Circulating Neutrophils Do Not Predict Subclinical Coronary Artery Disease in Women with Former Preeclampsia
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Coronary Artery Calcium (CAC) and Plaque Measurement
2.3. Blood Collection, Stimulation of Neutrophils and Red Blood Cell Lysis
2.4. Flow Cytometry
2.5. Statistical Analyses
3. Results
3.1. Baseline Characteristics
3.2. Total Neutrophil Numbers in Subclinical CAD
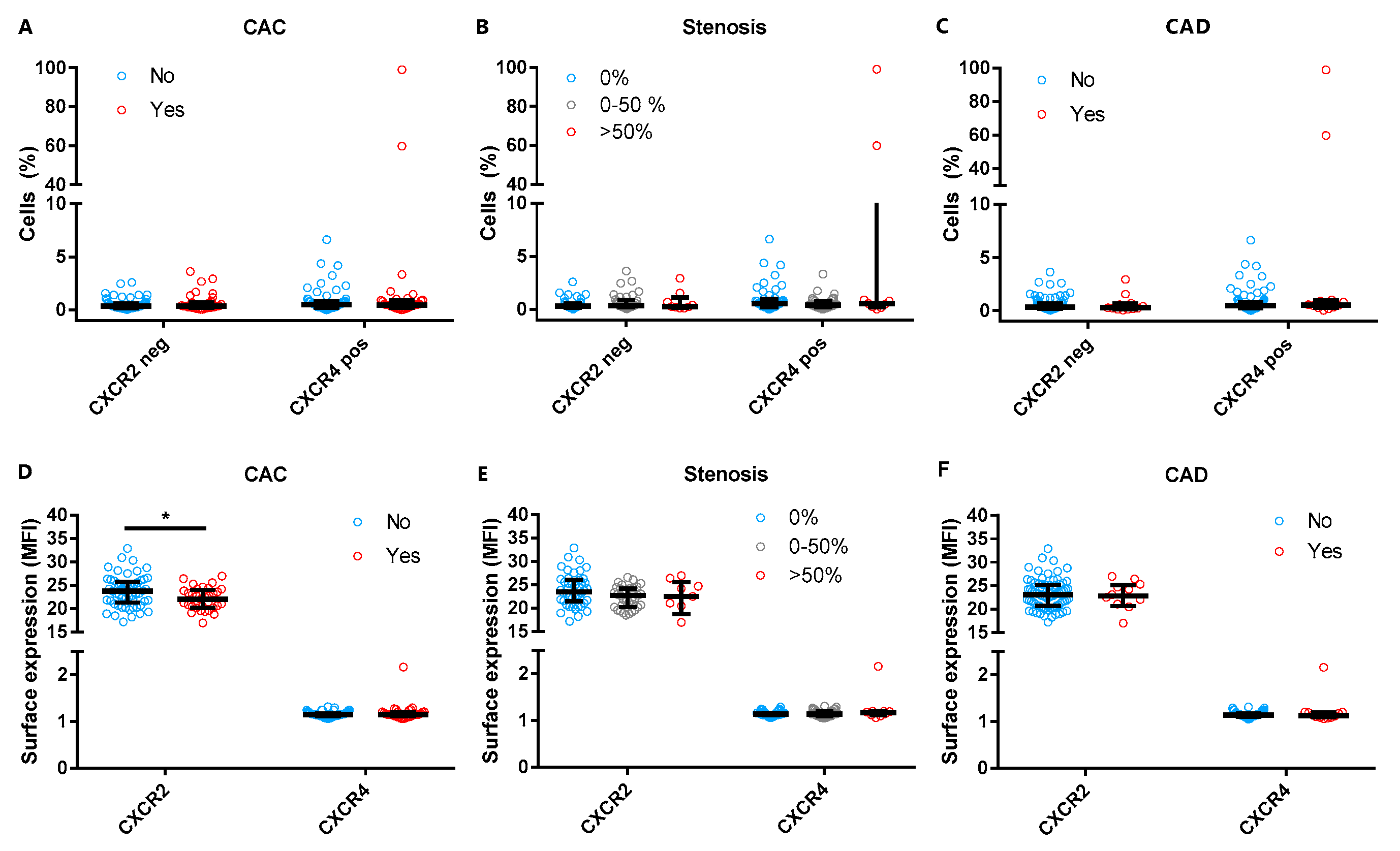
3.3. Neutrophil Chemokine Receptor Expression and Subclinical CAD
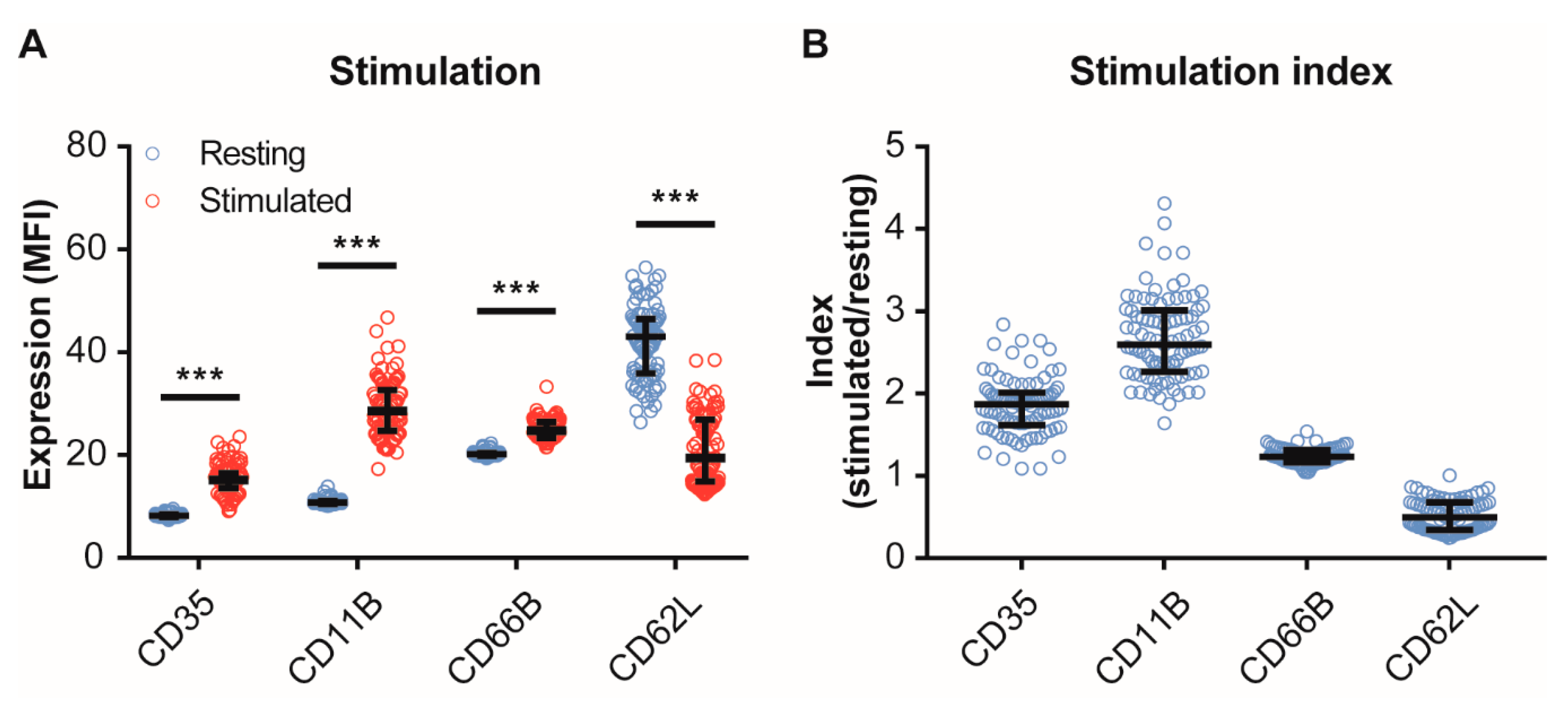
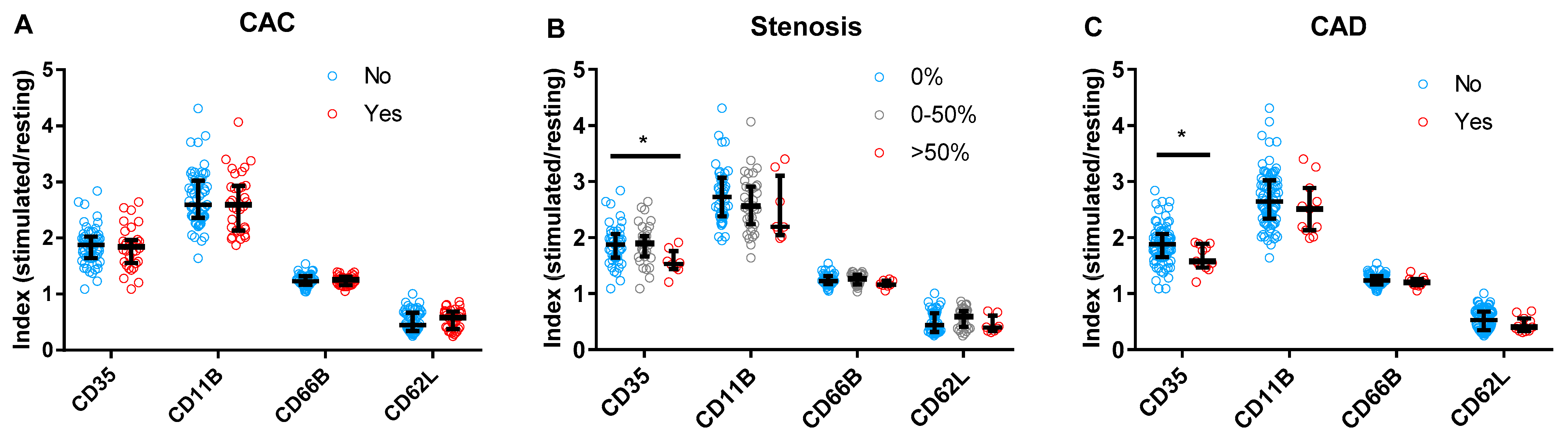
3.4. Neutrophil Activity and Subclinical CAD
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Mendis, S.; Armstrong, T.; Bettcher, D.; Branca, F.; Lauer, J.; Mace, C.; Poznyak, V.; Riley, L.; Da Costa E Silva, V.; Stevens, G. Global Status Report on Noncommunicable Diseases 2014; World Health Organisation: Geneva, Switzerland, 2014. [Google Scholar]
- Say, L.; Chou, D.; Gemmill, A.; Tunçalp, Ö.; Moller, A.B.; Daniels, J.; Gülmezoglu, A.M.; Temmerman, M.; Alkema, L. Global causes of maternal death: A WHO systematic analysis. Lancet Glob. Heal. 2014, 2, e323–e333. [Google Scholar] [CrossRef]
- Mol, B.W.J.; Roberts, C.T.; Thangaratinam, S.; Magee, L.A.; De Groot, C.J.M.; Hofmeyr, G.J. Pre-eclampsia. Lancet 2016, 387, 999–1011. [Google Scholar] [CrossRef]
- Haukkamaa, L.; Salminen, M.; Laivuori, H.; Leinonen, H.; Hiilesmaa, V.; Kaaja, R. Risk for subsequent coronary artery disease after preeclampsia. Am. J. Cardiol. 2004, 93, 805–808. [Google Scholar] [CrossRef] [PubMed]
- Ray, J.G.; Vermeulen, M.J.; Schull, M.J.; Redelmeier, D.A. Cardiovascular health after maternal placental syndromes (CHAMPS): Population-based retrospective cohort study. Lancet 2005, 366, 1797–1803. [Google Scholar] [CrossRef]
- Riise, H.K.R.; Sulo, G.; Tell, G.S.; Igland, J.; Nygård, O.; Vollset, S.E.; Iversen, A.; Austgulen, R.; Daltveit, A.K. Incident Coronary Heart Disease After Preeclampsia: Role of Reduced Fetal Growth, Preterm Delivery, and Parity. J. Am. Heart Assoc. 2017, 6, e004158. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.; Haththotuwa, R.; Kwok, C.S.; Babu, A.; Kotronias, R.A.; Rushton, C.; Zaman, A.; Fryer, A.A.; Kadam, U.; Chew-Graham, C.A.; et al. Preeclampsia and Future Cardiovascular Health. Circ. Cardiovasc. Qual. Outcomes 2017, 10, e003497. [Google Scholar] [CrossRef]
- Mosca, L.; Benjamin, E.J.; Berra, K.; Bezanson, J.L.; Dolor, R.J.; Lloyd-Jones, D.M.; Newby, L.K.; Piña, I.L.; Roger, V.L.; Shaw, L.J.; et al. Effectiveness-Based Guidelines for the Prevention of Cardiovascular Disease in Women—2011 Update. Circulation 2011, 123, 1243–1262. [Google Scholar] [CrossRef]
