Blood Contamination in CSF and Its Impact on Quantitative Analysis of Alpha-Synuclein
Abstract
1. Introduction
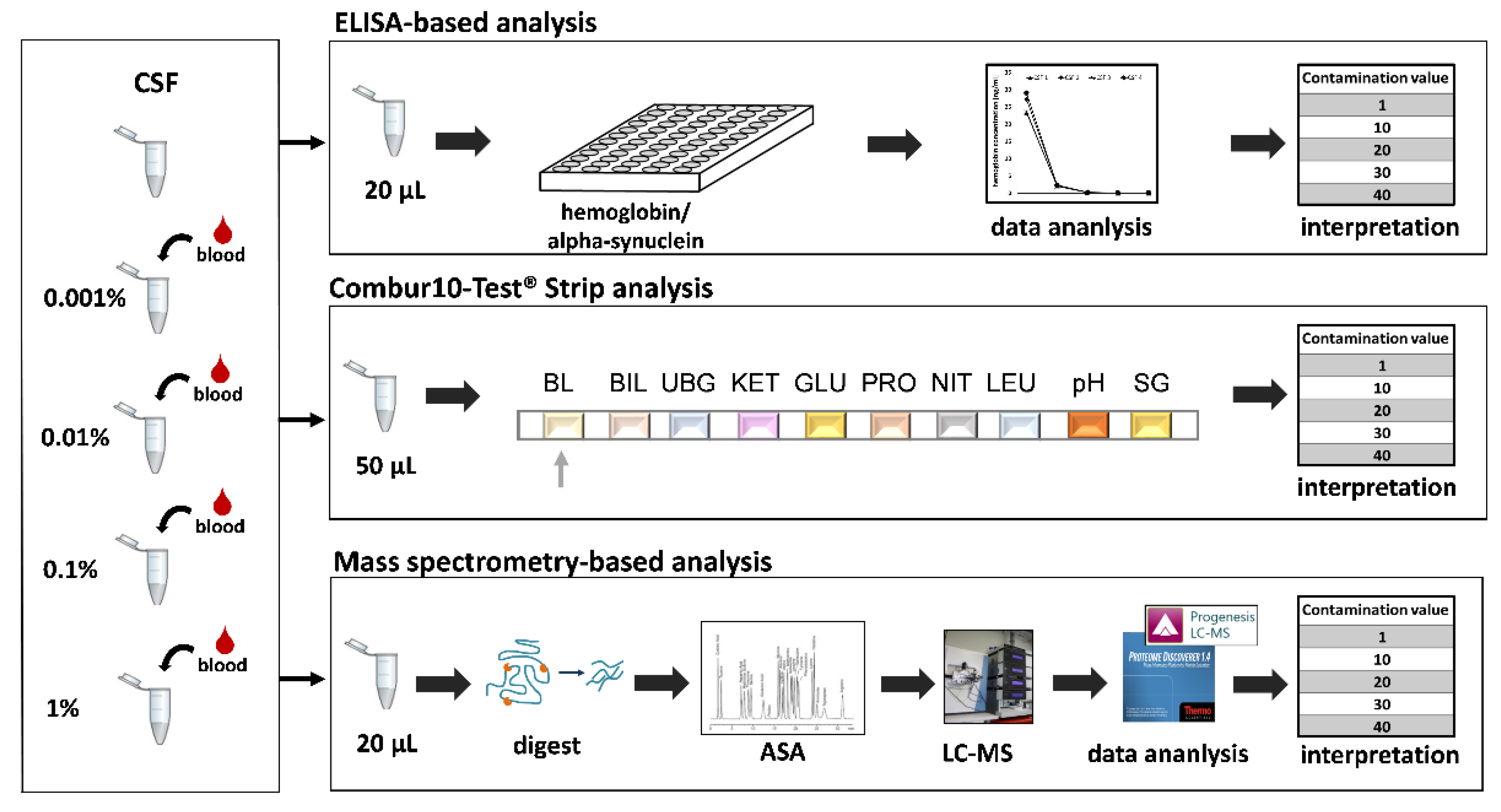
2. Materials and Methods
2.1. Sample Preparation
2.2. Immuno-Based Quantification of Hemoglobin and aSyn
2.3. Combur10-Test® Strip Analysis
2.4. Protein Digestion
2.5. Nano LC-MS/MS Analysis
2.6. Protein Identification and Quantification
3. Results
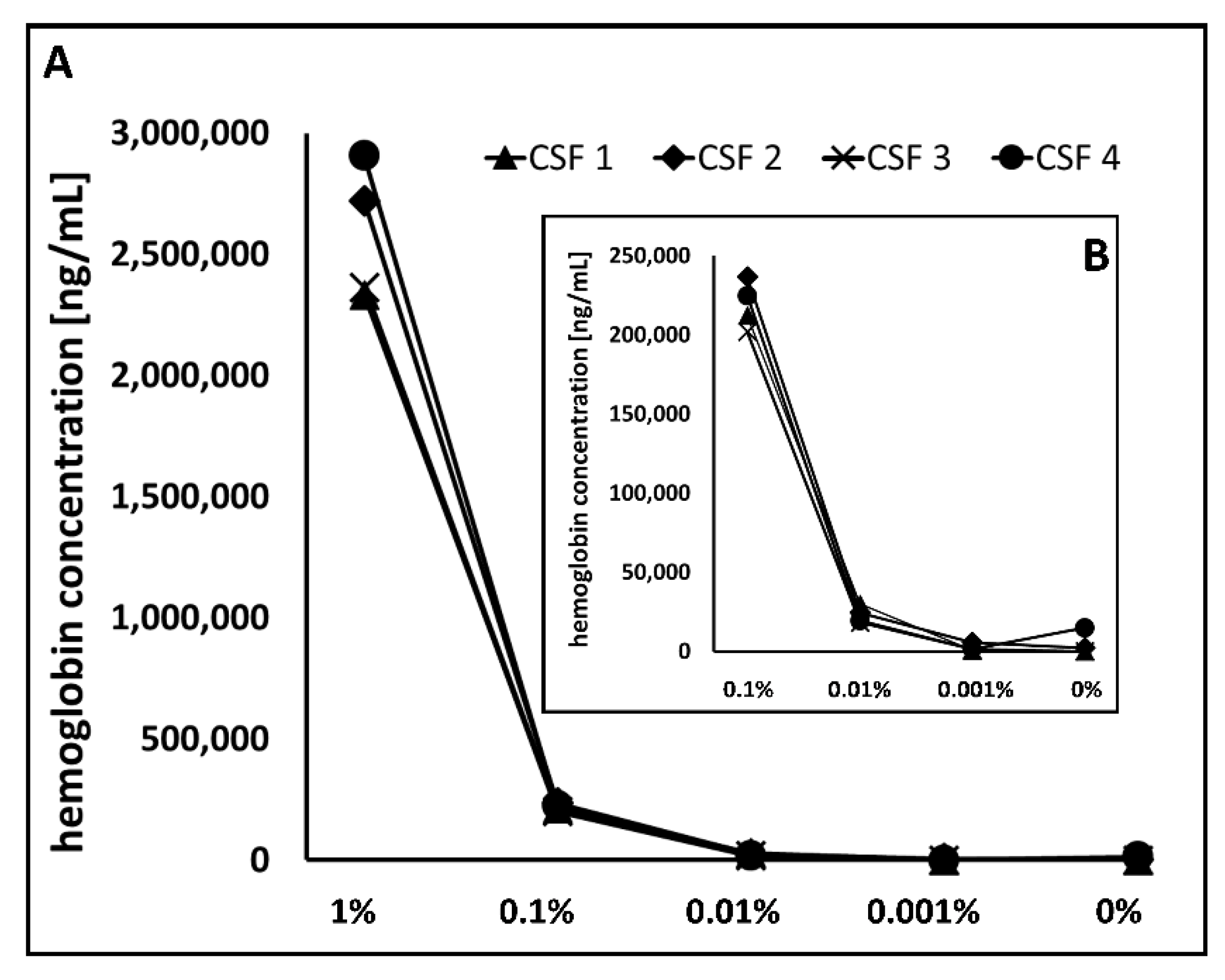
3.1. Detection of Blood Levels in CSF
3.1.1. Hemoglobin ELISA
3.1.2. Combur10-Test® Strip
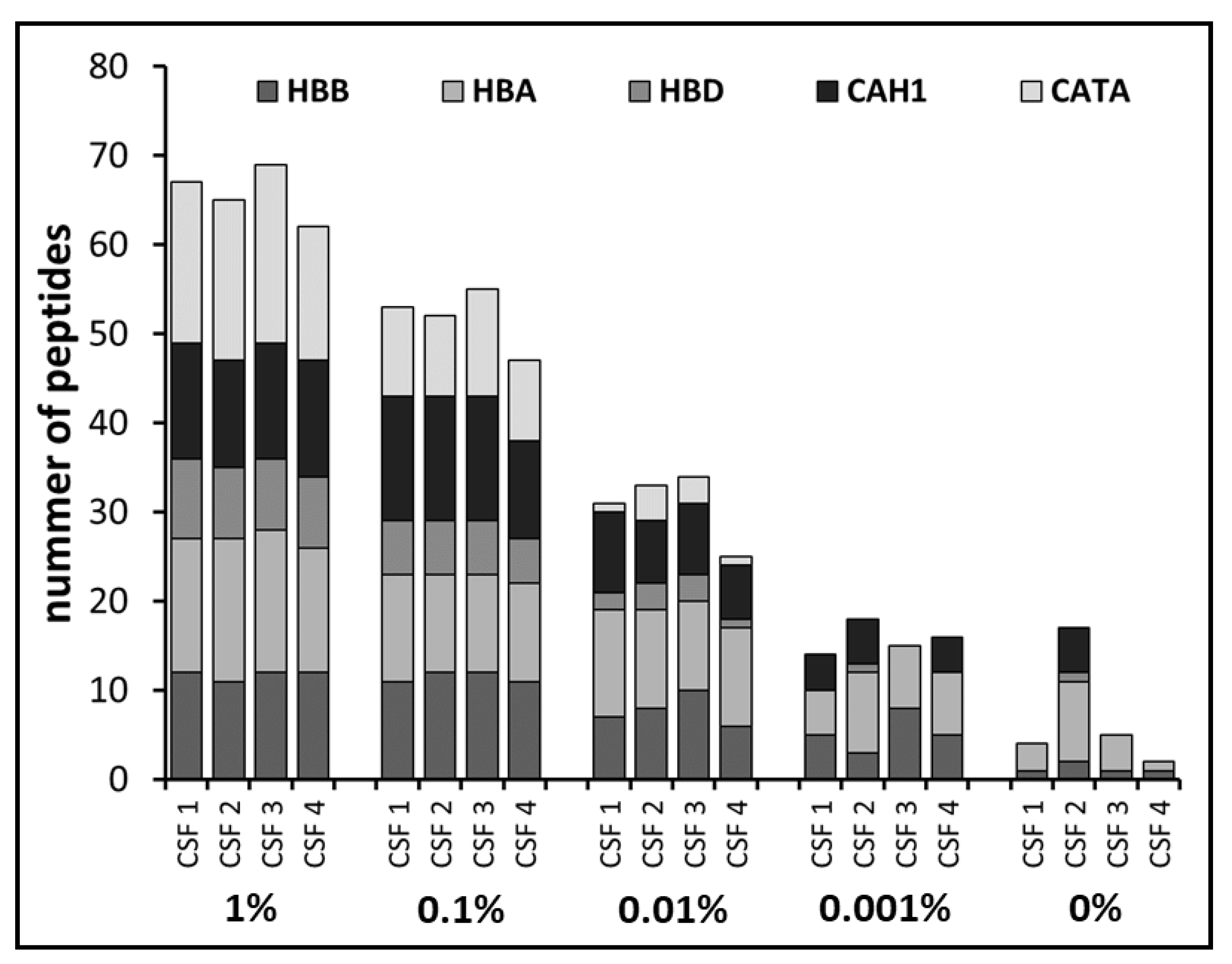
3.2. Definition of Blood Protein Markers by Mass Spectrometry
3.3. Categorization of CSF Blood Levels
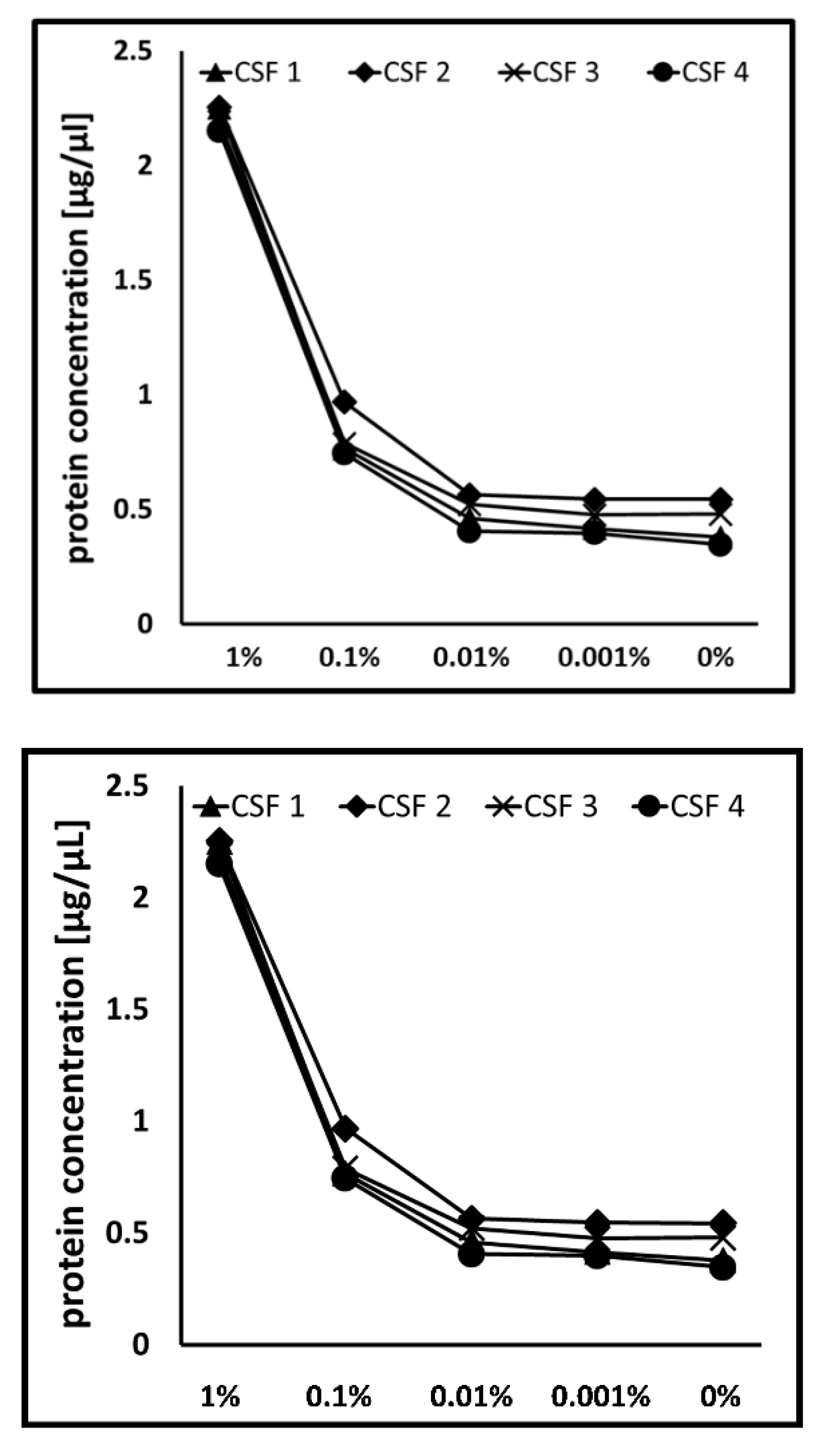
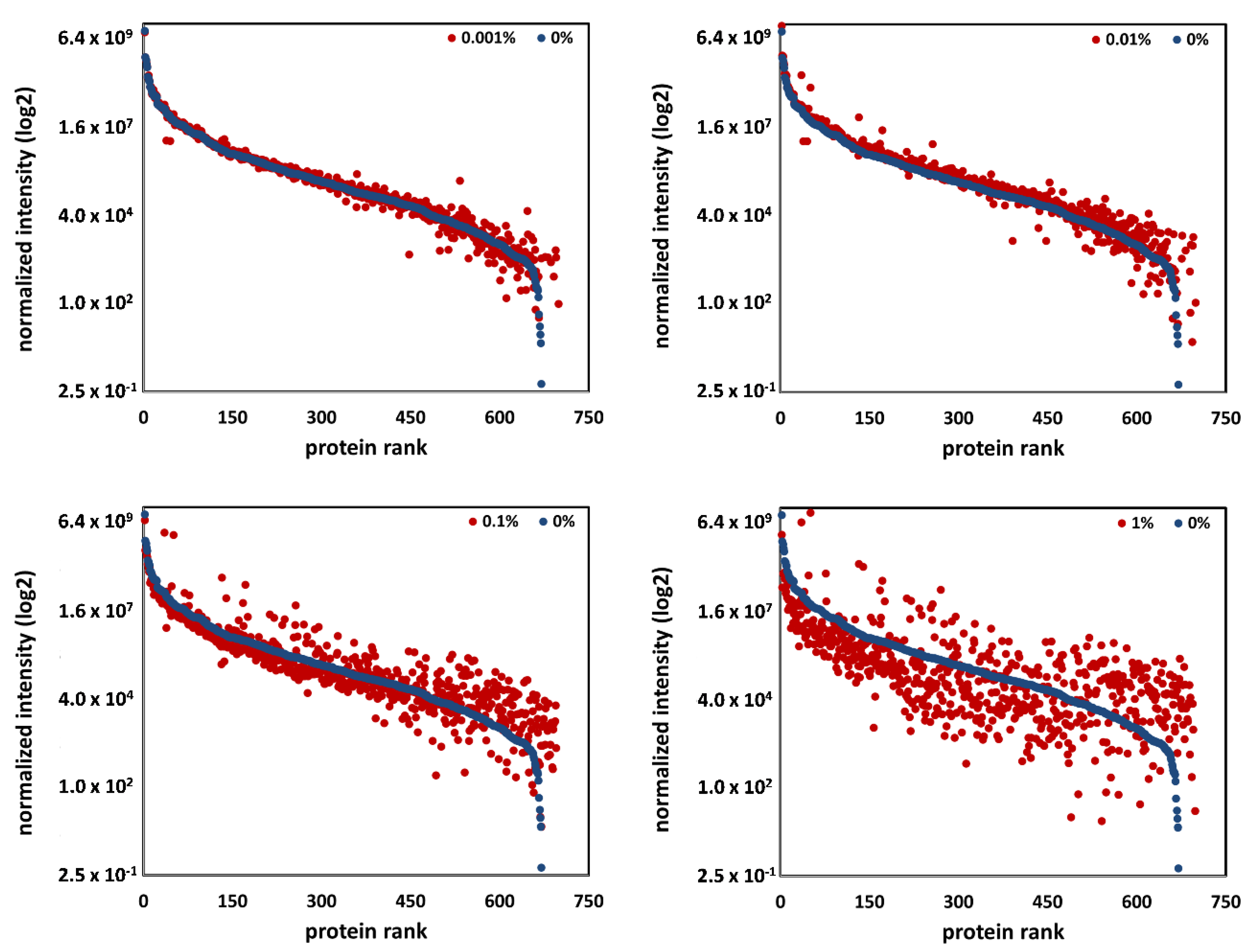
3.4. Blood Contamination Influenced the Global CSF Proteome
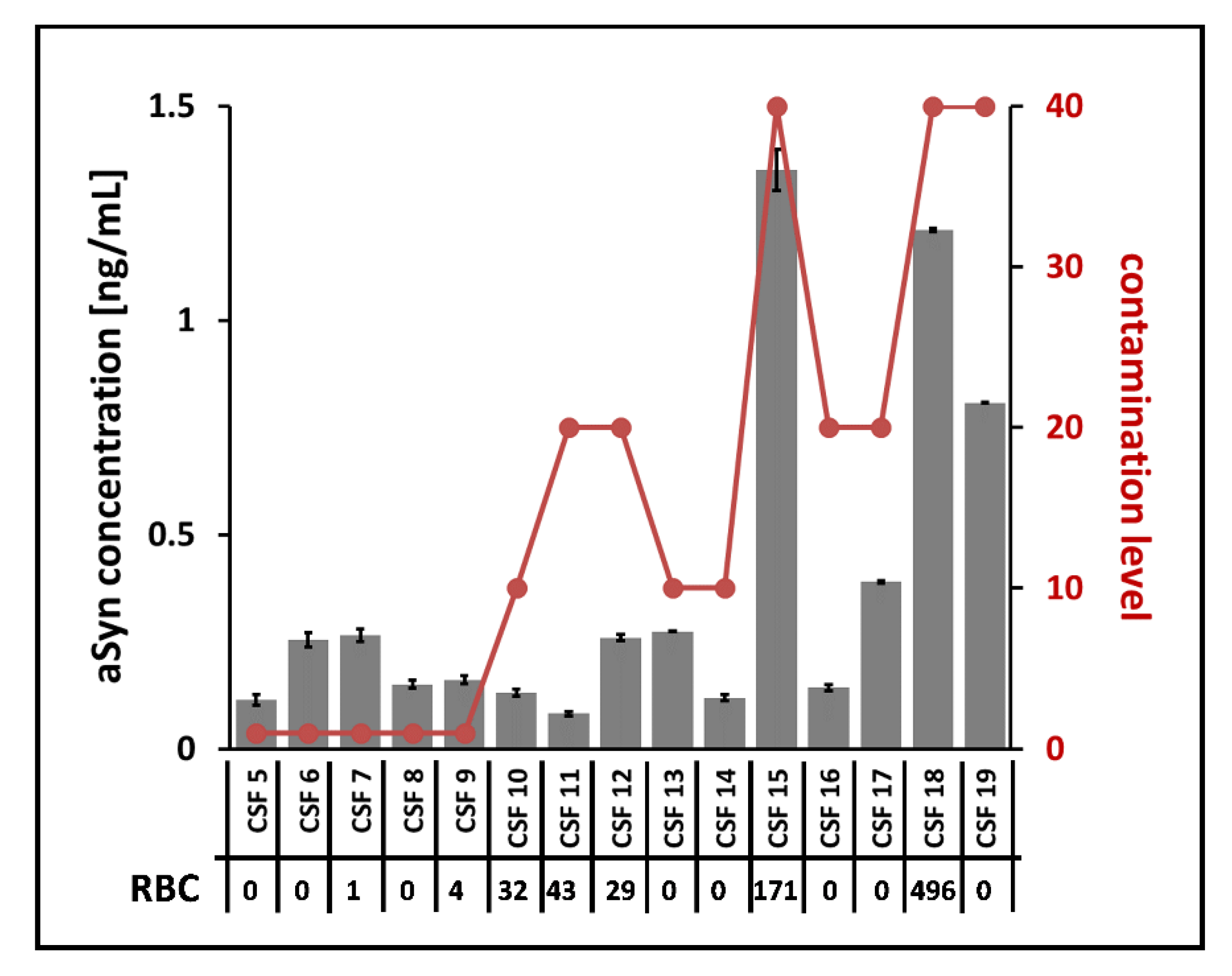
3.5. Impact of CSF Blood Contamination on aSyn Quantification
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Availability of Data and Materials
Submission Details
References
- Petzold, A.; Sharpe, L.T.; Keir, G. Spectrophotometry for cerebrospinal fluid pigment analysis. Neurocrit. Care 2006, 4, 153–162. [Google Scholar] [CrossRef]
- Hansson, O.; Mikulskis, A.; Fagan, A.M.; Teunissen, C.; Zetterberg, H.; Vanderstichele, H.; Molinuevo, J.L.; Shaw, L.M.; Vandijck, M.; Verbeek, M.M.; et al. The impact of preanalytical variables on measuring cerebrospinal fluid biomarkers for Alzheimer’s disease diagnosis: A review. Alzheimers Dement. 2018, 14, 1313–1333. [Google Scholar] [CrossRef] [PubMed]
