Psychosocial Risk and Health Behaviors as Predictors of Clinical Events in Patients Wait-Listed for a New Heart: Results from 7 Years of Follow-Up
Abstract
:1. Introduction
2. Materials and Methods
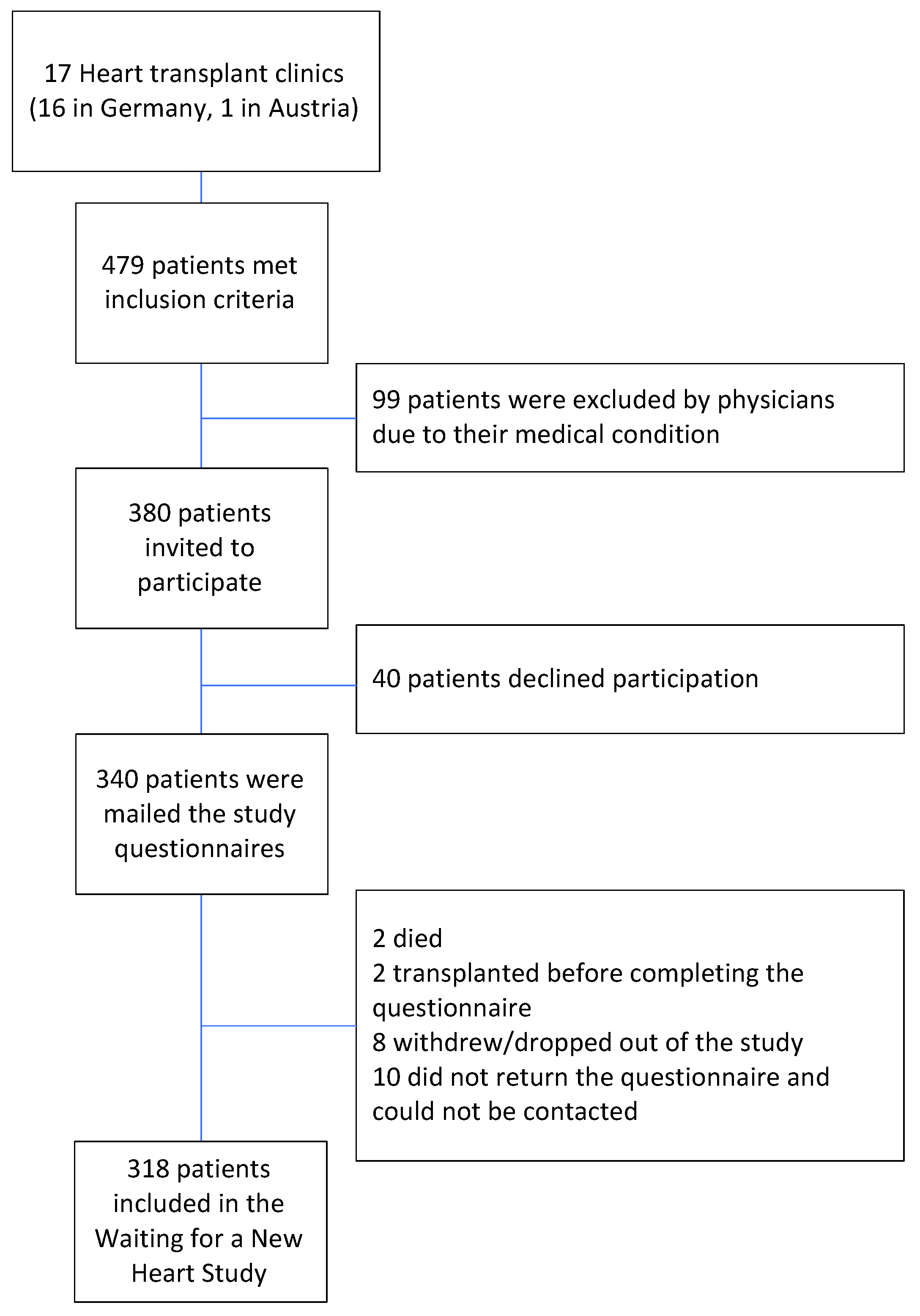
2.1. Study Population
2.2. Procedures and Participants
2.3. Variables
2.3.1. Waiting List Outcome Variables
2.3.2. Independent Variables
Dietary Habits
Physical Activity
Smoking Status
Medical Variables
Demographic Characteristics
2.4. Statistical Analyses
3. Results
3.1. Patient Characteristics
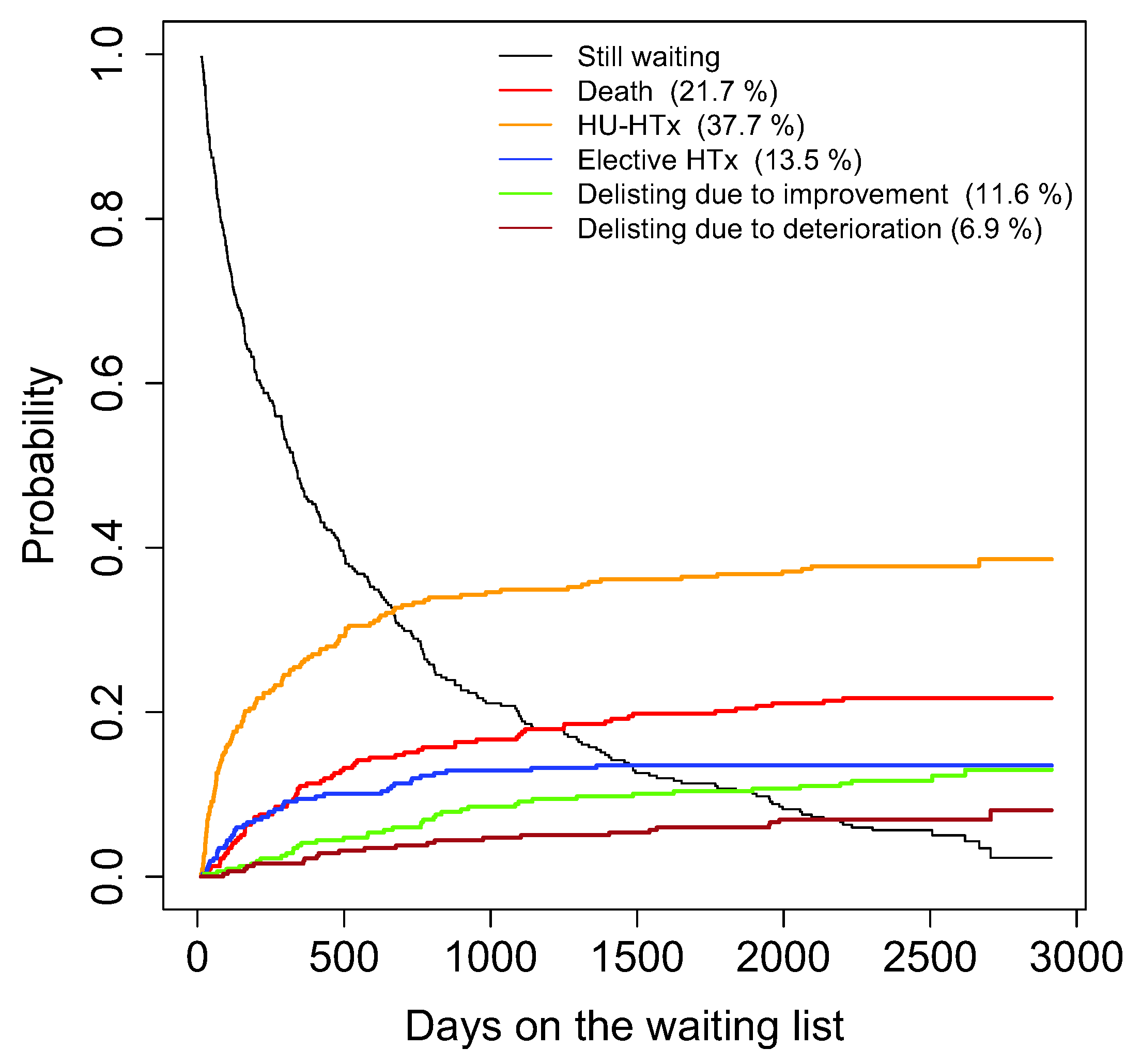
3.2. Waiting List Outcomes
3.3. Univariate Competing Risks Models
3.4. Multivariate Competing Risks Models
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Eurotransplant Statistics Report Library. Active Heart Waiting List (at Year End) in Eurotransplants, by Year, by Country; Eurotransplant: Leiden, The Netherlands, 2021. [Google Scholar]
- Eurotransplant Statistics Report Library. Heart Transplants (Deceased Donor), by Year, by Country; Eurotransplant: Leiden, The Netherlands, 2021. [Google Scholar]
- Maltês, S.; Rocha, B.M.L.; Cunha, G.J.L.; Brízido, C.; Strong, C.; Tralhão, A.; Weigert, A.; Duarte, J.S.; Aguiar, C.; Mendes, M.; et al. Challenges of Organ Shortage for Heart Transplant: Surviving Amidst the Chaos of Long Waiting Times. Transplant. Direct 2021, 7, e671. [Google Scholar] [CrossRef]
- Zipfel, S.; Löwe, B.; Paschke, T.; Immel, B.; Lange, R.; Zimmermann, R.; Herzog, W.; Bergmann, G. Psychological distress in patients awaiting heart transplantation. J. Psychosom. Res. 1998, 45, 465–470. [Google Scholar] [CrossRef]
- Rutledge, T.; Reis, V.A.; Linke, S.E.; Greenberg, B.H.; Mills, P.J. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J. Am. Coll. Cardiol. 2006, 48, 1527–1537. [Google Scholar] [CrossRef] [Green Version]
- Kaiser, P.; Allen, N.; Delaney, J.A.C.; Hirsch, C.H.; Carnethon, M.; Arnold, A.M.; Odden, M.C. The association of prediagnosis social support with survival after heart failure in the Cardiovascular Health Study. Ann. Epidemiol. 2020, 42, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Heidari Gorji, M.A.; Fatahian, A.; Farsavian, A. The impact of perceived and objective social isolation on hospital readmission in patients with heart failure: A systematic review and meta-analysis of observational studies. Gen. Hosp. Psychiatry 2019, 60, 27–36. [Google Scholar] [CrossRef]
- Gopal, D.M.; Kalogeropoulos, A.P.; Georgiopoulou, V.V.; Smith, A.L.; Bauer, D.C.; Newman, A.B.; Kim, L.; Bibbins-Domingo, K.; Tindle, H.; Harris, T.B.; et al. Cigarette smoking exposure and heart failure risk in older adults: The Health, Aging, and Body Composition Study. Am. Heart J. 2012, 164, 236–242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Son, Y.-J.; Lee, H.-J. Association between persistent smoking after a diagnosis of heart failure and adverse health outcomes: A systematic review and meta-analysis. Tob. Induc. Dis. 2020, 18, 5. [Google Scholar] [CrossRef]