- Bushnell, C.; McCullough, L.D.; Awad, I.A.; Chireau, M.V.; Fedder, W.N.; Furie, K.L.; Howard, V.J.; Lichtman, J.H.; Lisabeth, L.D.; Piña, I.L.; et al. Guidelines for the Prevention of Stroke in Women. Stroke 2014, 45, 1545–1588. [Google Scholar] [CrossRef]
- Heida, K.Y.; Bots, M.L.; de Groot, C.J.; van Dunné, F.M.; Hammoud, N.M.; Hoek, A.; Laven, J.S.; Maas, A.H.; Roeters van Lennep, J.E.; Velthuis, B.K.; et al. Cardiovascular risk management after reproductive and pregnancy-related disorders: A Dutch multidisciplinary evidence-based guideline. Eur. J. Prev. Cardiol. 2016, 23, 1863–1879. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef]
- De Jager, S.C.A.S.C.A.; Meeuwsen, J.A.L.J.A.L.; van Pijpen, F.M.F.M.; Zoet, G.A.G.A.; Barendrecht, A.D.A.D.; Franx, A.; Pasterkamp, G.; van Rijn, B.B.B.B.; Goumans, M.-J.M.-J.; den Ruijter, H.M.H.M. Preeclampsia and coronary plaque erosion: Manifestations of endothelial dysfunction resulting in cardiovascular events in women. Eur. J. Pharmacol. 2017, 816, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Laresgoiti-Servitje, E. A leading role for the immune system in the pathophysiology of preeclampsia. J. Leukoc. Biol. 2013, 94, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Wang, Z.; Lin, M. The role of neutrophil activation in pathogenesis of preeclampsia. J. Tongji Med. Univ. 2000, 20, 246. [Google Scholar] [PubMed]
- Crocker, I.P.; Wellings, R.P.; Fletcher, J.; Baker, P.N. Neutrophil function in women with pre-eclampsia. BJOG 1999, 106, 822–828. [Google Scholar] [CrossRef]
- Tsukimori, K.; Nakano, H.; Wake, N. Difference in neutrophil superoxide generation during pregnancy between preeclampsia and essential hypertension. Hypertension 2007, 9, 1436–1441. [Google Scholar] [CrossRef]
- Tsukimori, K.; Fukushima, K.; Tsushima, A.; Nakano, H. Generation of reactive oxygen species by neutrophils and endothelial cell injury in normal and preeclamptic pregnancies. Hypertension 2005, 6, 696–700. [Google Scholar] [CrossRef]
- Tsukimori, K.; Tsushima, A.; Fukushima, K.; Nakano, H.; Wake, N. Neutrophil-derived reactive oxygen species can modulate neutrophil adhesion to endothelial cells in preeclampsia. Am. J. Hypertens. 2008, 21, 587–591. [Google Scholar] [CrossRef]
- Barden, A.; Graham, D.; Beilin, L.J.; Ritchie, J.; Baker, R.; Walters, B.N.; Michael, C.A. Neutrophil CD11B expression and neutrophil activation in pre-eclampsia. Clin. Sci. 1997, 92, 37–44. [Google Scholar] [CrossRef]
