Impact of Lipoprotein(a) Levels on Perioperative Outcomes in Cardiac Surgery
Abstract
:1. Introduction
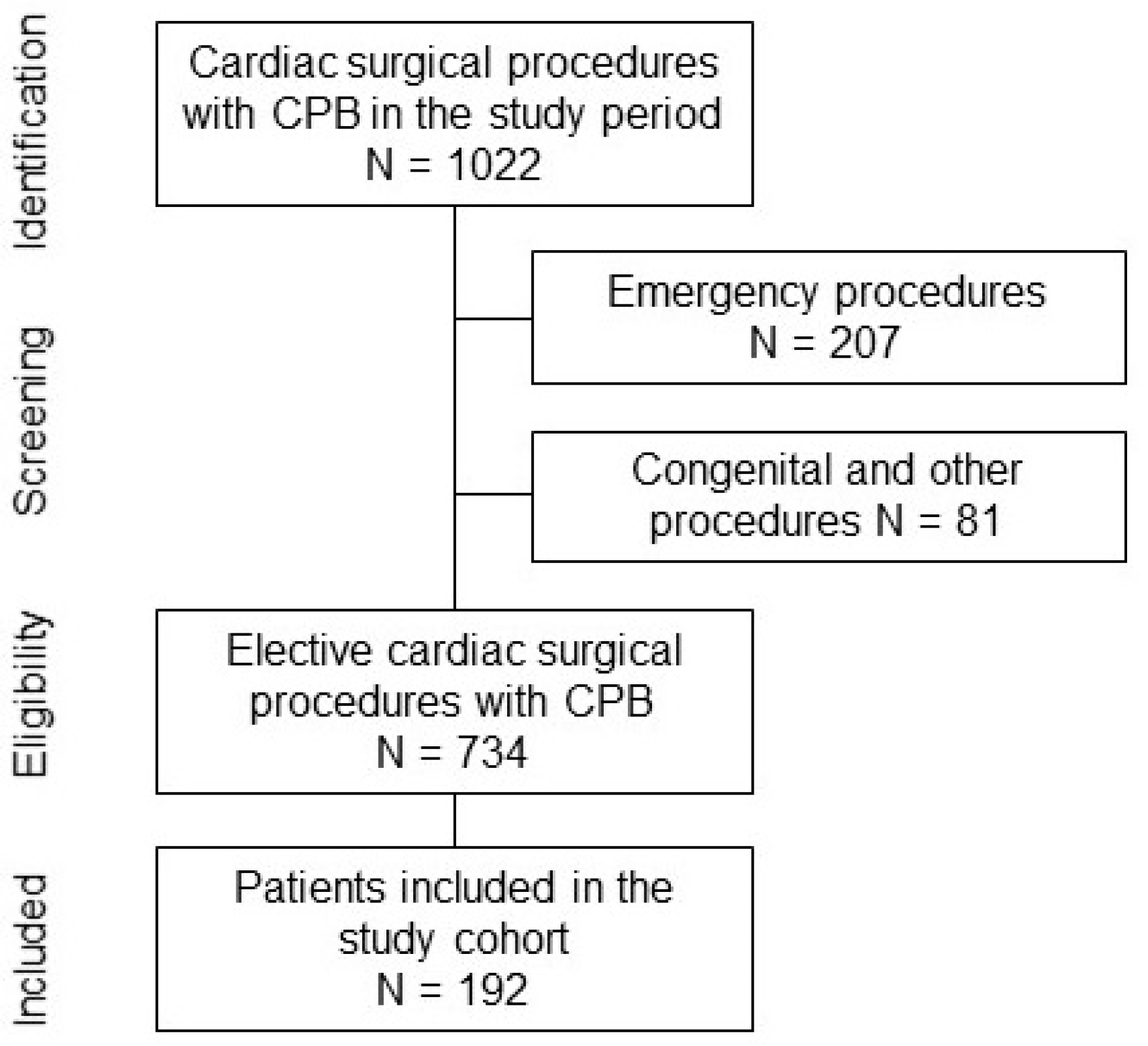
2. Materials and Methods
2.1. Cohort Description
2.2. Primary and Secondary Outcomes
2.3. Collection and Analysis of Blood Samples
2.4. Statistical Analysis
3. Results
3.1. Lp(a) Subanalysis of Primary and Secondary Outcomes
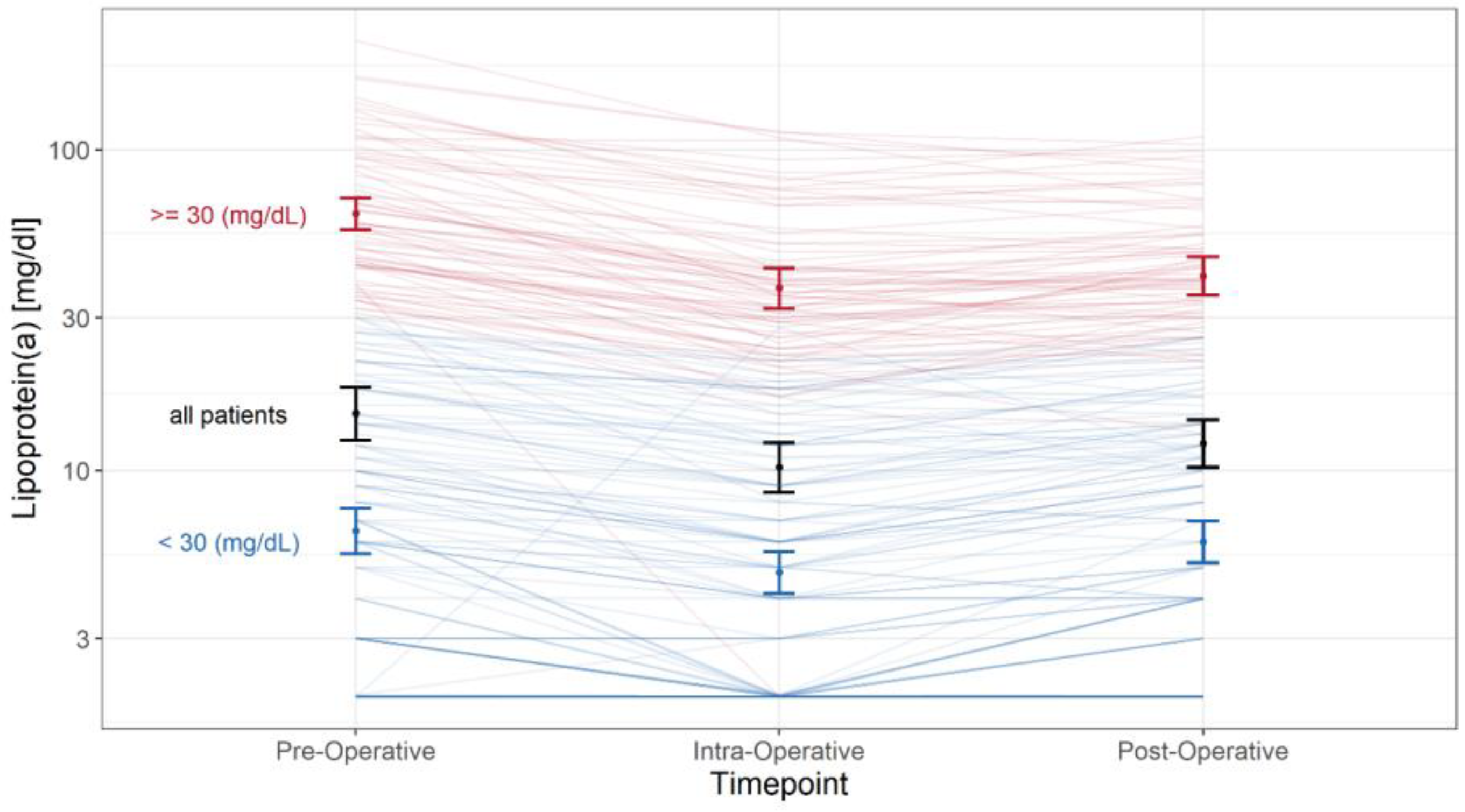
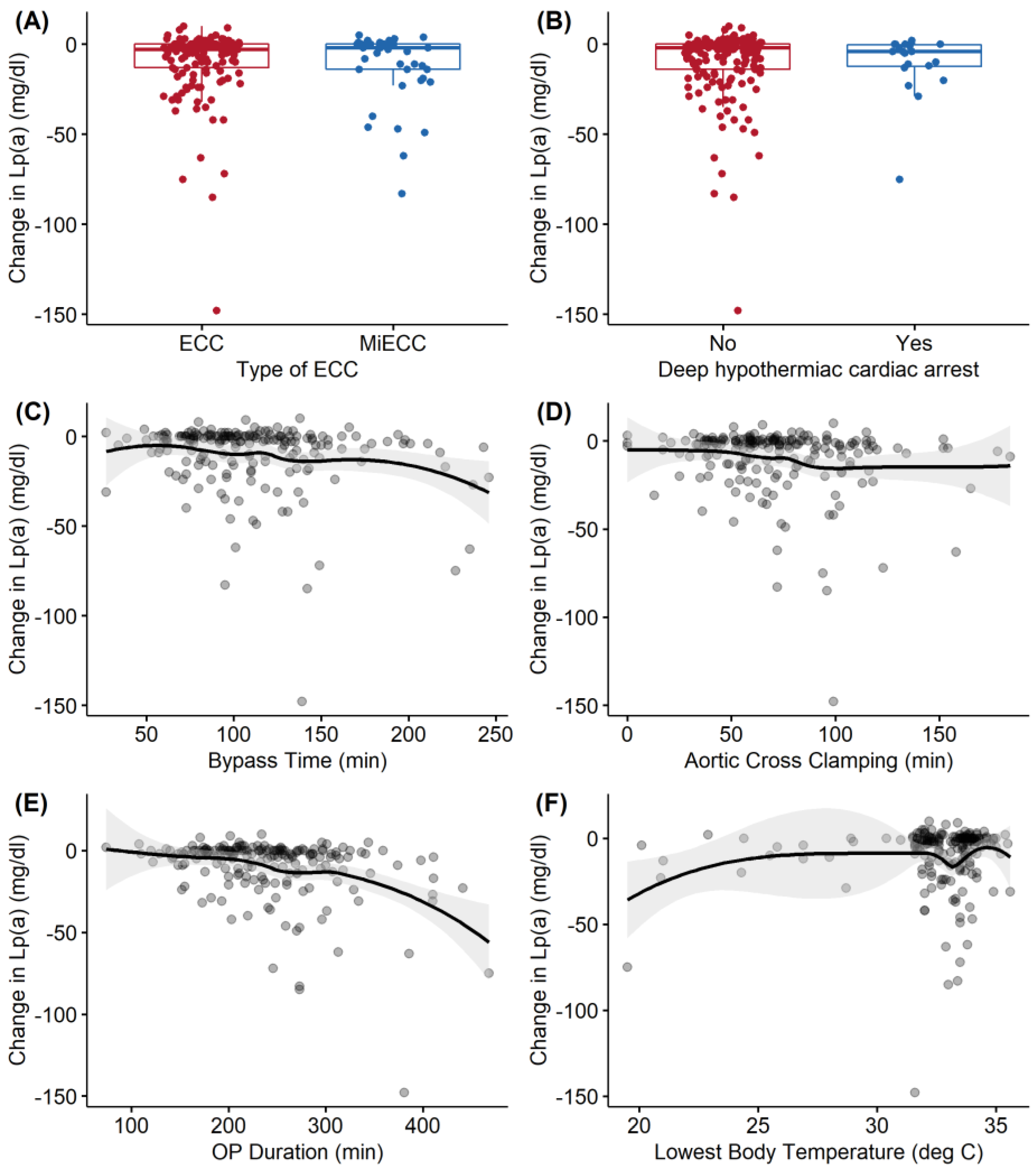
3.2. Lp(a) Subanalysis of Pre-, Intra-, and Postoperative Levels Stratified by Perioperative Covariates
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tsimikas, S.; Karwatowska-Prokopczuk, E.; Gouni-Berthold, I.; Tardif, J.C.; Baum, S.J.; Steinhagen-Thiessen, E.; Shapiro, M.D.; Stroes, E.S.; Moriarty, P.M.; Nordestgaard, B.G.; et al. Lipoprotein(a) Reduction in Persons with Cardiovascular Disease. N. Engl. J. Med. 2020, 382, 244–255. [Google Scholar] [CrossRef] [PubMed]
- Noma, A.; Abe, A.; Maeda, S.; Seishima, M.; Makino, K.; Yano, Y.; Shimokawa, K. Lp(a): An acute-phase reactant? Chem. Phys. Lipids 1994, 67, 411–417. [Google Scholar] [CrossRef]
- MBewu, A.D.; Durrington, P.N. Lipoprotein (a): Structure, properties and possible involvement in thrombogenesis and atherogenesis. Atherosclerosis 1990, 85, 1–14. [Google Scholar] [CrossRef]
- Larsson, S.C.; Gill, D.; Mason, A.M.; Jiang, T.; Bäck, M.; Butterworth, A.S.; Burgess, S. Lipoprotein(a) in Alzheimer, Atherosclerotic, Cerebrovascular, Thrombotic, and Valvular Disease: Mendelian Randomization Investigation. Circulation 2020, 141, 1826–1828. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Cui, X.; Jin, X.; Zhou, J.; Fu, M.; Zhong, C.; Sun, A.; Hu, K.; Fu, M.; Ge, J. Association between Lipoprotein (a) level on admission and the incidence of subsequent cardiovascular events in patients with acute coronary syndrome. Int. J. Cardiol. 2012, 158, 464–466. [Google Scholar] [CrossRef]
