1. Introduction
The well-being of the growing elderly population is becoming an increasingly important social and governmental concern [
1]. A significant proportion of frail and lonely older adults prefer to stay in their own homes rather than moving to residential care establishments, as relocation could be both financially burdensome and psychologically distressing [
2]. Aging can cause various complications, particularly for those living alone. Studies indicate a rising trend of older adults found deceased in their homes in England and Wales, unnoticed long after passing away. These so-called “undefined deaths” have been steadily increasing since 1980, linked to social isolation, austerity measures, and societal fragmentation [
3]. As reported by a study, “many people would be shocked that someone can lie dead at home for days, weeks, or even longer without anyone raising an alarm” [
4]. This growing crisis highlights a critical need for technological developments that can detect abnormal inactivity and provide timely alerts to caregivers.
Advancements in mobile technology offer potential solutions to this issue. Mobile phones are widely used across populations and contain built-in sensors, such as accelerometers, which, when combined with appropriate software, can monitor movement and detect anomalies in daily activity patterns [
5,
6]. Despite these opportunities, existing Internet of Things (IoT) deployments for healthcare, including innovative smart home environments and sensor networks specifically aimed at elderly monitoring, often present limitations [
7,
8]. These systems, while providing continuous data collection and alert capabilities, frequently face hurdles related to installation complexity, power management, and user acceptance, particularly for solutions requiring dedicated infrastructure beyond a conventional mobile phone [
9]. While recent advances in intelligent monitoring have leveraged powerful AI-driven models such as hybrid deep learning architectures (e.g., convolutional neural networks and long short-term memory neural networks) to improve anomaly detection [
10,
11,
12], there remains a significant research gap for a highly accessible, unobtrusive, and computationally efficient system suitable for real-time monitoring directly on conventional smartphones.
This study addresses this gap by introducing a novel remote monitoring system designed to enhance the safety and well-being of elderly individuals living independently. A key innovation of this system is its integration of fuzzy logic, an artificial intelligence (AI)-inspired approach, to analyze movement data and accurately detect abnormal patterns, such as prolonged inactivity. Fuzzy logic has been widely applied in various domains, including wireless computer networks, for identifying irregular patterns [
13,
14]. Our approach uniquely harnesses fuzzy logic due to its interpretability, low computational footprint, and suitability for real-time processing directly on standard mobile devices. This makes our system exceptionally cost-effective, non-wearable, and user-friendly, operating unobtrusively in the background without requiring undue technological expertise from users. Proactive remote monitoring not only enhances the safety and well-being of elderly individuals but also provides peace of mind for caregivers and family members, ensuring timely intervention in critical situations.
The primary objective of this pilot study is to develop and validate a functional prototype of a smartphone-based remote monitoring application that utilizes a novel fuzzy logic methodology to classify and detect abnormal movements, specifically prolonged inactivity. This system is intended to automatically dispatch timely alerts to designated caregivers or family members, thereby providing a simple, cheap, and easy solution to prevent unnoticed medical emergencies and directly address the concerning issue of elderly individuals dying unnoticed at home for extended periods.
The remainder of this paper is organized as follows:
Section 2 provides a comprehensive review of related studies on elderly monitoring and anomaly detection.
Section 3 details the methodology of our proposed fuzzy logic-based system.
Section 4 presents and discusses the experimental results.
Section 5 includes a discussion of our findings.
Section 6 outlines the study’s limitations and suggests future directions, while
Section 7 concludes the paper.
2. Literature Reviews
2.1. Remote Patient Monitoring
Remote patient monitoring (RPM) is a modern healthcare tool that enables healthcare providers and caregivers to track a patient’s health from a distance. Utilizing devices like smartphones, wearable sensors, or other technologies, RPM collects vital health data, such as heart rate, blood pressure, or activity levels, and transmits it to healthcare providers in real time. This capability aids in the early detection of potential problems, allowing for timely intervention before conditions worsen. For patients, particularly those with chronic conditions or recovering from illness, RPM offers a convenient way to maintain a connection with their care team, reducing the need for frequent hospital visits. It can be an effective means to improve health outcomes and make healthcare more accessible [
15]. Technological advancements have increasingly enabled patients to engage in normal daily activities at home while still being monitored through modern communication methods [
3,
16].
RPM systems facilitate timely emergency responses, contributing to reduced untimely deaths and healthcare costs through various communication technologies [
17]. Remote monitoring has proven useful in predicting diseases like diabetes and hypertension [
18], and in overseeing physiological signs [
19], pulmonary disease [
20], chronic illnesses [
21], and human activities [
22]. These systems target diverse subgroups, including individuals diagnosed with chronic illnesses, those with mobility issues or other disabilities, post-surgery patients, neonates, and elderly patients [
15,
16].
However, the main challenges with existing RPM approaches include variability in the accuracy of data collected by devices, which can lead to potential misdiagnosis or missed alerts. Patients, especially older adults or those with limited technological skills, may struggle to use RPM devices effectively. Furthermore, RPM can increase the workload for healthcare providers, potentially leading to burnout or inefficiencies. While RPM shows promise, long-term data on its comprehensive effectiveness in improving health outcomes or significantly reducing healthcare costs remains limited. RPM devices may also face technical challenges such as restricted battery life, connectivity issues, or inconsistent performance in diverse environments. Prior studies have additionally demonstrated that the accuracy of these methods can decline significantly when applied to both institutionalized and independent elderly individuals [
17]. To address these shortcomings, research trends in RPM are increasingly focusing on solutions that leverage readily available technology for specific needs like movement detection and analysis in home environments. By exploring approaches that utilize built-in sensors of conventional mobile phones and integrate advanced logic for activity analysis, studies aim to provide user-friendly, cost-effective, and non-intrusive solutions tailored to the elderly population, thereby enhancing the effectiveness and accessibility of remote patient monitoring.
2.2. Mobile Apps for Remote Monitoring
Traditional monitoring systems often rely on body-attached sensors, which can limit patient mobility and affect daily activities. This discomfort may distort physiological readings, especially among elderly patients, potentially misrepresenting their actual health conditions [
17]. To overcome these limitations, the use of mobile devices equipped with a variety of built-in sensors—such as GPS, vision, audio, light, temperature, direction, and acceleration—has created significant opportunities for data mining applications in health monitoring [
23,
24,
25]. Accurate body motion tracking with sensors typically requires strategic placement, ideally near the body’s center of mass (e.g., breastbone, lower back, or waist) to maximize data accuracy [
22]. Despite the potential of RPM, current devices often present challenges, including prohibitive costs that limit accessibility. Furthermore, their designs may not adequately address the diverse needs, experiences, and limitations of individual users, hindering effective adoption and long-term use. Smartphones, equipped with accelerometers and gyroscopes, offer a readily available option, and their common placement in pockets allows for effective motion tracking. However, further research is needed to establish their comprehensive accuracy and reliability for diverse monitoring applications.
The development of mobile applications for RPM running on tablets and smartphones eliminates the requirement for expensive, dedicated hardware [
26]. Such applications also enable patients to report symptoms and notify medical teams promptly if conditions worsen, facilitating timely healthcare decisions and reducing the need for in-person visits and associated delays [
26]. Several frameworks exist for mobile application development. Researchers have developed RPM applications using Java under the ADT (Android Development Toolkit by Google) [
27]. Despite its advantages, Java has limitations, such as a lack of inherent cross-platform integration [
28]. This limitation can be addressed by using cross-platform frameworks like Xamarin or React-Native, maintained by Microsoft and Facebook, respectively [
29]. For example, the Xamarin framework enables developers to create high-performance, native-like mobile applications for Android and iOS from a single C# codebase, significantly reducing development time and effort. It also offers seamless integration with the .NET ecosystem and access to native APIs, ensuring robust and feature-rich applications [
29].
2.3. Accelerometry Operation
Research in activity monitoring increasingly focuses on non-invasive sensors, which overcome the limitations of invasive counterparts, such as subject discomfort [
30]. Researchers, such as [
25], have investigated the utilization of multiple sensors, including microphones, accelerometers, GPS, and cameras, embedded in commercial smartphones for recognizing activities and enhancing mobile social networking applications. Among these, the accelerometer sensor, integrated as part of a mobile device, is particularly appealing due to its unobtrusive nature, its ability to gather data without extra equipment, and its potential for precise interpretation [
24].
Human activity detection using a triaxial accelerometer typically involves three stages: pre-processing, feature extraction, and classification [
31]. Feature extraction commonly involves deriving acceleration peaks, variance, fundamental frequencies’ magnitudes, intensity, and position relations [
24,
31]. Studies in this area often utilize magnitude accelerometry features to predict human movement or its absence, classifying it as normal or abnormal.
