Abstract
The aim of this study was to comprehensively assess the gait parameters in patients who had undergone treatment of pilon fractures by the Ilizarov method. We analyzed gait parameters in patients who had undergone treatment for pilon fractures by the Ilizarov method; 20 patients aged 47.0 years (25.2–78.6) were included in the study. The control group consisted of 32 healthy volunteers. Gait examination was performed using the pedobarographic platform. Statistically significant differences in the following gait parameters: maximum forefoot force (%), step length (cm), and step time (s) were found between the study group and the control group, between the nonoperated leg, and both the operated leg and the dominant limb. Statistically significant differences in the study group between the treated lower limb and the healthy lower limb were only observed in the case of the maximum forefoot force parameter (%). Healthy subjects from the control group obtained significantly higher values during locomotion for stride time, cadence step, and velocity than the patients, with stride time being statistically significantly shorter and the velocity and the cadence step higher. We observed symmetry in the gait parameters after treating pilon fractures by the Ilizarov method. This method of stabilization allows the restoration of gait parameters, with results similar to those obtained after the treatment of other motor organ pathologies described in the literature, although different from those observed in healthy subjects. In particular, the biomechanics of the lower limbs remain disturbed.
1. Introduction
Pilon fractures constitute about 1–6% of all lower limb fractures [1,2,3,4]. They are usually high-energy, comminuted, intra-articular fractures associated with extensive damage to soft tissues, complicating the process of treatment and recovery [3,4,5,6,7,8,9,10,11,12,13,14]. Various methods of stabilizing pilon fractures are available, one of which is the Ilizarov method [3,4,5,6,7,8,9,10,11,12,13,14]. Opinions on the effects of pilon fracture treatment are not unambiguous [3,4,5,6,7,8,9,10,12,13]. Although some authors indicate that it has positive results [3,4,5,8,10,12,13], others report poor results [3,6,7,12,14]. The literature provides publications that present treatment techniques for pilon fractures [3,4,5,6,7,8,9,10,11] and assess their clinical [3,4,5,6,7,8,9,10,11,12,13,14], functional [4,5,6,7,8,9,10,13,14], and radiological [3,4,5,6,8,9,11,12] outcomes. A small number of studies have examined gait parameters, which are very important as a measure of the effectiveness of the treatment method, in patients who have undergone treatment of pilon fractures [13,14], but our search found studies non dealing specifically with the Ilizarov method. Falzarano et al. assessed the gait of 34 patients after pilon fractures with three different stabilization methods [13]. Gait evaluation was limited, it concerned only a few selected parameters by the baropodometric examination [13]. However, they did not compare the results to a healthy control group. In the work of Jansen, the gait of 35 patients with pilon fractures with different stabilization methods was assessed using dynamic pedography [14]. In the evaluated patients, they found limitation of limb functions and the following gait disturbances: lower load on first metatarsal, medial forefoot, heel, and for the total foot in the limb after fracture [14]. However, they did not compare the results to a healthy control group. A comprehensive assessment of the results of lower limb treatment is important for physicians, physiotherapists, and patients [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35]. In addition to clinical and radiological evaluation, assessing the biomechanics of the lower extremities provides objective information on the effects of treating musculoskeletal system pathologies [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35]. There are publications showing the usefulness of the analysis of gait parameters in assessing treatment outcomes for various disorders of the lower extremities [17,18,19,21,22,23,24,25,26,27,28,29,30,31,32] using other types of therapy. Improvements in joint mobility, restoration of normal muscle strength, and reduction in pain and swelling allow normal gait parameters to be restored [17,18,19,21,23,24,25,26,27,30,32]; evaluation of these parameters can serve as measure of the effectiveness of the therapy. Considering the above, the assessment of gait parameters and symmetry in this group of patients seems to be an innovative idea. The aim of this study was to comprehensively assess the gait parameters and symmetry in patients who had undergone treatment of pilon fractures by the Ilizarov method.
2. Materials and Methods
2.1. Patient Recruitment
We analyzed gait parameters in patients who had undergone treatment for pilon fractures by the Ilizarov method. The criteria needed to qualify for the study were consent to participate in the study, treatment of the distal end of the tibia fracture by the Ilizarov method, clinical and radiological confirmation of complete bone union, a minimum follow-up period of two years from the end of treatment, availability of clinical and radiological treatment data, and availability of gait data. The exclusion criteria were: other or multiple injuries of the lower limbs and neurological diseases. Once the exclusion criteria had been applied, twenty patients aged 47.0 years (25.2–78.6) (Table 1) were included in the study. The control group consisted of 32 healthy volunteers with no significant medical history, homogeneously matched in terms of Body Mass Index (BMI), sex, and age (50.5 years (34.0–77.7)) to the study group (Table 1). The study was approved by the Bioethics Committee. All patients were informed that their participation in the study of gait parameters was voluntary.

Table 1.
Descriptive characteristics of the participants.
Treatment of pilon fractures by the Ilizarov method is performed through fracture stabilization, distraction, and reposition. The Ilizarov stabilizers consist of three or four rings attached to the tibia and the fibula with Kirschner’s wires. Gait was begun within one day after surgery with the use of two elbow crutches. Outpatient checks were performed every 2–6 weeks. During treatment, there was a gradual increase in the load on the operated limb, leading to weaning off the crutches and walking with full load, about 2–3 months after the start of treatment. The Ilizarov fixator was removed after the fracture had sufficiently fused, which was radiologically (the presence of at least three of the four cortical layers of bone) and clinically (no pain and no pathological mobility at the fracture site) confirmed. After this, for a period of four weeks, patients were advised to walk with two elbow crutches, and with partial support of the operated limb. The load on the limb was increased gradually, taking into account the degree of the fracture remodeling seen on the X-ray image. All patients had the same rehabilitation protocol throughout the entire period of wearing the stabilizer and for 6–12 weeks after its removal.