- Xu, N.; Tang, X.F.; Yao, Y.; Zhao, X.Y.; Chen, J.; Gao, Z.; Qiao, S.B.; Yang, Y.J.; Gao, R.L.; Xu, B.; et al. Association of Plasma Lipoprotein(a) With Long-Term Adverse Events in Patients with Chronic Kidney Disease Who Underwent Percutaneous Coronary Intervention. Am. J. Cardiol. 2018, 122, 2043–2048. [Google Scholar] [CrossRef]
- Hoover-Plow, J.; Huang, M. Lipoprotein(a) metabolism: Potential sites for therapeutic targets. Metabolism 2013, 62, 479–491. [Google Scholar] [CrossRef] [Green Version]
- Plakogiannis, R.; Sorbera, M.; Fischetti, B.; Chen, M. The Role of Antisense Therapies Targeting Lipoprotein(a). J. Cardiovasc. Pharmacol. 2021, 78, e5–e11. [Google Scholar] [CrossRef]
- Willeit, P.; Ridker, P.M.; Nestel, P.J.; Simes, J.; Tonkin, A.M.; Pedersen, T.R.; Schwartz, G.G.; Olsson, A.G.; Colhoun, H.M.; Kronenberg, F.; et al. Baseline and on-statin treatment lipoprotein(a) levels for prediction of cardiovascular events: Individual patient-data meta-analysis of statin outcome trials. Lancet 2018, 392, 1311–1320. [Google Scholar] [CrossRef] [Green Version]
- Wilson, D.P.; Jacobson, T.A.; Jones, P.H.; Koschinsky, M.; McNeal, C.J.; Nordestgaard, B.G.; Orringer, C.E. Use of Lipoprotein(a) in clinical practice: A biomarker whose time has come. A scientific statement from the National Lipid Association. J. Clin. Lipidol. 2019, 13, 374–392. [Google Scholar] [CrossRef]
- Kostner, G.M.; Avogaro, P.; Cazzolato, G.; Marth, E.; Bittolo-Bon, G.; Qunici, G.B. Lipoprotein Lp(a) and the risk for myocardial infarction. Atherosclerosis 1981, 38, 51–61. [Google Scholar] [CrossRef]
- Emerging Risk Factors Collaboration. Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA 2009, 302, 412–423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nordestgaard, B.G.; Chapman, M.J.; Ray, K.; Borén, J.; Andreotti, F.; Watts, G.; Ginsberg, H.; Amarenco, P.; Catapano, A.L.; Descamps, O.S.; et al. Lipoprotein(a) as a cardiovascular risk factor: Current status. Eur. Heart J. 2010, 31, 2844–2853. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M.; Schweizer, J.; Nakas, C.T.; Schütz, V.; Westphal, L.P.; Inauen, C.; Pokorny, T.; Luft, A.; Leichtle, A.; Arnold, M.; et al. Lipoprotein(a) is associated with large artery atherosclerosis stroke aetiology and stroke recurrence among patients below the age of 60 years: Results from the BIOSIGNAL study. Eur. Heart J. 2021, 42, 2186–2196. [Google Scholar] [CrossRef] [PubMed]
- Langsted, A.; Nordestgaard, B.G.; Kamstrup, P.R. Elevated Lipoprotein(a) and Risk of Ischemic Stroke. J. Am. Coll. Cardiol. 2019, 74, 54–66. [Google Scholar] [CrossRef]
- Mitsuda, T.; Uemura, Y.; Ishii, H.; Takemoto, K.; Uchikawa, T.; Koyasu, M.; Ishikawa, S.; Miura, A.; Imai, R.; Iwamiya, S.; et al. Lipoprotein(a) levels predict adverse vascular events after acute myocardial infarction. Heart Vessels 2016, 31, 1923–1929. [Google Scholar] [CrossRef] [PubMed]
- Xu, N.; Jiang, L.; Xu, L.; Tian, J.; Zhang, C.; Zhao, X.; Feng, X.; Wang, D.; Zhang, Y.; Sun, K.; et al. Impact of Lipoprotein(a) on Long-Term (Mean 6.2 Years) Outcomes in Patients With Three-Vessel Coronary Artery Disease. Am. J. Cardiol. 2020, 125, 528–533. [Google Scholar] [CrossRef]
- Akins, C.W.; Miller, D.C.; Turina, M.I.; Kouchoukos, N.T.; Blackstone, E.H.; Grunkemeier, G.L.; Takkenberg, J.; David, T.E.; Butchart, E.G.; Adams, D.H.; et al. Guidelines for reporting mortality and morbidity after cardiac valve interventions. J. Thorac. Cardiovasc. Surg. 2008, 135, 732–738. [Google Scholar] [CrossRef] [Green Version]
- von Haehling, S.; Morley, J.E.; Coats, A.J.S.; Anker, S.D. Ethical guidelines for publishing in the Journal of Cachexia, Sarcopenia and Muscle: Update 2019. J. Cachexia Sarcopenia Muscle 2019, 10, 1143–1145. [Google Scholar] [CrossRef] [Green Version]