The ubiquity of smartphones presents a compelling opportunity for RPM, particularly given the advancements in accelerometer technology integrated within these devices. Leveraging existing hardware like smartphones reduces the burden on both patients and healthcare systems by eliminating the need for specialized, often costly, equipment [
32]. The increasing integration of mobile devices, connected objects, and sensors into healthcare applications highlights the viability of smartphone-based monitoring for diverse patient populations [
33]. This technological availability plays a crucial role in enabling the scalability and feasibility of remote monitoring programs [
33].
Modern smartphone accelerometers, although not classified as medical-grade devices, can offer effective operation for numerous remote monitoring applications, especially those focused on gross motor activity, falls, and certain movement disorders [
34]. Numerous studies have directly compared smartphone accelerometry data with data obtained from research-grade wearable sensors or gold-standard motion capture systems. These studies often assess metrics such as fall detection accuracy, step count accuracy, and activity recognition accuracy. For instance, research has shown that smartphone accelerometers can achieve high sensitivity and specificity in fall detection algorithms [
34]. Similarly, studies have explored the use of these accelerometers for monitoring physical activity levels, gait patterns, and even subtle tremors in patients with conditions like Parkinson’s disease [
35]. While it is essential to acknowledge the limitations of smartphone accelerometers in detecting very fine movements or subtle changes, the level of accuracy they provide is often sufficient for many remote monitoring applications. A balanced discussion of these limitations strengthens the argument for their use by demonstrating a thorough understanding of the technology, including ongoing efforts to improve reliability and reduce issues such as false fall alerts through advanced techniques like deep learning [
36].
The real-time or near real-time data acquisition capabilities of smartphone accelerometers enable rapid detection of critical events, such as falls, and can trigger timely interventions. Smartphone processors are powerful enough to handle accelerometry data and execute algorithms in real-time, facilitating immediate feedback and alerts. Furthermore, the inherent connectivity of smartphones allows for seamless data transmission to healthcare providers or caregivers. For example, systems can be designed to automatically detect a fall and send an alert to designated contacts [
37]. Real-time activity data can also be used to provide personalized feedback and reminders to encourage adherence to exercise programs.
2.4. Fuzzy Logic in Activity Detection
As discussed by researchers [
31], the classification stage is crucial in detecting human activity. Researchers [
23] employed the k-nearest algorithm (KNN) to detect five human activities like phone detached, idle, walking, running, and jumping. The KNN classifier, although straightforward and widely employed, can achieve performance comparable to that of more sophisticated classifiers [
37]. Researchers such as [
37,
38] employed convolutional neural networks (CNNs) for predicting six human activities, including jogging, walking, going upstairs, going downstairs, sitting, and standing. Deep learning models like CNNs have demonstrated notable accuracy potential but necessitate more training data and computational resources.
To address limitations observed in existing RPM approaches, fuzzy logic has emerged as a promising method for interpreting accelerometry data. Fuzzy logic offers advantages in modeling complex systems with imprecise data by allowing variables to have degrees of truth, which enhances its suitability for real-world applications. Fuzzy logic can perform well with smaller datasets because it relies on fuzzy rules and membership functions rather than extensive training datasets. It can generalize effectively even with limited data, making it suitable for applications where data collection is challenging or expensive. Additionally, fuzzy logic systems are interpretable, allowing experts to understand and refine the rules and membership functions to improve system performance [
39]. Collected data can undergo analysis using fuzzy logic to identify human activities. In cases where anomalies are detected, alerts would be promptly sent to the emergency contact people added in the mobile application. This approach leverages fuzzy logic’s capability to interpret and respond to complex, uncertain data patterns, ensuring timely intervention and enhanced monitoring effectiveness [
40].
In summary, while many studies highlight the growing field of Remote Patient Monitoring (RPM), offering broad insights into its potential, they often do so without delving into specific, cost-effective solutions for individual behavioral monitoring using readily available technology. For instance, reviews like Shaik et al. [
41] broadly cover how AI and technologies such as IoT wearables can transform RPM. Holtz et al. [
42] focus on the promise of RPM from a strategic, policy, and infrastructure standpoint, discussing its role in addressing healthcare inequities. Similarly, systematic reviews by Tan et al. [
43] examine the impacts of various RPM interventions, including smartphone apps and wearables, on patient safety, adherence, and cost-related outcomes during care transitions. While these papers provide valuable overviews and impact analyses, they do not focus on the specific, practical needs our study addresses. For example, systems like the one in Zhang et al. [
44] do use smartphones, but they often rely on external wearable sensors for physiological data, which adds cost and complexity. Another advanced approach by Chinnaperumal et al. [
45] integrates complex AI with 5G networks for secure medical data acquisition, focusing on high-tech infrastructure. In sharp contrast to these approaches, our study does not use any separate IoT devices or external wearables. Instead, we uniquely leverage only the built-in accelerometer of a standard smartphone, making our system highly affordable and accessible. Our research further distinguishes itself by applying fuzzy logic—an AI method well-suited for real-time decision-making under uncertainty—to precisely detect abnormal inactivity (lack of movement). This specific focus directly addresses a critical, often overlooked, safety concern: preventing unnoticed deaths of lonely individuals, thereby offering a practical, user-friendly, and life-saving application within the broader RPM landscape.
3. Methods
This study employed quantitative and experimental methodologies to develop and validate a smartphone-based remote patient monitoring system. Our primary goal was to create a user-friendly and cost-effective eHealth solution capable of detecting abnormal inactivity and potential falls in elderly individuals, triggering timely alerts to caregivers. This section details the system’s architecture, mobile application development, data acquisition, the core fuzzy logic-based anomaly detection algorithm, and the notification system.
3.1. System Overview and Architecture
Our proposed system operates on a conventional mobile phone, leveraging its built-in accelerometer to continuously monitor user activity.
Figure 1 illustrates the overarching workflow. The system collects movement data in real-time, processes it using a fuzzy logic module, and then dispatches immediate alerts to designated caregivers if abnormal activity (prolonged inactivity or a fall) is detected. If activity is deemed normal, the system remains unobtrusive and takes no action.
The mobile application was developed using the ASP.NET Xamarin framework (version 5.0.0, Microsoft Corporation, Redmond, WA, USA) with C# as the primary programming language, and deployed on Samsung Galaxy 5G smartphones (Samsung, Suwon, Republic of Korea), with testing specifically conducted on models such as the Galaxy A53 5G, A73 5G, and M54 5G running Android version 12.0.0. It integrates a Python-based fuzzy logic engine (Python 3.10.x, Python Software Foundation, Beaverton, OR, USA) for intelligent decision-making, utilizing scikit-fuzzy (version 0.4.1), a common Python fuzzy logic library. Accelerometer data, collected by the Xamarin.Essentials.Accelerometer API (version 1.7.0, Microsoft Corporation, Redmond, WA, USA), are processed to extract the Signal Magnitude Vector (SMV) and timestamp. These data points are stored locally on the phone’s internal memory using SQLite (version 3.39.x, open-source). The stored data then serves as inputs to the Python fuzzy logic engine, which analyzes movement patterns based on predefined static rules to classify user activity and detect anomalies.
3.2. Mobile Application Development and Features
The mobile application was developed with user-friendliness and continuous, unobtrusive monitoring in mind, particularly for elderly users. We used the ASP.Net Xamarin framework with C# as the primary programming language, allowing for cross-platform development targeting Android devices. Testing was conducted on various Samsung 5G smartphones (e.g., Galaxy A53 5G, A73 5G, and M54 5G) running Android version 12.0.0, all equipped with built-in accelerometers and gyroscopes.