- Ahmed, A.A.; Patel, K.; Nyaku, M.A.; Kheirbek, R.E.; Bittner, V.; Fonarow, G.C.; Filippatos, G.S.; Morgan, C.J.; Aban, I.B.; Mujib, M.; et al. Risk of Heart Failure and Death After Prolonged Smoking Cessation. Circ. Heart Fail. 2015, 8, 694–701. [Google Scholar] [CrossRef] [Green Version]
- Duncan, M.S.; Freiberg, M.S.; Greevy, R.A., Jr.; Kundu, S.; Vasan, R.S.; Tindle, H.A. Association of Smoking Cessation With Subsequent Risk of Cardiovascular Disease. JAMA 2019, 322, 642–650. [Google Scholar] [CrossRef] [Green Version]
- Cacciatore, F.; Amarelli, C.; Ferrara, N.; Della Valle, E.; Curcio, F.; Liguori, I.; Bosco, Q.; Maiello, C.; Napoli, C.; Bonaduce, D.; et al. Protective effect of physical activity on mortality in older adults with advanced chronic heart failure: A prospective observational study. Eur. J. Prev. Cardiol. 2020, 26, 481–488. [Google Scholar] [CrossRef] [PubMed]
- Colin-Ramirez, E.; Castillo-Martinez, L.; Orea-Tejeda, A.; Zheng, Y.; Westerhout, C.M.; Ezekowitz, J.A. Dietary fatty acids intake and mortality in patients with heart failure. Nutrition 2014, 30, 1366–1371. [Google Scholar] [CrossRef] [PubMed]
- Zahn, D.; Weidner, G.; Beyersmann, J.; Smits, J.M.; Deng, M.C.; Kaczmarek, I.; Meyer, S.; Reichenspurner, H.; Mehlhorn, U.; Wagner, F.M.; et al. Composite risk scores and depression as predictors of competing waiting-list outcomes: The Waiting for a New Heart Study. Transpl. Int. 2010, 23, 1223–1232. [Google Scholar] [CrossRef]
- Weidner, G.; Zahn, D.; Mendell, N.R.; Smits, J.M.; Deng, M.C.; Zittermann, A.; Spaderna, H.; Waiting for a New Heart Study Group. Patients’ sex and emotional support as predictors of death and clinical deterioration in the waiting for a new heart study: Results from the 1-year follow-up. Prog Transpl. 2011, 21, 106–114. [Google Scholar] [CrossRef]
- Gali, K.; Spaderna, H.; Smits, J.M.; Bramstedt, K.A.; Weidner, G. Smoking Status at Time of Listing for a Heart Transplant Predicts Mortality on the Waiting List: A Multicenter Prospective Observational Study. Prog. Transpl. 2016, 26, 117–121. [Google Scholar] [CrossRef]
- Spaderna, H.; Mendell, N.R.; Zahn, D.; Wang, Y.; Kahn, J.; Smits, J.M.; Weidner, G. Social isolation and depression predict 12-month outcomes in the “waiting for a new heart study”. J. Heart Lung Transpl. 2010, 29, 247–254. [Google Scholar] [CrossRef]
- Spaderna, H.; Weidner, G.; Koch, K.C.; Kaczmarek, I.; Wagner, F.M.; Smits, J.M.; Waiting for a New Heart Study Group. Medical and psychosocial predictors of mechanical circulatory support device implantation and competing outcomes in the Waiting for a New Heart Study. J. Heart Lung Transpl. 2012, 31, 16–26. [Google Scholar] [CrossRef]
- Spaderna, H.; Vogele, C.; Barten, M.J.; Smits, J.M.A.; Bunyamin, V.; Weidner, G. Physical activity and depression predict event-free survival in heart transplant candidates. Health Psychol. 2014, 33, 1328–1336. [Google Scholar] [CrossRef] [PubMed]