2.2. Gait Analysis
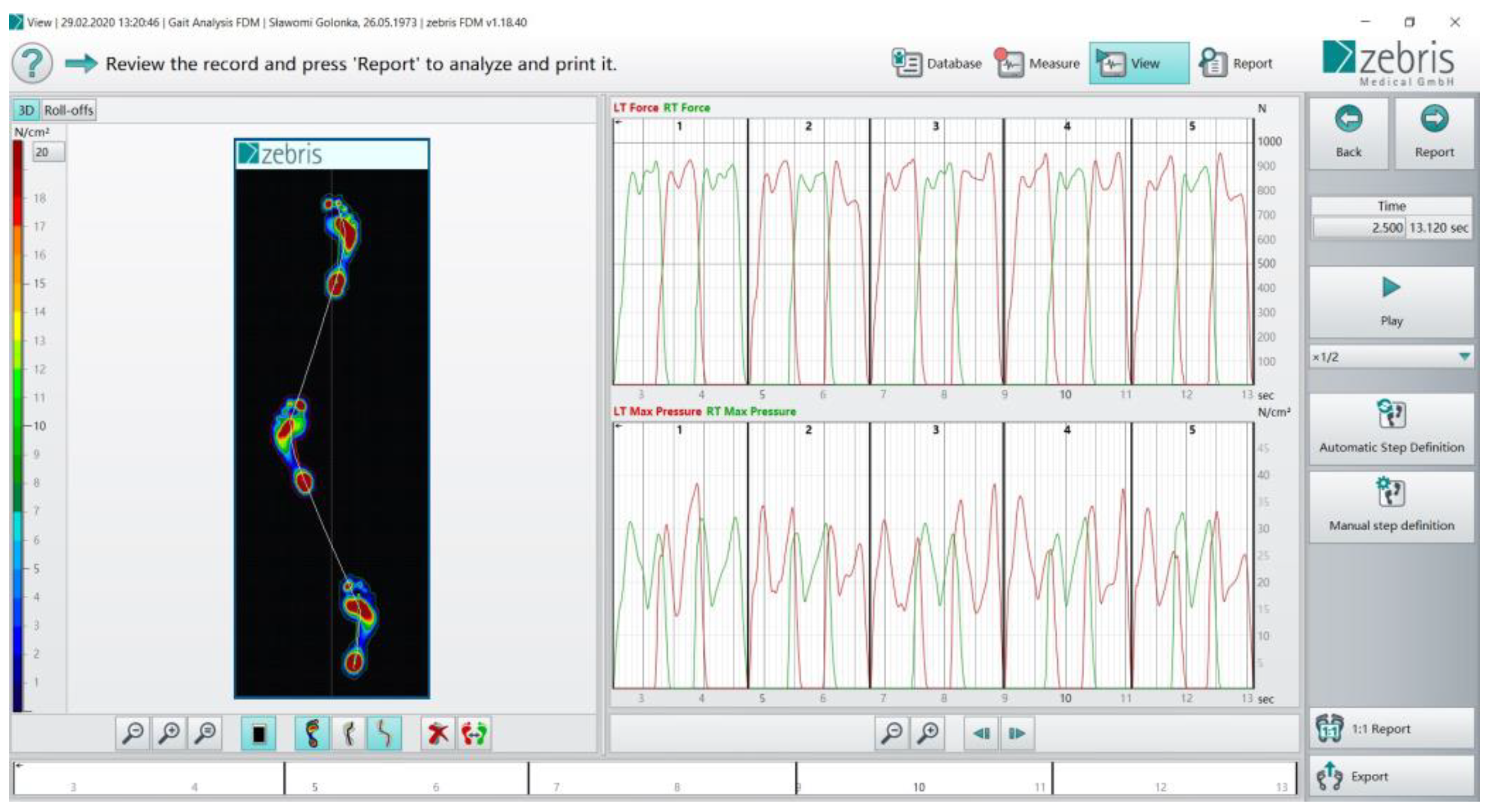
Gait examination was performed using the pedobarographic platform by Zebris Medical, which allowed computer registration of kinetic parameters, which later underwent statistical analysis (Figure 1).
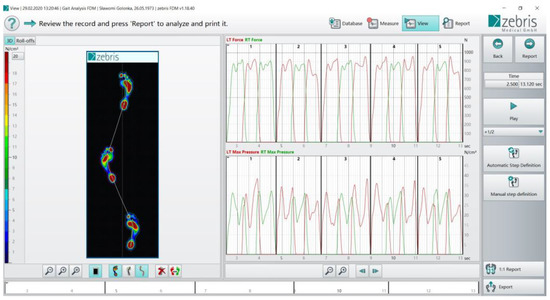
Figure 1.
The pedobarographic platform by Zebris Medical.
The platform, when connected to a computer equipped with the appropriate FootPrint software, enables the analysis of two- and three-dimensional distribution of ground reaction forces while walking. The device has a set of 11,264 sensors, and its size is 56 × 208 cm. Gait analysis data were processed and archived on a PC using the WinFDM software [17,30,33,34,35,36]. The following parameters were analyzed in this study:
- Maximum forefoot force (%) as a percentage of body weight
- Maximum hindfoot force (%) as a percentage of body weight
- Step length (cm)—the distance from the heel print of one foot to the heel print of the next foot during a walking stride
- Stance phase (%)―the period of time during which the foot is in contact with the ground
- Swing phase (%)―the period of time during which the foot is not in contact with the ground
- Step time (s)―the phase of the gait cycle between the contact of one heel with the ground and the contact of the other heel with the ground
- Stride time (s)―the time between the first contact of two consecutive footsteps of the left and the right feet
- Cadence step―step rate per minute
- Velocity (km/h)―the speed of walking.
Before beginning the measurements, the patients walked through the platform to become familiar with the test method. The examinee walked without shoes. The platform was calibrated before each patient. Each patient performed five trials. For further analysis, the arithmetic mean of three good trials was taken into account for each evaluated parameter. The trial was regarded as correct when the patient went through the platform with both feet at least three times, had his or her eyes open during the test, did not perform excessive torso rotations during the test, and walked continuously at his or her preferred speed [17,30,33,34,35,36]. To compare the study group with the control group, the dominant leg in the control group was defined. The parameters of the operated leg in the study group were compared with the nondominant leg in the control group, and the parameters of the healthy leg in the study group were compared with the dominant leg in the control group. The dominant leg mobilizes the function of the lower limb during juggling a ball or kicking [30,33,37].
2.3. Statistical Analysis
The data were analyzed using the SigmaPlot v13 statistics package (Systat Software, San Jose, CA, USA). Continuous variables were first analyzed for a normal distribution using the Kolmogorov–Smirnov test with the Lilliefors correction. All values were expressed as medians and 5th–95th percentiles. An unpaired Student’s t-test was used to test the differences between two groups. For data that did not pass the normality test, the significance of the differences was analyzed using the Mann–Whitney U-test. The level of statistical significance was set at p < 0.05.