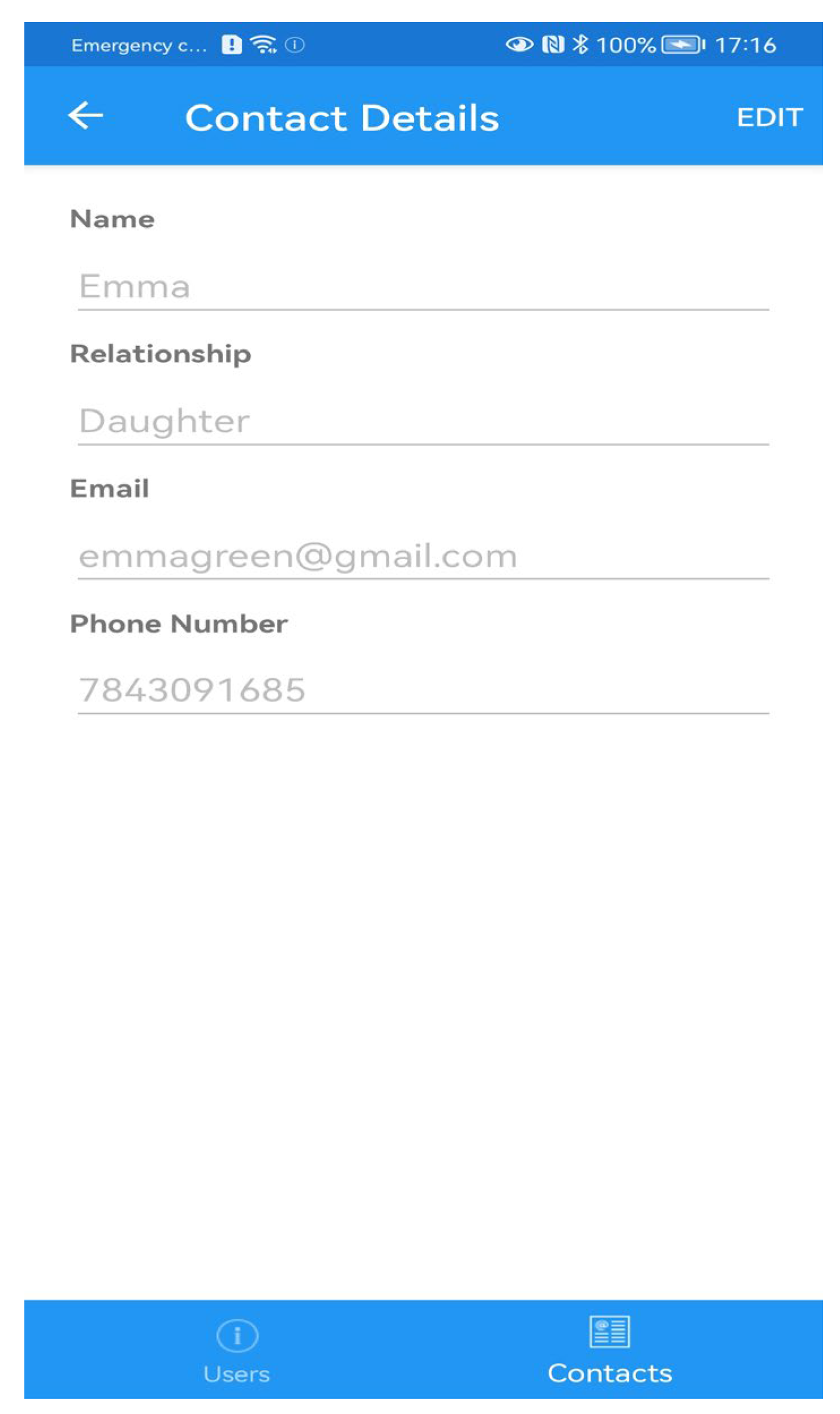
Designed for minimal user interference, the app operates seamlessly in the background, continuously collecting accelerometry data and performing activity analysis without requiring constant interaction. Upon installation, users grant necessary permissions and receive essential information about the app’s functionality. The application’s interface, exemplified by
Figure 2, prominently displays participant details (name, age, and gender) at the top, along with real-time motion activity graphs for the current day. To facilitate long-term health management and trend analysis, it also generates historical motion activity graphs for one week, one month, and three months. In these activity graphs, green lines illustrate a detected moving state (activity level plotted on the y-axis against time on the x-axis), while red lines signify an idle (not moving) state. This aggregated activity information is subsequently fed into the fuzzy logic module for classification and alert decision-making.
Figure 3 presents the interface for managing caregiver contact details, including name, phone number, email address, and relationship to the monitored individual.
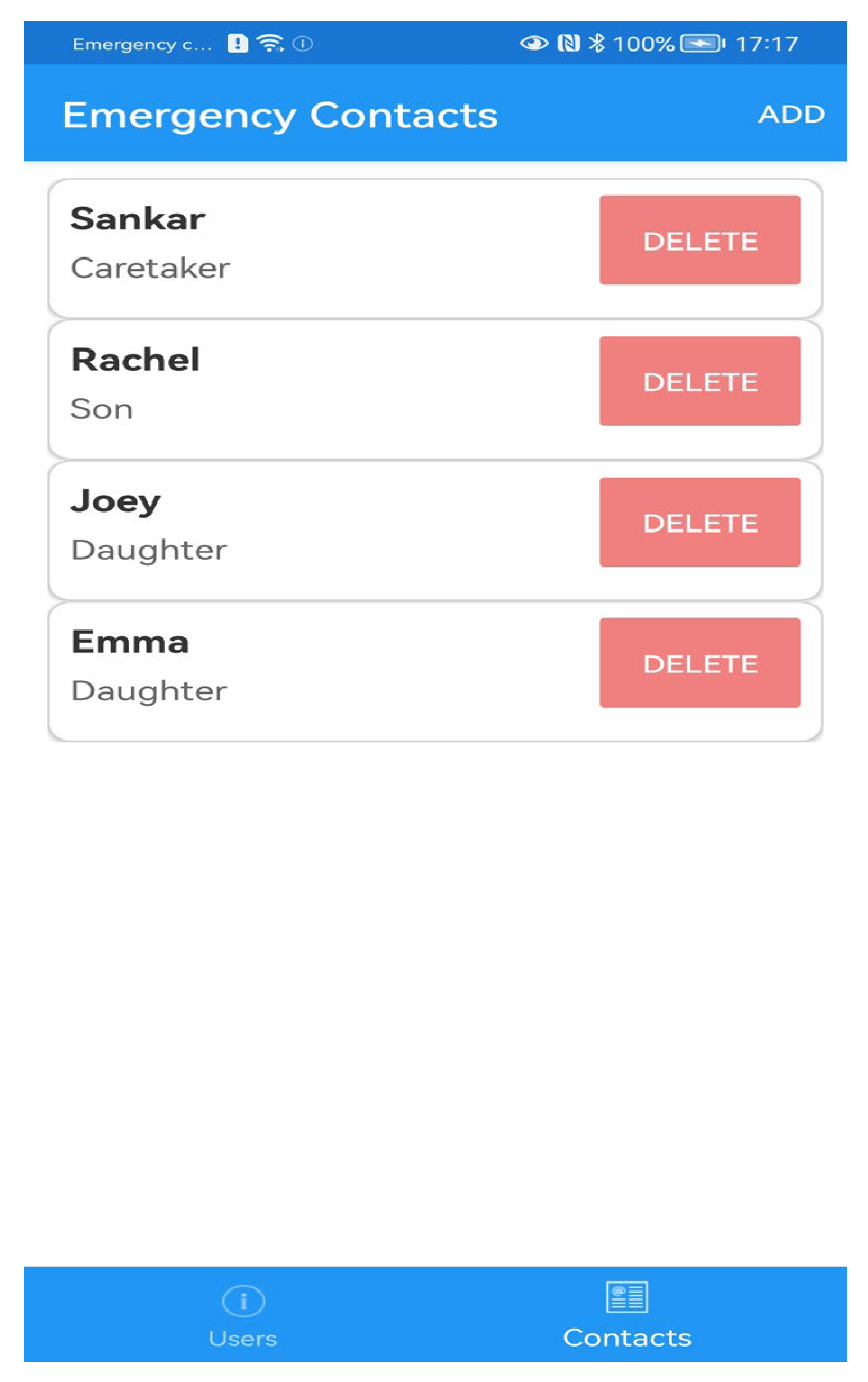
Further enhancing user control and safety,
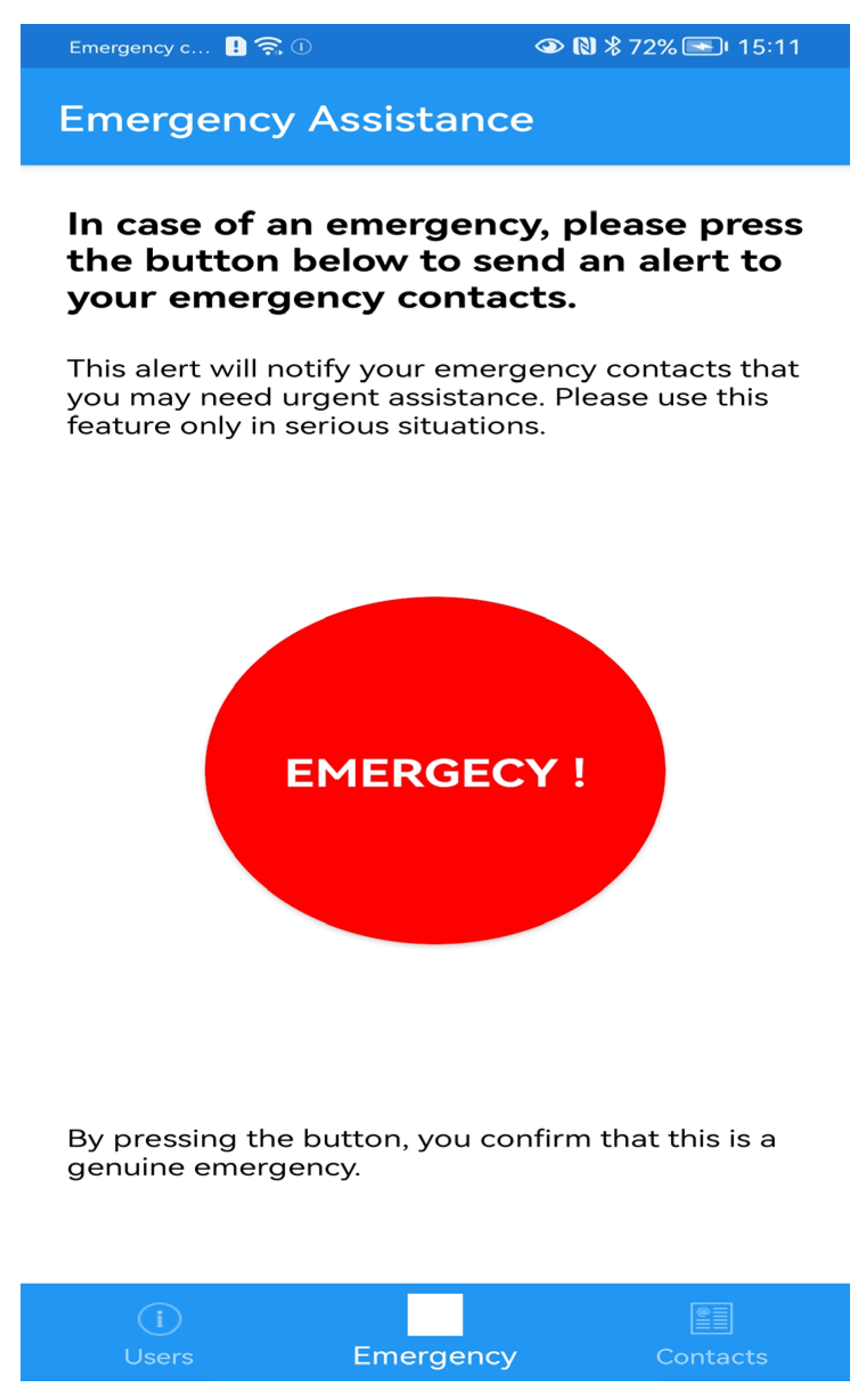
Figure 4 shows all configured caregiver (emergency) contacts, providing a comprehensive overview of designated recipients for alerts. Additionally, the application includes a prominent emergency button (shown in red in
Figure 5), enabling elderly users to manually send immediate alerts to caregivers in critical situations.
