Nanomodulation of Macrophages in Multiple Sclerosis
Abstract
1. Introduction
2. Macrophages in MS
2.1. Resident vs Infiltrating Macrophages
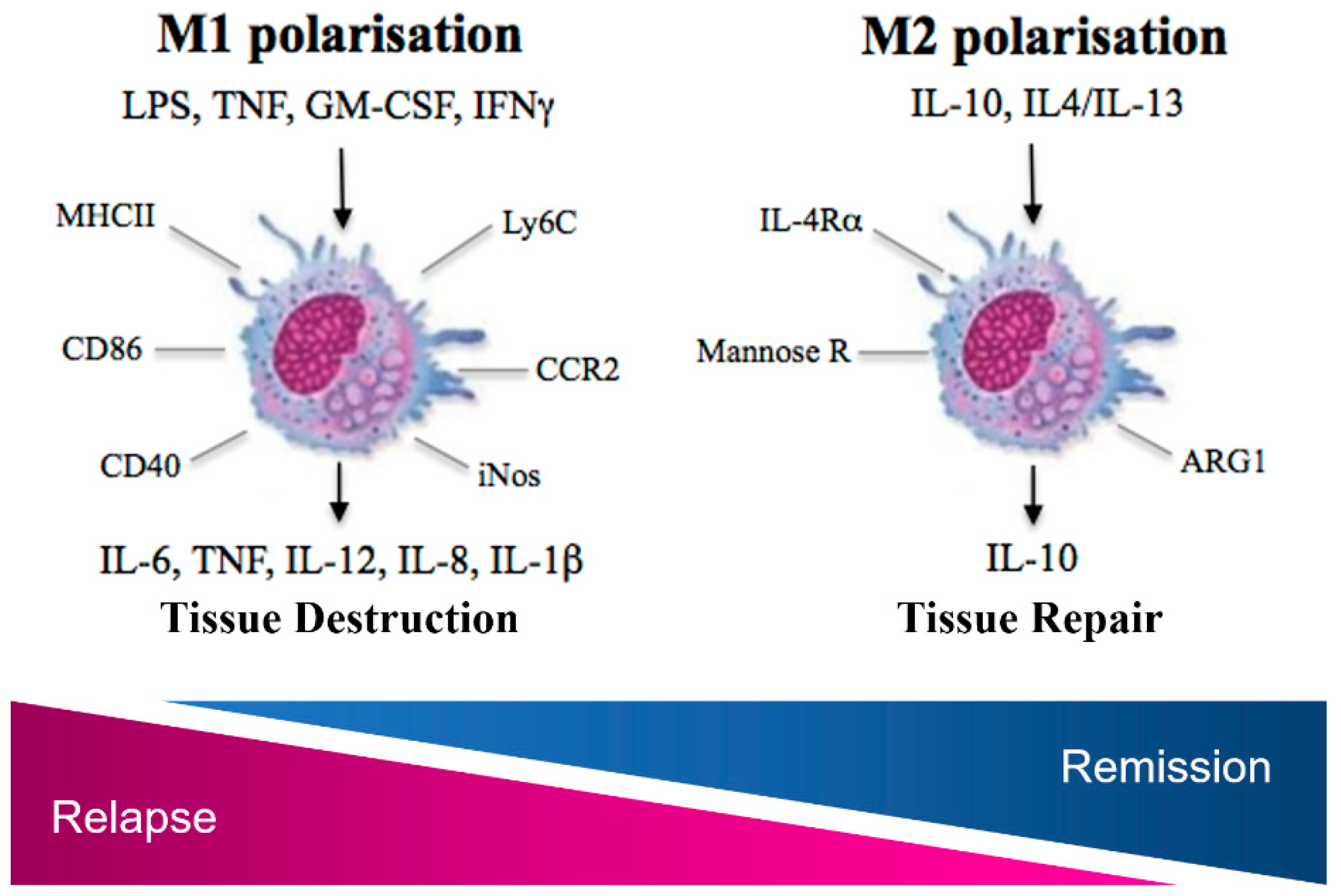
2.2. A Dual Role for Macrophages in MS
2.3. Current Therapeautics and Their Impact on Monocytes and Macrophages
2.3.1. Interferon-β
2.3.2. Glatiramer Acetate
2.3.3. Dimethyl Fumarate
2.3.4. Fingolimod
3. Nanoparticles and Microparticles in MS
3.1. Monocyte and Macrophage Depletion
3.2. NP/MP and Antigen Specific Tolerance Induction
3.3. Cortiocsteroid Delivery
3.4. NPs/MPs and Current MS Disease Modifying Therapies
3.5. NPs/MPs and Novel Drugs
4. Optimising Delivery and NP/MP Uptake in Macrophages
4.1. Size
4.2. Functionalisation
4.3. Macrophage Modulation: A Peripheral or CNS Centric Approach?
5. Concluding Remarks
Funding
Conflicts of Interest
References
- MS Prevalence: National Multiple Sclerosis Society. Available online: https://www.nationalmssociety.org/About-the-Society/MS-Prevalence (accessed on 23 October 2018).
- Pugliatti, M.; Rosati, G.; Carton, H.; Riise, T.; Drulovic, J.; Vecsei, L.; Milanov, I. The Epidemiology of Multiple Sclerosis in Europe. Eur. J. Neurol. 2006, 13, 700–722. [Google Scholar] [CrossRef] [PubMed]
- Compston, A.; Coles, A. Multiple Sclerosis. Lancet 2008, 372, 1502–1517. [Google Scholar] [CrossRef]
- Beecham, A.H.; Patsopoulos, N.A.; Xifara, D.K.; Davis, M.F.; Kemppinen, A.; Cotsapas, C.; Shah, T.S.; Spencer, C.; Booth, D.; Goris, A.; et al. Analysis of Immune-Related Loci Identifies 48 New Susceptibility Variants for Multiple Sclerosis. Nat. Genet. 2013, 45, 1353–1360. [Google Scholar] [CrossRef] [PubMed]
- Belbasis, L.; Bellou, V.; Evangelou, E.; Ioannidis, J.P.A.; Tzoulaki, I. Environmental Risk Factors and Multiple Sclerosis: An Umbrella Review of Systematic Reviews and Meta-Analyses. Lancet Neurol. 2015, 14, 263–273. [Google Scholar] [CrossRef]
- Hedström, A.K.; Åkerstedt, T.; Hillert, J.; Olsson, T.; Alfredsson, L. Shift Work at Young Age Is Associated with Increased Risk for Multiple Sclerosis. Ann. Neurol. 2011, 70, 733–741. [Google Scholar] [CrossRef] [PubMed]
- Balk, L.; Tewarie, P.; Killestein, J.; Polman, C.; Uitdehaag, B.; Petzold, A. Disease Course Heterogeneity and OCT in Multiple Sclerosis. Mult. Scler. J. 2014, 20, 1198–1206. [Google Scholar] [CrossRef]
- Lund, C.; Nakken, K.O.; Edland, A.; Celius, E.G. Multiple Sclerosis and Seizures: Incidence and Prevalence over 40 Years. Acta Neurol. Scand. 2014, 130, 368–373. [Google Scholar] [CrossRef]
- Dendrou, C.A.; Fugger, L.; Friese, M.A. Immunopathology of Multiple Sclerosis. Nat. Rev. Immunol. 2015, 15, 545–558. [Google Scholar] [CrossRef]
- McFarland, H.F.; Martin, R. Multiple Sclerosis: A Complicated Picture of Autoimmunity. Nat. Immunol. 2007, 8, 913–919. [Google Scholar] [CrossRef]
- Fletcher, J.M.; Lalor, S.J.; Sweeney, C.M.; Tubridy, N.; Mills, K.H.G. T Cells in Multiple Sclerosis and Experimental Autoimmune Encephalomyelitis. Clin. Exp. Immunol. 2010, 162, 1–11. [Google Scholar] [CrossRef]
- Kaskow, B.J.; Baecher-Allan, C. Effector T Cells in Multiple Sclerosis. Cold Spring Harb. Perspect. Med. 2018, 8, a029025. [Google Scholar] [CrossRef] [PubMed]
- Friese, M.A.; Fugger, L. Pathogenic CD8+ T Cells in Multiple Sclerosis. Ann. Neurol. 2009, 66, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Patterson, K.R.; Bar-Or, A. Reassessing B Cell Contributions in Multiple Sclerosis. Nat. Immunol. 2018, 19, 696–707. [Google Scholar] [CrossRef] [PubMed]
- Pröbstel, A.-K.; Sanderson, N.; Derfuss, T.; Pröbstel, A.-K.; Sanderson, N.S.R.; Derfuss, T. B Cells and Autoantibodies in Multiple Sclerosis. Int. J. Mol. Sci. 2015, 16, 16576–16592. [Google Scholar] [CrossRef] [PubMed]
- Mishra, M.K.; Yong, V.W. Myeloid Cells—Targets of Medication in Multiple Sclerosis. Nat. Rev. Neurol. 2016, 12, 539–551. [Google Scholar] [CrossRef] [PubMed]
- Henderson, A.P.D.; Barnett, M.H.; Parratt, J.D.E.; Prineas, J.W. Multiple Sclerosis: Distribution of Inflammatory Cells in Newly Forming Lesions. Ann. Neurol. 2009, 66, 739–753. [Google Scholar] [CrossRef] [PubMed]
- Lucchinetti, C.; Bruck, W.; Parisi, J.; Scheithauer, B.; Rodriguez, M.; Lassmann, H. Heterogeneity of Multiple Sclerosis Lesions. Ann. Neurol. 2000, 47, 707–717. [Google Scholar] [CrossRef]
- Bitsch, A.; Schuchardt, J.; Bunkowski, S.; Kuhlmann, T.; Bruck, W. Acute Axonal Injury in Multiple Sclerosis Correlation with Demyelination and Inflammatio. Brain 2000, 123, 1174–1183. [Google Scholar] [CrossRef] [PubMed]
- Frischer, J.M.; Bramow, S.; Dal-Bianco, A.; Lucchinetti, C.F.; Rauschka, H.; Schmidbauer, M.; Laursen, H.; Sorensen, P.S.; Lassmann, H. The Relation between Inflammation and Neurodegeneration in Multiple Sclerosis Brains. Brain 2009, 132, 1175–1189. [Google Scholar] [CrossRef]
- Brück, W.; Sommermeier, N.; Bergmann, M.; Zettl, U.; Goebel, H.H.; Kretzschmar, H.A.; Lassmann, H. Macrophages in Multiple Sclerosis. Immunobiology 1996, 195, 588–600. [Google Scholar] [CrossRef]
- Hill, K.; Zollinger, L.; Watt, H.; Carlson, N.; Rose, J. Inducible Nitric Oxide Synthase in Chronic Active Multiple Sclerosis Plaques: Distribution, Cellular Expression and Association with Myelin Damage. Neuroimmunology 2004, 151, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Kuhlmann, T.; Lingfeld, G.; Bitsch, A.; Schuchardt, J.; Brück, W. Acute Axonal Damage in Multiple Sclerosis Is Most Extensive in Early Disease Stages and Decreases over Time. Brain 2002, 125, 2202–2212. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, B.; Matyszak, M.K.; Esiri, M.M.; Perry, V.H. Axonal Damage in Acute Multiple Sclerosis Lesions. Brain 1997, 120, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Lassmann, H.; Bradl, M. Multiple Sclerosis: Experimental Models and Reality. Acta Neuropathol. 2017, 133, 223–244. [Google Scholar] [CrossRef] [PubMed]
- Terry, R.L.; Ifergan, I.; Miller, S.D. Experimental Autoimmune Encephalomyelitis in Mice. Methods Mol. Biol. 2016, 1304, 145–160. [Google Scholar] [CrossRef] [PubMed]
- Huseby, E.S.; Liggitt, D.; Brabb, T.; Schnabel, B.; Öhlén, C.; Goverman, J. A Pathogenic Role for Myelin-Specific CD8(+) T Cells in a Model for Multiple Sclerosis. J. Exp. Med. 2001, 194, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.; Whitaker, J.N.; Huang, Z.; Liu, D.; Coleclough, C.; Wekerle, H.; Raine, C.S. Myelin Antigen-Specific CD8+ T Cells Are Encephalitogenic and Produce Severe Disease in C57BL/6 Mice. J. Immunol. 2001, 166, 7579–7587. [Google Scholar] [CrossRef] [PubMed]
- Bjelobaba, I.; Begovic-Kupresanin, V.; Pekovic, S.; Lavrnja, I. Animal Models of Multiple Sclerosis: Focus on Experimental Autoimmune Encephalomyelitis. J. Neurosci. Res. 2018, 96, 1021–1042. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, M.A.; Carlson, T.J.; Andjelkovic, A.V.; Segal, B.M. IL-12- and IL-23-Modulated T Cells Induce Distinct Types of EAE Based on Histology, CNS Chemokine Profile, and Response to Cytokine Inhibition. J. Exp. Med. 2008, 205, 1535–1541. [Google Scholar] [CrossRef] [PubMed]
- Robinson, A.P.; Harp, C.T.; Noronha, A.; Miller, S.D. The Experimental Autoimmune Encephalomyelitis (EAE) Model of MS. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2014; Volume 122, pp. 173–189. [Google Scholar] [CrossRef]
- Teitelbaum, D.; Meshorer, A.; Hirshfeld, T.; Arnon, R.; Sela, M. Suppression of Experimental Allergic Encephalomyelitis by a Synthetic Polypeptide. Eur. J. Immunol. 1971, 1, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Yednock, T.A.; Cannon, C.; Fritz, L.C.; Sanchez-Madrid, F.; Steinman, L.; Karin, N. Prevention of Experimental Autoimmune Encephalomyelitis by Antibodies against A4βl Integrin. Nature 1992, 356, 63–66. [Google Scholar] [CrossRef] [PubMed]
- Fujino, M. Amelioration of Experimental Autoimmune Encephalomyelitis in Lewis Rats by FTY720 Treatment. J. Pharmacol. Exp. Ther. 2003, 305, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Kipp, M.; Nyamoya, S.; Hochstrasser, T.; Amor, S. Multiple Sclerosis Animal Models: A Clinical and Histopathological Perspective. Brain Pathol. 2017, 27, 123–137. [Google Scholar] [CrossRef] [PubMed]
- Committee for Medicinal Products for Human Use (CHMP). Guideline on Clinical Investigation of Medicinal Products for the Treatment of Multiple Sclerosis; CHMP/771815/2011 Rev. 2; European Medicines Agency: London, UK, 2015; p. 14. [Google Scholar]