3. Results
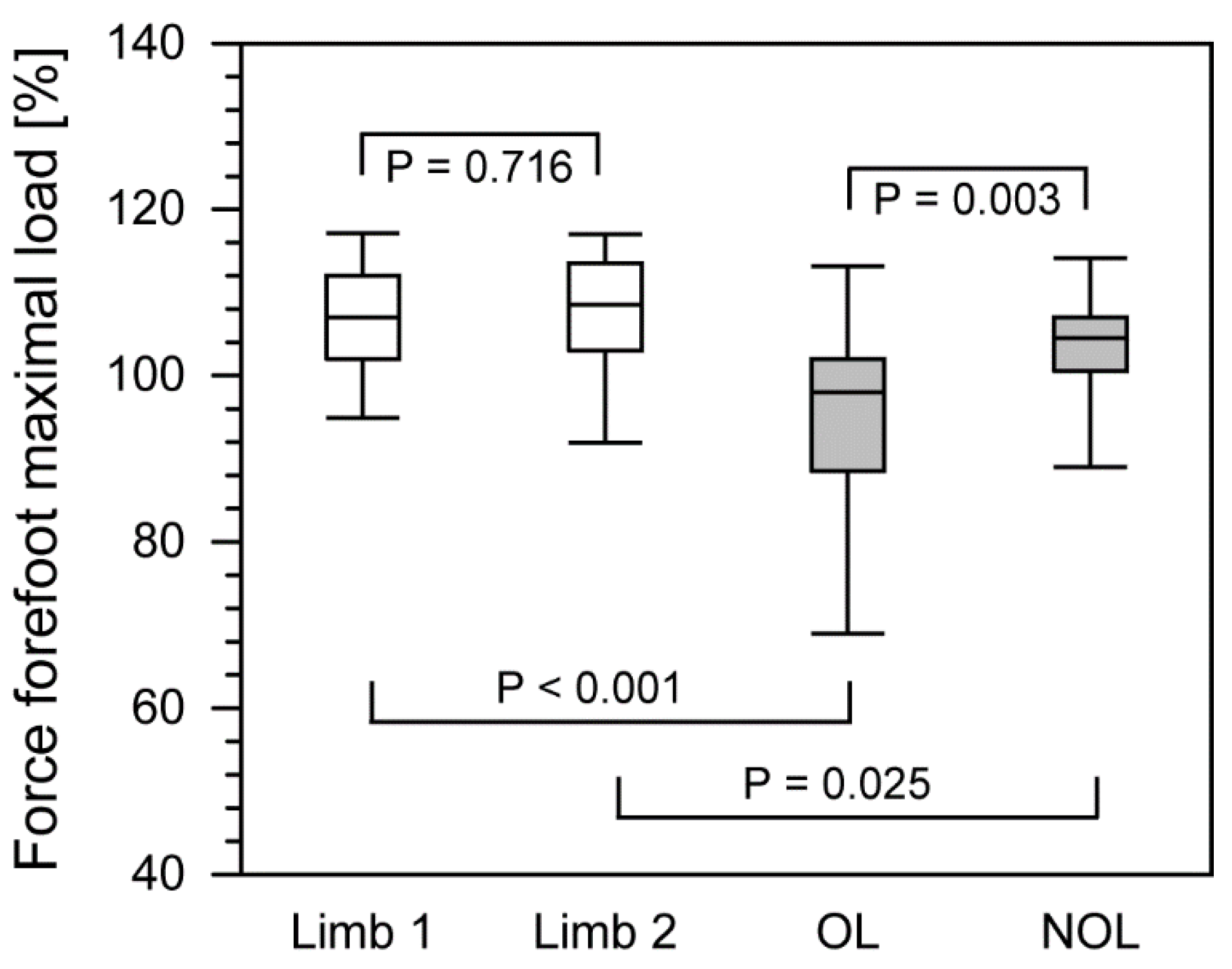
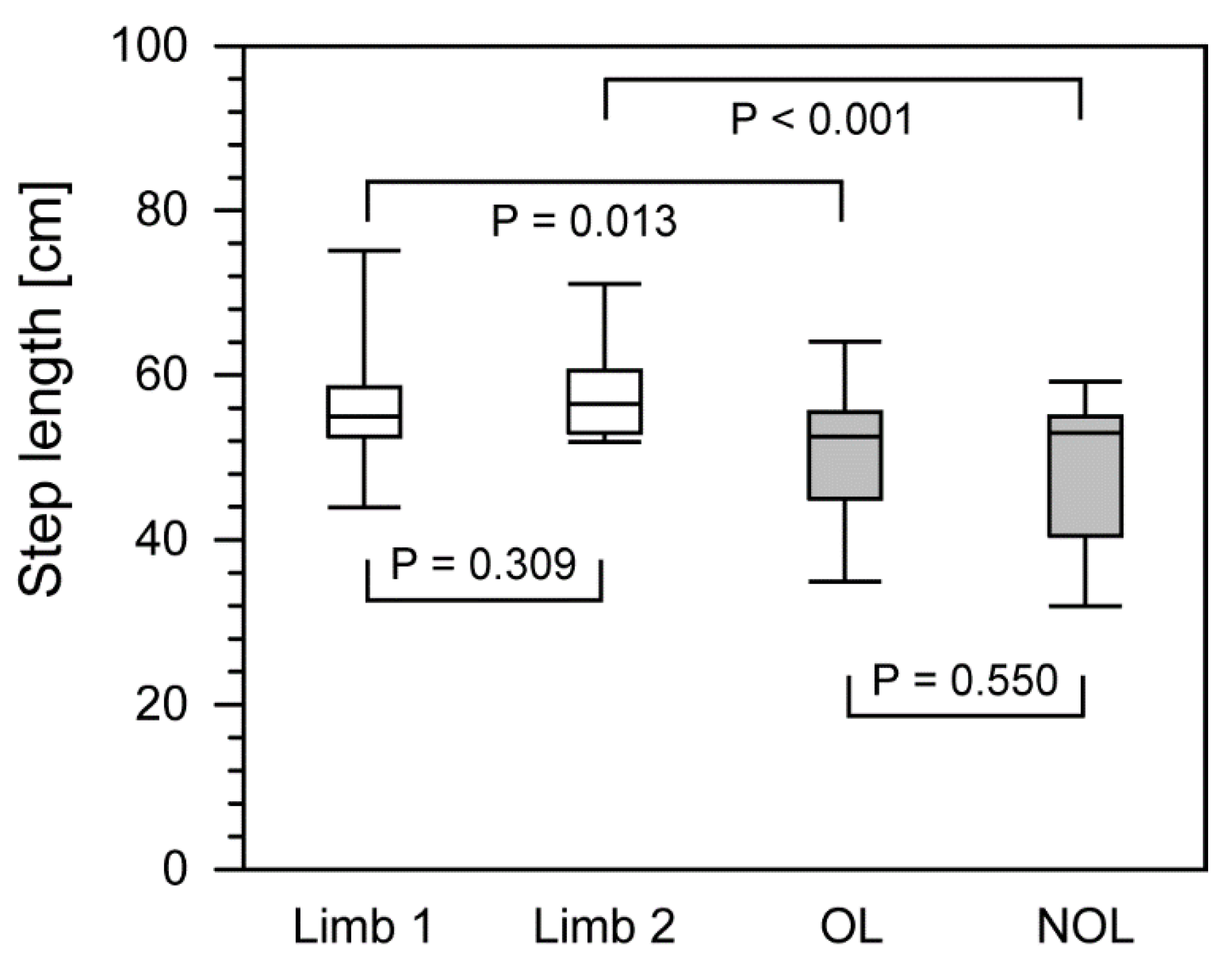
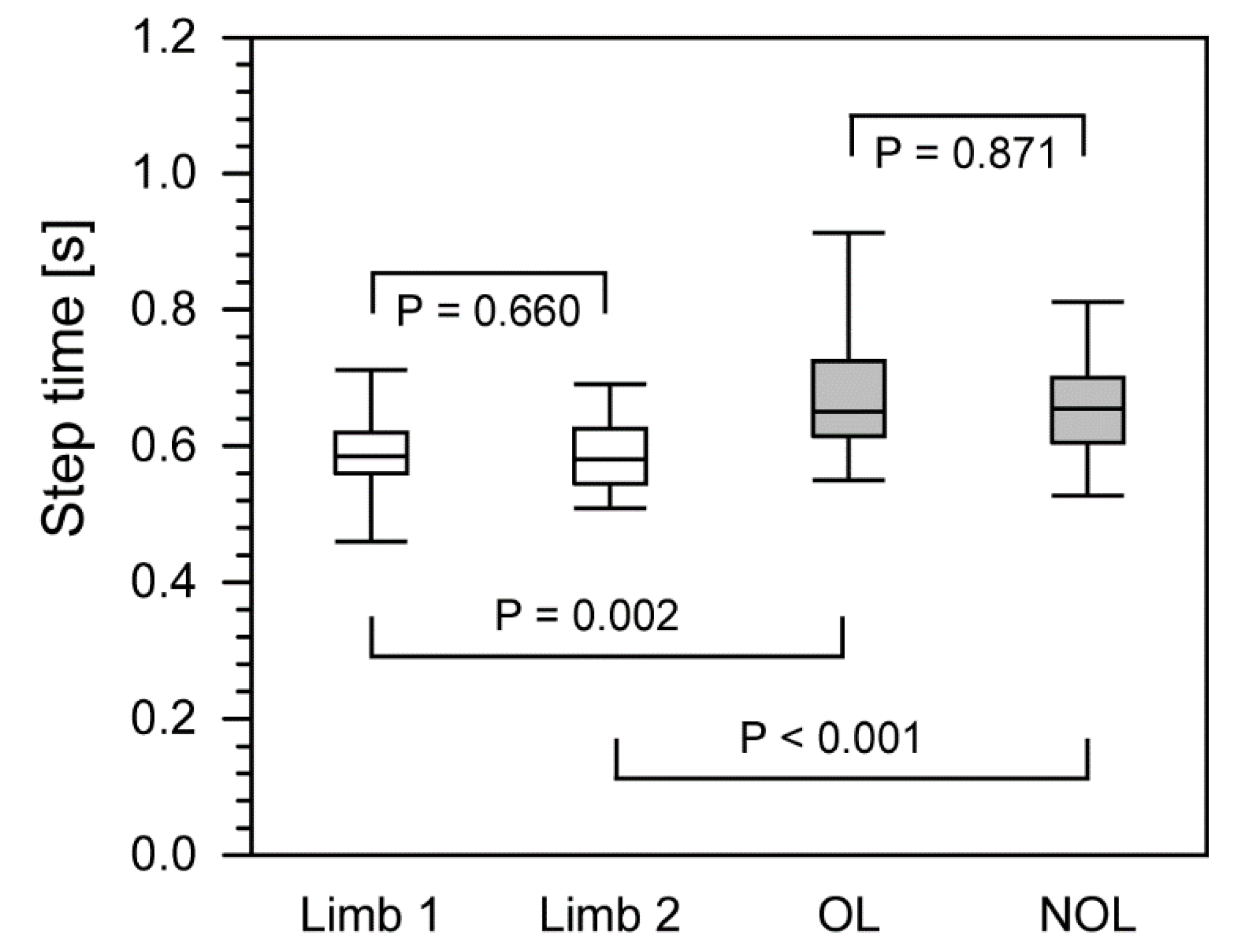
Statistically significant differences in the following gait parameters: maximum forefoot force (%), step length (cm), and step time (s) were found between the study group and the control group, between the nonoperated leg (NOL) and both the operated leg (OL) and the dominant limb (Table 2, Figure 2, Figure 3 and Figure 4).

Table 2.
Gait parameters for patients after treatment with the Ilizarov method vs. healthy control group.
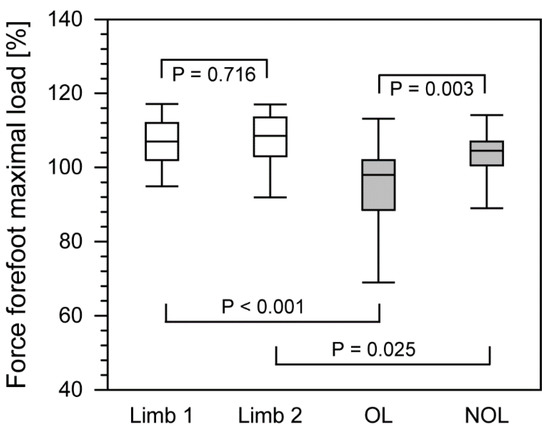
Figure 2.
The comparison of force forefoot maximal load between control group and patients after treatment with the Ilizarov method. The lower boundary of the box indicates the 