3.3. Accelerometer Data Acquisition and Local Storage
Accelerometer data, essential for monitoring user activity, are collected using Xamarin.Essentials.Accelerometer (version 1.7.0, Microsoft Corporation, Redmond, WA, USA), which provides processed
x,
y, and
z values along with corresponding timestamps. These raw accelerometer data are pre-processed to extract the Signal Magnitude Vector (
SMV), calculated using
For real-time monitoring, accelerometer data are collected at one-minute intervals (every 60 s). For each one-minute interval, only the highest Signal Magnitude Vector (SMV) recorded within that minute was retained. This single, highest SMV value per minute then served as the primary input feature for the fuzzy logic classification system.
A key advantage of this design is that all data are stored locally on the smartphone using SQLite, a lightweight, open-source, serverless database engine. This approach eliminates reliance on cloud storage, which may be susceptible to Internet connectivity issues, and significantly enhances data privacy and security by keeping sensitive information confined to the user’s device, reducing the risk of unauthorized access.
The SQLite database stores the three-dimensional acceleration data, the calculated SMV, and the corresponding timestamps. This method optimizes storage demands while preserving meaningful information for analysis. The database is designed to hold up to three months of historical acceleration data, enabling long-term activity tracking and pattern analysis valuable for identifying behavioral trends or sudden changes. To maintain optimal performance and storage capacity, data older than three months are automatically deleted. This design balances data privacy, local storage constraints, and real-time processing efficiency, ensuring the application remains responsive on mobile devices.
3.4. Fuzzy Logic-Based Activity and Anomaly Detection
The developed mobile application, integrated into conventional smartphones, continuously monitors user activity using its built-in accelerometer to collect movement data. This data is then processed via a fuzzy logic module to detect abnormal activity, such as prolonged inactivity or falls, enabling informed alert decisions. The system’s overall workflow is presented and generally explained in
Section 3.1 and visualized in
Figure 1.
This section details the fuzzy logic system, which forms the core AI for classifying activity levels and detecting anomalies. The system operates on a static set of fuzzy rules and membership functions, optimized for real-time performance on resource-constrained mobile devices. The system utilizes two primary fuzzy inputs: the Signal Magnitude Vector (
SMV), derived from accelerometer data as described in
Section 3.3, and the time of day input.
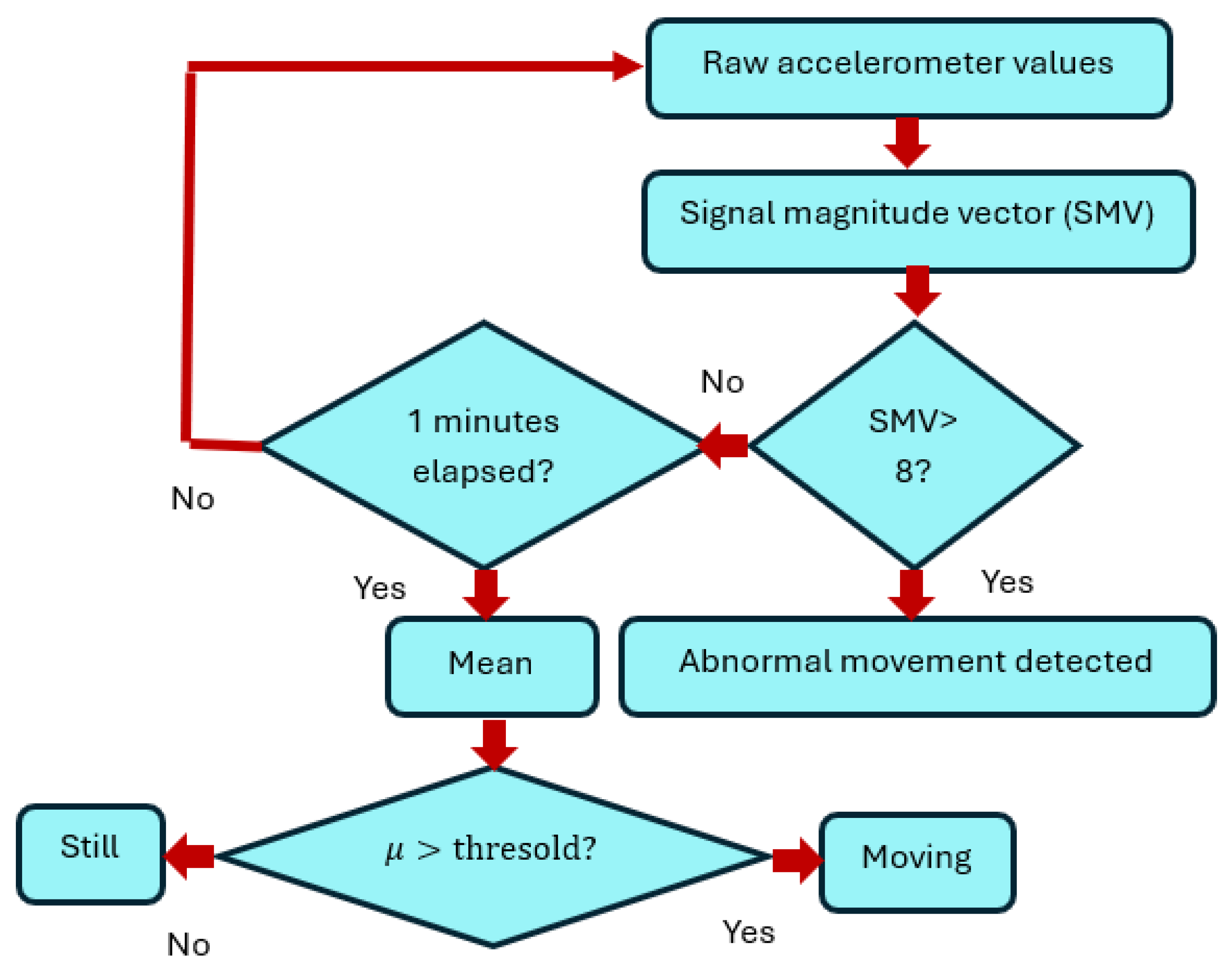
Before the main fuzzy logic processing, an initial classification algorithm processes raw accelerometer data to identify immediate abnormal movements (like falls) and categorize general activity states (moving or still).
Figure 6 presents the flowchart for this developed classification algorithm (where
μ = Mean).