- Spaderna, H.; Weidner, G.; Zahn, D.; Smits, J.M.A. Psychological characteristics and social integration of patients with ischemic and non-ischemic heart failure newly listed for heart transplantation: The Waiting for a New Heart Study. Appl. Psychol. Health Well-Being 2009, 1, 188–210. [Google Scholar] [CrossRef]
- Haneya, A.; Haake, N.; Diez, C.; Puehler, T.; Cremer, J.; Schmid, C.; Hirt, S.W. Impact of the eurotransplant high-urgency heart allocation system on the outcome of transplant candidates in Germany. Thorac. Cardiovasc. Surg. 2011, 59, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Herrmann-Lingen, C.; Buss, U.; Snaith, R.P. HADS-D Hospital Anxiety and Depression Scale—Deutsche Version. Ein Fragebogen zur Erfassung von Angst und Depressivität in der Somatischen Medizin, 2nd ed.; Huber: Bern, Switzerland, 2005. [Google Scholar]
- Herrmann, C. International experiences with the Hospital Axiety and Depression Scale—A review of validation data and clinical results. J. Psychosom. Res. 1997, 42, 17–41. [Google Scholar] [CrossRef]
- Frasure-Smith, N.; Lespérance, F.; Gravel, G.; Masson, A.; Juneau, M.; Talajic, M.; Bourassa, M.G. Social support, depression, and mortality during the first year after myocardial infarction. Circulation 2000, 101, 1919–1924. [Google Scholar] [CrossRef] [Green Version]
- Dlugosch, G.E.; Krieger, W. Fragebogen zur Erfassung des Gesundheitsverhaltens (FEG) [Questionnaire for the Assessment of health Behavior]; Swets Test Services: Frankfurt, Germany, 1995. [Google Scholar]
- Covas, M.I.; Konstantinidou, V.; Fito, M. Olive oil and cardiovascular health. J. Cardiovasc. Pharm. 2009, 54, 477–482. [Google Scholar] [CrossRef] [PubMed]
- Spaderna, H.; Zahn, D.; Pretsch, J.; Connor, S.L.; Zittermann, A.; Schulze Schleithoff, S.; Bramstedt, K.A.; Smits, J.M.; Weidner, G. Dietary habits are related to outcomes in patients with advanced heart failure awaiting heart transplantation. J. Card Fail. 2013, 19, 240–250. [Google Scholar] [CrossRef]
- Stewart, A.L.; Mills, K.M.; King, A.C.; Haskell, W.L.; Gillies, D.; Ritter, P.L. CHAMPS Physical Activity Questionnaire for Older Adults: Outcomes for interventions. Med. Sci. Sports Exerc. 2001, 33, 1126–1141. [Google Scholar] [CrossRef] [PubMed]
- Spaderna, H.; Zahn, D.; Schulze Schleithoff, S.; Stadlbauer, T.; Rupprecht, L.; Smits, J.M.A.; Krohne, H.W.; Münzel, T.; Weidner, G. Depression and disease severity as correlates of everyday physical activity in heart transplant candidates. Transpl. Int. 2010, 23, 813–822. [Google Scholar] [CrossRef] [PubMed]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of physical activities: An update of activity codes and MET intensities. Med. Sci. Sports Exerc. 2000, 32, 498–516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aaronson, K.D.; Schwartz, J.S.; Chen, T.-M.; Wong, K.-L.; Goin, J.E.; Mancini, D.M. Development and Prospective Validation of a Clinical Index to Predict Survival in Ambulatory Patients Referred for Cardiac Transplant Evaluation. Circulation 1997, 95, 2660–2667. [Google Scholar] [CrossRef]