- Molinari, E.A.; Pichler, P.F.; Grillhofer, H.; Kostner, G.M. Immunoturbidimetric determination of lipoprotein(a): Improvement in the measurement of turbid and triglyceride-rich samples. Clin. Chim. Acta 1995, 235, 59–69. [Google Scholar] [CrossRef]
- Roques, F.; Nashef, S.A.; Michel, P.; Gauducheau, E.; De Vincentiis, C.; Baudet, E.; Cortina, J.; David, M.; Faichney, A.; Gavrielle, F.; et al. Risk factors and outcome in European cardiac surgery: Analysis of the EuroSCORE multinational database of 19,030 patients. Europ. J. Cardio-Thorac. Surg. 1999, 15, 816–823. [Google Scholar] [CrossRef] [Green Version]
- Gaudino, M.; Rahouma, M.; Di Mauro, M.; Yanagawa, B.; Abouarab, A.; Demetres, M.; Di Franco, A.; Arisha, M.J.; Ibrahim, D.A.; Baudo, M.; et al. Early Versus Delayed Stroke After Cardiac Surgery: A Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2019, 8, e012447. [Google Scholar] [CrossRef] [PubMed]
- Cobbaert, C.; Louisa, A.; Struijk, L.; Demeyere, R.; Meyns, B. Lipoprotein(a) changes during and after coronary artery bypass grafting: An epiphenomenon? Clin. Biochem. 1998, 35 Pt 1, 75–79. [Google Scholar] [CrossRef] [Green Version]
- Schnitzler, J.G.; Poels, K.; Stiekema, L.C.A.; Yeang, C.; Tsimikas, S.; Kroon, J.; Stroes, E.S.G.; Lutgens, E.; Seijkens, T.T.P. Short-term regulation of hematopoiesis by lipoprotein(a) results in the production of pro-inflammatory monocytes. Int. J. Cardiol. 2020, 315, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Mihalj, M.; Heinisch, P.P.; Huber, M.; Schefold, J.C.; Hartmann, A.; Walter, M.; Steinhagen-Thiessen, E.; Schmidli, J.; Stüber, F.; Räber, L.; et al. Effect of Perioperative Lipid Status on Clinical Outcomes After Cardiac Surgery. Cells 2021, 10, 2717. Available online: https://www.mdpi.com/2073-4409/10/10/2717 (accessed on 19 October 2021). [CrossRef]
| All Patients | Low Lp(a) (<30 mg/dL) | High Lp(a) (≥30 mg/dL) | P | |
|---|---|---|---|---|
| N = 192 | N = 121 | N = 71 | ||