- Schwenkenbecher, P.; Janssen, T.; Wurster, U.; Konen, F.F.; Neyazi, A.; Ahlbrecht, J.; Puppe, W.; Bönig, L.; Sühs, K.W.; Stangel, M.; et al. The Influence of Blood Contamination on Cerebrospinal Fluid Diagnostics. Front. Neurol. 2019, 10, 584. [Google Scholar] [CrossRef] [PubMed]
- Atik, A.; Stewart, T.; Zhang, J. Alpha-Synuclein as a Biomarker for Parkinson’s Disease. Brain Pathol. 2016, 26, 410–418. [Google Scholar] [CrossRef] [PubMed]
- Nakai, M.; Fujita, M.; Waragai, M.; Sugama, S.; Wei, J.; Akatsu, H.; Ohtaka-Maruyama, C.; Okado, H.; Hashimoto, M. Expression of alpha-synuclein, a presynaptic protein implicated in Parkinson’s disease, in erythropoietic lineage. Biochem. Biophys. Res. Commun. 2007, 358, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Barkovits, K.; Linden, A.; Galozzi, S.; Schilde, L.; Pacharra, S.; Mollenhauer, B.; Stoepel, N.; Steinbach, S.; May, C.; Uszkoreit, J.; et al. Characterization of Cerebrospinal Fluid via Data-Independent Acquisition Mass Spectrometry. J. Proteome Res. 2018, 17, 3418–3430. [Google Scholar] [CrossRef]
- Aasebø, E.; Opsahl, J.A.; Bjørlykke, Y.; Myhr, K.M.; Kroksveen, A.C.; Berven, F.S. Effects of blood contamination and the rostro-caudal gradient on the human cerebrospinal fluid proteome. PLoS ONE 2014, 9, e90429. [Google Scholar] [CrossRef]
- Hall, S.; Öhrfelt, A.; Constantinescu, R.; Andreasson, U.; Surova, Y.; Bostrom, F.; Nilsson, C.; Håkan, W.; Decraemer, H.; Någga, K.; et al. Accuracy of a panel of 5 cerebrospinal fluid biomarkers in the differential diagnosis of patients with dementia and/or parkinsonian disorders. Arch. Neurol. 2012, 69, 1445–1452. [Google Scholar] [CrossRef]