- Sterne, J.A.; White, I.R.; Carlin, J.B.; Spratt, M.; Royston, P.; Kenward, M.G.; Wood, A.M.; Carpenter, J.R. Multiple imputation for missing data in epidemiological and clinical research: Potential and pitfalls. BMJ 2009, 338, b2393. [Google Scholar] [CrossRef]
- Kim, H.T. Cumulative incidence in competing risks data and competing risks regression analysis. Clin. Cancer Res. 2007, 13, 559–565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fine, J.P.; Gray, R.J. A Proportional Hazards Model for the Subdistribution of a Competing Risk. J. Am. Stat. Assoc. 1999, 94, 496–509. [Google Scholar] [CrossRef]
- Scrucca, L.; Santucci, A.; Aversa, F. Regression modeling of competing risk using R: An in depth guide for clinicians. Bone Marrow Transpl. 2010, 45, 1388–1395. [Google Scholar] [CrossRef] [Green Version]
- Weidner, G.; Spaderna, H. The role of the Heart Failure Survival Score and psychosocial stress in predicting event-free survival in patients referred for heart transplantation. J. Heart Lung Transpl. 2012, 31, 436–438. [Google Scholar] [CrossRef]
- Freedland, K.E.; Hesseler, M.J.; Carney, R.M.; Steinmeyer, B.C.; Skala, J.A.; Dávila-Román, V.G.; Rich, M.W. Major Depression and Long-Term Survival of Patients With Heart Failure. Psychosom Med. 2016, 78, 896–903. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Celano, C.M.; Villegas, A.C.; Albanese, A.M.; Gaggin, H.K.; Huffman, J.C. Depression and Anxiety in Heart Failure: A Review. Harv. Rev. Psychiatry 2018, 26, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Freedland, K.E.; Carney, R.M.; Rich, M.W.; Steinmeyer, B.C.; Rubin, E.H. Cognitive Behavior Therapy for Depression and Self-Care in Heart Failure Patients: A Randomized Clinical Trial. JAMA Intern. Med. 2015, 175, 1773–1782. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, M.S.; Jones, D.W.; Butler, J. Salt, No Salt, or Less Salt for Patients With Heart Failure? Am. J. Med. 2020, 133, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Mahtani, K.R.; Heneghan, C.; Onakpoya, I.; Tierney, S.; Aronson, J.K.; Roberts, N.; Hobbs, F.D.R.; Nunan, D. Reduced Salt Intake for Heart Failure: A Systematic Review. JAMA Intern. Med. 2018, 178, 1693–1700. [Google Scholar] [CrossRef]
- Frediani, J.K.; Reilly, C.M.; Higgins, M.; Clark, P.C.; Gary, R.A.; Dunbar, S.B. Quality and Adequacy of Dietary Intake in a Southern Urban Heart Failure Population. J. Cardiovasc. Nurs. 2013, 28, 119–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mozaffarian, D.; Micha, R.; Wallace, S. Effects on Coronary Heart Disease of Increasing Polyunsaturated Fat in Place of Saturated Fat: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. PLOS Med. 2010, 7, e1000252. [Google Scholar] [CrossRef] [PubMed]