| Demographics | ||||
| Age (years) | 67.0 (60.0;73.0) | 66.0 (60.0;73.0) | 69.0 (61.0;74.5) | 0.246 |
| Height (cm) | 173 (8.71) | 173 (8.69) | 173 (8.80) | 0.593 |
| Weight (kg) | 80.4 (70.0;90.1) | 82.0 (70.7;94.0) | 78.4 (70.0;89.4) | 0.201 |
| BMI (kg/m2) | 26.1 (23.7;30.4) | 26.7 (23.8;30.4) | 25.4 (23.4;29.7 | 0.206 |
| Sex (Male) | 145 (75.5%) | 94 (77.7%) | 51 (71.8%) | 0.461 |
| Comorbidities | ||||
| Diabetes (Yes) | 35 (18.2%) | 25 (20.7%) | 10 (14.1%) | 0.344 |
| Diabetes on insulin | 0.667 | |||
| No | 24 (68.6%) | 18 (72.0%) | 6 (60.0%) | |
| Yes | 11 (31.4%) | 7 (28.0%) | 4 (40.0%) | |
| Hypertension † (Yes) | 130 (68.4%) | 79 (66.4%) | 51 (71.8%) | 0.535 |
| Dyslipidaemia † (Yes) | 111 (58.1%) | 70 (58.3%) | 41 (57.7%) | 1.000 |
| Nicotine † | 0.173 | |||
| Former smoker | 49 (26.1%) | 36 (30.0%) | 13 (19.1%) | |
| Non-smoker | 97 (51.6%) | 61 (50.8%) | 36 (52.9%) | |
| Smoker | 42 (22.3%) | 23 (19.2%) | 19 (27.9%) | |
| Adipositas (Yes) | 52 (27.1%) | 34 (28.1%) | 18 (25.4%) | 0.806 |
| Preoperative renal disease (Yes) | 43 (22.4%) | 24 (19.8%) | 19 (26.8%) | 0.351 |
| Peripheral vascular disease † | 0.528 | |||
| No | 167 (93.8%) | 107 (94.7%) | 60 (92.3%) | |
| Stage 1 | 4 (2.25%) | 3 (2.65%) | 1 (1.54%) | |
| Stage 2 | 4 (2.25%) | 1 (0.88%) | 3 (4.62%) | |
| Stage 3 | 1 (0.56%) | 1 (0.88%) | 0 (0.00%) | |
| Stage 4 | 2 (1.12%) | 1 (0.88%) | 1 (1.54%) | |
| Carotid disease † | 0.226 | |||
| <50% | 1 (0.58%) | 1 (0.94%) | 0 (0.00%) | |
| >90% | 3 (1.75%) | 1 (0.94%) | 2 (3.08%) | |
| 50–69%, | 9 (5.26%) | 5 (4.72%) | 4 (6.15%) | |
| 70–89% | 2 (1.17%) | 0 (0.00%) | 2 (3.08%) | |
| no | 156 (91.2%) | 99 (93.4%) | 57 (87.7%) | |
| Myocardial infarction † | 0.832 | |||
| No MI | 171 (89.5%) | 106 (88.3%) | 65 (91.5%) | |
| MI 0–7 days before operation | 3 (1.57%) | 2 (1.67%) | 1 (1.41%) | |
| MI 8–90 days before operation | 8 (4.19%) | 5 (4.17%) | 3 (4.23%) | |