- Örgül, G.; Aydın Haklı, D.; Özten, G.; Fadiloğlu, E.; Tanacan, A.; Beksaç, M.S. First trimester complete blood cell indices in early and late onset preeclampsia. J. Turkish Soc. Obstet. Gynecol. 2019, 16, 112–117. [Google Scholar] [CrossRef]
- Yuksel, S.; Ozyurek, S.E.; Acar, D.K.; Ozdemir, C.; Guler, S.; Kiyak, H.; Gedikbasi, A. Urinary neutrophil gelatinase-associated lipocalin is associated with preeclampsia in a cohort of Turkish women. Hypertens. Pregnancy 2019, 38, 157–162. [Google Scholar] [CrossRef]
- Libby, P.; Lichtman, A.H.; Hansson, G.K. Immune Effector Mechanisms Implicated in Atherosclerosis: From Mice to Humans. Immunity 2013, 38, 1092–1104. [Google Scholar] [CrossRef] [PubMed]
- Hansson, G.K.; Libby, P.; Tabas, I. Inflammation and plaque vulnerability. J. Intern. Med. 2015, 278, 483–493. [Google Scholar] [CrossRef] [PubMed]
- Libby, P. Inflammation in atherosclerosis. Nature 2002, 420, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Libby, P.; Ridker, P.M.; Hansson, G.K. Progress and challenges in translating the biology of atherosclerosis. Nature 2011, 473, 317–325. [Google Scholar] [CrossRef]
- Hartwig, H.; Roig, C.; Daemen, M.; Lutgens, E.; Soehnlein, O. Neutrophils in atherosclerosis. Hamostaseologie 2015, 35, 121–127. [Google Scholar]
- Drechsler, M.; Megens, R.T.; van Zandvoort, M.; Weber, C.; Soehnlein, O. Hyperlipidemia-triggered neutrophilia promotes early atherosclerosis. Circulation 2010, 122, 1837–1845. [Google Scholar] [CrossRef]
- Ionita, M.G.; van den Borne, P.; Catanzariti, L.M.; Moll, F.L.; de Vries, J.-P.P.M.; Pasterkamp, G.; Vink, A.; de Kleijn, D.P.V. High Neutrophil Numbers in Human Carotid Atherosclerotic Plaques Are Associated With Characteristics of Rupture-Prone Lesions. Arterioscler. Thromb. Vasc. Biol. 2010, 30, 1842–1848. [Google Scholar] [CrossRef]
- Naruko, T.; Ueda, M.; Haze, K.; Van der Wal, A.C.; van der Loos, C.M.; Itoh, A.; Komatsu, R.; Ikura, Y.; Ogami, M.; Shimada, Y.; et al. Neutrophil infiltration of culprit lesions in acute coronary syndromes. Circulation 2002, 106, 2894–2900. [Google Scholar] [CrossRef]
- Lenglet, S.; Thomas, A.; Soehnlein, O.; Montecucco, F.; Burger, F.; Pelli, G.; Galan, K.; Cravatt, B.; Staub, C.; Steffens, S. Fatty Acid Amide Hydrolase Deficiency Enhances Intraplaque Neutrophil Recruitment in Atherosclerotic Mice. Arterioscler. Thromb. Vasc. Biol. 2013, 33, 215–223. [Google Scholar] [CrossRef]
- Döring, Y.; Drechsler, M.; Wantha, S.; Kemmerich, K.; Lievens, D.; Vijayan, S.; Gallo, R.L.; Weber, C.; Soehnlein, O. Lack of Neutrophil-Derived CRAMP Reduces Atherosclerosis in Mice. Circ. Res. 2012, 110, 1052–1056. [Google Scholar] [CrossRef]