- Hong, Z.; Shi, M.; Chung, K.A.; Quinn, J.F.; Peskind, E.R.; Galasko, D.; Jankovic, J.; Zabetian, C.P.; Leverenz, J.B.; Baird, G.; et al. DJ-1 and alpha-synuclein in human cerebrospinal fluid as biomarkers of Parkinson’s disease. Brain 2010, 133, 713–726. [Google Scholar] [CrossRef]
- Teunissen, C.E.; Petzold, A.; Bennett, J.L.; Berven, F.S.; Brundin, L.; Comabella, M.; Franciotta, D.; Frederiksen, J.L.; Fleming, J.O.; Furlan, R.; et al. A consensus protocol for the standardization of cerebrospinal fluid collection and biobanking. Neurology 2009, 73, 1914–1922. [Google Scholar] [CrossRef]
- del Campo, M.; Mollenhauer, B.; Bertolotto, A.; Engelborghs, S.; Hampel, H.; Simonsen, A.H.; Kapaki, E.; Kruse, N.; Le Bastard, N.; Lehmann, S.; et al. Recommendations to standardize preanalytical confounding factors in Alzheimer’s and Parkinson’s disease cerebrospinal fluid biomarkers: An update. Biomark. Med. 2012, 6, 419–430. [Google Scholar] [CrossRef] [PubMed]
- Joshi, D.; Kundana, K.; Puranik, A.; Joshi, R. Diagnostic accuracy of urinary reagent strip to determine cerebrospinal fluid chemistry and cellularity. J. Neurosci. Rural. Pr. 2013, 4, 140–145. [Google Scholar] [CrossRef] [PubMed]
- Parmar, R.C.; Warke, S.; Sira, P.; Kamat, J.R. Rapid diagnosis of meningitis using reagent strips. Indian J. Med. Sci. 2004, 58, 62–66. [Google Scholar] [PubMed]
- Mazumder, S.; Ramya, B.S.; Biligi, D.S. Utility of urine reagent strips in cerebrospinal fluid analysis: An aid to bedside diagnosis of meningitis. Indian J. Pathol. Microbiol. 2018, 61, 356–359. [Google Scholar] [CrossRef]