- Polman, C.H.; Dijkstra, C.D.; Sminia, T.; Koetsier, J.C. Immunohistological Analysis of Macrophages in the Central Nervous System of Lewis Rats with Acute Experimental Allergic Encephalomyelitis. J. Neuroimmunol. 1986, 11, 215–222. [Google Scholar] [CrossRef]
- Nimmerjahn, A.; Kirchhoff, F.; Helmchen, F. Resting Microglial Cells Are Highly Dynamic Surveillants of Brain Parenchyma in Vivo. Science 2005, 308, 1314–1318. [Google Scholar] [CrossRef] [PubMed]
- Ginhoux, F.; Greter, M.; Leboeuf, M.; Nandi, S.; See, P.; Gokhan, S.; Mehler, M.F.; Conway, S.J.; Ng, L.G.; Stanley, E.R.; et al. Microglia Derive from Primitive Macrophages. Science 2010, 701, 841–845. [Google Scholar] [CrossRef] [PubMed]
- Schulz, C.; Perdiguero, E.G.; Chorro, L.; Szabo-Rogers, H.; Cagnard, N.; Kierdorf, K.; Prinz, M.; Wu, B.; Jacobsen, S.E.W.; Pollard, J.W.; et al. A Lineage of Myeloid Cells Independent of Myb and Hematopoietic Stem Cells. Science 2012, 336, 86–90. [Google Scholar] [CrossRef]
- Ajami, B.; Bennett, J.L.; Krieger, C.; Tetzlaff, W.; Rossi, F.M.V. Local Self-Renewal Can Sustain CNS Microglia Maintenance and Function throughout Adult Life. Nat. Neurosci. 2007, 10, 1538–1543. [Google Scholar] [CrossRef]
- Goldmann, T.; Wieghofer, P.; Jordão, M.J.C.; Prutek, F.; Hagemeyer, N.; Frenzel, K.; Amann, L.; Staszewski, O.; Kierdorf, K.; Krueger, M.; et al. Origin, Fate and Dynamics of Macrophages at Central Nervous System Interfaces. Nat. Immunol. 2016, 17, 797–805. [Google Scholar] [CrossRef]
- Heppner, F.L.; Greter, M.; Marino, D.; Falsig, J.; Raivich, G.; Hövelmeyer, N.; Waisman, A.; Rülicke, T.; Prinz, M.; Priller, J.; et al. Experimental Autoimmune Encephalomyelitis Repressed by Microglial Paralysis. Nat. Med. 2005, 11, 146–152. [Google Scholar] [CrossRef]
- Ponomarev, E.D.; Shriver, L.P.; Maresz, K.; Dittel, B.N. Microglial Cell Activation and Proliferation Precedes the Onset of CNS Autoimmunity. J. Neurosci. Res. 2005, 81, 374–389. [Google Scholar] [CrossRef] [PubMed]
- Ajami, B.; Bennett, J.L.; Krieger, C.; McNagny, K.M.; Rossi, F.M.V. Infiltrating Monocytes Trigger EAE Progression, but Do Not Contribute to the Resident Microglia Pool. Nat. Neurosci. 2011, 14, 1142–1150. [Google Scholar] [CrossRef] [PubMed]
- Brosnan, C.F.; Bornstein, M.B.; Bloom, B.R. The Effects of Macrophage Depletion on the Clinical and Pathologic Expression of Experimental Allergic Encephalomyelitis. J. Immunol. 1981, 126, 614–620. [Google Scholar] [PubMed]
- Huitinga, I.; van Rooijen, N.; de Groot, C.J.; Uitdehaag, B.M.; Dijkstra, C.D. Suppression of Experimental Allergic Encephalomyelitis in Lewis Rats after Elimination of Macrophages. J. Exp. Med. 1990, 172, 1025–1033. [Google Scholar] [CrossRef] [PubMed]
- Tran, E.H.; Hoekstra, K.; Van Rooijen, N.; Dijkstra, D.; Owens, T. Immune Invasion of the Central Nervous System Parenchyma and Experimental Allergic Encephalomyelitis, But Not Leukocyte Extravasation from Blood, Are Prevented in Macrophage-Depleted Mice. J. Immunol. 1998, 161, 3767–3775. [Google Scholar] [PubMed]
- Moreno, M.A.; Burns, T.; Yao, P.; Miers, L.; Pleasure, D.; Soulika, A.M. Therapeutic Depletion of Monocyte-Derived Cells Protects from Long-Term Axonal Loss in Experimental Autoimmune Encephalomyelitis. J. Neuroimmunol. 2016, 290, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Lewis, N.D.; Hill, J.D.; Juchem, K.W.; Stefanopoulos, D.E.; Modis, L.K. RNA Sequencing of Microglia and Monocyte-Derived Macrophages from Mice with Experimental Autoimmune Encephalomyelitis Illustrates a Changing Phenotype with Disease Course. J. Neuroimmunol. 2014, 277, 26–38. [Google Scholar] [CrossRef] [PubMed]
- Barnett, M.H.; Prineas, J.W. Relapsing and Remitting Multiple Sclerosis: Pathology of the Newly Forming Lesion. Ann. Neurol. 2004, 55, 458–468. [Google Scholar] [CrossRef] [PubMed]
- Howell, O.W.; Rundle, J.L.; Garg, A.; Komada, M.; Brophy, P.J.; Reynolds, R. Activated Microglia Mediate Axoglial Disruption That Contributes to Axonal Injury in Multiple Sclerosis. J. Neuropathol. Exp. Neurol. 2010, 69, 1017–1033. [Google Scholar] [CrossRef] [PubMed]
- Van Noort, J.M.; van den Elsen, P.J.; van Horssen, J.; Geurts, J.J.G.; van der Valk, P.; Amor, S. Preactive Multiple Sclerosis Lesions Offer Novel Clues for Neuroprotective Therapeutic Strategies. CNS Neurol. Disord. Drug Targets 2011, 10, 68–81. [Google Scholar] [CrossRef]
- Vogel, D.Y.S.; Vereyken, E.J.F.; Glim, J.E.; Heijnen, P.D.A.M.; Moeton, M.; van der Valk, P.; Amor, S.; Teunissen, C.E.; van Horssen, J.; Dijkstra, C.D. Macrophages in Inflammatory Multiple Sclerosis Lesions Have an Intermediate Activation Status. J. Neuroinflammation 2013, 10, 1. [Google Scholar] [CrossRef] [PubMed]
- Izikson, L.; Klein, R.S.; Charo, I.F.; Weiner, H.L.; Luster, A.D. Resistance to Experimental Autoimmune Encephalomyelitis in Mice Lacking the CC Chemokine Receptor (CCR)2. J. Exp. Med. 2000, 192, 1075–1080. [Google Scholar] [CrossRef] [PubMed]
- Fife, B.T.; Huffnagle, G.B.; Kuziel, W.A.; Karpus, W.J. CC Chemokine Receptor 2 Is Critical for Induction of Experimental Autoimmune Encephalomyelitis. J. Exp. Med. 2000, 192, 899–905. [Google Scholar] [CrossRef] [PubMed]
- Gaupp, S.; Pitt, D.; Kuziel, W.A.; Cannella, B.; Raine, C.S. Experimental Autoimmune Encephalomyelitis (EAE) in CCR2-/-Mice: Susceptibility in Multiple Strains. Am. J. Pathol. 2003, 162, 139–150. [Google Scholar] [CrossRef]
- Huang, D.; Wang, J.; Kivisakk, P.; Rollins, B.J.; Ransohoff, R.M. Absence of Monocyte Chemoattractant Protein 1 in Mice Leads to Decreased Local Macrophage Recruitment and Antigen-Specific T Helper Cell Type 1 Immune Response in Experimental Autoimmune Encephalomyelitis. J. Exp. Med. 2001, 193, 713–726. [Google Scholar] [CrossRef] [PubMed]
- Mildner, A.; Mack, M.; Schmidt, H.; Bruck, W.; Djukic, M.; Zabel, M.; Hille, A.; Priller, J.; Prinz, M. CCR2+Ly-6Chi Monocytes Are Crucial for the Effector Phase of Autoimmunity in the Central Nervous System. Brain 2009, 132, 2487–2500. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.; Taylor, P.R. Monocyte and Macrophage Heterogeneity. Nat. Rev. Immunol. 2005, 5, 953–964. [Google Scholar] [CrossRef] [PubMed]
- King, I.L.; Dickendesher, T.L.; Segal, B.M. Circulating Ly-6C+ Myeloid Precursors Migrate to the CNS and Play a Pathogenic Role during Autoimmune Demyelinating Disease. Blood 2009, 113, 3190–3197. [Google Scholar] [CrossRef] [PubMed]
- Codarri, L.; Gyülvészi, G.; Tosevski, V.; Hesske, L.; Fontana, A.; Magnenat, L.; Suter, T.; Becher, B. RORγt Drives Production of the Cytokine GM-CSF in Helper T Cells, Which Is Essential for the Effector Phase of Autoimmune Neuroinflammation. Nat. Immunol. 2011, 12, 560–567. [Google Scholar] [CrossRef] [PubMed]
- McQualter, J.L.; Darwiche, R.; Ewing, C.; Onuki, M.; Kay, T.W.; Hamilton, J.A.; Reid, H.H.; Bernard, C.C.A. Granulocyte Macrophage Colony-Stimulating Factor: A New Putative Therapeutic Target in Multiple Sclerosis. J. Exp. Med. 2001, 194, 873–882. [Google Scholar] [CrossRef]
- Croxford, A.L.; Lanzinger, M.; Hartmann, F.J.; Schreiner, B.; Mair, F.; Pelczar, P.; Clausen, B.E.; Jung, S.; Greter, M.; Becher, B. The Cytokine GM-CSF Drives the Inflammatory Signature of CCR2+ Monocytes and Licenses Autoimmunity. Immunity 2015, 43, 502–514. [Google Scholar] [CrossRef] [PubMed]
- Ziegler-Heitbrock, L.; Ancuta, P.; Crowe, S.; Dalod, M.; Grau, V.; Hart, D.N.; Leenen, P.J.M.; Liu, Y.-J.; MacPherson, G.; Randolph, G.J.; et al. Nomenclature of Monocytes and Dendritic Cells in Blood. Blood 2010, 116, e74–e80. [Google Scholar] [CrossRef] [PubMed]
- Bergh, F.T.; Dayyani, F.; Ziegler-Heitbrock, L. Impact of Type-I-Interferon on Monocyte Subsets and Their Differentiation to Dendritic Cells: An in Vivo and Ex Vivo Study in Multiple Sclerosis Patients Treated with Interferon-Beta. J. Neuroimmunol. 2004, 146, 176–188. [Google Scholar] [CrossRef]
- Chuluundorj, D.; Harding, S.A.; Abernethy, D.; La Flamme, A.C. Glatiramer Acetate Treatment Normalized the Monocyte Activation Profile in MS Patients to That of Healthy Controls. Immunol. Cell Biol. 2017, 95, 297–305. [Google Scholar] [CrossRef] [PubMed]