- Woollard, K.J.; Geissmann, F. Monocytes in atherosclerosis: Subsets and functions. Nat. Rev. Cardiol. 2010, 7, 77–86. [Google Scholar] [CrossRef] [PubMed]
- ó Hartaigh, B.; Bosch, J.A.; Thomas, G.N.; Lord, J.M.; Pilz, S.; Loerbroks, A.; Kleber, M.E.; Grammer, T.B.; Fischer, J.E.; Boehm, B.O.; et al. Which leukocyte subsets predict cardiovascular mortality? From the LUdwigshafen RIsk and Cardiovascular Health (LURIC) Study. Atherosclerosis 2012, 224, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Horne, B.D.; Anderson, J.L.; John, J.M.; Weaver, A.; Bair, T.L.; Jensen, K.R.; Renlund, D.G.; Muhlestein, J.B. Which White Blood Cell Subtypes Predict Increased Cardiovascular Risk? J. Am. Coll. Cardiol. 2005, 45, 1638–1643. [Google Scholar] [CrossRef] [PubMed]
- Grau, A.J.; Boddy, A.W.; Dukovic, D.A.; Buggle, F.; Lichy, C.; Brandt, T.; Hacke, W. Leukocyte Count as an Independent Predictor of Recurrent Ischemic Events. Stroke 2004, 35, 1147–1152. [Google Scholar] [CrossRef] [PubMed]
- Meissner, J.; Irfan, A.; Twerenbold, R.; Mueller, S.; Reiter, M.; Haaf, P.; Reichlin, T.; Schaub, N.; Winkler, K.; Pfister, O.; et al. Use of Neutrophil Count in Early Diagnosis and Risk Stratification of AMI. Am. J. Med. 2011, 124, 534–542. [Google Scholar] [CrossRef] [PubMed]
- Zernecke, A.; Bot, I.; Talab, Y.D.; Shagdarsuren, E.; Bidzhekov, K.; Meiler, S.; Krohn, R.; Schober, A.; Sperandio, M.; Soehnlein, O.; et al. Protective role of CXC receptor 4/CXC ligand 12 unveils the importance of neutrophils in atherosclerosis. Circ Res. 2008, 102, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Bot, I.; Daissormont, I.T.M.N.; Zernecke, A.; van Puijvelde, G.H.M.; Kramp, B.; de Jager, S.C.A.; Sluimer, J.C.; Manca, M.; Hérias, V.; Westra, M.M.; et al. CXCR4 blockade induces atherosclerosis by affecting neutrophil function. J. Mol. Cell. Cardiol. 2014, 74, 44–52. [Google Scholar] [CrossRef]
- Zoet, G.A.; Meun, C.; Benschop, L.; Boersma, E.; Budde, R.P.J.; Fauser, B.C.J.M.; de Groot, C.J.M.; van der Lugt, A.; Maas, A.H.E.M.; Moons, K.G.M.; et al. Cardiovascular RiskprofilE—IMaging and gender-specific disOrders (CREw-IMAGO): Rationale and design of a multicenter cohort study. BMC Womens Health 2017, 17, 60. [Google Scholar] [CrossRef]
- Zoet, G.A.; Benschop, L.; Boersma, E.; Budde, R.P.J.; Fauser, B.C.J.M.; van der Graaf, Y.; de Groot, C.J.M.; Maas, A.H.E.M.; Roeters van Lennep, J.E.; Steegers, E.A.P.; et al. Prevalence of Subclinical Coronary Artery Disease Assessed by Coronary Computed Tomography Angiography in 45- to 55-Year-Old Women With a History of Preeclampsia. Circulation 2018, 137, 877–879. [Google Scholar] [CrossRef]
