | 334 |
| 38 | male | 86 | 23,613.5 | 364 |
| 39 | female | 87 | 22,256.0 | 391 |
| 39 | male | 57 | 23,559.5 | 242 |
| 40 | female | 76 | 22,089.5 | 344 |
| 40 | male | 69 | 23,295.0 | 296 |
| 41 | female | 84 | 21,828.0 | 385 |
| 41 | male | 67 | 22,951.0 | 292 |
| 42 | female | 58 | 21,565.0 | 269 |
| 42 | male | 54 | 22,540.5 | 240 |
| 43 | female | 75 | 21,524.5 | 348 |
| 43 | male | 60 | 22,262.0 | 270 |
| 44 | female | 73 | 21,412.5 | 341 |
| 44 | male | 60 | 22,019.0 | 272 |
| 45 | female | 56 | 21,348.0 | 262 |
| 45 | male | 66 | 21,708.0 | 304 |
| 46 | female | 69 | 21,288.0 | 324 |
| 46 | male | 52 | 21,490.0 | 242 |
| 47 | female | 60 | 21,231.0 | 283 |
| 47 | male | 47 | 21,333.5 | 220 |
| 48 | female | 68 | 21,111.5 | 322 |
| 48 | male | 60 | 21,103.0 | 284 |
| 49 | female | 78 | 20,932.5 | 373 |
| 49 | male | 54 | 20,899.5 | 258 |
| 50 | female | 64 | 20,872.5 | 307 |
| 50 | male | 47 | 20,698.0 | 227 |
| 51 | female | 73 | 20,785.5 | 351 |
| 51 | male | 41 | 20,434.5 | 201 |
| 52 | female | 73 | 20,593.5 | 354 |
| 52 | male | 41 | 20,184.0 | 203 |
| 53 | female | 63 | 20,383.0 | 309 |
| 53 | male | 39 | 19,930.5 | 196 |
| 54 | female | 59 | 20,319.0 | 290 |
| 54 | male | 35 | 19,722.5 | 177 |
| 55 | female | 59 | 20,235.5 | 292 |
| 55 | male | 43 | 19,500.0 | 221 |
| 56 | female | 45 | 20,070.0 | 224 |
| 56 | male | 47 | 19,236.0 | 244 |
| 57 | female | 51 | 19,830.0 | 257 |
| 57 | male | 42 | 19,028.0 | 221 |
| 58 | female | 68 | 19,440.5 | 350 |
| 58 | male | 34 | 18,676.5 | 182 |
| 59 | female | 52 | 19,053.5 | 273 |
| 59 | male | 52 | 18,291.0 | 284 |
| 60 | female | 53 | 18,631.0 | 284 |
| 60 | male | 39 | 17,973.5 | 217 |
| 61 | female | 44 | 18,128.0 | 243 |
| 61 | male | 26 | 17,556.5 | 148 |
| 62 | female | 45 | 17,598.5 | 256 |
| 62 | male | 28 | 17,052.0 | 164 |
| 63 | female | 0 | 17,059.0 | 0 |
| 63 | male | 0 | 16,621.5 | 0 |
| 64 | female | 0 | 16,566.0 | 0 |
| 64 | male | 0 | 16,051.0 | 0 |
| 65 | female | 0 | 16,019.5 | 0 |
| 65 | male | 1 | 15,442.5 | 6 |
| 66 | female | 0 | 15,407.5 | 0 |
| 66 | male | 1 | 14,743.0 | 7 |
| 67 | female | 0 | 14,851.5 | 0 |
| 67 | male | 1 | 14,102.5 | 7 |
| 68 | female | 0 | 14,137.0 | 0 |
| 68 | male | 1 | 13,371.5 | 7 |
| 69 | female | 0 | 13,453.5 | 0 |
| 69 | male | 2 | 12,649.5 | 16 |
| 70 | female | 0 | 12,771.5 | 0 |
| 70 | male | 0 | 11,956.5 | 0 |
| 71 | female | 1 | 12,120.5 | 8 |
| 71 | male | 0 | 11,264.5 | 0 |
| 72 | female | 0 | 11,437.0 | 0 |
| 72 | male | 0 | 10,583.0 | 0 |
| 73 | female | 0 | 10,810.5 | 0 |
| 73 | male | 0 | 9958.5 | 0 |
| 74 | female | 0 | 10,254.5 | 0 |
| 74 | male | 0 | 9308.5 | 0 |
| 75 | female | 0 | 9743.5 | 0 |
| 75 | male | 0 | 8627.5 | 0 |
| 76 | female | 1 | 9217.5 | 11 |
| 76 | male | 0 | 8005.0 | 0 |
| 77 | female | 0 | 8691.0 | 0 |
| 77 | male | 0 | 7418.5 | 0 |
| 78 | female | 0 | 8235.0 | 0 |
| 78 | male | 0 | 6882.0 | 0 |
| 79 | female | 2 | 7843.0 | 26 |
| 79 | male | 0 | 6406.0 | 0 |
| 80 | female | 0 | 7406.0 | 0 |
| 80 | male | 0 | 5922.5 | 0 |
| 81 | female | 0 | 6997.0 | 0 |
| 81 | male | 0 | 5507.5 | 0 |
| 82 | female | 0 | 6583.0 | 0 |
| 82 | male | 0 | 5062.0 | 0 |
| 83 | female | 0 | 6221.0 | 0 |
| 83 | male | 0 | 4610.5 | 0 |
| 84 | female | 0 | 5838.5 | 0 |
| 84 | male | 1 | 4185.0 | 24 |
| 85 | female | 0 | 5375.0 | 0 |
| 85 | male | 0 | 3746.0 | 0 |
| 86 | female | 0 | 4975.0 | 0 |
| 86 | male | 0 | 3296.0 | 0 |