- Chuluundorj, D.; Harding, S.A.; Abernethy, D.; La Flamme, A.C. Expansion and Preferential Activation of the CD14+ CD16+ Monocyte Subset during Multiple Sclerosis. Immunol. Cell Biol. 2014, 92, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Ingersoll, M.; Spanbroek, R.; Lottaz, C.; Gautier, E.; Frankenberger, M.; Hoffman, R.; Lang, R.; Hannifa, M.; Collin, M.; Tacke, F.; et al. Comparison of Gene Expression Profiles between Human and Mouse Monocyte Subsets. Blood 2010, 115, e10–e19. [Google Scholar] [CrossRef]
- Simpson, J.; Newcombe, J.; Cuzner, M.; Woodroofe, M. Expression of Monocyte Chemoattractant Protein-1 and Other β-Chemokines by Resident Glia and Inflammatory Cells in Multiple Sclerosis Lesions. J. Neuroimmunol. 1998, 84, 238–249. [Google Scholar] [CrossRef]
- McManus, C.; Berman, J.W.; Brett, F.M.; Staunton, H.; Farrell, M.; Brosnan, C.F. MCP-1, MCP-2 and MCP-3 Expression in Multiple Sclerosis Lesions: An Immunohistochemical and in Situ Hybridization Study. J. Neuroimmunol. 1998, 86, 20–29. [Google Scholar] [CrossRef]
- Prins, M.; Dutta, R.; Baselmans, B.; Brevé, J.J.P.; Bol, J.G.J.M.; Deckard, S.A.; van der Valk, P.; Amor, S.; Trapp, B.D.; de Vries, H.E.; et al. Discrepancy in CCL2 and CCR2 Expression in White versus Grey Matter Hippocampal Lesions of Multiple Sclerosis Patients. Acta Neuropathol. Commun. 2014, 2, 98. [Google Scholar] [CrossRef]
- Van Der Voorn, P.; Tekstra, J.; Beelen, R.H.J.; Tensen, C.P.; Van Der Valk, P.; De Groot, C.J.A. Expression of MCP-1 by Reactive Astrocytes in Demyelinating Multiple Sclerosis Lesions. Am. J. Pathol. 1999, 154, 45–51. [Google Scholar] [CrossRef]
- Sorensen, T.L.; Ransohoff, R.M.; Strieter, R.M.; Sellebjerg, F. Chemokine CCL2 and Chemokine Receptor CCR2 in Early Active Multiple Sclerosis. Eur. J. Neurol. 2004, 11, 445–449. [Google Scholar] [CrossRef] [PubMed]
- Mahad, D.J.; Ransohoff, R.M. The Role of MCP-1 (CCL2) and CCR2 in Multiple Sclerosis and Experimental Autoimmune Encephalomyelitis (EAE). Semin. Immunol. 2003, 15, 23–32. [Google Scholar] [CrossRef]
- Bose, S.; Cho, J. Role of Chemokine CCL2 and Its Receptor CCR2 in Neurodegenerative Diseases. Arch. Pharm. Res. 2013, 36, 1039–1050. [Google Scholar] [CrossRef] [PubMed]
- Lagumersindez-Denis, N.; Wrzos, C.; Mack, M.; Winkler, A.; van der Meer, F.; Reinert, M.C.; Hollasch, H.; Flach, A.; Brühl, H.; Cullen, E.; et al. Differential Contribution of Immune Effector Mechanisms to Cortical Demyelination in Multiple Sclerosis. Acta Neuropathol. 2017, 134, 15–34. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Sica, A.; Sozzani, S.; Allavena, P.; Vecchi, A.; Locati, M. The Chemokine System in Diverse Forms of Macrophage Activation and Polarization. Trends Immunol. 2004, 25, 677–686. [Google Scholar] [CrossRef] [PubMed]
- Girvin, A.M.; Dal Canto, M.C.; Miller, S.D. CD40/CD40L Interaction Is Essential for the Induction of EAE in the Absence of CD28-Mediated Co-Stimulation. J. Autoimmun. 2002, 18, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Bartholomäus, I.; Kawakami, N.; Odoardi, F.; Schläger, C.; Miljkovic, D.; Ellwart, J.W.; Klinkert, W.E.F.; Flügel-Koch, C.; Issekutz, T.B.; Wekerle, H.; et al. Effector T Cell Interactions with Meningeal Vascular Structures in Nascent Autoimmune CNS Lesions. Nature 2009, 462, 94–98. [Google Scholar] [CrossRef]
- Jiang, Z.; Jiang, J.X.; Zhang, G.X. Macrophages: A Double-Edged Sword in Experimental Autoimmune Encephalomyelitis. Immunol. Lett. 2014, 160, 1722. [Google Scholar] [CrossRef]
- Kornek, B.; Storch, M.K.; Weissert, R.; Wallstroem, E.; Stefferl, A.; Olsson, T.; Linington, C.; Schmidbauer, M.; Lassmann, H. Multiple Sclerosis and Chronic Autoimmune Encephalomyelitis: A Comparative Quantitative Study of Axonal Injury in Active, Inactive, and Remyelinated Lesions. Am. J. Pathol. 2000, 157, 267–276. [Google Scholar] [CrossRef]
- Nikić, I.; Merkler, D.; Sorbara, C.; Brinkoetter, M.; Kreutzfeldt, M.; Bareyre, F.M.; Brück, W.; Bishop, D.; Misgeld, T.; Kerschensteiner, M. A Reversible Form of Axon Damage in Experimental Autoimmune Encephalomyelitis and Multiple Sclerosis. Nat. Med. 2011, 17, 495–499. [Google Scholar] [CrossRef]
- Yamasaki, R.; Lu, H.; Butovsky, O.; Ohno, N.; Rietsch, A.M.; Cialic, R.; Wu, P.; Doykan, C.; Lin, J.; Cotleur, A.C.; et al. Differential Roles of Microglia and Monocytes in the Inflamed Central Nervous System. J. Exp. Med. 2014, 211, 1533–1549. [Google Scholar] [CrossRef] [PubMed]
- López-Moratalla, N.; González, Á.; Aymerich, M.; Lopez-Zabalza, M.; Pio, R.; de Castro, P.; Santiago, E. Monocyte Inducible Nitric Oxide Synthase in Multiple Sclerosis: Regulatory Role of Nitric Oxide. Nitric Oxide 1997, 1, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Bö, L.; Dawson, T.M.; Wesselingh, S.; Möurk, S.; Choi, S.; Kong, P.A.; Hanley, D.; Trapp, B.D. Induction of Nitric Oxide Synthase in Demyelinating Regions of Multiple Sclerosis Brains. Ann. Neurol. 1994, 36, 778–786. [Google Scholar] [CrossRef] [PubMed]
- Locatelli, G.; Theodorou, D.; Kendirli, A.; Joana, M.; Jordão, C.; Staszewski, O.; Phulphagar, K.; Cantuti-castelvetri, L.; Dagkalis, A.; Bessis, A.; et al. Mononuclear Phagocytes Locally Specify and Adapt Their Phenotype in a Multiple Sclerosis Model. Nat. Neurosci. 2018, 21, 1196–1208. [Google Scholar] [CrossRef] [PubMed]
- Giles, D.A.; Washnock-Schmid, J.M.; Duncker, P.C.; Dahlawi, S.; Ponath, G.; Pitt, D.; Segal, B.M. Myeloid Cell Plasticity in the Evolution of Central Nervous System Autoimmunity. Ann. Neurol. 2018, 83, 131–141. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S. Alternative Activation of Macrophages. Nat. Rev. Immunol. 2003, 3, 23–35. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, M.; Torrance, D.; Picha, K.; Mohler, K. Analysis of Cytokine MRNA Expression in the Central Nervous System of Mice with Experimental Autoimmune Encephalomyelitis Reveals That IL-10 MRNA Expression Correlates with Recovery. J. Immunol. 1992, 149, 2496–2505. [Google Scholar] [PubMed]
- Jander, S.; Pohl, J.; D’Urso, D.; Gillen, C.; Stoll, G. Time Course and Cellular Localization of Interleukin-10 MRNA and Protein Expression in Autoimmune Inflammation of the Rat Central Nervous System. Am. J. Pathol. 1998, 152, 975–982. [Google Scholar] [PubMed]
- Payne, N.L.; Sun, G.; McDonald, C.; Moussa, L.; Emerson-Webber, A.; Loisel-Meyer, S.; Medin, J.A.; Siatskas, C.; Bernard, C.C. Human Adipose-Derived Mesenchymal Stem Cells Engineered to Secrete IL-10 Inhibit APC Function and Limit CNS Autoimmunity. Brain. Behav. Immun. 2013, 30, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Fiorentino, D.F.; Zlotnik, A.; Vieira, P.; Mosmann, T.R.; Howard, M.; Moore, K.W.; O’Garra, A. IL-10 Acts on the Antigen-Presenting Cell to Inhibit Cytokine Production by Th1 Cells. J. Immunol. 1991, 146, 3444–3451. [Google Scholar] [PubMed]
- O’Garra, A.; Vieira, P.L.; Vieira, P.; Goldfeld, A.E. IL-10–producing and Naturally Occurring CD4+ Tregs: Limiting Collateral Damage. J. Clin. Invest. 2004, 114, 1372–1378. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, A.D.; Passos dos Santos, R.; Zarruk, J.G.; Salmon, C.K.; Kroner, A.; David, S. Arginase-1 Is Expressed Exclusively by Infiltrating Myeloid Cells in CNS Injury and Disease. Brain. Behav. Immun. 2016, 56, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Boven, L.A.; Van Meurs, M.; Van Zwam, M.; Wierenga-Wolf, A.; Hintzen, R.Q.; Boot, R.G.; Aerts, J.M.; Amor, S.; Nieuwenhuis, E.E.; Laman, J.D. Myelin-Laden Macrophages Are Anti-Inflammatory, Consistent with Foam Cells in Multiple Sclerosis. Brain 2006, 129, 517–526. [Google Scholar] [CrossRef] [PubMed]
- Hulshof, S.; Montagne, L.; De Groot, C.J.A.; Van Der Valk, P. Cellular Localization and Expression Patterns of Interleukin-10, Interleukin-4, and Their Receptors in Multiple Sclerosis Lesions. Glia 2002, 38, 24–35. [Google Scholar] [CrossRef] [PubMed]
- Tierney, J.B.; Kharkrang, M.; La Flamme, A.C. Type II-Activated Macrophages Suppress the Development of Experimental Autoimmune Encephalomyelitis. Immunol. Cell Biol. 2009, 87, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.-R.; Milovanović, M.; Allan, D.; Niedbala, W.; Besnard, A.-G.; Fukada, S.Y.; Alves-Filho, J.C.; Togbe, D.; Goodyear, C.S.; Linington, C.; et al. IL-33 Attenuates EAE by Suppressing IL-17 and IFN-γ Production and Inducing Alternatively Activated Macrophages. Eur. J. Immunol. 2012, 42, 1804–1814. [Google Scholar] [CrossRef] [PubMed]