| MI >90 days before operation | 9 (4.71%) | 7 (5.83%) | 2 (2.82%) | |
| COPD † (Yes) | 23 (12.1%) | 17 (14.3%) | 6 (8.45%) | 0.336 |
| NYHA † | 0.879 | |||
| 1 | 60 (31.4%) | 37 (30.8%) | 23 (32.4%) | |
| 2 | 90 (47.1%) | 59 (49.2%) | 31 (43.7%) | |
| 3 | 38 (19.9%) | 22 (18.3%) | 16 (22.5%) | |
| 4 | 3 (1.57%) | 2 (1.67%) | 1 (1.41%) | |
| CCS † | 0.950 | |||
| 0 | 118 (62.4%) | 72 (61.0%) | 46 (64.8%) | |
| 1 | 34 (18.0%) | 22 (18.6%) | 12 (16.9%) | |
| 2 | 25 (13.2%) | 17 (14.4%) | 8 (11.3%) | |
| 3 | 9 (4.76%) | 5 (4.24%) | 4 (5.63%) | |
| 4 | 3 (1.59%) | 2 (1.69%) | 1 (1.41%) | |
| Ejection fraction † | 60.0 (55.0;65.0) | 60.0 (55.0;65.0) | 60.0 (55.0;65.0) | 0.807 |
| EuroSCORE2 † | 1.73 (0.90;2.93) | 1.75 (0.90;2.79) | 1.67 (0.91;3.26) | 0.924 |
| Logistic EuroSCORE † | 4.65 (2.34;8.00) | 4.65 (2.44;7.41) | 4.92 (2.08;10.9) | 0.667 |
| Valve type | ||||
| Aortic valve (Yes) | 86 (44.8%) | 55 (45.5%) | 31 (43.7%) | 0.928 |
| Mitral valve (Yes) | 45 (23.4%) | 30 (24.8%) | 15 (21.1%) | 0.687 |
| Tricuspid valve (Yes) | 17 (8.85%) | 12 (9.92%) | 5 (7.04%) | 0.679 |
| Coronary artery bypass (Yes) | 77 (40.1%) | 42 (34.7%) | 35 (49.3%) | 0.066 |
| Ascending aortic (Yes) | 38 (19.8%) | 23 (19.0%) | 15 (21.1%) | 0.867 |
| Aortic arch (Yes) | 11 (5.73%) | 7 (5.79%) | 4 (5.63%) | 1.000 |
| Preoperative Lipoproteins | ||||
| Cholesterol (mmol/L) | 4.42 (1.13) | 4.52 (1.15) | 4.26 (1.08) | 0.123 |
| HDL cholesterol(mmol/L) | 1.13 (0.92;1.35) | 1.08 (0.92;1.36) | 1.16 (0.92;1.34) | 0.609 |
| LDL cholesterol (mmol/L) | 2.68 (2.14;3.40) | 2.72 (2.30;3.41) | 2.47 (2.00;3.26) | 0.096 |
| Quotient overall (.) | 2.50 (1.80;3.20) | 2.50 (1.90;3.20) | 2.40 (1.60;2.95) | 0.149 |
| Triglycerides (mmol/L) | 1.33 (0.97;1.88) | 1.40 (1.04;1.98) | 1.16 (0.92;1.63) | 0.027 |
| Lipoprotein(a) (mg/dl) | 15.5 (5.00;45.2) | 7.00 (3.00;14.0) | 59.0 (44.0;91.5) | < 0.001 |