25th percentile whereas upper boundary of the box corresponds to the 75th percentile. The median is marked by a line located in the box. Whiskers indicate the 90th and 10th percentiles. White boxes, control group; gray boxes, patients after surgery. OL, operated limb; NOL, non-operated limb.
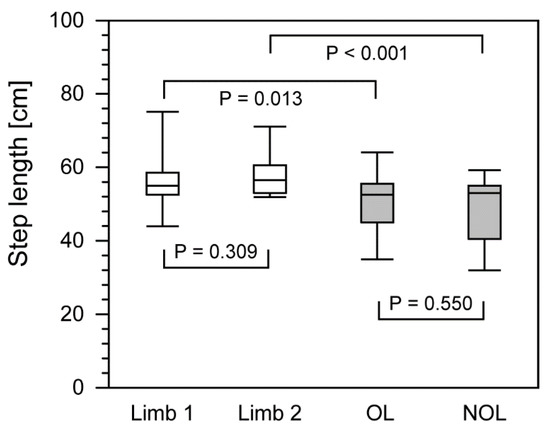
Figure 3.
The comparison of step length between control group and patients after treatment with the Ilizarov method. The lower boundary of the box indicates the 25th percentile whereas upper boundary of the box corresponds to the 75th percentile. The median is marked by a line located in the box. Whiskers indicate the 90th and 10th percentiles. White boxes, control group; gray boxes, patients after surgery. OL, operated limb; NOL, non-operated limb.