| 87 | female | 0 | 4620.5 | 0 |
| 87 | male | 0 | 2872.5 | 0 |
| 88 | female | 0 | 4146.0 | 0 |
| 88 | male | 0 | 2447.0 | 0 |
| 89 | female | 0 | 3639.0 | 0 |
| 89 | male | 0 | 2065.5 | 0 |
| 90 | female | 0 | 3121.0 | 0 |
| 90 | male | 0 | 1660.5 | 0 |
| 91 | female | 0 | 2671.0 | 0 |
| 91 | male | 0 | 1307.0 | 0 |
| 92 | female | 0 | 2219.5 | 0 |
| 92 | male | 0 | 1012.5 | 0 |
| 93 | female | 0 | 1806.0 | 0 |
| 93 | male | 0 | 766.0 | 0 |
| 94 | female | 0 | 1387.0 | 0 |
| 94 | male | 0 | 528.5 | 0 |
| 95 | female | 0 | 996.0 | 0 |
| 95 | male | 0 | 376.5 | 0 |
| 96 | female | 0 | 695.0 | 0 |
| 96 | male | 0 | 245.0 | 0 |
| 97 | female | 0 | 470.5 | 0 |
| 97 | male | 0 | 152.5 | 0 |
| 98 | female | 0 | 318.0 | 0 |
| 98 | male | 0 | 97.0 | 0 |
| 99 | female | 0 | 214.0 | 0 |
| 99 | male | 0 | 54.0 | 0 |
| 100 | female | 0 | 141.0 | 0 |
| 100 | male | 0 | 34.0 | 0 |
| 101 | female | 0 | 82.0 | 0 |
| 101 | male | 0 | 19.0 | 0 |
| 102 | female | 0 | 51.5 | 0 |
| 102 | male | 0 | 11.5 | 0 |
| 103 | female | 0 | 34.5 | 0 |
| 103 | male | 0 | 7.0 | 0 |
| 104 | female | 0 | 21.0 | 0 |
| 104 | male | 0 | 4.5 | 0 |
| 105 | female | 0 | 10.0 | 0 |
| 105 | male | 0 | 0.0 | NaN |
| 106 | female | 0 | 9.0 | 0 |
| 106 | male | 0 | 0.0 | NaN |
| 107 | female | 0 | 5.5 | 0 |
| 107 | male | 0 | 0.0 | NaN |
| 108 | female | 0 | 2.0 | 0 |
| 108 | male | 0 | 0.0 | NaN |
| 109 | female | 0 | 1.0 | 0 |
| 109 | male | 0 | 0.0 | NaN |
References
- Safiri, S.; Kolahi, A.-A.; Hoy, D.; Buchbinder, R.; Mansournia, M.A.; Bettampadi, D.; Ashrafi-Asgarabad, A.; Almasi-Hashiani, A.; Smith, E.; Sepidarkish, M.; et al. Global, regional, and national burden of neck pain in the general population, 1990-2017: Systematic analysis of the Global Burden of Disease Study 2017. BMJ 2020, 368, m791. [Google Scholar] [CrossRef]
- Spitzer, W.O.; Skovron, M.L.; Salmi, L.R.; Cassidy, J.D.; Duranceau, J.; Suissa, S.; Zeiss, E. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: Redefining "whiplash" and its management. Spine 1995, 20 (Suppl. 8), 1s–73s. [Google Scholar] [PubMed]
- Panjabi, M.M.; Cholewicki, J.; Nibu, K.; Grauer, J.N.; Babat, L.B.; Dvorak, J. Mechanism of whiplash injury. Clin. Biomech. 1998, 13, 239–249. [Google Scholar] [CrossRef] [PubMed]
- Pina, D.; Puente-López, E.; Ruiz-Hernández, J.A.; Ruiz-Cabello, A.L.; Aguerrevere, L.; Magalhães, T. Whiplash-Associated Disorders. Biopsychosocial Profiles of Pain Perception in Forensic Cases of Victims of Motor Vehicle Accidents. Front. Psychol. 2021, 12, 716513. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, R.; Russell, A.S.; Carroll, L.J.; Cassidy, J.D. A re-examination of the whiplash associated disorders (WAD) as a systemic illness. Ann. Rheum. Dis. 2005, 64, 1337–1342. [Google Scholar] [CrossRef]
- Mayou, R.; Bryant, B. Outcome of ‘whiplash’ neck injury. Injury 1996, 27, 617–623. [Google Scholar] [CrossRef]
- Lee, J.; Giles, K.; Drummond, P.D. Psychological disturbances and an exaggerated response to pain in patients with whiplash injury. J. Psychosom. Res. 1993, 37, 105–110. [Google Scholar] [CrossRef]
- Cassidy, J.D.; Carroll, L.J.; Côté, P.; Lemstra, M.; Berglund, A.; Nygren, A. Effect of eliminating compensation for pain and suffering on the outcome of insurance claims for whiplash injury. N. Engl. J. Med. 2000, 342, 1179–1186. [Google Scholar] [CrossRef]