The process of detecting activity and potential anomalies starts by continuously gathering raw movement data from the smartphone’s built-in accelerometer. This raw data is immediately used to calculate the Signal Magnitude Vector (SMV), which is a single number representing the overall strength or intensity of the user’s movement at any given moment. The system first performs a quick check: If this SMV value instantly jumps above 8, it is considered a sudden, strong impact, like a fall, and an “Abnormal movement detected” alert is triggered right away for a quick response. If the SMV does not jump above 8, meaning no immediate fall is detected, the system then begins to monitor activity over time. It continuously collects SMV data and watches if one minute has passed. If not, it keeps gathering more data until a full minute is complete. Once a minute has passed, the system calculates the average (or mean, represented by μ) of all the SMV values collected during that minute. This average SMV provides a smoother picture of the user’s activity level during that time. Finally, this average SMV (μ) is compared to a set crisp threshold to define the user’s preliminary activity state. If the average movement (μ) is above this crisp threshold, the user is classified as “Moving”, indicating they are active. If the average movement is at or below the crisp threshold, the user is classified as “Still”, indicating a period of inactivity. This initial classification of “Moving”, “Still”, or “Abnormal movement detected” provides the basic information that feeds into the more advanced fuzzy logic system. In the fuzzy logic module (as detailed in upcoming sections describing fuzzy sets and rules), these states and SMV values are further processed to determine nuanced activity levels and trigger alerts based on complex conditions, such as prolonged inactivity.
3.4.1. Fuzzification
Fuzzification is the process of converting crisp, numerical input values (like SMV or time of day) into degrees of membership for predefined fuzzy sets. For this system, standard Triangular and Trapezoidal membership functions were employed, as commonly found in Python fuzzy logic libraries like scikit-fuzzy. The parameters defining the precise shape and range of these membership functions were initially established using an “Intuition method” and subsequently refined through manual adjustment based on empirical observations and optimization of detection performance.
Time of Day Fuzzification
The “Time of Day” input is fuzzified into three distinct fuzzy sets: Night, Day, and Evening. This process allows the system to apply different logic based on the typical behavioral patterns expected during various periods of a 24 h cycle. These sets utilize static membership functions defined by specific time boundaries, transforming a precise hour into a degree of belonging to “Night”, “Day”, or “Evening”.
Table 2 provides illustrative examples of the parameters for these membership functions.
These membership functions define how each hour of the day contributes to the “Day”, “Evening”, or “Night” categories, with overlaps allowing for smooth transitions between periods. For example, the “Day” fuzzy set uses a Trapezoidal membership function with parameters [22, 23, 5, 6]. This means its membership begins to increase from 22:00 (10 p.m.), reaches full (100%) membership between 23:00 (11 p.m.) and 5:00 (5 a.m.), and then gradually decreases to zero by 6:00 (6 a.m.).
The “Evening” fuzzy set uses a Triangular membership function with parameters [7, 13, 19]. For this set, membership starts at 7:00 (7 a.m.), reaches its peak (100%) at 13:00 (1 p.m.), and then drops to zero by 19:00 (7 p.m.).
Lastly, the “Night” fuzzy set, also a Trapezoidal function, has parameters [17, 19, 22, 24]. Here, membership begins to increase from 17:00 (5 p.m.), reaches full membership between 19:00 (7 p.m.) and 22:00 (10 p.m.), and then gradually decreases to zero by midnight (24:00). These specific fuzzy definitions enable the system to adapt its behavior and alert strategies to different periods of the day as defined by these sets.
3.4.2. Fuzzy Inference System (FIS)
The fuzzified inputs are fed into the Fuzzy Inference System. This system employs a Mamdani-type inference engine, which is widely used for its interpretability. It processes the inputs using a static set of nine predefined “IF-THEN” fuzzy rules. These rules, detailed in
Table 3, combine the fuzzified activity level (Low, Medium, High) and time of day (Night, Day, Evening) to infer the appropriate output, such as “Normal Activity”, “Inactivity Detected”, or “Fall Detected”.
The “Action” column in
Table 3 defines the system’s immediate response based on the inferred activity output. For instance, the “Start 4-h timer” action is triggered when the system detects a “Low” activity level during “Day” or “Evening” hours (Rules 1 and 3). Instead of immediately triggering an alert, the system initiates a 4 h inactivity timer. This means the system will wait for four continuous hours of low activity; if movement does not resume within this 4 h period, it indicates prolonged inactivity, and an alert will then be dispatched to caregivers. This timer helps to avoid false alarms for short periods of rest, ensuring alerts are only sent for genuinely concerning extended inactivity.
Conversely, the “Start 3 s timer” action is specifically triggered when a “High” activity level is detected, regardless of the time of day (Rules 7, 8, and 9). A high activity level is indicative of a sudden, forceful movement, strongly suggesting a fall. Upon detecting such high activity, the system immediately starts a 3 s monitoring timer. During these 3 s, the system re-confirms the fall event; if the high activity is sustained or validated within this very short window (e.g., no immediate recovery movement), an emergency alert is rapidly sent to caregivers. This brief timer ensures quick verification while prioritizing swift notification for critical events like falls.
3.4.3. Defuzzification
Defuzzification is the final stage of the fuzzy logic process, as illustrated in the overall architecture shown in
Figure 7. Its primary function is to convert the aggregated fuzzy output from the Fuzzy Inference System (FIS), which represents the inferred state (e.g., degree of “Inactivity Detected”), into a single, crisp, and actionable decision that the system can execute. For this specific system, the Centroid (Center of Area) method was employed for defuzzification. This method calculates the center of gravity of the combined output fuzzy set, effectively yielding a precise numerical value that then directly triggers the appropriate actionable response.
This crisp numerical output then dictates the system’s subsequent actions, as defined by the fuzzy rules detailed in
Table 3. For instance, if the fuzzy logic system identifies a “Low” activity level during “Day” or “Evening” hours (corresponding to Rules 1 and 3 in
Table 3), the defuzzified output triggers a 4 h inactivity timer. This timer ensures that an alert is only sent to caregivers if the user remains continuously inactive for this full four-hour period, providing a contextual buffer to avoid false alarms during normal, extended rest. Conversely, if a “High” activity level is detected, indicating a potential fall (corresponding to Rules 7, 8, and 9 in
Table 3), the defuzzified output instantly activates a 3 s monitoring timer. This brief timer allows for immediate verification of the high-intensity event; if normal activity does not resume within these three seconds, caregivers are promptly notified of a potential emergency, prioritizing rapid response for critical situations.
3.5. Alert Notification System
When abnormal activity is detected based on the fuzzy logic output and timer thresholds, the system automatically dispatches alerts to designated emergency contacts. These alerts are sent via email using SMTP (Simple Mail Transfer Protocol) to all contacts specified by the individual during the application’s setup. Additionally, an SMS notification is dispatched to the primary carer’s phone number.
Figure 8 provides an example of an email alert dispatched by the system upon detecting an abnormality.
4. Results
This section presents the experimental findings and performance validation of the developed smartphone-based remote monitoring system. The system was rigorously tested with six volunteer participants, comprising university staff and MSc students, who installed and used the application on their mobile phones over a continuous two-month period. These tests were designed to evaluate the system’s effectiveness in detecting both abnormal events (such as falls) and prolonged periods of inactivity, triggering timely alerts when appropriate. In total, 123 fall scenarios and 138 idle scenarios were tested across the six participants, as detailed below in
Table 4.