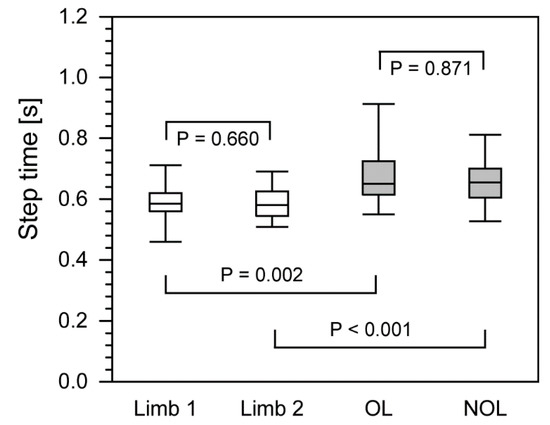
Figure 4.
The comparison of step time between control group and patients after surgery with the Ilizarov method. The lower boundary of the box indicates the 25th percentile whereas upper boundary of the box corresponds to the 75th percentile. The median is marked by a line located in the box. Whiskers indicate the 90th and 10th percentiles. White boxes, control group; gray boxes, patients after surgery. OL, operated limb; NOL, non-operated limb.
Comparison of these parameters in both limbs revealed statistically significantly higher values only for some gait parameters (Table 2, Figure 2, Figure 3 and Figure 4). Statistically significant differences in the study group between the treated lower limb and the healthy lower limb were only observed in the case of the maximum forefoot force parameter [%].
In the case of the study group, the maximum forefoot force [%] of the operated limb was 98.0% (69.5–112.6), while that of the nonoperated limb was 104.5% (89.1–114.0) (Table 2, Figure 2). By comparison, in the group of healthy people, this was 107.0% (95.6–117.0) for the nondominant limb and 108.5% (93.9–117.0) for the dominant limb.
Statistically significant differences were also found between the operated and non-operated limbs in the patients who had undergone treatment of pilon fractures, specifically in the case of the step length parameter (Table 2, Figure 3). In patients treated with the Ilizarov method, the mean distance from the heel print of one foot to the heel print of the next foot of the operated limb was smaller and amounted to 52.5 cm (35.2–63.8 cm) compared to the nonoperated limb 53.0 (32.0–58.9). In the case of healthy subjects, these parameters were 56.5 (52.0–70.3) for the nondominant limb and 55.0 cm (47.2–69.1) for the dominant limb, respectively.
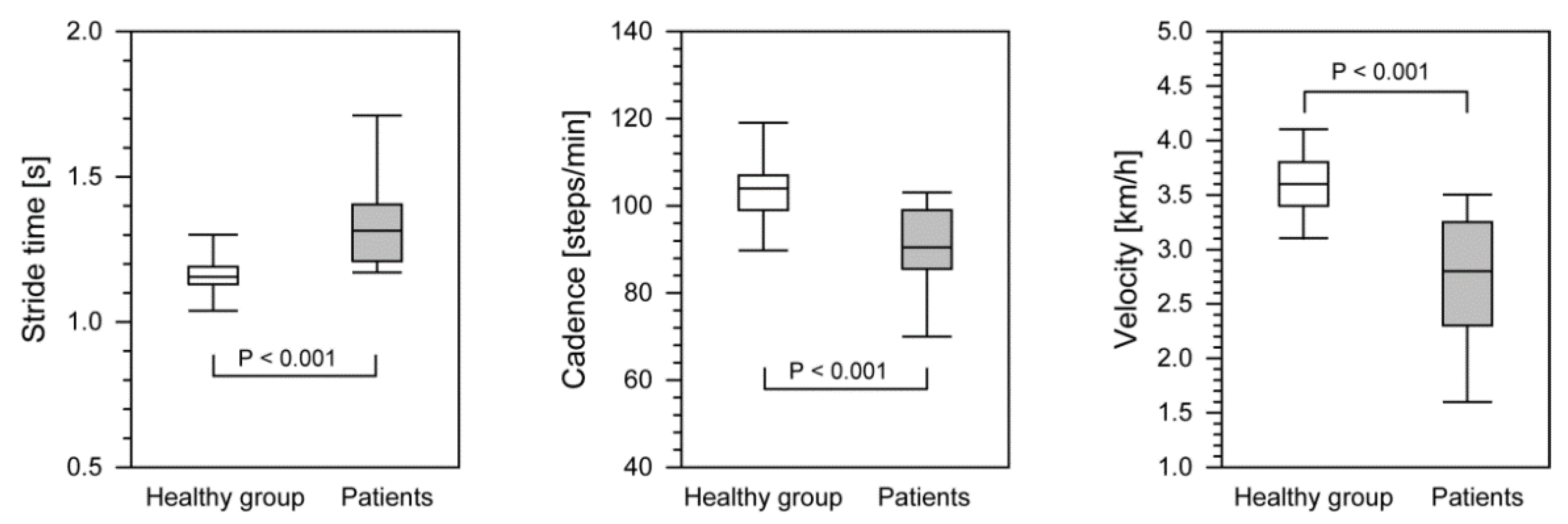
Healthy subjects from the control group obtained significantly higher values during locomotion for stride time, cadence step, and velocity, than the patients (Table 3, Figure 5), with stride time being statistically significantly shorter and the velocity and the cadence step higher (Table 3, Figure 5). All these parameters showed statistically significant differences between the group treated with the Ilizarov method and the control group of healthy people.

Table 3.
Differences of gait parameters between control healthy group and patients after Ilizarov method therapy.
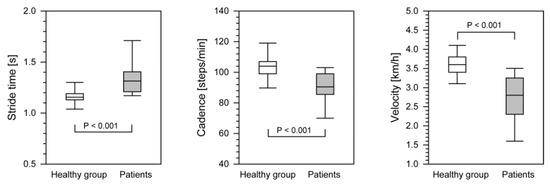
Figure 5.
The differences in gait parameters between control group and patients after treatment with the Ilizarov method. The lower boundary of the box indicates the 25th percentile whereas upper boundary of the box corresponds to the 75th percentile. The median is marked by a line located in the box. Whiskers indicate the 90th and 10th percentiles. White boxes, control group; gray boxes, patients after surgery. OL, operated limb; NOL, non-operated limb.
4. Discussion
Due to their specificity, pilon fractures constitute a significant medical and social problem [3,4,5,6,7,8,9,10,11,12,13,14]. Their treatment is difficult and associated with frequent complications, which make it less effective in some patients [3,4,5,6,7,8,9,10,11,12,13,14]. It has been shown that various methods of stabilization after pilon fractures yield different treatment outcomes [3,4,5,6,7,8,9,10,11,12,13,14]. Some authors suggest that closed reposition and treatment with a plaster cast gives poor results [3,12]. Open reposition and periosteal stabilization, or the use of external stabilizers, is reported to give good treatment results [3,4,5,8,10,12,13]. Nevertheless, some authors have reported poor results after treating pilon fractures with various stabilization methods [3,6,7,12,14].