- Marshall, R.A.; Hejamanowski, C. Urine test strips to exclude cerebral spinal fluid blood. West J. Emerg. Med. 2011, 12, 63–66. [Google Scholar]
- Reeve, S.F.; Johnson, J.S.; Marshall, R. Urine Test Strips as a Bedside Diagnostic Aid to Rule out Blood in CSF: A Validation. Mil. Med. 2016, 181, 199–201. [Google Scholar] [CrossRef][Green Version]
- Mollenhauer, B.; Locascio, J.J.; Schulz-Schaeffer, W.; Sixel-Doring, F.; Trenkwalder, C.; Schlossmacher, M.G. alpha-Synuclein and tau concentrations in cerebrospinal fluid of patients presenting with parkinsonism: A cohort study. Lancet Neurol. 2011, 10, 230–240. [Google Scholar] [CrossRef]
- Kruse, N.; El-Agnaf, O.M.; Mollenhauer, B. Validation of electrochemiluminescence assays for highly sensitive and reproducible quantification of alpha-synuclein in cerebrospinal fluid. Bioanalysis 2017, 9, 621–630. [Google Scholar] [CrossRef]
- Molina, M.; Steinbach, S.; Park, Y.M.; Yun, S.Y.; Di Lorenzo Alho, A.T.; Heinsen, H.; Grinberg, L.T.; Marcus, K.; Leite, R.E.; May, C. Enrichment of single neurons and defined brain regions from human brain tissue samples for subsequent proteome analysis. J. Neural. Transm. 2015, 122, 993–1005. [Google Scholar] [CrossRef]
- Vizcaino, J.A.; Csordas, A.; del-Toro, N.; Dianes, J.A.; Griss, J.; Lavidas, I.; Mayer, G.; Perez-Riverol, Y.; Reisinger, F.; Ternent, T.; et al. 2016 update of the PRIDE database and its related tools. Nucleic Acids Res. 2016, 44, D447–D456. [Google Scholar] [CrossRef]