- Berglund, A.; Alfredsson, L.; Jensen, I.; Bodin, L.; Nygren, Å. Occupant- and Crash-Related Factors Associated with the Risk of Whiplash Injury. Ann. Epidemiol. 2003, 13, 66–72. [Google Scholar] [CrossRef]
- Holm, L.W.; Carroll, L.J.; Cassidy, J.D.; Hogg-Johnson, S.; Côté, P.; Guzman, J.; Peloso, P.; Nordin, M.; Hurwitz, E.; van der Velde, G.; et al. The burden and determinants of neck pain in whiplash-associated disorders after traffic collisions: Results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008, 33, S52–S59. [Google Scholar] [CrossRef]
- EEVC WG20. Updated State-of-the-Art Review on Whiplash Injury Prevention; WD80; European Enhanced Vehicle-Safety Committee: Brussels, Belgium, 2005. [Google Scholar]
- Leth-Petersen, S.; Rotger, G.P. Long-term labour-market performance of whiplash claimants. J. Health Econ. 2009, 28, 996–1011. [Google Scholar] [CrossRef]
- Jennum, P.; Kjellberg, J.; Ibsen, R.; Bendix, T. Health, social, and economic consequences of neck injuries: A controlled national study evaluating societal effects on patients and their partners. Spine 2013, 38, 449–457. [Google Scholar] [CrossRef]
- Styrke, J.; Stålnacke, B.M.; Bylund, P.O.; Sojka, P.; Björnstig, U. A 10-year incidence of acute whiplash injuries after road traffic crashes in a defined population in northern Sweden. PM R J. Inj. Funct. Rehabil. 2012, 4, 739–747. [Google Scholar] [CrossRef] [PubMed]
- Quinlan, K.P.; Annest, J.L.; Myers, B.; Ryan, G.; Hill, H. Neck strains and sprains among motor vehicle occupants—United States, 2000. Accid. Anal. Prev. 2004, 36, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Pines, J.M.; Griffey, R.T. What we have learned from a decade of ED crowding research. Acad. Emerg. Med. 2015, 22, 985–987. [Google Scholar] [CrossRef] [PubMed]
- Pearce, S.; Marchand, T.; Shannon, T.; Ganshorn, H.; Lang, E. Emergency department crowding: An overview of reviews describing measures causes, and harms. Intern. Emerg. Med. 2023, 18, 1137–1158. [Google Scholar] [CrossRef]
- Pearce, S.; Marr, E.; Shannon, T.; Marchand, T.; Lang, E. Overcrowding in emergency departments: An overview of reviews describing global solutions and their outcomes. Intern. Emerg. Med. 2024, 19, 483–491. [Google Scholar] [CrossRef]
- Morley, C.; Unwin, M.; Peterson, G.M.; Stankovich, J.; Kinsman, L. Emergency department crowding: A systematic review of causes, consequences and solutions. PLoS ONE 2018, 13, e0203316. [Google Scholar] [CrossRef]
- Hong, M.; Thind, A.; Zaric, G.S.; Sarma, S. The impact of improved access to after-hours primary care on emergency department and primary care utilization: A systematic review. Health Policy 2020, 124, 812–818. [Google Scholar] [CrossRef]
- Rasouli, H.R.; Aliakbar Esfahani, A.; Abbasi Farajzadeh, M. Challenges, consequences, and lessons for way-outs to emergencies at hospitals: A systematic review study. BMC Emerg. Med. 2019, 19, 62. [Google Scholar] [CrossRef]
- Tefft, B.C. Traffic Safety Impact of the COVID-19 Pandemic: Fatal Crashes in 2020–2022 (Research Brief); AAA Foundation for Traffic Safety: Washington, DC, USA, 2024. [Google Scholar]
- Ebrahim Shaik, M.; Ahmed, S. An overview of the impact of COVID-19 on road traffic safety and travel behavior. Transp. Eng. 2022, 9, 100119. [Google Scholar] [CrossRef]
- Hagstofan. Mesta Fjölgun Íbúa Frá Upphafi. Available online: https://hagstofa.is/utgafur/frettasafn/mannfjoldi/mannfjoldinn-1-januar-2023/ (accessed on 28 February 2024).