In this context, a comprehensive evaluation―clinical, radiological, and biomechanical―of the results of treatment for musculoskeletal pathologies is crucial [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35]. No publications to date have comprehensively assessed gait in patients who have undergone treatment for pilon fractures. Several studies have assessed the gait of patients after distraction–corrective osteotomy using the Ilizarov method [17,27,28]. Only a few studies have assessed selected gait parameters in patients who have undergone treatment for pilon fractures [13,14]; however, those patients were not treated with the Ilizarov method and were not compared to healthy controls. Falzarano et al. assessed the gait of 34 patients after pilon fractures with three different stabilization methods [13]. Gait evaluation was limited, it concerned only a few selected parameters by the baropodometric examination [13]. In the work of Jansen, the gait of 35 patients with pilon fractures with different stabilization methods was assessed using dynamic pedography [14]. In the evaluated patients, they found limitation of limb functions and the following gait disturbances: lower load on first metatarsal, medial forefoot, heel, and for the total foot in the limb after fracture [14]. Some studies have used a pedobarographic platform to assess gait parameters in patients with degenerative changes in the hip joints, after calcaneus and ankle fractures [19,22,26,30]. However, the authors of some of these assessed the gait parameters qualitatively, not quantitatively, or else only evaluated selected gait parameters (in some cases, only the force parameters), without providing a comprehensive analysis of all available gait parameters [17,19,22,26,27,28]. It has been shown that the use of a pedobarographic platform for gait analysis allows for a quantitative, repeatable, and objective assessment of the biomechanics of the lower limbs [17,19,20,22,26,30], which was the leitmotiv of our research.
Correct gait parameters indicate an improvement in muscle strength and joint mobility, and a reduction in pain and swelling [17,18,19,21,23,24,25,27,30,32]; their evaluation and comparison to healthy controls can thus be treated as an objective measure of therapy outcome.
Morasiewicz and her team indicated that increased tension in the postural muscles and the higher energy demand related to the shortening and deformation of limbs worsens the parameters of the gait and disturbs its symmetry [17]. The disturbed phase of propulsion may result from the weakening of the gastrocnemius muscle [17]. Aiona et al. reported that shortening of the limbs causes pain and the activation of compensatory mechanisms, which causes higher energy expenditure and disturbs gait parameters [21]. Lee et al. assessed patients after shank osteotomy [23], finding an increase in walking speed and an improvement in gait parameters, which could be associated with a reduction of pain and an increase in muscle strength [23]. Shrader and his team, in turn, noted an improvement in gait parameters after the reduction of pain in patients with gonatrosis [24]. According to Saraph, the factors that contribute to better gait parameters are improved movement in the knee and hip joints and appropriate rehabilitation [25]. Manjra et al. examined eleven patients who had undergone osteotomy with external fixation of the tibia, and found abnormal gait parameters after treatment, mainly due to limited movement of the ankle joint [27]. In his work, Bhave noted an improvement in gait parameters and the normalization of gait symmetry after osteotomy performed using the Ilizarov method [28]. Wu observed deterioration in gait parameters and a reduction in foot mobility after ankle arthrodesis [31]. Karol et al. found abnormal gait parameters in patients who had undergone treatment of congenital pseudarthrosis of the tibia, which resulted from a decrease in the muscular strength of the affected limb and increased energy expenditure during walking [32].
The shortening and deformation of the lower limbs negatively affects gait parameters [17,21,25,28,29]. The patients ha we assessed did not have such dysfunctions or anatomical changes, which confirms the effectiveness of the treatment. Falzarano and Jansen reported abnormal load distribution on the foot and lateral gait axes in patients treated with different techniques due to pilon fractures [13,14].
The walking speed in patients, as assessed by other investigators, ranged from 0.57 m/s to 1.45 m/s [21,23,24,25,29,30]. The walking speed—including cadence—as well as the stance phase, step length, swing phase, step time, and stride time in the patients examined by our team was similar to the values obtained by other authors [24,25,30].
In our group of patients, most of the gait parameters—except for the maximum hindfoot force, stance phase, and swing phase—differed statistically from those found in healthy volunteers in the control group. The lack of proper muscle strength worsens gait parameters [17,23,24,32]. Worse flexor strength affects the propulsion phase [17]. The lack of improvement in joint mobility results in worse gait parameters [17,19,25,27,31]. In particular, limited movement of the ankle joint increases the energy expenditure while walking [17,27]. The ankle joint is damaged in pilon fractures, often leading to movement of this joint being restricted [19,21,23]. Okcu et al. found that the mobility of the ankle joint after stabilization of pilon fractures with the Ilizarov apparatus without foot restraint was better than in patients treated using a monolateral stabilizer, with foot restraint [21]. Pain is also a factor that disturbs gait parameters [19,23,24].
It seems that, in our group of patients who underwent treatment for pilon fractures, the mobility of the joints (especially the ankle joint) and the correct muscle strength were not fully restored, and complete relief from pain was not achieved. The lack of improvement in the gait parameters after treatment may be caused by the rehabilitation being too short or not sufficiently intense [17,25,30]. In treating pilon fractures, it is therefore important to employ a rehabilitation protocol that allows the mobility of the joint (especially of the ankle joint) to improve and reduces pain and swelling.
On the other hand, the gait parameters of the patients in our study were similar to those from literature data [21,23,24,25,29,30]. It was also possible to obtain symmetry between the operated and the healthy limbs in most of the gait parameters assessed. Normal gait is symmetrical [17,28]. This may indicate the restoration of relatively good lower limb biomechanics after treatment of pilon fractures by the Ilizarov method. Our research allowed us to draw several practical implications. Treatment of pilon fractures using the Ilizarov method is effective, because it allows for symmetrical gait parameters to be obtained. Doctors, physiotherapists, and patients should pay attention to intensive rehabilitation after treatment of pilon fractures in order to improve gait parameters. After pilon fractures, as with the treatment of other types of lower leg fractures, it is not possible to obtain fully normal gait parameters.
The shortcomings of our work are the small number of people treated, and the lack of results for pretreatment gait parameters. The small number of patients can be explained the fact that some lived far from the research site and could not reach it, that many patients could not access the pedobarographic platform, that there were a limited number of patients with pilon fractures in our clinic, and that, in some cases, pilon fractures were supplied with internal stabilization and not treated by the Ilizarov method. We decided to include a control group with an appropriate age range. Their greater number was verified by an identical % share of people of the same age, compatible with the group of patients, which was confirmed by the lack of a statistically significant difference with regard to age, but also to anthropometric parameters. Studies of other authors also assessed gait in a similar or smaller number of patients [17,18,27,28,32]. The fact that the gait was not assessed before treatment was due to the fact that they were trauma patients with fractures who were admitted to the ward immediately after the injury. The major strengths of our work are its comprehensive pedobarographic gait analysis, which allows for repeatable and objective measurements, the fact that surgery was performed by two experienced orthopedists, and the uniform postoperative and rehabilitation protocol for patients.