- You, J.S.; Gelfanova, V.; Knierman, M.D.; Witzmann, F.A.; Wang, M.; Hale, J.E. The impact of blood contamination on the proteome of cerebrospinal fluid. Proteomics 2005, 5, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Scheltema, R.A.; Hauschild, J.P.; Lange, O.; Hornburg, D.; Denisov, E.; Damoc, E.; Kuehn, A.; Makarov, A.; Mann, M. The Q Exactive HF, a Benchtop mass spectrometer with a pre-filter, high-performance quadrupole and an ultra-high-field Orbitrap analyzer. Mol. Cell Proteom. 2014, 13, 3698–3708. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.; Mann, M. MaxQuant enables high peptide identification rates, individualized p.p.b.-range mass accuracies and proteome-wide protein quantification. Nat. Biotechnol. 2008, 26, 1367–1372. [Google Scholar] [CrossRef] [PubMed]
- Schilde, L.M.; Kösters, S.; Steinbach, S.; Schork, K.; Eisenacher, M.; Galozzi, S.; Turewicz, M.; Barkovits, K.; Mollenhauer, B.; Marcus, K.; et al. Protein variability in cerebrospinal fluid and its possible implications for neurological protein biomarker research. PLoS ONE 2018, 13, e0206478. [Google Scholar] [CrossRef]
- Lleó, A.; Cavedo, E.; Parnetti, L.; Vanderstichele, H.; Herukka, S.K.; Andreasen, N.; Ghidoni, R.; Lewczuk, P.; Jeromin, A.; Winblad, B.; et al. Cerebrospinal fluid biomarkers in trials for Alzheimer and Parkinson diseases. Nat. Rev. Neurol. 2015, 11, 41–55. [Google Scholar] [CrossRef]
- Roche, S.; Gabelle, A.; Lehmann, S. Clinical proteomics of the cerebrospinal fluid: Towards the discovery of new biomarkers. Proteom. Clin. Appl. 2008, 2, 428–436. [Google Scholar] [CrossRef]