- Guasch-Ferré, M.; Babio, N.; Martínez-González, M.A.; Corella, D.; Ros, E.; Martín-Peláez, S.; Estruch, R.; Arós, F.; Gómez-Gracia, E.; Fiol, M.; et al. Dietary fat intake and risk of cardiovascular disease and all-cause mortality in a population at high risk of cardiovascular disease. Am. J. Clin. Nutr. 2015, 102, 1563–1573. [Google Scholar] [CrossRef] [Green Version]
- Hooper, L.; Martin, N.; Jimoh, O.F.; Kirk, C.; Foster, E.; Abdelhamid, A.S. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database Syst. Rev. 2020, CD011737. [Google Scholar] [CrossRef] [PubMed]
- Pellicori, P.; Kaur, K.; Clark, A.L. Fluid Management in Patients with Chronic Heart Failure. Card Fail. Rev. 2015, 1, 90–95. [Google Scholar] [CrossRef] [Green Version]
- Abu-Sawwa, R.; Dunbar, S.B.; Quyyumi, A.A.; Sattler, E.L.P. Nutrition intervention in heart failure: Should consumption of the DASH eating pattern be recommended to improve outcomes? Heart Fail. Rev. 2019, 24, 565–573. [Google Scholar] [CrossRef]
- Levitan, E.B.; Lewis, C.E.; Tinker, L.F.; Eaton, C.B.; Ahmed, A.; Manson, J.E.; Snetselaar, L.G.; Martin, L.W.; Trevisan, M.; Howard, B.V. Mediterranean and DASH diet scores and mortality in women with heart failure: The Women’s Health Initiative. Circ. Heart Fail. 2013, 6, 1116–1123. [Google Scholar] [CrossRef] [Green Version]
- Tuttolomondo, A.; Di Raimondo, D.; Casuccio, A.; Velardo, M.; Salamone, G.; Cataldi, M.; Corpora, F.; Restivo, V.; Pecoraro, R.; Della Corte, V.; et al. Mediterranean diet adherence and congestive heart failure: Relationship with clinical severity and ischemic pathogenesis. Nutrition 2020, 70, 110584. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Gea, A.; Ruiz-Canela, M. The Mediterranean Diet and Cardiovascular Health. Circ. Res. 2019, 124, 779–798. [Google Scholar] [CrossRef]
- Patel, K.; Sui, X.; Zhang, Y.; Fonarow, G.C.; Aban, I.B.; Brown, C.J.; Bittner, V.; Kitzman, D.W.; Allman, R.M.; Banach, M.; et al. Prevention of heart failure in older adults may require higher levels of physical activity than needed for other cardiovascular events. Int. J. Cardiol. 2013, 168, 1905–1909. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doukky, R.; Mangla, A.; Ibrahim, Z.; Poulin, M.F.; Avery, E.; Collado, F.M.; Kaplan, J.; Richardson, D.; Powell, L.H. Impact of Physical Inactivity on Mortality in Patients With Heart Failure. Am. J. Cardiol. 2016, 117, 1135–1143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoffmann, J.M.; Hellwig, S.; Brandenburg, V.M.; Spaderna, H. Measuring Fear of Physical Activity in Patients with Heart Failure. Int. J. Behav. Med. 2018, 25, 294–303. [Google Scholar] [CrossRef] [PubMed]
- Spaderna, H.; Hoffman, J.M.; Hellwig, S.; Brandenburg, V.M. Fear of Physical Activity, Anxiety, and Depression: Barriers to Physical Activity in Outpatients With Heart Failure? Eur. J. Health Psychol. 2020, 27, 3–13. [Google Scholar] [CrossRef]
- Ohiomoba, R.O.; Youmans, Q.R.; Akanyirige, P.W.; Ezema, A.U.; Anderson, A.S.; Bryant, A.; Jackson, K.; Mandieka, E.; Pham, D.T.; Raza, Y.; et al. History of cigarette smoking and heart transplant outcomes. Int. J. Cardiol. Heart Vasc. 2020, 30, 100599. [Google Scholar] [CrossRef] [PubMed]