- Mikita, J.; Dubourdieu-Cassagno, N.; Deloire, M.S.; Vekris, A.; Biran, M.; Raffard, G.; Brochet, B.; Canron, M.H.; Franconi, J.M.; Boiziau, C.; et al. Altered M1/M2 Activation Patterns of Monocytes in Severe Relapsing Experimental Rat Model of Multiple Sclerosis. Amelioration of Clinical Status by M2 Activated Monocyte Administration. Mult. Scler. J. 2011, 17, 2–15. [Google Scholar] [CrossRef] [PubMed]
- Kotter, M.R.; Zhao, C.; Van Rooijen, N.; Franklin, R.J.M. Macrophage-Depletion Induced Impairment of Experimental CNS Remyelination Is Associated with a Reduced Oligodendrocyte Progenitor Cell Response and Altered Growth Factor Expression. Neurobiol. Dis. 2005, 18, 166–175. [Google Scholar] [CrossRef]
- Miron, V.E.; Boyd, A.; Zhao, J.W.; Yuen, T.J.; Ruckh, J.M.; Shadrach, J.L.; Van Wijngaarden, P.; Wagers, A.J.; Williams, A.; Franklin, R.J.M.; et al. M2 Microglia and Macrophages Drive Oligodendrocyte Differentiation during CNS Remyelination. Nat. Neurosci. 2013, 16, 1211–1218. [Google Scholar] [CrossRef]
- Mokhtarian, F.; Shi, Y.; Shirazian, D.; Morgante, L.; Miller, A.; Grob, D. Defective Production of Anti-Inflammatory Cytokine, TGF-Beta by T Cell Lines of Patients with Active Multiple Sclerosis. J. Immunol. 1994, 152, 6003–6010. [Google Scholar]
- Carrieri, P.B.; Provitera, V.; Bruno, R.; Perrella, M.; Tartaglia, G.; Busto, A.; Perrella, O. Possible Role of Transforming Growth Factor-Beta in Relapsing-Remitting Multiple Sclerosis. Neurol. Res. 1997, 19, 599–600. [Google Scholar] [CrossRef] [PubMed]
- Raine, C.S. Multiple Sclerosis: The Resolving Lesion Revealed. J. Neuroimmunol. 2017, 304, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Wingerchuk, D.M.; Carter, J.L. Multiple Sclerosis: Current and Emerging Disease-Modifying Therapies and Treatment Strategies. Mayo Clin. Proc. 2014, 89, 225–240. [Google Scholar] [CrossRef] [PubMed]
- Cross, A.H.; Naismith, R.T. Established and Novel Disease-Modifying Treatments in Multiple Sclerosis. J. Intern. Med. 2014, 275, 350–363. [Google Scholar] [CrossRef] [PubMed]
- Polman, C.H.; O’Connor, P.W.; Havrdova, E.; Hutchinson, M.; Kappos, L.; Miller, D.H.; Phillips, J.T.; Lublin, F.D.; Giovannoni, G.; Wajgt, A.; et al. A Randomized, Placebo-Controlled Trial of Natalizumab for Relapsing Multiple Sclerosis. N. Engl. J. Med. 2006, 354, 899–910. [Google Scholar] [CrossRef] [PubMed]
- Coles, A.J.; Twyman, C.L.; Arnold, D.L.; Cohen, J.A.; Confavreux, C.; Fox, E.J.; Hartung, H.-P.; Havrdova, E.; Selmaj, K.W.; Weiner, H.L.; et al. Alemtuzumab for Patients with Relapsing Multiple Sclerosis after Disease-Modifying Therapy: A Randomised Controlled Phase 3 Trial. Lancet (London, England) 2012, 380, 1829–1839. [Google Scholar] [CrossRef]
- US Food and Drug Administration. Drug Safety and Availability—FDA Working with Manufacturers to Withdraw Zinbryta from the Market in the United States. US Department of Health and Human Services. Available online: https://www.fda.gov/drugs/drug-safety-and-availability/fda-working-manufacturers-withdraw-zinbryta-market-united-states (accessed on 10 April 2019).
- O’Connor, P.; Filippi, M.; Arnason, B.; Comi, G.; Cook, S.; Goodin, D.; Hartung, H.-P.; Jeffery, D.; Kappos, L.; Boateng, F.; et al. 250 Mg or 500 Mg Interferon Beta-1b versus 20 Mg Glatiramer Acetate in Relapsing-Remitting Multiple Sclerosis: A Prospective, Randomised, Multicentre Study. Lancet Neurol. 2009, 8, 889–897. [Google Scholar] [CrossRef]
- Dhib-Jalbut, S.; Marks, S. Interferon-Beta Mechanisms of Action in Multiple Sclerosis. Neurology 2010, 74 (Suppl. 1), S17–S24. [Google Scholar] [CrossRef]
- Guo, B.; Chang, E.Y.; Cheng, G. The Type I IFN Induction Pathway Constrains Th17-Mediated Autoimmune Inflammation in Mice. J. Clin. Invest. 2008, 118, 1680–1690. [Google Scholar] [CrossRef] [PubMed]
- Shinohara, M.L.; Kim, J.-H.; Garcia, V.A.; Cantor, H. Engagement of the Type I Interferon Receptor on Dendritic Cells Inhibits T Helper 17 Cell Development: Role of Intracellular Osteopontin. Immunity 2008, 29, 68–78. [Google Scholar] [CrossRef]
- Liu, B.-S.; Janssen, H.L.A.; Boonstra, A. Type I and III Interferons Enhance IL-10R Expression on Human Monocytes and Macrophages, Resulting in IL-10-Mediated Suppression of TLR-Induced IL-12. Eur. J. Immunol. 2012, 42, 2431–2440. [Google Scholar] [CrossRef] [PubMed]
- PRISMS (Prevention of Relapses and Disability by Interferon Beta-1a Subcutaneously in Multiple Sclerosis) Study Group. Randomised Double-Blind Placebo-Controlled Study of Interferon Beta-1a in Relapsing/Remitting Multiple Sclerosis. Lancet (London, England) 1998, 352, 1498–1504. [Google Scholar]
- Duda, P.W.; Schmied, M.C.; Cook, S.L.; Krieger, J.I.; Hafler, D.A. Glatiramer Acetate (Copaxone®) Induces Degenerate, Th2-Polarized Immune Responses in Patients with Multiple Sclerosis. J. Clin. Investig. 2000, 105, 967–976. [Google Scholar] [CrossRef] [PubMed]
- Gran, B.; Tranquill, L.R.; Chen, M.; Bielekova, B.; Zhou, W.; Dhib-Jalbut, S.; Martin, R. Mechanisms of Immunomodulation by Glatiramer Acetate. Neurology 2000, 55, 1704–1714. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Ifergan, I.; Antel, J.P.; Seguin, R.; Duddy, M.; Lapierre, Y.; Jalili, F.; Bar-Or, A. Type 2 Monocyte and Microglia Differentiation Mediated by Glatiramer Acetate Therapy in Patients with Multiple Sclerosis. J. Immunol. 2004, 172, 7144–7153. [Google Scholar] [CrossRef] [PubMed]
- Burger, D.; Molnarfi, N.; Weber, M.S.; Brandt, K.J.; Benkhoucha, M.; Gruaz, L.; Chofflon, M.; Zamvil, S.S.; Lalive, P.H. Glatiramer Acetate Increases IL-1 Receptor Antagonist but Decreases T Cell-Induced IL-1 in Human Monocytes and Multiple Sclerosis. Proc. Natl. Acad. Sci. USA 2009, 106, 4355–4359. [Google Scholar] [CrossRef] [PubMed]
- Weber, M.S.; Starck, M.; Wagenpfeil, S.; Meinl, E.; Hohlfeld, R.; Farina, C. Multiple Sclerosis: Glatiramer Acetate Inhibits Monocyte Reactivity in Vitro and in Vivo. Brain 2004, 127, 1370–1378. [Google Scholar] [CrossRef] [PubMed]
- Pul, R.; Moharregh-Khiabani, D.; Škuljec, J.; Skripuletz, T.; Garde, N.; Voß, E.V.; Stangel, M. Glatiramer Acetate Modulates TNF-α and IL-10 Secretion in Microglia and Promotes Their Phagocytic Activity. J. Neuroimmune Pharm. 2011, 6, 381–388. [Google Scholar] [CrossRef]
- Pul, R.; Morbiducci, F.; Škuljec, J.; Skripuletz, T.; Singh, V.; Diederichs, U.; Garde, N.; Voss, E.V.; Trebst, C.; Stangel, M. Glatiramer Acetate Increases Phagocytic Activity of Human Monocytes In Vitro and in Multiple Sclerosis Patients. PLoS ONE 2012, 7. [Google Scholar] [CrossRef]
- Mindur, J.E.; Ito, N.; Dhib-Jalbut, S.; Ito, K. Early Treatment with Anti-VLA-4 MAb Can Prevent the Infiltration and/or Development of Pathogenic CD11b+CD4+ T Cells in the CNS during Progressive EAE. PLoS ONE 2014, 9, e99068. [Google Scholar] [CrossRef]
- Michell-Robinson, M.A.; Moore, C.S.; Healy, L.M.; Osso, L.A.; Zorko, N.; Grouza, V.; Touil, H.; Poliquin-Lasnier, L.; Trudelle, A.M.; Giacomini, P.S.; et al. Effects of Fumarates on Circulating and CNS Myeloid Cells in Multiple Sclerosis. Ann. Clin. Transl. Neurol. 2016, 3, 27–41. [Google Scholar] [CrossRef] [PubMed]
- Qin, C.; Fan, W.-H.; Liu, Q.; Shang, K.; Murugan, M.; Wu, L.-J.; Wang, W.; Tian, D.-S. Fingolimod Protects Against Ischemic White Matter Damage by Modulating Microglia Toward M2 Polarization via STAT3 Pathway. Stroke 2017, 48, 3336–3346. [Google Scholar] [CrossRef] [PubMed]
- Luessi, F.; Kraus, S.; Trinschek, B.; Lerch, S.; Ploen, R.; Paterka, M.; Roberg, T.; Poisa-Beiro, L.; Klotz, L.; Wiendl, H.; et al. FTY720 (Fingolimod) Treatment Tips the Balance towards Less Immunogenic Antigen-Presenting Cells in Patients with Multiple Sclerosis. Mult. Scler. J. 2015, 21, 1811–1822. [Google Scholar] [CrossRef] [PubMed]
- Thomas, K.; Sehr, T.; Proschmann, U.; Rodriguez-Leal, F.A.; Haase, R.; Ziemssen, T. Fingolimod Additionally Acts as Immunomodulator Focused on the Innate Immune System beyond Its Prominent Effects on Lymphocyte Recirculation. J. Neuroinflamm. 2017, 14, 41. [Google Scholar] [CrossRef] [PubMed]
- Di Dario, M.; Colombo, E.; Govi, C.; De Feo, D.; Messina, M.J.; Romeo, M.; Sangalli, F.; Moiola, L.; Rodegher, M.; Martino, G.; et al. Myeloid Cells as Target of Fingolimod Action in Multiple Sclerosis. Neurol.-Neuroimmunol. Neuroinflamm. 2015, 2, e157. [Google Scholar] [CrossRef]