4.1. Evaluation Metrics and Overall Performance
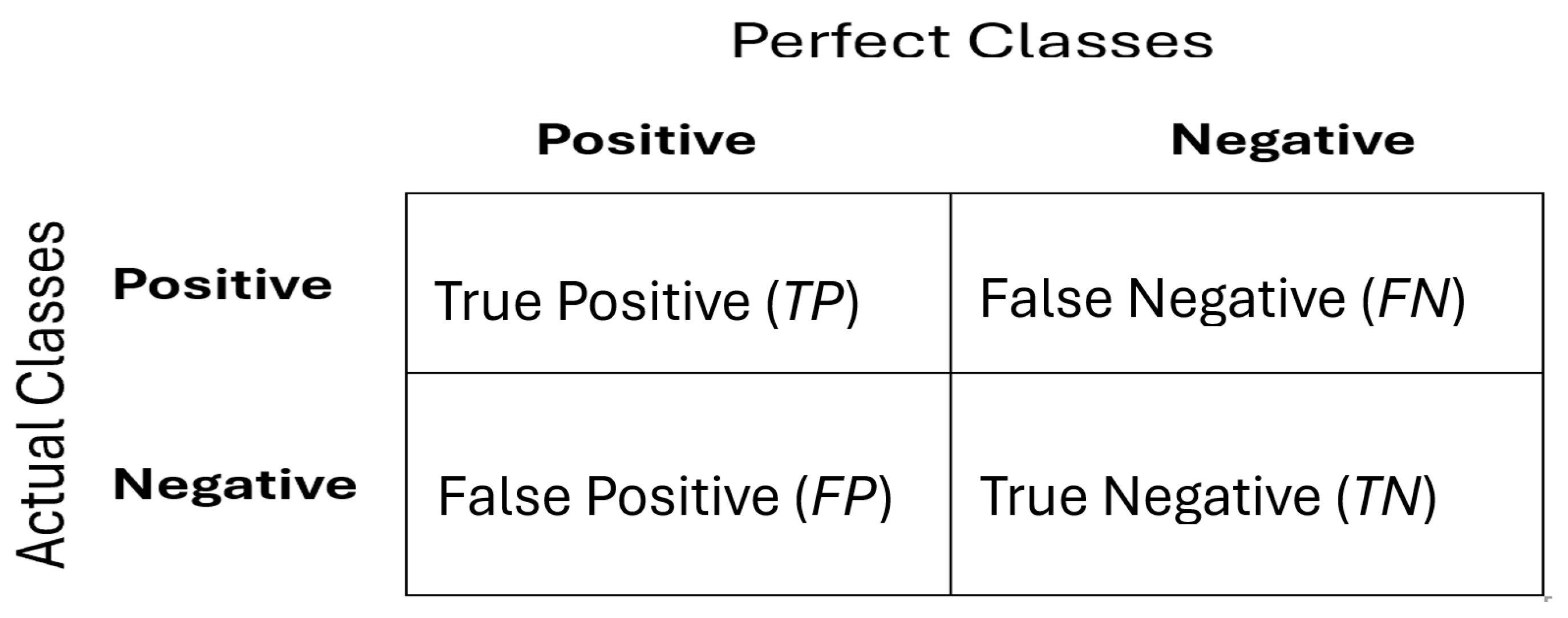
The performance of the eHealth mobile application was primarily evaluated using a confusion matrix, which provided a statistical summary of the model’s classification results, highlighting errors and their categories. This matrix is often referred to as the error matrix.
Figure 9 illustrates the confusion matrix for the abnormal detection (ABD) system, defining its key components:
True Positive (TP): The number of abnormal instances correctly classified as abnormal.
False Positive (FP) (Type I Error): The number of normal instances incorrectly classified as abnormal.
True Negative (TN): The number of normal instances correctly classified as normal.
False Negative (FN) (Type II Error): The number of abnormal instances incorrectly classified as normal.
Accuracy represents the percentage of correct predictions across all samples and is calculated as follows:
The overall performance for both fall and idle detection is summarized in
Table 5.
4.2. Activity Monitoring and Behavioral Trends
The application effectively captured and visualized users’ daily, weekly, and monthly physical activity patterns throughout the two-month study.
Figure 10 illustrates a representative report of weekly and monthly active hours for User 1, demonstrating the system’s capability to track long-term behavioral trends over periods greater than 24 h.
In the “Weekly Active Hours” graph (the top visualization in
Figure 10), each vertical bar represents a day of the week. The numerical value displayed at the top of each bar indicates the total active hours for that specific day. Within each bar, the bright green sections consistently represent periods where movement was detected, signifying that the user was actively using or carrying the phone. The lighter, transparent (or uncolored) sections within the bars indicate periods of detected inactivity. Users can navigate through different weeks’ reports using the “PREV” and “NEXT” buttons.
The “Monthly Active Hours” graph (the bottom visualization in
Figure 10) displays the active hours per day over a period of approximately one month, presented as a line graph. The area shaded in green underneath the line also signifies periods of detected movement, allowing caregivers and users to visualize overarching activity trends and patterns across several weeks or a full month. This comprehensive visual data significantly aids in monitoring activity trends over time, supporting the early detection of significant changes in behavior or health status that might indicate a change in health.
4.3. Inactivity Detection Performance
The system’s ability to identify prolonged periods of user inactivity was a primary focus of its evaluation. Through quantitative analysis of the 138 idle scenarios tested, the system achieved a high classification performance. As detailed in
Table 5, the idle detection demonstrated 104 True Positives, 7 False Positives, 22 True Negatives, and 5 False Negatives, resulting in an overall accuracy of 91.3%.
The integrated fuzzy logic effectively managed alert triggering based on contextual rules. For instance, in accordance with Rule 1 from
Table 3, the system consistently triggered an alert when continuous low activity (inactivity) was detected for four consecutive hours during daytime (07:00–18:00). Conversely, adhering to Rule 5 (
Table 3), no alerts were dispatched for similar four-hour inactivity periods occurring during nighttime (after 22:00), accurately recognizing typical sleep patterns. The system further demonstrated robustness by automatically resetting the inactivity timer if movement resumed within the four-hour threshold, preventing unnecessary alerts. While the system performed well in classifying expected scenarios, false positives did occur, predominantly when participants’ normal behaviors deviated from the predefined fuzzy rules. For instance, in one observed case, a participant who took a longer-than-usual mid-day rest (exceeding the 4 h inactivity threshold during daytime) triggered an alert despite being entirely normal. This highlights the inherent challenge of distinguishing genuine anomalies from individual behavioral variations with static rules.
4.4. Fall Detection Performance
Fall detection, a critical aspect of the system’s functionality, was rigorously tested through 123 simulated emergency scenarios. In these controlled tests, the system demonstrated strong performance. As presented in
Table 5, the fall detection achieved 92 True Positives, 10 False Positives, 15 True Negatives, and 6 False Negatives, resulting in an overall accuracy of 87.7%. In all simulated fall events that were correctly detected (falling under the 92 True Positives), the system successfully triggered an emergency alert within three seconds of a detected high-intensity movement.
Figure 11 provides a visual representation of the system’s daily activity monitoring, including an example of a detected fall. At the top of the interface, essential participant details are displayed, providing immediate context for the activity data. The main “Daily Activity Graph” visualizes the “Activity Level” on the Y-axis against “Time” on the X-axis, presented in a 24 h format (e.g., from 20:00 to 24:00). In this graph, continuous green lines represent periods of normal, sustained activity, while sharp red peaks distinctively indicate sudden, forceful changes in movement characteristic of a detected fall, as seen around 23:40 in the example. These sharp red peaks are direct visual evidence of the high-intensity movements that trigger the fall detection mechanism. The corresponding fuzzy rules—Rule 7 (daytime), Rule 8 (evening), and Rule 9 (nighttime) from
Table 3—were instrumental in ensuring that the system immediately bypassed the four-hour inactivity threshold for these critical events, directly triggering a 3 s monitoring period for fall confirmation and subsequent alerts.
4.5. Alert Notification Efficacy and Robustness
Upon the detection of a confirmed anomaly (either prolonged inactivity or a fall), the system consistently dispatched timely alerts to designated emergency contacts. These notifications were sent via email (using SMTP) to all registered contacts and via SMS to the primary carer’s phone number.
Figure 12 provides a representative example of an email notification triggered by the system upon detecting an abnormality, demonstrating the seamless and automated nature of the alert mechanism.
Furthermore, the system’s robustness was confirmed in various normal usage scenarios. Participants intentionally remained idle for short durations before resuming movement within the set threshold, and the system correctly identified these as non-alert scenarios. This ensured that unnecessary alerts were not triggered during routine, short periods of stillness, thereby enhancing user experience and minimizing false positives. The quantitative results, as detailed in
Section 4.1 and
Table 5, serve as a strong validation of the proposed fuzzy logic methodology and the prototype application’s capability to identify abnormal motion patterns using built-in smartphone accelerometers. These figures, derived from controlled and simulated scenarios with six participants over a two-month period, demonstrate the system’s technical feasibility and real-time detection potential within the scope of this pilot study.
5. Discussions
This section interprets the findings of the eHealth mobile application, considering its implications for remote elderly monitoring. The system represents a significant advancement by leveraging readily available mobile phone sensors and fuzzy logic, offering a continuous and non-invasive health monitoring solution. Unlike often expensive and uncomfortable wearable IoT devices, our system’s reliance on built-in mobile accelerometers provides a cost-effective and highly accessible approach for tracking daily activity. We opted for fuzzy logic over more complex machine learning models due to its proven efficiency and capability for offline data processing, which enables real-time decision-making without constant Internet connectivity.
One key challenge observed during testing was the occurrence of false alerts. As detailed in the Results Section, these arose when individual activity and sleep behaviors deviated from the static, predefined fuzzy logic rules. For instance, a participant taking an unscheduled, longer-than-usual mid-day rest could trigger an alert despite being entirely normal. This highlights the inherent difficulty in distinguishing genuine anomalies from typical individual behavioral variations with fixed rules, pointing towards the need for more adaptable systems.
The pilot study’s results, demonstrating an 87.7% accuracy for fall detection and 91.3% for idle detection, validate the technical feasibility of our fuzzy logic-based methodology. These figures confirm the prototype application’s capability to accurately identify abnormal motion patterns using conventional smartphone accelerometers. The findings highlight the potential of remote patient monitoring (RPM) systems in enhancing elderly care by enabling real-time prolonged inactivity detection and rapid emergency responses, offering a more accessible and scalable alternative to traditional wearable devices.