- Vorlat, A.; Even, P.; Devrieze, Y.; Buyens, E.; Vermeulen, T.; Rodrigus, I.; Heidbuchel, H.; Claeys, M. The deleterious effects of smoking resumption after heart transplantation. Acta Cardiol. 2021, 76, 970–974. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Schlesinger, S.; Norat, T.; Riboli, E. Tobacco smoking and the risk of heart failure: A systematic review and meta-analysis of prospective studies. Eur. J. Prev. Cardiol. 2019, 26, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Dew, M.A.; DiMartini, A.F.; Dobbels, F.; Grady, K.L.; Jowsey-Gregoire, S.G.; Kaan, A.; Kendall, K.; Young, Q.R.; Abbey, S.E.; Butt, Z.; et al. The 2018 ISHLT/APM/AST/ICCAC/STSW Recommendations for the Psychosocial Evaluation of Adult Cardiothoracic Transplant Candidates and Candidates for Long-term Mechanical Circulatory Support. Psychosomatics 2018, 59, 415–440. [Google Scholar] [CrossRef] [PubMed]
| Original Data | Imputed Data (n = 318) | |||||||
|---|---|---|---|---|---|---|---|---|
| n | n/M | %/SD | M | %/SD | MinM/Minn | MaxM/Maxn | ||
| Demographics | ||||||||
| Gender, n (%) | 318 | |||||||
| Male | 260 | 81.8% | ||||||
| Female | 58 | 18.2% | ||||||
| Age (years) | 318 | 53.1 | 11.1 | |||||
| Education, n (%) | 318 | |||||||
| ≤9 Years | 199 | 62.6% | ||||||
| >9 Years | 119 | 37.4% | ||||||
| Medical Characteristics | ||||||||
| HFSS a | 224 | 7.9 | 0.9 | 7.86 | 0.9 | 7.9 | 7.9 | |
| Creatinine | 301 | 1.4 | 0.5 | 1.39 | 0.5 | 1.4 | 1.4 | |
| Cardiac Index | 289 | 2.0 | 0.6 | 2.06 | 0.6 | 2.0 | 2.1 | |
| Inpatient | 318 | |||||||
| Yes | 87 | 27.4% | ||||||
| No | 231 | 72.6% | ||||||
| Body Mass Index | 318 | 25.9 | 4.0 | |||||
| Psychological Factors | ||||||||
| Depressive symptoms, n (%) | 318 | |||||||
| Low | 195 | 61.3% | ||||||
| High | 123 | 38.7% | ||||||
| Social network size | 318 | 8.2 | 6.2 | |||||
| Psychosocial risk b, n (%) | 318 | |||||||
| Low | 47 | 14.8% | ||||||
| High | 271 | 85.2% | ||||||
| Emotional support, n (%) | 318 | |||||||
| Low | 58 | 18.2% | ||||||
| High | 260 | 81.8% | ||||||
| Dietary Habits | ||||||||
| Salt | 318 | 2.1 | 0.4 | |||||
| Saturated fatty acids | 318 | 2.2 | 0.4 | |||||
| PUFA + MUFA c | 318 | 2.3 | 0.4 | |||||
| Physical Activity | ||||||||
| Number of Physical Activities | 318 | 3.5 | 2.4 | |||||
| Caloric expenditure (kcal/week) | 318 | 17.0 | 17.2 | |||||
| Smoking status | 316 | |||||||
| Non (never and quit > 10 y) | 166 | 52.5% | 166 | 168 | ||||
| Former | 138 | 43.7% | 138 | 139 | ||||
| Current | 12 | 3.8% | 12 | 13 | ||||
| Death/Deteriorated (n = 92) | HU-HTx (n = 121) | Elective HTx (n = 43) | Improved (n = 39) | |||||
|---|---|---|---|---|---|---|---|---|
| Independent Variable | SHR (95% CI) | p | SHR (95% CI) | p | SHR (95% CI) | p | SHR (95% CI) | p |
| Demographics | ||||||||