- Galasko, D. Lewy Body Disorders. Neurol. Clin. 2017, 35, 325–338. [Google Scholar] [CrossRef]
- Mollenhauer, B.; El-Agnaf, O.M.; Marcus, K.; Trenkwalder, C.; Schlossmacher, M.G. Quantification of α-synuclein in cerebrospinal fluid as a biomarker candidate: Review of the literature and considerations for future studies. Biomark. Med. 2010, 4, 683–699. [Google Scholar] [CrossRef]
- Halbgebauer, S.; Ockl, P.; Wirth, K.; Steinacker, P.; Otto, M. Protein biomarkers in Parkinson’s disease: Focus on cerebrospinal fluid markers and synaptic proteins. Mov. Disord. 2016, 31, 848–860. [Google Scholar] [CrossRef]
- Müller, M.; Kuiperij, H.B.; Claassen, J.A.; Küsters, B.; Verbeek, M.M. MicroRNAs in Alzheimer’s disease: Differential expression in hippocampus and cell-free cerebrospinal fluid. Neurobiol. Aging 2014, 35, 152–158. [Google Scholar] [CrossRef]
- Müller, M.; Jäkel, L.; Bruinsma, I.B.; Claassen, J.A.; Kuiperij, H.B.; Verbeek, M.M. MicroRNA-29a Is a Candidate Biomarker for Alzheimer’s Disease in Cell-Free Cerebrospinal Fluid. Mol. Neurobiol. 2016, 53, 2894–2899. [Google Scholar] [CrossRef] [PubMed]
- Al Moudallal, Z.; Altschuh, D.; Briand, J.P.; Van Regenmortel, M.H. Comparative sensitivity of different ELISA methods for detecting monoclonal antibodies to viruses. Dev. Biol. Stand. 1984, 57, 35–40. [Google Scholar] [PubMed]
- Mollenhauer, B.; Bowman, F.D.; Drake, D.; Duong, J.; Blennow, K.; El-Agnaf, O.; Shaw, L.M.; Masucci, J.; Taylor, P.; Umek, R.M.; et al. Antibody-based methods for the measurement of α-synuclein concentration in human cerebrospinal fluid - method comparison and round robin study. J. Neurochem. 2019, 149, 126–138. [Google Scholar] [CrossRef] [PubMed]