| Procedural characteristics | ||||
| ECC or MiECC | 0.566 | |||
| ECC | 149 (77.6%) | 96 (79.3%) | 53 (74.6%) | |
| MiECC | 43 (22.4%) | 25 (20.7%) | 18 (25.4%) | |
| Bypass time (min) | 104 (80.0;132) | 103 (78.0;130) | 109 (83.0;136) | 0.572 |
| Aortic cross-clamping (min) | 68.5 (52.0;91.8) | 68.0 (51.0;90.0) | 70.0 (53.5;95.5) | 0.774 |
| Lowest body temperature (°C) | 33.2 (32.1;33.8) | 33.3 (32.0;33.9) | 33.2 (32.3;33.8) | 0.998 |
| Deep hypothermic cardiac arrest † (Yes) | 19 (9.95%) | 13 (10.7%) | 6 (8.57%) | 0.816 |
| Operation duration (min) | 234 (195;276) | 223 (188;269) | 248 (208;287) | 0.030 |
| All Patients | Low Lp(a) (<30 mg/dL) | High Lp(a) (≥30 mg/dL) | P | P-adj * | |
|---|---|---|---|---|---|
| N = 192 | N = 121 | N = 71 | |||
| Postoperative stroke† | 0.335 | 0.729 | |||
| No | 179 (94.2%) | 114 (95.8%) | 65 (91.5%) | ||
| Yes | 11 (5.79%) | 5 (4.20%) | 6 (8.45%) | ||
| 30-day mortality | 0.530 | 0.729 | |||
| Died | 2 (1.04%) | 2 (1.65%) | 0 (0.00%) | ||
| Survived | 190 (99.0%) | 119 (98.3%) | 1 (100%) | ||
| 1-Year follow-up‡ | 0.729 | 0.729 | |||
| Alive | 179 (96.2%) | 114 (95.8%) | 65 (97.0%) | ||
| Deceased | 7 (3.76%) | 5 (4.20%) | 2 (2.99%) |
| All Patients | Low Lp(a) (<30 mg/dL) | High Lp(a) (≥30 mg/dL) | P | |
|---|---|---|---|---|
| N = 192 | N = 121 | N = 71 | ||
| Length of postoperative hospital stay (days) | 7.00 (6.00;9.00) | 7.00 (6.00;9.00) | 7.00 (6.00;9.00) | 0.367 |
| Renal complications | 0.370 | |||
| No | 191 (99.5%) | 121 (100%) | 70 (98.6%) | |
| Yes | 1 (0.52%) | 0 (0.00%) | 1 (1.41%) | |
| Renal replacement therapy | >0.99 | |||
| No | 191 (99.5%) | 120 (99.2%) | 71 (100%) | |
| Yes | 1 (0.52%) | 1 (0.83%) | 0 (0.00%) | |
| Postoperative atrial fibrillation | 0.784 | |||
| No | 148 (77.1%) | 92 (76.0%) | 56 (78.9%) | |
| Yes | 44 (22.9%) | 29 (24.0%) | 15 (21.1%) | |
| Myocardial infarction | >0.99 | |||
| No | 186 (96.9%) | 117 (96.7%) | 69 (97.2%) | |