5. Conclusions
We observed symmetry in the gait parameters after treating pilon fractures by the Ilizarov method. This method of stabilization allows the restoration of gait parameters, with results similar to those obtained after the treatment of other motor organ pathologies described in the literature, although different from those observed in healthy subjects. In particular the biomechanics of the lower limbs remains disturbed. Following treatment, intense and long-term rehabilitation is recommended in order to restore normal ankle mobility.
Author Contributions
Conceptualization, Ł.P., P.W., and P.M.; methodology, Ł.P., P.W., and A.P.K., M.P. and P.M.; software, Ł.P., F.F.-L., M.P., and P.M.; validation, Ł.P., P.M., A.L., S.Ż., R.G., W.U., F.F.-L. and P.M.; formal analysis, Ł.P., P.W., A.P.K., A.L., S.Ż., R.G., W.U., P.M., F.F.-L., and P.M.; investigation, Ł.P., P.M., A.P.K., A.L., S.Ż., R.G., W.U., P.M., F.F.-L., and P.M.; resources, Ł.P., P.M., A.P.K., A.L., S.Ż., R.G., W.U., P.M., F.F.-L., and P.M.; data curation: Ł.P., P.W., M.P., F.F.-L., and P.M.; writing—original draft preparation, Ł.P., P.W., M.P., F.F.-L., and P.M.; writing—review and editing, Ł.P., P.W., M.P., F.F.-L., and P.M.; visualization, Ł.P., P.W., M.P., F.F.-L., and P.M.; supervision, Ł.P. and P.M.; project administration, Ł.P. and P.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of University School of Physical Education in Wroclaw (protocol code 5/2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kelsey, J.L.; Samelson, E.J. Variation in Risk Factors for Fractures at Different Sites. Curr. Osteoporos. Rep. 2009, 27–133. [Google Scholar] [CrossRef] [PubMed]
- Holloway, K.L.; Yousif, D.; Bucki-Smith, G.; Hosking, S.; Betson, A.G.; Williams, L.J.; Brennan-Olsen, S.L.; Kotowicz, M.A.; Sepetavc, A.; Pasco, J.A. Lower Limb Fracture Presentations at a Regional Hospital. Arch. Osteoporos. 2017, 12. [Google Scholar] [CrossRef] [PubMed]
- Papadokostakis, G.; Kontakis, G.; Giannoudis, P.; Hadjipavlou, A. External Fixation Devices in the Treatment of Fractures of the Tibial Plafond: A Systematic Review of the Literature. J. Bone Jt. Surg.-Ser. B 2008, 90, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Villaseñor, L.E.; Olea Leyva, M.A.; Rodríguez Flores, R.; Hernández López, J.L. Clinical Outcome of a Bilateral Tibial Pylon Fracture Treated with a Minimally Invasive Technique. Acta Ortopédica Mex. 2009, 23, 163–166. [Google Scholar]
- Okcu, G.; Aktuglu, K. Intra-Articular Fractures of the Tibial Plafond. A Comparison of the Results Using Articulated and Ring External Fixators. J. Bone Jt. Surg.-Ser. B 2004, 868–875. [Google Scholar] [CrossRef] [PubMed]
- García-Balderas, A.; Beltrán-Cota, E.R.; Ruiz-Barrios, J.M.; Caldera-Barbosa, O. Results of the treatment of high energy tibial pylon fractures. Acta Ortopédica Mex. 2013, 27, 363–366. [Google Scholar]
- Závitkovský, P.; Malkus, T. Fractures of the Tibial Pylon: Treatment Options and Outcomes. Acta Chir. Orthop. Traumatol. Cech. 2004, 71, 228–22836. [Google Scholar]
- Aktuǧlu, K.; Özsoy, M.H.; Yensel, U. Treatment of Displaced Pylon Fractures with Circular External Fixators of Ilizarov. Foot Ankle Int. 1998, 19, 208–216. [Google Scholar] [CrossRef]
- Bastian, L.; Blauth, M.; Thermann, H.; Tscherne, H. Verschiedene Therapiekonzepte Bei Schweren Frakturen Des Pilon Tibiale (Typ-C-Verletzungen). Unfallchirurg 1995, 98, 551–558. [Google Scholar]
- Zheng, Y.; Zhang, J.D.; Shen, J.M.; Chen, J.J.; Toy, L.; Huang, J.F. A Modified 2-Stage Treatment for AO/OTA 43-C1 Pilon Fractures Accompanied by Distal Fibular and Posterior Lip of the Distal Tibia Fracture. J. Foot Ankle Surg. 2020, 59, 972–978. [Google Scholar] [CrossRef]
- Campbell, S.T.; Goodnough, L.H.; Salazar, B.; Lucas, J.F.; Bishop, J.A.; Gardner, M.J. How Do Pilon Fractures Heal? An Analysis of Dual Plating and Bridging Callus Formation. Injury 2020, 51, 1655–1661. [Google Scholar] [CrossRef]
- Malik-Tabassum, K.; Pillai, K.; Hussain, Y.; Bleibleh, S.; Babu, S.; Giannoudis, P.V.; Tosounidis, T.H. Post-Operative Outcomes of Open Reduction and Internal Fixation versus Circular External Fixation in Treatment of Tibial Plafond Fractures: A Systematic Review and Meta-Analysis. Injury 2020, 1448–1456. [Google Scholar] [CrossRef]
- Falzarano, G.; Pica, G.; Medici, A.; Rollo, G.; Bisaccia, M.; Cioffi, R.; Pavone, M.; Meccariello, L. Foot Loading and Gait Analysis Evaluation of Nonarticular Tibial Pilon Fracture: A Comparison of Three Surgical Techniques. J. Foot Ankle Surg. 2018, 57, 894–898. [Google Scholar] [CrossRef]
- Jansen, H.; Fenwick, A.; Doht, S.; Frey, S.; Meffert, R. Clinical Outcome and Changes in Gait Pattern after Pilon Fractures. Int. Orthop. 2013, 37, 51–58. [Google Scholar] [CrossRef]
- Czamara, A.; Markowska, I.; Królikowska, A.; Szopa, A.; Domagalska Szopa, M. Kinematics of Rotation in Joints of the Lower Limbs and Pelvis during Gait: Early Results—SB ACLR Approach versus DB ACLR Approach. Biomed. Res. Int. 2015, 2015. [Google Scholar] [CrossRef]