- Goldman, J.G.; Andrews, H.; Amara, A.; Naito, A.; Alcalay, R.N.; Shaw, L.M.; Taylor, P.; Xie, T.; Tuite, P.; Henchcliffe, C.; et al. Cerebrospinal fluid, plasma, and saliva in the BioFIND study: Relationships among biomarkers and Parkinson’s disease Features. Mov. Disord. 2018, 33, 282–288. [Google Scholar] [CrossRef]
- Kang, J.H.; Mollenhauer, B.; Coffey, C.S.; Toledo, J.B.; Weintraub, D.; Galasko, D.R.; Irwin, D.J.; Van Deerlin, V.; Chen-Plotkin, A.S.; Caspell-Garcia, C.; et al. CSF biomarkers associated with disease heterogeneity in early Parkinson’s disease: The Parkinson’s Progression Markers Initiative study. Acta Neuropathol. 2016, 131, 935–949. [Google Scholar] [CrossRef]
- Dersch, R.; Benkler, D.; Robinson, T.; Baumgartner, A.; Rauer, S.; Stich, O. Erythrophages do not develop when lumbar CSF and blood samples are mixed in vitro. Fluids Barriers CNS 2018, 15, 31. [Google Scholar] [CrossRef]


| Sample | 1% | 0.1% | 0.01% | 0.001% | 0% |
|---|---|---|---|---|---|
| CSF 1 | ++++ | ++++ | +++ | ++ | neg |
| CSF 2 | ++++ | ++++ | ++++ | +++ | ++ |
| CSF 3 | ++++ | ++++ | +++ | ++ | neg |
| CSF 4 | ++++ | ++++ | +++ | ++ | neg |
| Contamination value | HB ELISA (ng/mL) | Combur 10-Test® | LC-MS |
|---|---|---|---|
| 1 | 0 | negative | no HB or < 5 peptides |
| 10 | > 0 to 1,000 | 1+ | HB (≥ 5 peptides) |
| 20 | > 1,000 to 15,000 | 2+ (++) | HB and CAH1 |
| 30 | > 15,000 to 100,000 | 3+ (+++) | HB, CAH1 and CATA (≤ 4 peptides) |