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10). Available online: https://icd.who.int/browse10/2019/en (accessed on 19 March 2025).
- Hagstofa.is. Meðalmannfjöldi Eftir Sveitarfélagi, Kyni og Aldri 1998-2022—Sveitarfélagaskipan 1. Janúar 2023. Available online: https://px.hagstofa.is/pxis/pxweb/is/Ibuar/Ibuar__mannfjoldi__2_byggdir__sveitarfelog/MAN02008.px (accessed on 5 April 2025).
- Samgöngustofa. Slysaskýrsla 2022. Available online: https://downloads.ctfassets.net/8k0h54kbe6bj/1BvtyLH6PLM3dZfrYJ0D6L/a13dea7983b4de7a2cda7bc538977013/Slysaskyrsla2022.pdf (accessed on 18 February 2025).
- ITF. ITF Transport Outlook 2019; ITF: Paris, France, 2019. [Google Scholar]
- Vegagerðin. 3 Lykilteljarar á Höfuðborgarsvæðinu 2025. Available online: https://www.vegagerdin.is/vegagerdin/gagnasafn/umferdartolur/tolfraedi-umferdar/3-lykilteljarar-a-hofudborgarsvaedinu-2025 (accessed on 6 April 2025).
- D’Elia, A.; Newstead, S. Retrospective evaluation of vehicle whiplash-reducing head restraint systems to prevent whiplash injury in Victoria, Australia. Accid. Anal. Prev. 2021, 150, 105941. [Google Scholar] [CrossRef] [PubMed]
- Cullen, P.; Möller, H.; Woodward, M.; Senserrick, T.; Boufous, S.; Rogers, K.; Brown, J.; Ivers, R. Are there sex differences in crash and crash-related injury between men and women? A 13-year cohort study of young drivers in Australia. SSM Popul. Health 2021, 14, 100816. [Google Scholar] [CrossRef]
- Cronn, S.; Somasundaram, K.; Driesslein, K.; Tomas, C.W.; Pintar, F. Sex-related disparities in vehicle crash injury and hemodynamics. Front. Public Health 2024, 12, 1331313. [Google Scholar] [CrossRef] [PubMed]
- Vasavada, A.N.; Danaraj, J.; Siegmund, G.P. Head and neck anthropometry, vertebral geometry and neck strength in height-matched men and women. J. Biomech. 2008, 41, 114–121. [Google Scholar] [CrossRef]
- Atwood, J.; Noh, E.Y.; Craig, M.J. Female crash fatality risk relative to males for similar physical impacts. Traffic Inj. Prev. 2023, 24, S1–S8. [Google Scholar] [CrossRef]
- Booth, G.R.; Cripton, P.A.; Siegmund, G.P. The Lack of Sex, Age, and Anthropometric Diversity in Neck Biomechanical Data. Front. Bioeng. Biotechnol. 2021, 9, 684217. [Google Scholar] [CrossRef]
- Jónsson, R.; Mogensen, B.; Richter, I.; Sigvaldason, H. Hálshnykkur—Faraldsfræðileg athugun í Reykjavík 1974–1991. Læknablaðið 1992, 78 (Suppl. 22), 38. [Google Scholar]
- Island.is. Bílpróf og Fyrsta Ökuskírteinið, B-Próf. Available online: https://island.is/bilprof-og-fyrsta-oekuskirteinid-b-prof (accessed on 20 April 2025).