- Królikowska, A.; Sikorski, Ł.; Czamara, A.; Reichert, P. Effects of Postoperative Physiotherapy Supervision Duration on Clinical Outcome, Speed, and Agility in Males 8 Months after Anterior Cruciate Ligament Reconstruction. Med. Sci. Monit. 2018, 24, 6823–6831. [Google Scholar] [CrossRef] [PubMed]
- Morasiewicz, M.; Koprowski, P.; Wrzosek, Z.; Dragan, S. Gait analysis in patients after lengthening and correction of tibia with Ilizarov technique. Fizjoterapia 2010, 18, 9–18. [Google Scholar] [CrossRef]
- Butler, R.J.; Barrios, J.A.; Royer, T.; Davis, I.S. Frontal-Plane Gait Mechanics in People with Medial Knee Osteoarthritis Are Different from Those in People with Lateral Knee Osteoarthritis. Phys. Ther. 2011, 91, 1235–1243. [Google Scholar] [CrossRef] [PubMed]
- Cichy, B.; Wilk, M. Gait Analysis in Osteoarthritis of the Hip. Med. Sci. Monit. 2006, 12, 507–513. [Google Scholar]
- Klöpfer-Krämer, I.; Brand, A.; Wackerle, H.; Müßig, J.; Kröger, I.; Augat, P. Gait Analysis—Available Platforms for Outcome Assessment. Injury 2020, 51, S90–S96. [Google Scholar] [CrossRef] [PubMed]
- Aiona, M.; Do, K.P.; Emara, K.; Dorociak, R.; Pierce, R. Gait Patterns in Children with Limb Length Discrepancy. J. Pediatric Orthop. 2015, 35, 280–284. [Google Scholar] [CrossRef] [PubMed]
- Fenwick, A.; Kröger, N.; Jovic, S.; Hölscher-Doht, S.; Meffert, R.; Jansen, H. Pedobarography Shows No Differences in Gait after Talar Fractures. Technol. Health Care 2020, 28, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Lee, O.S.; Teo, S.H.; Lee, Y.S. Change in Gait after High Tibial Osteotomy: A Systematic Review and Meta-Analysis. Gait Posture 2017, 57, 57–68. [Google Scholar] [CrossRef]
- Shrader, M.W.; Draganich, L.F.; Pottenger, L.A.; Piotrowski, G.A. Effects of Knee Pain Relief in Osteoarthritis on Gait and Stair-Stepping. Clin. Orthop. Relat. Res. 2004, 421, 188–193. [Google Scholar] [CrossRef]
- Saraph, V.; Zwick, E.B.; Steinwender, G.; Auner, C.; Schneider, F.; Linhart, W. Leg Lengthening as Part of Gait Improvement Surgery in Cerebral Palsy: An Evaluation Using Gait Analysis. Gait Posture 2006, 23, 83–90. [Google Scholar] [CrossRef]
- Genc, Y.; Gultekin, A.; Duymus, T.M.; Mutlu, S.; Mutlu, H.; Komur, B. Pedobarography in the Assessment of Postoperative Calcaneal Fracture Pressure with Gait. J. Foot Ankle Surg. 2016, 55, 99–105. [Google Scholar] [CrossRef]
- Manjra, M.A.; Naude, J.; Birkholtz, F.; Glatt, V.; Tetsworth, K.; Hohmann, E. The Relationship between Gait and Functional Outcomes in Patients Treated with Circular External Fixation for Malunited Tibial Fractures. Gait Posture 2019, 68, 569–574. [Google Scholar] [CrossRef]
- Bhave, A.; Paley, D.; Herzenberg, J.E. Improvement in Gait Parameters after Lengthening for the Treatment of Limb-Length Discrepancy. J. Bone Jt. Surg.-Ser. A 1999, 81, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Song, K.M.; Halliday, S.E.; Little, D.G. The Effect of Limb-Length Discrepancy on Gait. J. Bone Jt. Surg.-Ser. A 1997, 79, 1690–1698. [Google Scholar] [CrossRef] [PubMed]
- Suciu, O.; Onofrei, R.R.; Totorean, A.D.; Suciu, S.C.; Amaricai, E.C. Gait Analysis and Functional Outcomes after Twelve-Week Rehabilitation in Patients with Surgically Treated Ankle Fractures. Gait Posture 2016, 49, 184–189. [Google Scholar] [CrossRef]
- Wu, W.L.; Su, F.C.; Cheng, Y.M.; Huang, P.J.; Chou, Y.L.; Chou, C.K. Gait Analysis after Ankle Arthrodesis. Gait Posture 2000, 11, 54–61. [Google Scholar] [CrossRef]
- Karol, L.A.; Haideri, N.F.; Halliday, S.E.; Smitherman, T.B.; Johnston, C.E. Gait Analysis and Muscle Strength in Children with Congenital Pseudarthrosis of the Tibia: The Effect of Treatment. J. Pediatric Orthop. 1998, 18, 381–386. [Google Scholar] [CrossRef]
- Morasiewicz, P.; Dragan, S.; Dragan, S.Ł.; Wrzosek, Z.; Pawik, Ł. Pedobarographic Analysis of Body Weight Distribution on the Lower Limbs and Balance after Ilizarov Corticotomies. Clin. Biomech. 2016, 31, 2–6. [Google Scholar] [CrossRef]
- Morasiewicz, P.; Konieczny, G.; Dejnek, M.; Morasiewicz, L.; Urbański, W.; Kulej, M.; Dragan, S.Ł.; Dragan, S.F.; Pawik, Ł. Pedobarographic Analysis of Body Weight Distribution on the Lower Limbs and Balance after Ankle Arthrodesis with Ilizarov Fixation and Internal Fixation. Biomed. Eng. Online 2018, 17, 174. [Google Scholar] [CrossRef]
- Morasiewicz, P.; Konieczny, G.; Dejnek, M.; Urbański, W.; Dragan, S.Ł.; Kulej, M.; Dragan, S.F.; Pawik, Ł. Assessment of the Distribution of Load on the Lower Limbs and Balance before and after Ankle Arthrodesis with the Ilizarov Method. Sci. Rep. 2018, 8, 15693. [Google Scholar] [CrossRef]
- Lorkowski, J.; Trybus, M.; Hładki, W.; Brongel, L. Underfoot Pressure Distribution of a Patient with Unilateral Ankylosis of Talonavicular Joint during Rheumatoid Arthritis—Case Report. Przegla̧d Lek. 2008, 65, 54–56. [Google Scholar]
- Coren, S. The Lateral Preference Inventory for Measurement of Handedness, Footedness, Eyedness, and Earedness: Norms for Young Adults. Bull. Psychon. Soc. 1993, 31, 1–3. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).