| Female | 1.54 (0.95, 2.49) | 0.08 | 0.79 (0.47, 1.33) | 0.37 | 1.40 (0.69, 2.85) | 0.35 | 0.65 (0.25, 1.67) | 0.37 |
| Age (years) | 1.02 (1.00, 1.04) | 0.07 | 0.99 (0.97, 1.00) | 0.12 | 1.01 (0.98, 1.04) | 0.51 | 0.99 (0.96, 1.02) | 0.45 |
| Medical Characteristics | ||||||||
| HFSS a | 0.81 (0.64, 1.02) | 0.07 | 0.80 (0.66, 0.96) | 0.02 | 1.06 (0.70, 1.60) | 0.80 | 1.68 (1.32, 2.15) | <0.001 |
| Cardiac Index | 0.86 (0.64, 1.14) | 0.29 | 0.52 (0.38, 0.72) | <0.001 | 1.36 (1.08, 1.73) | <0.01 | 1.65 (1.25, 2.18) | <0.001 |
| Creatinine | 1.45 (0.97, 2.17) | 0.07 | 1.11 (0.79, 1.57) | 0.55 | 1.01 (0.53, 1.91) | 0.98 | 0.52 (0.23, 1.18) | 0.12 |
| Inpatient Status | 0.44 (0.25, 0.79) | <0.01 | 3.22 (2.20, 4.71) | <0.001 | 1.54 (0.81, 2.89) | 0.19 | 0.29 (0.10, 0.80) | 0.02 |
| Death/Deteriorated (n = 92) | HU-HTx (n = 121) | Elective HTx (n = 43) | Improved (n = 39) | |||||
|---|---|---|---|---|---|---|---|---|
| Independent Variable | SHR (95% CI) | p | SHR (95% CI) | p | SHR (95% CI) | p | SHR (95% CI) | p |
| Psychosocial Factors | ||||||||
| Low Depressive Symptoms uni | 0.78 (0.52, 1.18) | 0.23 | 0.80 (0.56, 1.15) | 0.23 | 1.06 (0.57, 1.97) | 0.85 | 2.59 (1.20, 5.60) | 0.02 |
| Low Depressive Symptoms adj | 0.80 (0.53, 1.22) | 0.30 | 0.81 (0.56, 1.17) | 0.27 | 1.01 (0.55, 1.86) | 0.98 | 2.52 (1.15, 5.51) | 0.02 |
| Social Networks uni | 0.97 (0.94, 1.01) | 0.11 | 1.03 (1.01, 1.06) | <0.01 | 0.98 (0.92, 1.04) | 0.53 | 1.02 (0.98, 1.06) | 0.42 |
| Social Networks adj | 0.98 (0.94, 1.01) | 0.19 | 1.02 (0.99, 1.04) | 0.28 | 0.98 (0.91, 1.05) | 0.50 | 1.01 (0.96, 1.05) | 0.77 |
| Low Psychosocial Risk uni | 0.29 (0.12, 0.73) | <0.01 | 1.53 (0.97, 2.43) | 0.07 | 0.74 (0.29, 1.90) | 0.54 | 2.58 (1.27, 5.26) | <0.01 |
| Low Psychosocial Risk adj | 0.31 (0.13, 0.78) | 0.01 | 1.66 (1.02, 2.70) | 0.04 | 0.67 (0.26, 1.72) | 0.40 | 2.45 (1.07, 5.64) | 0.04 |
| Low Emotional Support uni | 1.12 (0.67, 1.89) | 0.66 | 0.83 (0.50, 1.36) | 0.46 | 1.57 (0.80, 3.09) | 0.19 | 0.81 (0.34, 1.95) | 0.64 |
| Low Emotional Support adj | 1.24 (0.74, 2.08) | 0.42 | 0.83 (0.49, 1.39) | 0.48 | 1.69 (0.85, 3.37) | 0.13 | 0.61 (0.23, 1.62) | 0.32 |
| Dietary Habits | ||||||||
| Salty Foods uni | 0.56 (0.32, 0.98) | 0.04 | 2.60 (1.45, 4.67) | <0.01 | 0.90 (0.36, 2.23) | 0.81 | 0.67 (0.29, 1.53) | 0.34 |
| Salty Foods adj | 0.58 (0.32, 1.06) | 0.08 | 1.73 (0.93, 3.20) | 0.08 | 1.21 (0.47, 3.11) | 0.70 | 0.75 (0.28, 2.04) | 0.57 |
| PUFA + MUFA uni | 0.76 (0.48, 1.19) | 0.23 | 1.08 (0.71, 1.65) | 0.72 | 0.52 (0.27, 0.99) | 0.05 | 2.13 (1.01, 4.48) | 0.05 |
| PUFA + MUFA adj | 0.74 (0.46, 1.19) | 0.21 | 1.16 (0.76, 1.79) | 0.49 | 0.47 (0.22, 0.98) | 0.04 | 2.20 (1.03, 4.71) | 0.04 |
| Physical Activity | ||||||||
| Number of Physical Activities uni | 0.97 (0.89, 1.05) | 0.46 | 0.88 (0.81, 0.96) | <0.01 | 1.03 (0.91, 1.16) | 0.68 | 1.17 (1.07, 1.27) | <0.001 |
| Number of Physical Activities adj | 1.00 (0.92, 1.08) | 0.90 | 0.95 (0.87, 1.04) | 0.28 | 1.05 (0.92, 1.19) | 0.51 | 1.12 (1.01, 1.25) | 0.03 |