- Tranquilli, A.L.; Dekker, G.; Magee, L.; Roberts, J.; Sibai, B.M.; Steyn, W.; Zeeman, G.G.; Brown, M.A. The classification, diagnosis and management of the hypertensive disorders of pregnancy: A revised statement from the ISSHP. Pregnancy Hypertens. An Int. J. Women’s Cardiovasc. Heal. 2014, 4, 97–104. [Google Scholar] [CrossRef]
- Agatston, A.S.; Janowitz, W.R.; Hildner, F.J.; Zusmer, N.R.; Viamonte, M.; Detrano, R. Quantification of coronary artery calcium using ultrafast computed tomography. J. Am. Coll. Cardiol. 1990, 15, 827–832. [Google Scholar] [CrossRef]
- Austen, W.G.; Edwards, J.E.; Frye, R.L.; Gensini, G.G.; Gott, V.L.; Griffith, L.S.; McGoon, D.C.; Murphy, M.L.; Roe, B.B. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation 1975, 51, 5–40. [Google Scholar] [CrossRef] [PubMed]
- Raff, G.L.; Chair; Abidov, A.; Achenbach, S.; Berman, D.S.; Boxt, L.M.; Budoff, M.J.; Cheng, V.; DeFrance, T.; Hellinger, J.C.; et al. SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. J. Cardiovasc. Comput. Tomogr. 2009, 3, 122–136. [Google Scholar] [CrossRef]
- McClelland, R.L.; Chung, H.; Detrano, R.; Post, W.; Kronmal, R.A. Distribution of Coronary Artery Calcium by Race, Gender, and Age. Circulation 2006, 113, 30–37. [Google Scholar] [CrossRef]
- Hadamitzky, M.; Achenbach, S.; Al-Mallah, M.; Berman, D.; Budoff, M.; Cademartiri, F.; Callister, T.; Chang, H.-J.; Cheng, V.; Chinnaiyan, K.; et al. Optimized Prognostic Score for Coronary Computed Tomographic Angiography. J. Am. Coll. Cardiol. 2013, 62, 468–476. [Google Scholar] [CrossRef]
- Allaire, J.J. RStudio: Integrated Development Environment for R; John Wiley & Sons: Hoboken, NJ, USA, 2015. [Google Scholar]
- R Core Team R Core Team. R: A Language and Environment for Statistical Computing; The R Foundation: Vienna, Austria, 2014. [Google Scholar]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Gogoi, P.; Sinha, P.; Gupta, B.; Firmal, P.; Rajaram, S. Neutrophil-to-lymphocyte ratio and platelet indices in pre-eclampsia. Int. J. Gynecol. Obstet. 2019, 144, 16–20. [Google Scholar] [CrossRef]
- Panwar, M.; Kumari, A.; HP, A.; Arora, R.; Singh, V.; Bansiwal, R. Raised neutrophil lymphocyte ratio and serum beta hCG level in early second trimester of pregnancy as predictors for development and severity of preeclampsia. Drug Discov. Ther. 2019, 13, 34–37. [Google Scholar] [CrossRef]
- Yavuzcan, A.; Cağlar, M.; Ustün, Y.; Dilbaz, S.; Ozdemir, I.; Yildiz, E.; Ozbilgeç, S.; Kumru, S. Mean platelet volume, neutrophil-lymphocyte ratio and platelet-lymphocyte ratio in severe preeclampsia. Ginekol. Pol. 2014, 85, 197–203. [Google Scholar] [CrossRef]