6. Limitations and Future Directions
A primary limitation of the current study is the small experimental sample size, involving six volunteer participants over a two-month period. This pilot study was primarily designed to validate the feasibility of the fuzzy logic-based methodology and the functional prototype of the eHealth mobile application. While these initial results are promising for confirming the method’s working principle and the app’s operational capabilities, a comprehensive assessment of its long-term efficacy in enhancing health outcomes or ensuring sustained user adaptation necessitates further work.
Despite the advantages of smartphone-based remote monitoring, we acknowledge inherent technical constraints such as battery life, reliance on network connectivity for alerts, and potential sensor performance variability in diverse environments. Our design deliberately minimizes battery drain by utilizing one-minute interval data sampling and performing all core activity detection and fuzzy logic processing locally on the device. This approach reduces continuous power demands and reliance on constant Internet connectivity.
Future research necessitates expanding the cohort significantly by recruiting a larger and more diverse group of elderly participants to enhance the generalizability of findings and gather more extensive long-term data on various activity patterns. Alongside this, comprehensive usability studies with diverse elderly individuals are crucial to further assess the app’s ease of use and refine its interface, complemented by the development of accessible user guides. Future work will also investigate optimized power management techniques and strategies for handling prolonged connectivity outages, such as localized on-device alerts for the user, and explore cloud storage for long-term data retention.
Expanding on the adaptive fuzzy logic, future developments will focus on integrating AI-driven learning to dynamically adjust fuzzy rules based on individual behavioral patterns over a one-week period, thereby significantly reducing false alerts and improving accuracy and personalization. Furthermore, a critical next step involves conducting comprehensive comparative experiments with state-of-the-art deep learning-based activity detection methods, such as convolutional neural networks (CNNs) and long short-term memory (LSTM) networks. This will allow for a robust evaluation of our fuzzy logic approach against these advanced techniques in terms of accuracy, robustness to diverse user behaviors, and computational complexity, especially considering the resource constraints and real-time processing requirements of mobile devices. The integration of more advanced fuzzy logic techniques, such as an adaptive neuro-Fuzzy Inference System, can further improve the tool’s operation. Future enhancements will also include activity trend graphs (daily, weekly, and monthly) to provide caregivers and healthcare professionals with deeper insights into an individual’s activity patterns, supporting personalized and preventive care. Finally, exploring integration with iOS devices and expanded activity detection features will enhance accessibility and effectiveness.
7. Conclusions
This pilot study successfully demonstrated the technical feasibility and preliminary effectiveness of a secure eHealth mobile application for remote elderly monitoring. By utilizing triaxial accelerometers from conventional smartphones, it provides a non-invasive, cost-effective, and user-friendly solution for continuous health tracking. The system, leveraging fuzzy logic, efficiently detected activity patterns and identified prolonged inactivity or potential falls, ensuring timely alerts to caregivers or emergency contacts. The promising results from this initial study, conducted with six participants over two months, validate the core methodology and the functional prototype’s capability to classify activities and trigger alerts, thereby laying a foundational step for future extensive evaluations. This mobile-based approach offers a highly accessible and scalable alternative to traditional wearable IoT devices, potentially reducing healthcare costs and the burden on caregivers while offering enhanced safety, improved healthcare outcomes, and peace of mind for families.
Author Contributions
A.S. managed the overall project and took charge of its administration. R.S. focused on the methodology, design, and implementation, particularly the fuzzy logic aspect, while M.B. contributed to designing the security features of the system. K.A. and R.B. were responsible for coding and implementing the technical components of the project. Y.J. led the literature review, providing critical research to support the work. K.S. gathered user feedback and worked on optimizing the system based on those insights. A.S., R.S., K.S. and M.B. worked together to validate and review the manuscript, and all authors were involved in writing, editing, and finalizing the paper. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by an internal Department Funded Research Project grant from Sheffield Hallam University (internal project reference N160). The Article Processing Charge (APC) was funded by the authors.
Institutional Review Board Statement
Ethical approval for this study was obtained from Sheffield Hallam University and reviewed by the University’s Research Ethics Committee. The ethics application code: ER76195762 was approved on 25 January 2025. All procedures were conducted in accordance with institutional guidelines and regulations.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data is contained within the article.
Acknowledgments
The implementation code, datasets, and additional materials related to this study are available as open-source and can be accessed for replication or further research. All supporting resources will be shared upon request or through a designated public repository.
Conflicts of Interest
Author Karim Shebani was employed by The Rotherham NHS Foundation Trust. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Ahmed, S.; Irfan, S.; Kiran, N.; Masood, N.; Anjum, N.; Ramzan, N. Remote Health Monitoring Systems for Elderly People: A Survey. Sensors 2023, 23, 7095. [Google Scholar] [CrossRef] [PubMed]
- Kok, L.; Berden, C.; Sadiraj, K. Costs and Benefits of Home Care for the Elderly versus Residential Care: A Comparison Using Propensity Scores. Eur. J. Health Econ. 2015, 16, 119–131. [Google Scholar] [CrossRef] [PubMed]
- Philip, N.Y.; Rodrigues, J.J.; Wang, H.; Fong, S.J.; Chen, J. Internet of Things for In-Home Health Monitoring Systems: Current Advances, Challenges and Future Directions. IEEE J. Sel. Areas Commun. 2021, 39, 300–310. [Google Scholar] [CrossRef]
- Taiwo, O.; Ezugwu, A.E. Smart Healthcare Support for Remote Patient Monitoring during COVID-19 Quarantine. Inform. Med. Unlocked 2020, 20, 100428. [Google Scholar] [CrossRef]
- Soni, V.; Yadav, H.; Semwal, V.B.; Roy, B.; Choubey, D.K.; Mallick, D.K. A Novel Smartphone-Based Human Activity Recognition Using Deep Learning in Health Care. In Machine Learning, Image Processing, Network Security and Data Sciences; Springer: Singapore, 2023; pp. 493–503. [Google Scholar] [CrossRef]
- Rocha, M.; Nepomuceno, A.C.; Chi, H.R.; Radwan, A.; André, P.; Alberto, N.; Antunes, P.F.d.C.; Domingues, M.d.F. Indoor Localization Using Fiber Bragg Grating-Based Accelerometers for Smart Healthcare. IEEE Trans. Consum. Electron. 2023, 70, 68–77. [Google Scholar] [CrossRef]
- Ali, A.; Montanaro, T.; Sergi, I.; Carrisi, S.; Galli, D.; Distante, C.; Patrono, L. An Innovative IoT and Edge Intelligence Framework for Monitoring Elderly People Using Anomaly Detection on Data from Non-Wearable Sensors. Sensors 2025, 25, 1735. [Google Scholar] [CrossRef]
- Khan, W.; Ahmad, R.; Rizwan, S.; Abid, Z. IoT-Based Elderly Health Monitoring System Using Firebase Cloud Computing. Wirel. Commun. Mob. Comput. 2025, 8, e70498. [Google Scholar] [CrossRef]