- Cohen, J.A.; Barkhof, F.; Comi, G.; Hartung, H.-P.; Khatri, B.O.; Montalban, X.; Pelletier, J.; Capra, R.; Gallo, P.; Izquierdo, G.; et al. Oral Fingolimod or Intramuscular Interferon for Relapsing Multiple Sclerosis. N. Engl. J. Med. 2010, 362, 402–415. [Google Scholar] [CrossRef]
- O’Connor, P.; Wolinsky, J.S.; Confavreux, C.; Comi, G.; Kappos, L.; Olsson, T.P.; Benzerdjeb, H.; Truffinet, P.; Wang, L.; Miller, A.; et al. Randomized Trial of Oral Teriflunomide for Relapsing Multiple Sclerosis. N. Engl. J. Med. 2011, 365, 1293–1303. [Google Scholar] [CrossRef]
- Schilling, S.; Goelz, S.; Linker, R.; Luehder, F.; Gold, R. Fumaric Acid Esters Are Effective in Chronic Experimental Autoimmune Encephalomyelitis and Suppress Macrophage Infiltration. Clin. Exp. Immunol. 2006, 145, 101–107. [Google Scholar] [CrossRef]
- Parodi, B.; Rossi, S.; Morando, S.; Cordano, C.; Bragoni, A.; Motta, C.; Usai, C.; Wipke, B.T.; Scannevin, R.H.; Mancardi, G.L.; et al. Fumarates Modulate Microglia Activation through a Novel HCAR2 Signaling Pathway and Rescue Synaptic Dysregulation in Inflamed CNS. Acta Neuropathol. 2015, 130, 279–295. [Google Scholar] [CrossRef]
- Kornberg, M.D.; Bhargava, P.; Kim, P.M.; Putluri, V.; Snowman, A.M.; Putluri, N.; Calabresi, P.A.; Snyder, S.H. Dimethyl Fumarate Targets GAPDH and Aerobic Glycolysis to Modulate Immunity. Science 2018, 360, 449–453. [Google Scholar] [CrossRef]
- Schulze-Topphoff, U.; Varrin-Doyer, M.; Pekarek, K.; Spencer, C.M.; Shetty, A.; Sagan, S.A.; Cree, B.A.C.; Sobel, R.A.; Wipke, B.T.; Steinman, L.; et al. Dimethyl Fumarate Treatment Induces Adaptive and Innate Immune Modulation Independent of Nrf2. Proc. Natl. Acad. Sci. USA 2016, 113, 4777–4782. [Google Scholar] [CrossRef] [PubMed]
- Han, R.; Xiao, J.; Zhai, H.; Hao, J. Dimethyl Fumarate Attenuates Experimental Autoimmune Neuritis through the Nuclear Factor Erythroid-Derived 2-Related Factor 2/Hemoxygenase-1 Pathway by Altering the Balance of M1/M2 Macrophages. J. Neuroinflamm. 2016, 13, 97. [Google Scholar] [CrossRef] [PubMed]
- Gold, R.; Kappos, L.; Arnold, D.L.; Bar-Or, A.; Giovannoni, G.; Selmaj, K.; Tornatore, C.; Sweetser, M.T.; Yang, M.; Sheikh, S.I.; et al. Placebo-Controlled Phase 3 Study of Oral BG-12 for Relapsing Multiple Sclerosis. N. Engl. J. Med. 2012, 367, 1098–1107. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, C.J.; Kutz, C.; Dix, A.; Boster, A.; Sanossian, N.; Kaplan, J. Intracerebral Haemorrhage during Alemtuzumab Administration. Lancet. Neurol. 2019, 18, 329–331. [Google Scholar] [CrossRef]
- Fox, E.J. Mechanism of Action of Mitoxantrone. Neurology 2004, 63 (12 Suppl. 6), S15–S18. [Google Scholar] [CrossRef] [PubMed]
- Kopadze, T.; Dehmel, T.; Hartung, H.-P.; Stüve, O.; Kieseier, B.C. Inhibition by Mitoxantrone of In Vitro Migration of Immunocompetent Cells. Arch. Neurol. 2006, 63, 1572. [Google Scholar] [CrossRef] [PubMed]
- Mitoxantrone in Progressive Multiple Sclerosis: A Placebo-Controlled, Double-Blind, Randomised, Multicentre Trial. Lancet 2002, 360, 2018–2025. [CrossRef]
- Montalban, X.; Hauser, S.L.; Kappos, L.; Arnold, D.L.; Bar-Or, A.; Comi, G.; de Seze, J.; Giovannoni, G.; Hartung, H.-P.; Hemmer, B.; et al. Ocrelizumab versus Placebo in Primary Progressive Multiple Sclerosis. N. Engl. J. Med. 2017, 376, 209–220. [Google Scholar] [CrossRef]
- Guarda, G.; Braun, M.; Staehli, F.; Tardivel, A.; Mattmann, C.; Förster, I.; Farlik, M.; Decker, T.; Du Pasquier, R.A.; Romero, P.; et al. Type I Interferon Inhibits Interleukin-1 Production and Inflammasome Activation. Immunity 2011, 34, 213–223. [Google Scholar] [CrossRef]
- Comabella, M.; Imitola, J.; Weiner, H.L.; Khoury, S.J. Interferon-Beta Treatment Alters Peripheral Blood Monocytes Chemokine Production in MS Patients. J. Neuroimmunol. 2002, 126, 205–212. [Google Scholar] [CrossRef]
- Rep, M.H.; Schrijver, H.M.; van Lopik, T.; Hintzen, R.Q.; Roos, M.T.; Adèr, H.J.; Polman, C.H.; van Lier, R.A. Interferon (IFN)-Beta Treatment Enhances CD95 and Interleukin 10 Expression but Reduces Interferon-Gamma Producing T Cells in MS Patients. J. Neuroimmunol. 1999, 96, 92–100. [Google Scholar] [CrossRef]
- Ersoy, E.; Kus, C.N.S.; Sener, U.; Coker, I.; Zorlu, Y. The Effects of Interferon-Beta on Interleukin-10 in Multiple Sclerosis Patients. Eur. J. Neurol. 2005, 12, 208–211. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Milo, R.; Panitch, H.; Swoveland, P.; Bever, C.T. Glatiramer Acetate Blocks the Activation of THP-1 Cells by Interferon-γ. Eur. J. Pharmacol. 1998, 342, 303–310. [Google Scholar] [CrossRef]
- Jung, S.; Siglienti, I.; Grauer, O.; Magnus, T.; Scarlato, G.; Toyka, K. Induction of IL-10 in Rat Peritoneal Macrophages and Dendritic Cells by Glatiramer Acetate. J. Neuroimmunol. 2004, 148, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Robinson, S.; Miller, R.H. Contact with Central Nervous System Myelin Inhibits Oligodendrocyte Progenitor Maturation. Dev. Biol. 1999, 216, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Spadaro, M.; Montarolo, F.; Perga, S.; Martire, S.; Brescia, F.; Malucchi, S.; Bertolotto, A. Biological Activity of Glatiramer Acetate on Treg and Anti-Inflammatory Monocytes Persists for More than 10 Years in Responder Multiple Sclerosis Patients. Clin. Immunol. 2017, 181, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Schimrigk, S.; Brune, N.; Hellwig, K.; Lukas, C.; Bellenberg, B.; Rieks, M.; Hoffmann, V.; Pohlau, D.; Przuntek, H. Oral Fumaric Acid Esters for the Treatment of Active Multiple Sclerosis: An Open-Label, Baseline-Controlled Pilot Study. Eur. J. Neurol. 2006, 13, 604–610. [Google Scholar] [CrossRef] [PubMed]
- Linker, R.A.; Lee, D.; Ryan, S.; van Dam, A.; Conrad, R.; Bista, P.; Zeng, W.; Hronowsky, X.; Buko, A.; Chollate, S.; et al. Fumaric Acid Esters Exert Neuroprotective Effects in Neuroinflammation via Activation of the Nrf2 Antioxidant Pathway. Brain 2011, 134, 678–692. [Google Scholar] [CrossRef]
- McGuire, V.A.; Ruiz-Zorrilla Diez, T.; Emmerich, C.H.; Strickson, S.; Ritorto, M.S.; Sutavani, R.V.; Weiβ, A.; Houslay, K.F.; Knebel, A.; Meakin, P.J.; et al. Dimethyl Fumarate Blocks Pro-Inflammatory Cytokine Production via Inhibition of TLR Induced M1 and K63 Ubiquitin Chain Formation. Sci. Rep. 2016, 6, 31159. [Google Scholar] [CrossRef]
- Diebold, M.; Sievers, C.; Bantug, G.; Sanderson, N.; Kappos, L.; Kuhle, J.; Lindberg, R.L.P.; Derfuss, T. Dimethyl Fumarate Influences Innate and Adaptive Immunity in Multiple Sclerosis. J. Autoimmun. 2018, 86, 39–50. [Google Scholar] [CrossRef]
- Lim, J.L.; van der Pol, S.M.A.; Di Dio, F.; van het Hof, B.; Kooij, G.; de Vries, H.E.; van Horssen, J. Protective Effects of Monomethyl Fumarate at the Inflamed Blood–brain Barrier. Microvasc. Res. 2016, 105, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Mazzola, M.A.; Raheja, R.; Regev, K.; Beynon, V.; von Glehn, F.; Paul, A.; Pierre, I.; Kivisakk, P.; Weiner, H.L.; Gandhi, R. Monomethyl Fumarate Treatment Impairs Maturation of Human Myeloid Dendritic Cells and Their Ability to Activate T Cells. Mult. Scler. J. 2019, 25, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Angiari, S.; O’Neill, L.A. Dimethyl Fumarate: Targeting Glycolysis to Treat MS. Cell Res. 2018, 28, 613–615. [Google Scholar] [CrossRef] [PubMed]
- Klotz, L.; Havla, J.; Schwab, N.; Hohlfeld, R.; Barnett, M.; Reddel, S.; Wiendl, H. Risks and Risk Management in Modern Multiple Sclerosis Immunotherapeutic Treatment. Ther. Adv. Neurol. Disord. 2019, 12, 1756286419836571. [Google Scholar] [CrossRef] [PubMed]
- Mundargi, R.C.; Babu, V.R.; Rangaswamy, V.; Patel, P.; Aminabhavi, T.M. Nano/Micro Technologies for Delivering Macromolecular Therapeutics Using Poly(d,l-Lactide-Co-Glycolide) and Its Derivatives. J. Control. Release 2008, 125, 193–209. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Talekar, M.; Raikar, A.; Amiji, M. Macrophage-Targeted Delivery Systems for Nucleic Acid Therapy of Inflammatory Diseases. J. Control. Release 2014, 190, 515–530. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Bi, J.; Yi, H.; Fan, T.; Ruan, Q.; Cai, L.; Chen, Y.H.; Wan, X. Silencing C-Rel in Macrophages Dampens Th1 and Th17 Immune Responses and Alleviates Experimental Autoimmune Encephalomyelitis in Mice. Immunol. Cell Biol. 2017, 95, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Montes-Cobos, E.; Ring, S.; Fischer, H.J.; Heck, J.; Strauß, J.; Schwaninger, M.; Reichardt, S.D.; Feldmann, C.; Lühder, F.; Reichardt, H.M. Targeted Delivery of Glucocorticoids to Macrophages in a Mouse Model of Multiple Sclerosis Using Inorganic-Organic Hybrid Nanoparticles. J. Control. Release 2017, 245, 157–169. [Google Scholar] [CrossRef]