- Gezer, C.; Ekin, A.; Ertas, I.E.; Ozeren, M.; Solmaz, U.; Mat, E.; Taner, C.E. High first-trimester neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios are indicators for early diagnosis of preeclampsia. Ginekol. Pol. 2016, 87, 431–435. [Google Scholar] [CrossRef]
- Zheng, W.-F.; Zhan, J.; Chen, A.; Ma, H.; Yang, H.; Maharjan, R. Diagnostic value of neutrophil-lymphocyte ratio in preeclampsia. Medicine 2019, 98, e18496. [Google Scholar] [CrossRef] [PubMed]
- De Moreuil, C.; Herry, E.; Lacut, K.; Chauvet, J.; Moineau, M.-P.; Lede, F.; Tremouilhac, C.; Merviel, P.; Petesch, B.P.; Le Moigne, E.; et al. Correlation of biological parameters with placental parameters and pregnancy outcomes in pre-eclamptic women. Pregnancy Hypertens. 2020, 19, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.D.; Denaxas, S.; Nicholas, O.; Hingorani, A.D.; Hemingway, H. Neutrophil Counts and Initial Presentation of 12 Cardiovascular Diseases: A CALIBER Cohort Study. J. Am. Coll. Cardiol. 2017, 69, 1160–1169, Correction in 2017, 69, 3125–3126. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, H.; Mori, T.; Kawano, T.; Kono, S.; Sasaki, J.; Arakawa, K. Band neutrophil count and the presence and severity of coronary atherosclerosis. Am. Heart J. 1996, 132, 9–12. [Google Scholar] [CrossRef]
- Tikhonov, I.; Doroshenko, T.; Chaly, Y.; Smolnikova, V.; Pauza, C.D.; Voitenok, N. Down-regulation of CXCR1 and CXCR2 expression on human neutrophils upon activation of whole blood by S. aureus is mediated by TNF-α. Clin. Exp. Immunol. 2001, 125, 414–422. [Google Scholar] [CrossRef]
- Bruèhl, H.; Wagner, K.; Kellner, H.; Schattenkirchner, M.; Schloèndorff, D.; Mack, M. Surface expression of CC- and CXC-chemokine receptors on leucocyte subsets in inflammatory joint diseases. Clin. Exp. Immunol. 2001, 126, 551–559. [Google Scholar] [CrossRef]
- Wu, D.; Hong, H.; Huang, X.; Huang, L.; He, Z.; Fang, Q.; Luo, Y. CXCR2 is decreased in preeclamptic placentas and promotes human trophoblast invasion through the Akt signaling pathway. Placenta 2016, 43, 17–25. [Google Scholar] [CrossRef]
- Rosenbloom, A.J.; Pinsky, M.R.; Bryant, J.L.; Shin, A.; Tran, T.; Whiteside, T. Leukocyte activation in the peripheral blood of patients with cirrhosis of the liver and SIRS. Correlation with serum interleukin-6 levels and organ dysfunction. JAMA 1995, 274, 58–65. [Google Scholar] [CrossRef]
- Sadallah, S.; Lach, E.; Lutz, H.U.; Schwarz, S.; Guerne, P.-A.; Schifferli, J.A. Cr1, CD35 IN synovial fluid from patients with inflammatory joint diseases. Arthritis Rheum. 1997, 40, 520–526. [Google Scholar] [CrossRef]