- Muñoz Esquivel, K.; Gillespie, J.; Kelly, D.; Condell, J.; Davies, R.; McHugh, C.; Duffy, W.; Nevala, E.; Alamäki, A.; Jalovaara, J.; et al. Factors Influencing Continued Wearable Device Use in Older Adult Populations: Quantitative Study. JMIR Aging 2023, 6, e36807. [Google Scholar] [CrossRef]
- Peng, Z.; Chen, S.; Lin, J.; Chen, W. A method for real-time detection of vessel abnormal behavior based on CNN-LSTM. Expert Syst. Appl. 2025, 288, 128303. [Google Scholar] [CrossRef]
- Zhao, S.; Zhu, J.; Lu, J.; Song, R.; Ma, S. Lightweight Human Behavior Recognition Method for Visual Communication AGV Based on CNN-LSTM. Int. J. Crowd Sci. 2025, 9, 133–138. [Google Scholar] [CrossRef]
- Al-Otaibi, Z.A.; Mohammad, T.K.; Al-Khalidi, Q.H. Enhancing Healthcare Monitoring: A Deep Learning Approach to Human Activity Recognition using Wearable Sensors. Eng. Technol. Appl. Sci. Res. 2024, 14, 12933–12938. [Google Scholar] [CrossRef]
- Salama, A.; Saatchi, R.; Burke, D. Fuzzy Logic and Regression Approaches for Adaptive Sampling of Multimedia Traffic in Wireless Computer Networks. Technologies 2018, 6, 24. [Google Scholar] [CrossRef]
- Salama, A.; Saatchi, R. Evaluation of Wirelessly Transmitted Video Quality Using a Modular Fuzzy Logic System. Technologies 2019, 7, 67. [Google Scholar] [CrossRef]
- Manani, S.M.; Baretta, M.; Giuliani, A.; Virzì, G.M.; Martino, F.; Crepaldi, C.; Ronco, C. Remote Monitoring in Peritoneal Dialysis: Benefits on Clinical Outcomes and on Quality of Life. J. Nephrol. 2020, 33, 1301–1308. [Google Scholar] [CrossRef]
- Malasinghe, L.P.; Ramzan, N.; Dahal, K. Remote Patient Monitoring: A Comprehensive Study. J. Ambient Intell. Humaniz. Comput. 2019, 10, 57–76. [Google Scholar] [CrossRef]
- Boikanyo, K.; Zungeru, A.M.; Sigweni, B.; Yahya, A.; Lebekwe, C. Remote Patient Monitoring Systems: Applications, Architecture, and Challenges. Sci. Afr. 2023, 20, e01638. [Google Scholar] [CrossRef]
- Chatrati, S.P.; Hossain, G.; Goyal, A.; Bhan, A.; Bhattacharya, S.; Gaurav, D.; Tiwari, S.M. Smart Home Health Monitoring System for Predicting Type 2 Diabetes and Hypertension. J. King Saud Univ. Comput. Inf. Sci. 2022, 34, 862–870. [Google Scholar] [CrossRef]
- Al Bassam, N.; Hussain, S.A.; Al Qaraghuli, A.; Khan, J.; Sumesh, E.P.; Lavanya, V. IoT Based Wearable Device to Monitor the Signs of Quarantined Remote Patients of COVID-19. Inform. Med. Unlocked 2021, 24, 100588. [Google Scholar] [CrossRef]
- Van Lieshout, F.; Yang, R.; Stamenova, V.; Agarwal, P.; Palma, D.C.; Sidhu, A.; Engel, K.; Erwood, A.; Bhatia, R.S.; Bhattacharyya, O.; et al. Evaluating the Implementation of a Remote-Monitoring Program for Chronic Obstructive Pulmonary Disease: Qualitative Methods from a Service Design Perspective. J. Med. Internet Res. 2020, 22, e18148. [Google Scholar] [CrossRef]
- Shaik, T.; Tao, X.; Higgins, N.; Li, L.; Gururajan, R.; Zhou, X.; Acharya, U.R. Remote Patient Monitoring Using Artificial Intelligence: Current State, Applications, and Challenges. WIREs Data Min. Knowl. Discov. 2023, 13, e1485. [Google Scholar] [CrossRef]
- Palanisamy, P.; Padmanabhan, A.; Ramasamy, A.; Subramaniam, S. Remote Patient Activity Monitoring System by Integrating IoT Sensors and Artificial Intelligence Techniques. Sensors 2023, 23, 5869. [Google Scholar] [CrossRef] [PubMed]
- Hung, W.-C.; Shen, F.; Wu, Y.-L.; Hor, M.-K.; Tang, C.-Y. Activity Recognition with Sensors on Mobile Devices. In Proceedings of the 2014 International Conference on Machine Learning and Cybernetics, Lanzhou, China, 13–16 July 2014; pp. 449–454. [Google Scholar] [CrossRef]
- Wang, X.; Kim, H. Detecting User Activities with the Accelerometer on Android Smartphones. J. Multimed. Inf. Syst. 2015, 2, 207. [Google Scholar] [CrossRef]
- Cornacchia, M.; Ozcan, K.; Zheng, Y.; Velipasalar, S. A Survey on Activity Detection and Classification Using Wearable Sensors. IEEE Sens. J. 2017, 17, 386–403. [Google Scholar] [CrossRef]
- George, L.A.; Cross, R.K. Remote Monitoring and Telemedicine in IBD: Are We There Yet? Curr. Gastroenterol. Rep. 2020, 22, 12. [Google Scholar] [CrossRef]
- Bessmeltsev, V.P.; Katasonov, D.N.; Mazurok, B.S.; Makeev, I.V.; Sluev, V.A.; Morozov, V.V.; Shevela, A.I. Mobile System for Automated Remote Monitoring of Cardiac Activity. Biomed. Eng. 2015, 49, 7–11. [Google Scholar] [CrossRef]
- Abolfazli, S.; Sanaei, Z.; Gani, A.; Xia, F.; Yang, L.T. Rich Mobile Applications: Genesis, Taxonomy, and Open Issues. J. Netw. Comput. Appl. 2014, 40, 345–362. [Google Scholar] [CrossRef]
- Kousar, N.; Malik, M.S.; Sarwar, A.; Mohy-ud-din, B.; Shahid, A. Software Engineering: Challenges and Their Solution in Mobile App Development. Int. J. Adv. Comput. Sci. Appl. 2018, 9, 267–272. [Google Scholar] [CrossRef]
- Villena Gonzales, W.; Mobashsher, A.T.; Abbosh, A. The Progress of Glucose Monitoring—A Review of Invasive to Minimally and Non-Invasive Techniques, Devices and Sensors. Sensors 2019, 19, 800. [Google Scholar] [CrossRef]
- Sucerquia, A.; López, J.D.; Vargas-Bonilla, J.F. Real-Life/Real-Time Elderly Fall Detection with a Triaxial Accelerometer. Sensors 2018, 18, 1101. [Google Scholar] [CrossRef]
- Jafleh, E.A.; Alnaqbi, F.A.; Almaeeni, H.A.; Faqeeh, S.; Alzaabi, M.A.; Al Zaman, K. The Role of Wearable Devices in Chronic Disease Monitoring and Patient Care: A Comprehensive Review. Cureus 2024, 16, e68921. [Google Scholar] [CrossRef]
- Mondragón-González, S.L.; Burguière, E.; N’diaye, K. Mobile Devices, Connected Objects, and Sensors. In Machine Learning for Brain Disorders; Elsevier: Amsterdam, The Netherlands, 2023; pp. 355–388. [Google Scholar] [CrossRef]
- Stampfler, T.; Elgendi, M.; Fletcher, R.R.; Menon, C. Fall Detection Using Accelerometer-Based Smartphones: Where Do We Go from Here? Front. Public Health 2022, 10, 996021. [Google Scholar] [CrossRef] [PubMed]
- Toffersson, A.; Lindén, M. A Systematic Review of Wearable Sensors for Monitoring Physical Activity. Sensors 2022, 22, 573. [Google Scholar] [CrossRef] [PubMed]
- Mishra, R. Reducing False Fall Alerts in Fall Detection Using Deep Learning Models. Ph.D. Thesis, University of Missouri, Columbia, MO, USA, 2024. [Google Scholar] [CrossRef]
- Ignatov, A. Real-Time Human Activity Recognition from Accelerometer Data Using Convolutional Neural Networks. Appl. Soft Comput. 2018, 62, 915–922. [Google Scholar] [CrossRef]
- Jordao, A.; Torres, L.A.B.; Schwartz, W.R. Novel Approaches to Human Activity Recognition Based on Accelerometer Data. Signal Image Video Process. 2018, 12, 1387–1394. [Google Scholar] [CrossRef]
- Peckol, J.K. Introduction to Fuzzy Logic; Wiley: Hoboken, NJ, USA, 2021. [Google Scholar]
- Panja, S.; Chattopadhyay, A.K.; Nag, A.; Singh, J.P. Fuzzy-Logic-Based IoMT Framework for COVID-19 Patient Monitoring. Comput. Ind. Eng. 2023, 176, 108941. [Google Scholar] [CrossRef]
- Ullah, F.; Khan, F.; Abdullah; Khan, M.I.; Ashraf, M.U.; Bibi, S.; Nadeem, A. Artificial Intelligence: Current State, Applications, and Challenges. Comput. Intell. Neurosci. 2022, 2022, 8415710. [Google Scholar] [CrossRef]
- Holtz, B.E.; Urban, F.A.; Oesterle, J.; Blake, R.; Henry, A. The Promise of Remote Patient Monitoring. Telemed. E-Health 2024, 30, 31–38. [Google Scholar] [CrossRef]
- Tan, S.Y.; Sumner, J.; Wang, Y.; Yip, A.W. A Systematic Review of the Impacts of Remote Patient Monitoring (RPM) Interventions on Safety, Adherence, Quality-of-Life and Cost-Related Outcomes. NPJ Digit. Med. 2024, 7, 192. [Google Scholar] [CrossRef]
- Zhang, Y.; Liu, H.; Su, X.; Jiang, P.; Wei, D. Remote Mobile Health Monitoring System Based on Smart Phone and Browser/Server Structure. J. Healthc. Eng. 2015, 6, 717–738. [Google Scholar] [CrossRef]
- Chinnaperumal, S.; Periyasamy, M.; AliAlhussan, A.A.; Kannan, S.; Khafaga, D.S.; Raju, S.K.; Eid, M.M.; El-kenawy, E.M. Secure and Intelligent 5G-Enabled Remote Patient Monitoring Using ANN and Choquet Integral Fuzzy VIKOR. Sci. Rep. 2024, 28, 1947–1965. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).