- Schmidt, J.; Metselaar, J.M.; Wauben, M.H.M.; Toyka, K.V.; Storm, G.; Gold, R. Drug Targeting by Long-Circulating Liposomal Glucocorticosteroids Increases Therapeutic Efficacy in a Model of Multiple Sclerosis. Brain 2003, 126, 1895–1904. [Google Scholar] [CrossRef]
- Linker, R.A.; Weller, C.; Lühder, F.; Mohr, A.; Schmidt, J.; Knauth, M.; Metselaar, J.M.; Gold, R. Liposomal Glucocorticosteroids in Treatment of Chronic Autoimmune Demyelination: Long-Term Protective Effects and Enhanced Efficacy of Methylprednisolone Formulations. Exp. Neurol. 2008, 211, 397–406. [Google Scholar] [CrossRef]
- Turjeman, K.; Bavli, Y.; Kizelsztein, P.; Schilt, Y.; Allon, N.; Katzir, T.B.; Sasson, E.; Raviv, U.; Ovadia, H.; Barenholz, Y. Nano-Drugs Based on Nano Sterically Stabilized Liposomes for the Treatment of Inflammatory Neurodegenerative Diseases. PLoS ONE 2015, 10, e0130442. [Google Scholar] [CrossRef] [PubMed]
- Gaillard, P.J.; Appeldoorn, C.C.M.; Rip, J.; Dorland, R.; van der Pol, S.M.A.; Kooij, G.; de Vries, H.E.; Reijerkerk, A. Enhanced Brain Delivery of Liposomal Methylprednisolone Improved Therapeutic Efficacy in a Model of Neuroinflammation. J. Control. Release 2012, 164, 364–369. [Google Scholar] [CrossRef] [PubMed]
- Kuo, R.; Saito, E.; Miller, S.D.; Shea, L.D. Peptide-Conjugated Nanoparticles Reduce Positive Co-Stimulatory Expression and T Cell Activity to Induce Tolerance. Mol. Ther. 2017, 25, 1676–1685. [Google Scholar] [CrossRef] [PubMed]
- Maldonado, R.A.; LaMothe, R.A.; Ferrari, J.D.; Zhang, A.-H.; Rossi, R.J.; Kolte, P.N.; Griset, A.P.; O’Neil, C.; Altreuter, D.H.; Browning, E.; et al. Polymeric Synthetic Nanoparticles for the Induction of Antigen-Specific Immunological Tolerance. Proc. Natl. Acad. Sci. USA 2015, 112, E156–E165. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, D.P.; Yap, J.W.T.; Harp, C.T.; Song, W.K.; Chen, J.; Pearson, R.M.; Miller, S.D.; Shea, L.D. An Antigen-Encapsulating Nanoparticle Platform for TH1/17 Immune Tolerance Therapy. Nanomed. Nanotechnol. Biol. Med. 2017, 13, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Pearson, R.M.; Casey, L.M.; Hughes, K.R.; Wang, L.Z.; North, M.G.; Getts, D.R.; Miller, S.D.; Shea, L.D. Controlled Delivery of Single or Multiple Antigens in Tolerogenic Nanoparticles Using Peptide-Polymer Bioconjugates. Mol. Ther. 2017, 25, 1655–1664. [Google Scholar] [CrossRef]
- Gholamzad, M.; Ebtekar, M.; Ardestani, M. Intravenous Injection of Myelin Oligodendrocyte Glycoprotein-Coated PLGA Microparticles Have Tolerogenic Effects in Experimental Autoimmune Encephalomyelitis. Iran. J. Allergy Asthma Immunol. 2017, 16, 271–281. [Google Scholar]
- Yeste, A.; Nadeau, M.; Burns, E.J.; Weiner, H.L.; Quintana, F.J. Nanoparticle-Mediated Codelivery of Myelin Antigen and a Tolerogenic Small Molecule Suppresses Experimental Autoimmune Encephalomyelitis. Proc. Natl. Acad. Sci. USA 2012, 109, 11270–11275. [Google Scholar] [CrossRef]
- Al-Ghobashy, M.A.; Elmeshad, A.N.; Abdelsalam, R.M.; Nooh, M.M.; Al-Shorbagy, M.; Laible, G. Development and Pre-Clinical Evaluation of Recombinant Human Myelin Basic Protein Nano Therapeutic Vaccine in Experimental Autoimmune Encephalomyelitis Mice Animal Model. Sci. Rep. 2017, 7, 1–16. [Google Scholar] [CrossRef]
- Cappellano, G.; Woldetsadik, A.D.; Orilieri, E.; Shivakumar, Y.; Rizzi, M.; Carniato, F.; Gigliotti, C.L.; Boggio, E.; Clemente, N.; Comi, C.; et al. Subcutaneous Inverse Vaccination with PLGA Particles Loaded with a MOG Peptide and IL-10 Decreases the Severity of Experimental Autoimmune Encephalomyelitis. Vaccine 2014, 32, 5681–5689. [Google Scholar] [CrossRef]
- Peine, K.J.; Guerau-De-Arellano, M.; Lee, P.; Kanthamneni, N.; Severin, M.; Probst, G.D.; Peng, H.; Yang, Y.; Vangundy, Z.; Papenfuss, T.L.; et al. Treatment of Experimental Autoimmune Encephalomyelitis by Codelivery of Disease Associated Peptide and Dexamethasone in Acetalated Dextran Microparticles. Mol. Pharm. 2014, 11, 828–835. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.J.; Stewart, J.M.; Drashansky, T.T.; Brusko, M.A.; Zuniga, A.N.; Lorentsen, K.J.; Keselowsky, B.G.; Avram, D. An Antigen-Specific Semi-Therapeutic Treatment with Local Delivery of Tolerogenic Factors through a Dual-Sized Microparticle System Blocks Experimental Autoimmune Encephalomyelitis. Biomaterials 2017, 143, 79–92. [Google Scholar] [CrossRef] [PubMed]
- Hunter, Z.; McCarthy, D.P.; Yap, W.T.; Harp, C.T.; Getts, D.R.; Shea, L.D.; Miller, S.D. A Biodegradable Nanoparticle Platform for the Induction of Antigen-Specific Immune Tolerance for Treatment of Autoimmune Disease. ACS Nano 2014, 8, 2148–2160. [Google Scholar] [CrossRef] [PubMed]
- Getts, D.R.; Martin, A.J.; Mccarthy, D.P.; Terry, R.L.; Hunter, Z.N.; Yap, W.T.; Getts, M.T.; Pleiss, M.; Luo, X.; King, N.J.C.; et al. Microparticles Bearing Encephalitogenic Peptides Induce T-Cell Tolerance and Ameliorate Experimental Autoimmune Encephalomyelitis. Nat. Biotechnol. 2012, 30, 1217–1224. [Google Scholar] [CrossRef] [PubMed]
- Getts, D.R.; Terry, R.L.; Getts, M.T.; Deffrasnes, C.; Müller, M.; Vreden, C.; Ashhurst, T.M.; Chami, B.; McCarthy, D.; Wu, H.; et al. Therapeutic Inflammatory Monocyte Modulation Using Immune-Modifying Microparticles. Sci. Transl. Med. 2014, 6. [Google Scholar] [CrossRef] [PubMed]
- Kishimoto, T.K.; Maldonado, R.A. Nanoparticles for the Induction of Antigen-Specific Immunological Tolerance. Front. Immunol. 2018, 9, 230. [Google Scholar] [CrossRef] [PubMed]
- LaMothe, R.A.; Kolte, P.N.; Vo, T.; Ferrari, J.D.; Gelsinger, T.C.; Wong, J.; Chan, V.T.; Ahmed, S.; Srinivasan, A.; Deitemeyer, P.; et al. Tolerogenic Nanoparticles Induce Antigen-Specific Regulatory T Cells and Provide Therapeutic Efficacy and Transferrable Tolerance against Experimental Autoimmune Encephalomyelitis. Front. Immunol. 2018, 9, 281. [Google Scholar] [CrossRef]
- Avnir, Y.; Turjeman, K.; Tulchinsky, D.; Sigal, A.; Kizelsztein, P.; Tzemach, D.; Gabizon, A.; Barenholz, Y. Fabrication Principles and Their Contribution to the Superior in Vivo Therapeutic Efficacy of Nano-Liposomes Remote Loaded with Glucocorticoids. PLoS ONE 2011, 6, e25721. [Google Scholar] [CrossRef]
- Kumar, P.; Sharma, G.; Gupta, V.; Kaur, R.; Thakur, K.; Malik, R.; Kumar, A.; Kaushal, N.; Raza, K. Preclinical Explorative Assessment of Dimethyl Fumarate-Based Biocompatible Nanolipoidal Carriers for the Management of Multiple Sclerosis. ACS Chem. Neurosci. 2018, 9, 1152–1158. [Google Scholar] [CrossRef]
- Antonazzo, I.C.; Poluzzi, E.; Forcesi, E.; Riise, T.; Bjornevik, K.; Baldin, E.; Muratori, L.; De Ponti, F.; Raschi, E. Liver Injury with Drugs Used for Multiple Sclerosis: A Contemporary Analysis of the FDA Adverse Event Reporting System. Mult. Scler. 2018, 1352458518799598. [Google Scholar] [CrossRef]
- Gadhave, D.G.; Kokare, C.R. Nanostructured Lipid Carriers Engineered for Intranasal Delivery of Teriflunomide in Multiple Sclerosis: Optimization and in Vivo Studies. Drug Dev. Ind. Pharm. 2019, 45, 839–851. [Google Scholar] [CrossRef] [PubMed]
- Rittchen, S.; Boyd, A.; Burns, A.; Park, J.; Fahmy, T.M.; Metcalfe, S.; Williams, A. Myelin Repair in Vivo Is Increased by Targeting Oligodendrocyte Precursor Cells with Nanoparticles Encapsulating Leukaemia Inhibitory Factor (LIF). Biomaterials 2015, 56, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Youssef, A.E.H.; Dief, A.E.; El Azhary, N.M.; Abdelmonsif, D.A.; El-fetiany, O.S. LINGO-1 SiRNA Nanoparticles Promote Central Remyelination in Ethidium Bromide-Induced Demyelination in Rats. J. Physiol. Biochem. 2019, 75, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Tran, J.Q.; Rana, J.; Barkhof, F.; Melamed, I.; Gevorkyan, H.; Wattjes, M.P.; de Jong, R.; Brosofsky, K.; Ray, S.; Xu, L.; et al. Randomized Phase I Trials of the Safety/Tolerability of Anti-LINGO-1 Monoclonal Antibody BIIB033. Neurol. Neuroimmunol. Neuroinflamm. 2014, 1, e18. [Google Scholar] [CrossRef] [PubMed]