- De Vries, M.A.; Trompet, S.; Mooijaart, S.P.; Smit, R.A.J.; Böhringer, S.; Castro Cabezas, M.; Jukema, J.W. Complement receptor 1 gene polymorphisms are associated with cardiovascular risk. Atherosclerosis 2017, 257, 16–21. [Google Scholar] [CrossRef]
- Boiocchi, C.; Zorzetto, M.; Sbarsi, I.; Pirotta, A.; Schirinzi, S.; Falcone, C.; Cuccia, M. CR1 genotype and haplotype involvement in coronary artery disease: The pivotal role of hypertension and dyslipidemia. Int. J. Mol. Med. 2009, 24, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Doeing, D.C.; Borowicz, J.L.; Crockett, E.T. Gender dimorphism in differential peripheral blood leukocyte counts in mice using cardiac, tail, foot, and saphenous vein puncture methods. BMC Clin. Pathol. 2003, 3, 3. [Google Scholar] [CrossRef] [PubMed]
- Mestas, J.; Hughes, C.C.W. Of Mice and Not Men: Differences between Mouse and Human Immunology. J. Immunol. 2004, 172, 2731–2738. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, J.A.; Zhang, P. Gender differences in neutrophil function and cytokine-induced neutrophil chemoattractant generation in endotoxic rats. Inflammation 1996, 20, 485–498. [Google Scholar] [CrossRef]
- Tillack, K.; Naegele, M.; Haueis, C.; Schippling, S.; Wandinger, K.-P.; Martin, R.; Sospedra, M. Gender differences in circulating levels of neutrophil extracellular traps in serum of multiple sclerosis patients. J. Neuroimmunol. 2013, 261, 108–119. [Google Scholar] [CrossRef]
- Yavuz, S.; Ozilhan, G.; Elbir, Y.; Tolunay, A.; Eksioglu-Demiralp, E.; Direskeneli, H. Activation of neutrophils by testosterone in Behçet’s disease. Clin. Exp. Rheumatol. 2007, 25, S46–S51. [Google Scholar]
- Gohar, A.; Gonçalves, I.; Vrijenhoek, J.; Haitjema, S.; van Koeverden, I.; Nilsson, J.; de Borst, G.J.; de Vries, J.-P.; Pasterkamp, G.; den Ruijter, H.M.; et al. Circulating GDF-15 levels predict future secondary manifestations of cardiovascular disease explicitly in women but not men with atherosclerosis. Int. J. Cardiol. 2017, 241, 430–436. [Google Scholar] [CrossRef]

| Controls | CAD Cases | p | |
|---|---|---|---|
| n = 78 | n = 12 | ||
| Patient characteristics | |||
| Age (years) | 49.4 ± 3.7 | 49.0 ± 5.0 | 0.72 |
| GA delivery (days) | 213.0 ± 28.4 | 205.6 ± 20.4 | 0.39 |
| Clinical measurements | |||
| Systolic blood pressure (mmHg) | 130.8 ± 16.0 | 127.5 ± 15.1 | 0.50 |
| Diastolic blood pressure (mmHg) | 80.1 ± 10.0 | 77.7 ± 10.6 | 0.43 |
| BMI (kg/m2) | 27.6 ± 5.1 | 29.7 ± 6.9 | 0.20 |
| Waist circumference (cm) | 88.4 ± 11.9 | 94.6 ± 11.6 | 0.09 |