| Smoking Status | ||||||||
| Non-Smoking (Referent) | ||||||||
| Former uni | 1.18 (0.78, 1.80) | 0.44 | 0.88 (0.61, 1.26) | 0.48 | 0.73 (0.39, 1.36) | 0.32 | 0.92 (0.48, 1.75) | 0.79 |
| Current uni | 2.38 (0.98, 5.79) | 0.06 | 0.36 (0.09, 1.50) | 0.16 | 0.50 (0.07, 3.47) | 0.48 | 1.41 (0.32, 6.25) | 0.65 |
| Former adj | 1.49 (0.95, 2.35) | 0.09 | 0.74 (0.50, 1.10) | 0.14 | 0.79 (0.41, 1.51) | 0.47 | 0.77 (0.39, 1.49) | 0.43 |
| Current adj | 2.49 (1.06, 5.85) | 0.04 | 0.31 (0.07, 1.29) | 0.11 | 0.56 (0.08, 3.92) | 0.56 | 1.72 (0.39, 7.56) | 0.47 |
| Death/Deteriorated (n = 92) | HU-HTx (n = 121) | Elective HTx (n = 43) | Improved (n = 39) | |||||
|---|---|---|---|---|---|---|---|---|
| Independent Variable | SHR (95% CI) | p | SHR (95% CI) | p | SHR (95% CI) | p | SHR (95% CI) | p |
| Psychosocial Factors | ||||||||
| Low Psychosocial Risk | 0.34 (0.13, 0.86) | 0.02 | 1.45 (0.89, 2.37) | 0.14 | 0.59 (0.23, 1.49) | 0.26 | 2.41 (0.99, 5.83) | 0.052 |
| Dietary Habits | ||||||||
| Salty Foods | 0.57 (0.31, 1.03) | 0.06 | 2.19 (1.20, 3.99) | 0.01 | 1.26 (0.49, 3.25) | 0.63 | 0.61 (0.22, 1.71) | 0.35 |
| PUFA + MUFA | 0.72 (0.44, 1.18) | 0.20 | 1.18 (0.76, 1.84) | 0.46 | 0.41 (0.18, 0.94) | 0.04 | 2.27 (1.04, 4.96) | 0.04 |
| Physical Activity | ||||||||
| Number of Physical Activities | 1.00 (0.92, 1.09) | 0.95 | 0.79 (0.71, 0.89) | <0.001 | 1.06 (0.92, 1.23) | 0.44 | 1.13 (1.02, 1.25) | 0.03 |
| Smoking Status | ||||||||
| Non-Smoking (Referent) | ||||||||
| Former | 1.28 (0.83, 1.99) | 0.26 | 0.78 (0.53, 1.16) | 0.23 | 0.65 (0.30, 1.39) | 0.27 | 0.87 (0.44, 1.73) | 0.70 |
| Current | 2.67 (1.08, 6.61) | 0.03 | 0.33 (0.08, 1.41) | 0.13 | 0.48 (0.06, 3.67) | 0.48 | 1.35 (0.21, 8.82) | 0.75 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gali, K.; Weidner, G.; Smits, J.M.A.; Beyersmann, J.; Spaderna, H. Psychosocial Risk and Health Behaviors as Predictors of Clinical Events in Patients Wait-Listed for a New Heart: Results from 7 Years of Follow-Up. Life 2021, 11, 1438. https://doi.org/10.3390/life11121438
Gali K, Weidner G, Smits JMA, Beyersmann J, Spaderna H. Psychosocial Risk and Health Behaviors as Predictors of Clinical Events in Patients Wait-Listed for a New Heart: Results from 7 Years of Follow-Up. Life. 2021; 11(12):1438. https://doi.org/10.3390/life11121438
Chicago/Turabian StyleGali, Kathleen, Gerdi Weidner, Jacqueline M. A. Smits, Jan Beyersmann, and Heike Spaderna. 2021. "Psychosocial Risk and Health Behaviors as Predictors of Clinical Events in Patients Wait-Listed for a New Heart: Results from 7 Years of Follow-Up" Life 11, no. 12: 1438. https://doi.org/10.3390/life11121438
APA StyleGali, K., Weidner, G., Smits, J. M. A., Beyersmann, J., & Spaderna, H. (2021). Psychosocial Risk and Health Behaviors as Predictors of Clinical Events in Patients Wait-Listed for a New Heart: Results from 7 Years of Follow-Up. Life, 11(12), 1438. https://doi.org/10.3390/life11121438