- Mellion, M.; Edwards, K.R.; Hupperts, R.; Drulović, J.; Montalban, X.; Hartung, H.-P.; Brochet, B.; Calabresi, P.A.; Rudick, R.; Ibrahim, A.; et al. Efficacy Results from the Phase 2b SYNERGY Study: Treatment of Disabling Multiple Sclerosis with the Anti-LINGO-1 Monoclonal Antibody Opicinumab (S33.004). Neurology 2017, 88 (16 Supplement), S33.004. [Google Scholar]
- Eitan, E.; Hutchison, E.R.; Greig, N.H.; Tweedie, D.; Celik, H.; Ghosh, S.; Fishbein, K.W.; Spencer, R.G.; Sasaki, C.Y.; Ghosh, P.; et al. Combination Therapy with Lenalidomide and Nanoceria Ameliorates CNS Autoimmunity. Exp. Neurol. 2015, 273, 151–160. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.; Metselaar, J.; Ben, L.-H.; Cravens, P.D.; Singh, M.P.; Frohman, E.M.; Eagar, T.N.; Racke, M.K.; Kieseier, B.C.; Stüve, O. PEG Minocycline-Liposomes Ameliorate CNS Autoimmune Disease. PLoS ONE 2009, 4, e4151. [Google Scholar] [CrossRef]
- Kohane, D.S. Microparticles and Nanoparticles for Drug Delivery. Biotechnol. Bioeng. 2007, 96, 203–209. [Google Scholar] [CrossRef]
- Chono, S.; Tauchi, Y.; Morimoto, K. Influence of Particle Size on the Distributions of Liposomes to Atherosclerotic Lesions in Mice. Drug Dev. Ind. Pharm. 2006, 32, 125–135. [Google Scholar] [CrossRef]
- Chono, S.; Tanino, T.; Seki, T.; Morimoto, K. Uptake Characteristics of Liposomes by Rat Alveolar Macrophages: Influence of Particle Size and Surface Mannose Modification. J. Pharm. Pharmacol. 2007, 59, 75–80. [Google Scholar] [CrossRef]
- Lawlor, C.; O’sullivan, M.P.; Sivadas, N.; O’leary, S.; Gallagher, P.J.; Keane, J.; Cryan, S.-A. The Application of High-Content Analysis in the Study of Targeted Particulate Delivery Systems for Intracellular Drug Delivery to Alveolar Macrophages. Mol. Pharm. 2011, 8, 1101–1112. [Google Scholar] [CrossRef]
- Yue, H.; Wei, W.; Yue, Z.; Lv, P.; Wang, L.; Ma, G.; Su, Z. Particle Size Affects the Cellular Response in Macrophages. Eur. J. Pharm. Sci. 2010, 41, 650–657. [Google Scholar] [CrossRef]
- Patel, B.K.; Parikh, R.H.; Patel, N. Targeted Delivery of Mannosylated-PLGA Nanoparticles of Antiretroviral Drug to Brain. Int. J. Nanomed. 2018, 13, 97–100. [Google Scholar] [CrossRef]
- Yadav, S.; Gandham, S.K.; Panicucci, R.; Amiji, M.M. Intranasal Brain Delivery of Cationic Nanoemulsion-Encapsulated TNFα SiRNA in Prevention of Experimental Neuroinflammation. Nanomed. Nanotechnol. Biol. Med. 2016, 12, 987–1002. [Google Scholar] [CrossRef]
- Gao, W.; Li, J. Targeted SiRNA Delivery Reduces Nitric Oxide Mediated Cell Death after Spinal Cord Injury. J. Nanobiotechnol. 2017, 15, 1–11. [Google Scholar] [CrossRef]
- Zhou, Y.L.; Zhang, L.; Zhou, Z.; Liu, W.; Lu, Y.; He, S.; Cui, Y.; Qin, Y.; Hua, M. Antibody Modified Nanoparticle-Mediated Delivery of MiR-124 Regulates Apoptosis via Repression the Stat3 Signal in Mycobacterial-Infected Microglia. J. Biomed. Nanotechnol. 2018, 14, 2185–2197. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Lillard, J.W., Jr. Nanoparticle-Based Targeted Drug Delivery. Exp. Mol. Pathol. 2009, 86, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Mistry, A.; Glud, S.Z.; Kjems, J.; Randel, J.; Howard, K.A.; Stolnik, S.; Illum, L. Effect of Physicochemical Properties on Intranasal Nanoparticle Transit into Murine Olfactory Epithelium. J. Drug Target. 2009, 17, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, E.; Feng, Y.; Qi, J.; Fan, W.; Ma, Y.; He, H.; Xia, F.; Dong, X.; Zhao, W.; Lu, Y.; et al. Evidence of Nose-to-Brain Delivery of Nanoemulsions: Cargoes but Not Vehicles. Nanoscale 2017, 9, 1174–1183. [Google Scholar] [CrossRef]
- Hoppstädter, J.; Seif, M.; Dembek, A.; Cavelius, C.; Huwer, H.; Kraegeloh, A.; Kiemer, A.K. M2 Polarization Enhances Silica Nanoparticle Uptake by Macrophages. Front. Pharm. 2015, 6, 1–12. [Google Scholar] [CrossRef]
- Rathore, A.; Jain, A.; Gulbake, A.; Shilpi, S.; Khare, P.; Jain, A.; Jain, S.K. Mannosylated Liposomes Bearing Amphotericin B for Effective Management of Visceral Leishmaniasis. J. Liposome Res. 2011, 21, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Nahar, M.; Jain, N.K. Preparation, Characterization and Evaluation of Targeting Potential of Amphotericin B-Loaded Engineered PLGA Nanoparticles. Pharm. Res. 2009, 26, 2588–2598. [Google Scholar] [CrossRef] [PubMed]
- Xiao, B.; Laroui, H.; Ayyadurai, S.; Viennois, E.; Charania, M.A.; Zhang, Y.; Merlin, D. Mannosylated Bioreducible Nanoparticle-Mediated Macrophage-Specific TNF-α RNA Interference for IBD Therapy. Biomaterials 2013, 34, 7471–7482. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Guo, J.; Gui, S. Orally Targeted Galactosylated Chitosan Poly(Lactic-Co-Glycolic Acid) Nanoparticles Loaded with TNF-ɑ SiRNA Provide a Novel Strategy for the Experimental Treatment of Ulcerative Colitis. Eur. J. Pharm. Sci. 2018, 125, 232–243. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Yi, H.; He, H.; Pan, H.; Cai, L.; Ma, Y. Tumor Associated Macrophage-Targeted MicroRNA Delivery with Dual-Responsive Polypeptide Nanovectors for Anti-Cancer Therapy. Biomaterials 2017, 134, 166–179. [Google Scholar] [CrossRef] [PubMed]
- Niu, M.; Valdes, S.; Naguib, Y.W.; Hursting, S.D.; Cui, Z. Tumor-Associated Macrophage-Mediated Targeted Therapy of Triple-Negative Breast Cancer. Mol. Pharm. 2016, 13, 1833–1842. [Google Scholar] [CrossRef] [PubMed]
- Vieira, A.C.; Magalhães, J.; Rocha, S.; Cardoso, M.S.; Santos, S.G.; Borges, M.; Pinheiro, M.; Reis, S. Targeted Macrophages Delivery of Rifampicin-Loaded Lipid Nanoparticles to Improve Tuberculosis Treatment. Nanomedicine 2017, 12, 2721–2736. [Google Scholar] [CrossRef] [PubMed]
- He, H.; Yuan, Q.; Bie, J.; Wallace, R.L.; Yannie, P.J.; Wang, J.; Lancina, M.G.; Zolotarskaya, O.Y.; Korzun, W.; Yang, H.; et al. Development of Mannose Functionalized Dendrimeric Nanoparticles for Targeted Delivery to Macrophages: Use of This Platform to Modulate Atherosclerosis. Transl. Res. 2018, 193, 13–30. [Google Scholar] [CrossRef] [PubMed]
- Davis, S.M.; Reichel, D.; Bae, Y.; Pennypacker, K.R. Leukemia Inhibitory Factor-Loaded Nanoparticles with Enhanced Cytokine Metabolic Stability and Anti-Inflammatory Activity. Pharm. Res. 2018, 35. [Google Scholar] [CrossRef]
- Cerqueira, S.R.; Silva, B.L.; Oliveira, J.M.; Mano, J.F.; Sousa, N.; Salgado, A.J.; Reis, R.L. Multifunctionalized CMCht/PAMAM Dendrimer Nanoparticles Modulate the Cellular Uptake by Astrocytes and Oligodendrocytes in Primary Cultures of Glial Cells. Macromol. Biosci. 2012, 12, 591–597. [Google Scholar] [CrossRef]
- Akinrinmade, O.A.; Chetty, S.; Daramola, A.K.; Islam, M.-U.; Thepen, T.; Barth, S. CD64: An Attractive Immunotherapeutic Target for M1-Type Macrophage Mediated Chronic Inflammatory Diseases. Biomedicines 2017, 5, 56. [Google Scholar] [CrossRef] [PubMed]
- Hristodorov, D.; Mladenov, R.; von Felbert, V.; Huhn, M.; Fischer, R.; Barth, S.; Thepen, T. Targeting CD64 Mediates Elimination of M1 but Not M2 Macrophages in Vitro and in Cutaneous Inflammation in Mice and Patient Biopsies. MABS 2015, 7, 853–862. [Google Scholar] [CrossRef] [PubMed]
- Moura, C.C.; Segundo, M.A.; das Neves, J.; Reis, S.; Sarmento, B. Co-Association of Methotrexate and SPIONs into Anti-CD64 Antibody-Conjugated PLGA Nanoparticles for Theranostic Application. Int. J. Nanomed. 2014, 9, 4911–4922. [Google Scholar] [CrossRef]
- Albuquerque, J.; Moura, C.C.; Sarmento, B.; Reis, S. Solid Lipid Nanoparticles: A Potential Multifunctional Approach towards Rheumatoid Arthritis Theranostics. Molecules 2015, 20, 11103–11118. [Google Scholar] [CrossRef] [PubMed]
- Yong, S.-B.; Kim, H.J.; Kim, J.K.; Chung, J.Y.; Kim, Y.-H. Human CD64-Targeted Non-Viral SiRNA Delivery System for Blood Monocyte Gene Modulation. Sci. Rep. 2017, 7, 42171. [Google Scholar] [CrossRef] [PubMed]
- Blanco, E.; Shen, H.; Ferrari, M. Principles of Nanoparticle Design for Overcoming Biological Barriers to Drug Delivery. Nat. Biotechnol. 2015, 33, 941–951. [Google Scholar] [CrossRef] [PubMed]
- Engelhardt, B.; Sorokin, L. The Blood–brain and the Blood–cerebrospinal Fluid Barriers: Function and Dysfunction. Semin. Immunopathol. 2009, 31, 497–511. [Google Scholar] [CrossRef] [PubMed]