| Total cholesterol (mmol/L) | 5.3 [4.8–6.0] | 5.6 [4.8–5.8] | 0.87 |
| Triglycerides (mmol/L) | 1.1 [0.8–1.5] | 1.2 [0.9–1.5] | 0.54 |
| HDL-cholesterol (mmol/L) | 1.5 [1.3–1.6] | 1.5 [1.3–1.6] | 1.00 |
| LDL-cholesterol (mmol/L) | 3.3 [2.8–3.9] | 3.4 [2.7–3.8] | 0.64 |
| Glucose (mmol/L) | 5.5 ± 1.3 | 5.3 ± 0.5 | 0.57 |
| CVD risk factors | |||
| Family history of premature CVD (no, %) | 31 (39.7) | 8 (66.7) | 0.15 |
| Hypertensiona (no, %) | 42 (54.5) | 8 (66.7) | 0.64 |
| Obesity (no, %) | 23 (29.5) | 4 (33.3) | 0.75† |
| Diabetes (no, %) | 3 (3.8) | 0 (0.0) | 1.00† |
| Current smoking (no, %) | 8 (10.5) | 0 (0.0) | 0.59† |
| Metabolic syndromeb (no, %) | 25 (32.1) | 4 (33.3) | 1.00† |
| FRS (percentage) | 6.4 ± 4.0 | 5.5 ± 3.5 | 0.48 |
| Intermediate–high risk, FRS ≥10% (no, %) | 12 (15.8) | 1 (9.1) | 1.00† |
| Whole blood count | |||
| WBC (G/L) | 6.8 [5.5–7.8] | 6.6 [5.5–8.4] | 0.79 |
| Lymphocytes (G/L) | 1.8 [1.4–2.1] | 1.8 [1.3–2.1] | 0.97 |
| Monocytes (G/L) | 0.7 [0.5–0.8] | 0.7 [0.6–0.7] | 0.72 |
| Granulocytes (G/L) | 4.1 [3.3–5.3] | 4.6 [3.6–5.7] | 0.45 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meeuwsen, J.A.L.; de Vries, J.; Zoet, G.A.; Franx, A.; Fauser, B.C.J.M.; Maas, A.H.E.M.; Velthuis, B.K.; Appelman, Y.E.; Visseren, F.L.; Pasterkamp, G.; et al. Circulating Neutrophils Do Not Predict Subclinical Coronary Artery Disease in Women with Former Preeclampsia. Cells 2020, 9, 468. https://doi.org/10.3390/cells9020468
Meeuwsen JAL, de Vries J, Zoet GA, Franx A, Fauser BCJM, Maas AHEM, Velthuis BK, Appelman YE, Visseren FL, Pasterkamp G, et al. Circulating Neutrophils Do Not Predict Subclinical Coronary Artery Disease in Women with Former Preeclampsia. Cells. 2020; 9(2):468. https://doi.org/10.3390/cells9020468
Chicago/Turabian StyleMeeuwsen, John A.L., Judith de Vries, Gerbrand A. Zoet, Arie Franx, Bart C. J. M. Fauser, Angela H. E. M. Maas, Birgitta K. Velthuis, Yolande E. Appelman, Frank L. Visseren, Gerard Pasterkamp, and et al. 2020. "Circulating Neutrophils Do Not Predict Subclinical Coronary Artery Disease in Women with Former Preeclampsia" Cells 9, no. 2: 468. https://doi.org/10.3390/cells9020468
APA StyleMeeuwsen, J. A. L., de Vries, J., Zoet, G. A., Franx, A., Fauser, B. C. J. M., Maas, A. H. E. M., Velthuis, B. K., Appelman, Y. E., Visseren, F. L., Pasterkamp, G., Hoefer, I. E., van Rijn, B. B., den Ruijter, H. M., & de Jager, S. C. A. (2020). Circulating Neutrophils Do Not Predict Subclinical Coronary Artery Disease in Women with Former Preeclampsia. Cells, 9(2), 468. https://doi.org/10.3390/cells9020468