| Yes | 6 (3.12%) | 4 (3.31%) | 2 (2.82%) | |
| Re-exploration for bleeding | >0.99 | |||
| No | 188 (97.9%) | 118 (97.5%) | 70 (98.6%) | |
| Yes | 4 (2.08%) | 3 (2.48%) | 1 (1.41%) |
| Coefficient | 95% CI 1 | P | |
|---|---|---|---|
| ECC or MiECC | |||
| ECC | |||
| MiECC | 9.8 | −5.6, 25 | 0.21 |
| Bypass time (hours) | −5.1 | −29, 19 | 0.67 |
| Aortic cross clamping (hours) | 4.8 | −18, 28 | 0.68 |
| Lowest body temperature (°C) | −4.0 | −8.0, −0.06 | 0.046 |
| Deep hypothermic cardiac arrest | |||
| No | |||
| Yes | −35 | −68, −1.7 | 0.039 |
| Operation duration (hours) | −11 | −20, −1.7 | 0.020 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heinisch, P.P.; Mihalj, M.; Huber, M.; Schefold, J.C.; Hartmann, A.; Walter, M.; Steinhagen-Thiessen, E.; Schmidli, J.; Stüber, F.; Räber, L.; et al. Impact of Lipoprotein(a) Levels on Perioperative Outcomes in Cardiac Surgery. Cells 2021, 10, 2829. https://doi.org/10.3390/cells10112829
Heinisch PP, Mihalj M, Huber M, Schefold JC, Hartmann A, Walter M, Steinhagen-Thiessen E, Schmidli J, Stüber F, Räber L, et al. Impact of Lipoprotein(a) Levels on Perioperative Outcomes in Cardiac Surgery. Cells. 2021; 10(11):2829. https://doi.org/10.3390/cells10112829
Chicago/Turabian StyleHeinisch, Paul Philipp, Maks Mihalj, Markus Huber, Joerg C. Schefold, Alexander Hartmann, Michael Walter, Elisabeth Steinhagen-Thiessen, Juerg Schmidli, Frank Stüber, Lorenz Räber, and et al. 2021. "Impact of Lipoprotein(a) Levels on Perioperative Outcomes in Cardiac Surgery" Cells 10, no. 11: 2829. https://doi.org/10.3390/cells10112829
APA StyleHeinisch, P. P., Mihalj, M., Huber, M., Schefold, J. C., Hartmann, A., Walter, M., Steinhagen-Thiessen, E., Schmidli, J., Stüber, F., Räber, L., & Luedi, M. M. (2021). Impact of Lipoprotein(a) Levels on Perioperative Outcomes in Cardiac Surgery. Cells, 10(11), 2829. https://doi.org/10.3390/cells10112829