| 40 | > 100,000 | 4+ (++++) | HB, CAH1 and CATA (≥ 5 peptides) |
| Sample | ELISA | strip | LC-MS |
|---|---|---|---|
| CSF 5 | 1 | 1 | 1 |
| CSF 6 | 1 | 1 | 1 |
| CSF 7 | 10 | 1 | 10 |
| CSF 8 | 1 | 1 | 1 |
| CSF 9 | 10 | 1 | 1 |
| CSF 10 | 10 | 10 | 10 |
| CSF 11 | 20 | 20 | 20 |
| CSF 12 | 20 | 20 | 20 |
| CSF 13 | 20 | 10 | 10 |
| CSF 14 | 10 | 10 | 10 |
| CSF 15 | 20 | 40 | 40 |
| CSF 16 | 20 | 20 | 20 |
| CSF 17 | 20 | 20 | 20 |
| CSF 18 | 30 | 40 | 40 |
| CSF 19 | 20 | 40 | 30 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barkovits, K.; Kruse, N.; Linden, A.; Tönges, L.; Pfeiffer, K.; Mollenhauer, B.; Marcus, K. Blood Contamination in CSF and Its Impact on Quantitative Analysis of Alpha-Synuclein. Cells 2020, 9, 370. https://doi.org/10.3390/cells9020370
Barkovits K, Kruse N, Linden A, Tönges L, Pfeiffer K, Mollenhauer B, Marcus K. Blood Contamination in CSF and Its Impact on Quantitative Analysis of Alpha-Synuclein. Cells. 2020; 9(2):370. https://doi.org/10.3390/cells9020370
Chicago/Turabian StyleBarkovits, Katalin, Niels Kruse, Andreas Linden, Lars Tönges, Kathy Pfeiffer, Brit Mollenhauer, and Katrin Marcus. 2020. "Blood Contamination in CSF and Its Impact on Quantitative Analysis of Alpha-Synuclein" Cells 9, no. 2: 370. https://doi.org/10.3390/cells9020370
APA StyleBarkovits, K., Kruse, N., Linden, A., Tönges, L., Pfeiffer, K., Mollenhauer, B., & Marcus, K. (2020). Blood Contamination in CSF and Its Impact on Quantitative Analysis of Alpha-Synuclein. Cells, 9(2), 370. https://doi.org/10.3390/cells9020370