- Mo, X.; Zheng, Z.; He, Y.; Zhong, H.; Kang, X.; Shi, M.; Liu, T.; Jiao, Z.; Huang, Y. Antiglioma via Regulating Oxidative Stress and Remodeling Tumor-Associated Macrophage Using Lactoferrin-Mediated Biomimetic Codelivery of Simvastatin/Fenretinide. J. Control. Release 2018, 287, 12–23. [Google Scholar] [CrossRef]
- Calvo, P.; Gouritin, B.; Villarroya, H.; Eclancher, F.; Giannavola, C.; Klein, C.; Andreux, J.P.; Couvreur, P. Quantification and Localization of PEGylated Polycyanoacrylate Nanoparticles in Brain and Spinal Cord during Experimental Allergic Encephalomyelitis in the Rat. Eur. J. Neurosci. 2002, 15, 1317–1326. [Google Scholar] [CrossRef]
- Zhao, P.; Wang, Y.; Kang, X.; Wu, A.; Yin, W.; Tang, Y.; Wang, J.; Zhang, M.; Duan, Y.; Huang, Y. Dual-Targeting Biomimetic Delivery for Anti-Glioma Activity: Via Remodeling the Tumor Microenvironment and Directing Macrophage-Mediated Immunotherapy. Chem. Sci. 2018, 9, 2674–2689. [Google Scholar] [CrossRef]
- Zou, L.; Tao, Y.; Payne, G.; Do, L.; Thomas, T.; Rodriguez, J.; Dou, H. Targeted Delivery of Nano-PTX to the Brain Tumor-Associated Macrophages. Oncotarget 2017, 8, 6564–6578. [Google Scholar] [CrossRef] [PubMed]
- Bourganis, V.; Kammona, O.; Alexopoulos, A.; Kiparissides, C. Recent Advances in Carrier Mediated Nose-to-Brain Delivery of Pharmaceutics. Eur. J. Pharm. Biopharm. 2018, 128, 337–362. [Google Scholar] [CrossRef] [PubMed]
- Samaridou, E.; Alonso, M.J. Nose-to-Brain Peptide Delivery—The Potential of Nanotechnology. Bioorg. Med. Chem. 2018, 26, 2888–2905. [Google Scholar] [CrossRef] [PubMed]
- Warnken, Z.N.; Smyth, H.D.C.; Watts, A.B.; Weitman, S.; Kuhn, J.G.; Williams, R.O. Formulation and Device Design to Increase Nose to Brain Drug Delivery. J. Drug Deliv. Sci. Technol. 2016, 35, 213–222. [Google Scholar] [CrossRef]
- Dalpiaz, A.; Fogagnolo, M.; Ferraro, L.; Capuzzo, A.; Pavan, B.; Rassu, G.; Salis, A.; Giunchedi, P.; Gavini, E. Nasal Chitosan Microparticles Target a Zidovudine Prodrug to Brain HIV Sanctuaries. Antivir. Res. 2015, 123, 146–157. [Google Scholar] [CrossRef] [PubMed]
- Fransson, M.; Piras, E.; Wang, H.; Burman, J.; Duprez, I.; Harris, R.A.; LeBlanc, K.; Magnusson, P.U.; Brittebo, E.; Loskog, A.S.I. Intranasal Delivery of Central Nervous System-Retargeted Human Mesenchymal Stromal Cells Prolongs Treatment Efficacy of Experimental Autoimmune Encephalomyelitis. Immunology 2014, 142, 431–441. [Google Scholar] [CrossRef] [PubMed]
- Mayo, L.; Da Cunha, A.P.; Madi, A.; Beynon, V.; Yang, Z.; Alvarez, J.I.; Prat, A.; Sobel, R.A.; Kobzik, L.; Lassmann, H.; et al. IL-10-Dependent Tr1 Cells Attenuate Astrocyte Activation and Ameliorate Chronic Central Nervous System Inflammation. Brain 2016, 139, 1939–1957. [Google Scholar] [CrossRef]
- Esposito, E.; Cortesi, R.; Drechsler, M.; Fan, J.; Fu, B.M.; Calderan, L.; Mannucci, S.; Boschi, F.; Nastruzzi, C. Nanoformulations for Dimethyl Fumarate: Physicochemical Characterization and in Vitro / in Vivo Behavior. Eur. J. Pharm. Biopharm. 2017, 115, 285–296. [Google Scholar] [CrossRef]
| Type | FDA Approval | Format (Oral/Injectable) | Mechanism of Action | Studies in Monocytes/Macrophages | Adverse Effects | |
|---|---|---|---|---|---|---|
| Interferon β | Cytokine | 1993 | Injection (SC or IM) |
|
| Flu-like symptoms [116] |
| Glatiramer Acetate | Synthetic Copolymer [E,K,A,Y]n | 1995 | Injection (SC) |
|
| Injection site reaction [111] |
| Natalizumab | Anti-alpha-4 integrin | 2003 | IV infusion |
| PML risk, Allergic Reactions [108] | |
| Fingolimod | Antagonist of sphingosine 1 phosphate receptor | 2010 | Oral |
| Cardiovascular complications [130] | |
| Teriflunomide | dihydroorotate dehydrogenase inhibitor | 2012 | Oral |
| - | abnormal liver enzymes, gastrointestinal symptoms [131] |
| Dimethyl Fumarate | Fumaric Acid Ester | 2013 | Oral |
| gastrointestinal symptoms, abnormal liver enzymes, flushing [137] | |
| Alemtuzumab | Anti-CD52 | 2014 | IV infusion |
| - | Development of other autoimmune disease, Intracerebral haemorrhage (rare) [109,138] |
| Mitoxantrone | Chemotherapeutic agent | 2003 | IV infusion |
|
| Leucopoenia [141] |
| Ocrelizumab | Anti CD-20 | 2017 | IV infusion |
| - | Infusion related reaction, infections [142] |
| Reference | NP/MP Chemistry | Size | Cargo | Functionalised | Route of Delivery | Model | Target Cells | Additional Points |
|---|---|---|---|---|---|---|---|---|
| [161] | PEG-PLL-PLLeu copolymers | not reported | c-Rel siRNA | - | IP | EAE | Macrophage | |
| [162] | inorganic-organic hybrid NP | 60–80 nm | glucocorticoids | - | IP and IV(more effective) | EAE | Macrophage | |
| [163] | PEGylated liposome | <100 nm | Prednisolone | PEG | IV | EAE | not specified | liposomes were found mostly in macrophages, microglia and astrocytes |
| [164] | liposome | <100 nm | methylprednisolone | - | IV | EAE | not specified | Compared with free drug, only liposomal formulation resulted in significantly decreased CD68+ cells |
| [165] | liposome | not reported | methylprednisolone | short peptide fragments of ApoE or of β-amyloid | IV | EAE | not specified | |
| [166] | PEGylated liposome | 95–120 nm | methylprednisolone | PEG + Glutathione | IV | EAE | non specified | Bigger reduction in disease score with the targeted vs non targeted liposome |
| [167] | PLGA | 540 nm | (tNP) PLP (coated) | - | IV | EAE | APCs | Taken up by macrophages and DCs, most antigen presentation by DCs |
| [168] | PLGA | not reported | (tNP) PLP + rapamycin | - | SC prophylactic, IV peak disease | EAE | APCs | in vivo trafficking—IV -accumulation in liver and spleen most localisation to Macrophages and DCs in the spleen, but SC goes to the draining lymphnodes |
| [169] | PLGA | 350–835 nm | (tNP) PLP | - | IV | EAE | APCs (Macrophage) | Immunofluorescence staining showing co localisation with F4/80 positive macrophages, lungs, spleen, lymph nodes |
| [170] | PLGA | 80nm, 400 nm | (tNP) PLP | - | IV | EAE | APC’s (DCs) | Larger particles show better uptake in BMDCs |
| [171] | PLGA | 400–1500 nm | (tNP) MOG (coated) | - | IV or SC | EAE | APCs | SC admin not effective, non-significant trend to bring on disease more quickly |
| [172] | Au | 60 nm | (tNP) MOG + small molecule (ITE) | PEG(to stabilize) | IV or IP | EAE | DC | ITE ligand activates the aryl hydrocarbon receptor (Ahr), which can induce tolerogenic DCs. Observed Ahr activation in Macrophages in vivo |
| [173] | poly(ε-caprolactone) | 300–600 nm range | (tNP) Recombinant human MBP | - | SC | EAE | APCs | Histological observation of no macrophage or T cell infiltration in treated animals |
| [174] | PLGA | 200 nm | (tNP) MOG and IL-10 | - | SC | EAE | APCs | Authors suggest that observed T cell anergy and inhibited lymphocyte proliferation is due to induction of tolerance in macrophages |
| [175] | Acetalated Dextran | not reported | (tNP) MOG and Dexamethasone | - | SC | APC’s (Macrophage) | Reduced macrophage GM-CSF and IL-17 | |
| [176] | PLGA | not reported | (tNP) MOG, Vitamin D3, TGFb, GM-CSF | - | SC | EAE | APCs | Macrophages have second highest MP uptake in axillary lymph after DC’s, while these cells show equal uptake in inguinal lymph nodes. Treatment results in decreases numbers of activated macrophages in CNS |
| [177] | PLGA | 400–500 nm | (tNP) PLP | - | IV | EAE | Localisation to spleen, liver, and lung at 3, 6, and 18 h post injection, cleared by 24 h | |
| [178] | polystyrene, PLGA | 500 nm | (tNP) PLP | - | IV | EAE | Macrophage | SC did not work as well as IV admin, NP show localisation to spleen marginal zone macrophages and uptake via MARCO receptor |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nally, F.K.; De Santi, C.; McCoy, C.E. Nanomodulation of Macrophages in Multiple Sclerosis. Cells 2019, 8, 543. https://doi.org/10.3390/cells8060543
Nally FK, De Santi C, McCoy CE. Nanomodulation of Macrophages in Multiple Sclerosis. Cells. 2019; 8(6):543. https://doi.org/10.3390/cells8060543
Chicago/Turabian StyleNally, Frances K., Chiara De Santi, and Claire E. McCoy. 2019. "Nanomodulation of Macrophages in Multiple Sclerosis" Cells 8, no. 6: 543. https://doi.org/10.3390/cells8060543
APA StyleNally, F. K., De Santi, C., & McCoy, C. E. (2019). Nanomodulation of Macrophages in Multiple Sclerosis. Cells, 8(6), 543. https://doi.org/10.3390/cells8060543