- Samgongustofa.is. Börn í bíl, Upplýsingar og Tilmæli. Available online: https://assets.ctfassets.net/8k0h54kbe6bj/4k9g0xJwbflC1EDgb6s34I/87f5ad6638ce53c309d6bdb6885538cb/O_RYGGI_BARNA_I__BI_L._2024.pdf (accessed on 15 April 2025).
- Anderson, D.M.; Peterson, R.W. Rear-facing child safety seat effectiveness: Evidence from motor vehicle crash data. Inj. Prev. 2023, 29, 320–326. [Google Scholar] [CrossRef]
- Durbin, D.R.; Hoffman, B.D. Child Passenger Safety. Pediatrics 2018, 142, e20182460. [Google Scholar] [CrossRef]
- Hagstofan. Mannfjöldi Eftir Þéttbýlisstöðum, Kyni og Aldri 1. Janúar 1998–2024. Available online: https://px.hagstofa.is/pxis/pxweb/is/Ibuar/Ibuar__mannfjoldi__2_byggdir__Byggdakjarnar/MAN030102.px (accessed on 25 April 2025).
- Lemeunier, N.; da Silva-Oolup, S.; Chow, N.; Southerst, D.; Carroll, L.; Wong, J.J.; Shearer, H.; Mastragostino, P.; Cox, J.; Côté, E.; et al. Reliability and validity of clinical tests to assess the anatomical integrity of the cervical spine in adults with neck pain and its associated disorders: Part 1—A systematic review from the Cervical Assessment and Diagnosis Research Evaluation (CADRE) Collaboration. Eur. Spine J. 2017, 26, 2225–2241. [Google Scholar] [CrossRef] [PubMed]



| Years | Total MVCs | Total MVCs with Injuries (% of Total MVCs) | All ED Visits with ICPC 2 “Traffic Accident” | Whiplash (% of Total MVCs) |
|---|---|---|---|---|
| 2010 | 4193 | 428 (10) | 1786 | 806 (19) |
| 2011 | 4065 | 393 (10) | 1746 | 755 (19) |
| 2012 | 3811 | 359 (9) | 1627 | 690 (18) |
| 2013 | 4051 | 389 (10) | 1755 | 753 (19) |
| 2014 | 4160 | 419 (10) | 1692 | 722 (17) |
| 2015 | 4246 | 449 (11) | 1920 | 798 (19) |
| 2016 | 4503 | 450 (10) | 1955 | 787 (17) |
| 2017 | 4534 | 475 (10) | 1745 | 661 (15) |
| 2018 | 4900 | 413 (8) | 1688 | 572 (12) |
| 2019 | 4756 | 376 (8) | 1243 | 393 (8) |
| 2020 | 4063 | 368 (9) | 812 | 238 (6) |
| 2021 | 4841 | 442 (9) | 965 | 323 (7) |
| 2022 | 5267 | 475 (9) | 786 | 294 (6) |
| 2023 | 5425 | 489 (9) | 1042 | 271 (5) |
| 2024 | NA 3 | NA | 846 | 193 (NA) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ragnarsdóttir, H.; Arnardóttir, K.R.; Briem, K.; Nicholls, M.; Björnsson, H.M. Fifteen Years of Emergency Visits for Whiplash Injuries: Impact of COVID-19 and Campaign to Reduce Minor Injury Admission. Life 2025, 15, 987. https://doi.org/10.3390/life15070987
Ragnarsdóttir H, Arnardóttir KR, Briem K, Nicholls M, Björnsson HM. Fifteen Years of Emergency Visits for Whiplash Injuries: Impact of COVID-19 and Campaign to Reduce Minor Injury Admission. Life. 2025; 15(7):987. https://doi.org/10.3390/life15070987
Chicago/Turabian StyleRagnarsdóttir, Harpa, Kristín Rut Arnardóttir, Kristín Briem, Micah Nicholls, and Hjalti Már Björnsson. 2025. "Fifteen Years of Emergency Visits for Whiplash Injuries: Impact of COVID-19 and Campaign to Reduce Minor Injury Admission" Life 15, no. 7: 987. https://doi.org/10.3390/life15070987
APA StyleRagnarsdóttir, H., Arnardóttir, K. R., Briem, K., Nicholls, M., & Björnsson, H. M. (2025). Fifteen Years of Emergency Visits for Whiplash Injuries: Impact of COVID-19 and Campaign to Reduce Minor Injury Admission. Life, 15(7), 987. https://doi.org/10.3390/life15070987





