Effect of Perioperative Lipid Status on Clinical Outcomes after Cardiac Surgery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cohort Description
2.2. Collection and Analysis of Blood Samples
2.3. Statistical Analysis
3. Results
3.1. Subgroup Analysis of Statin Therapy
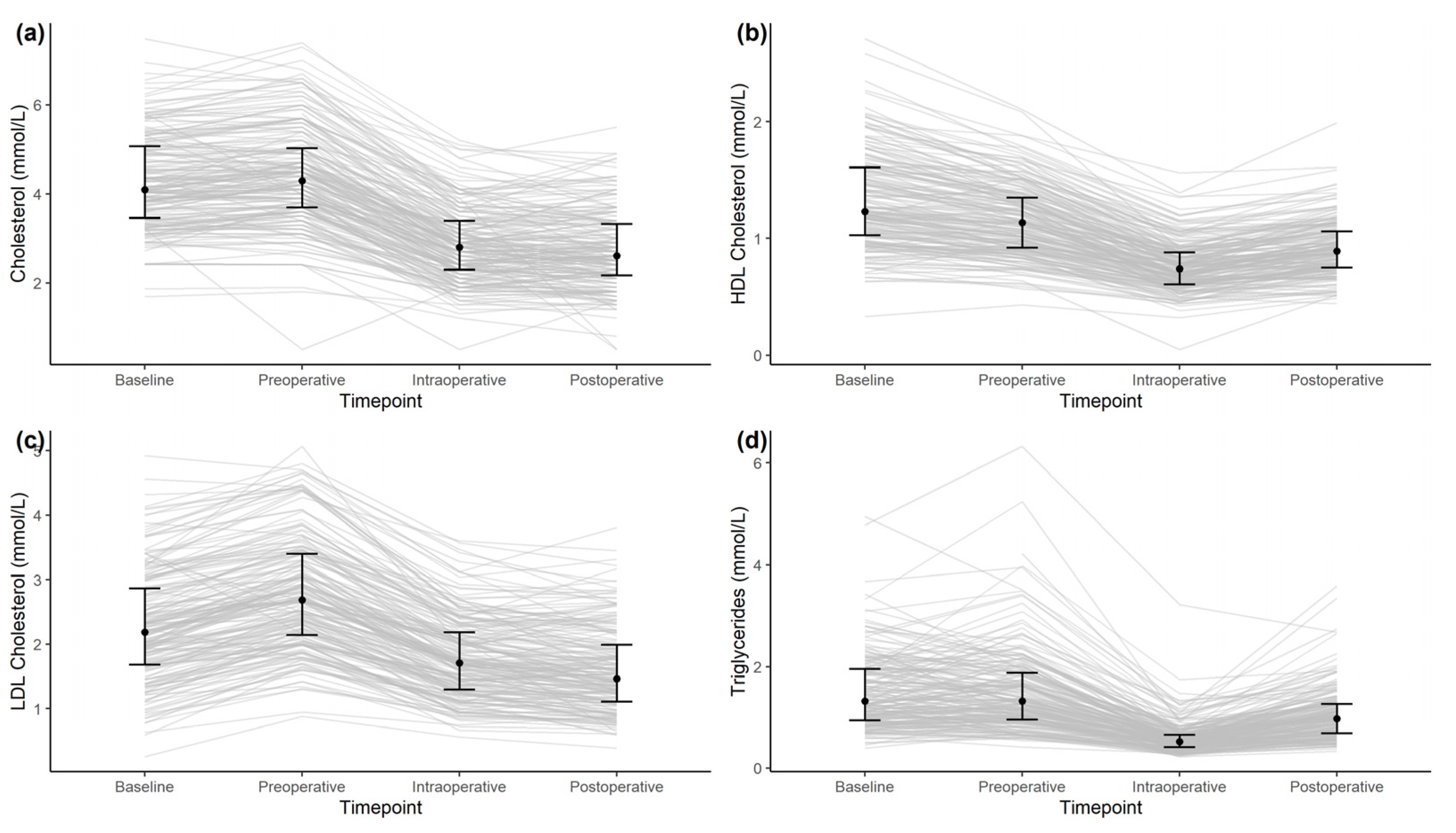
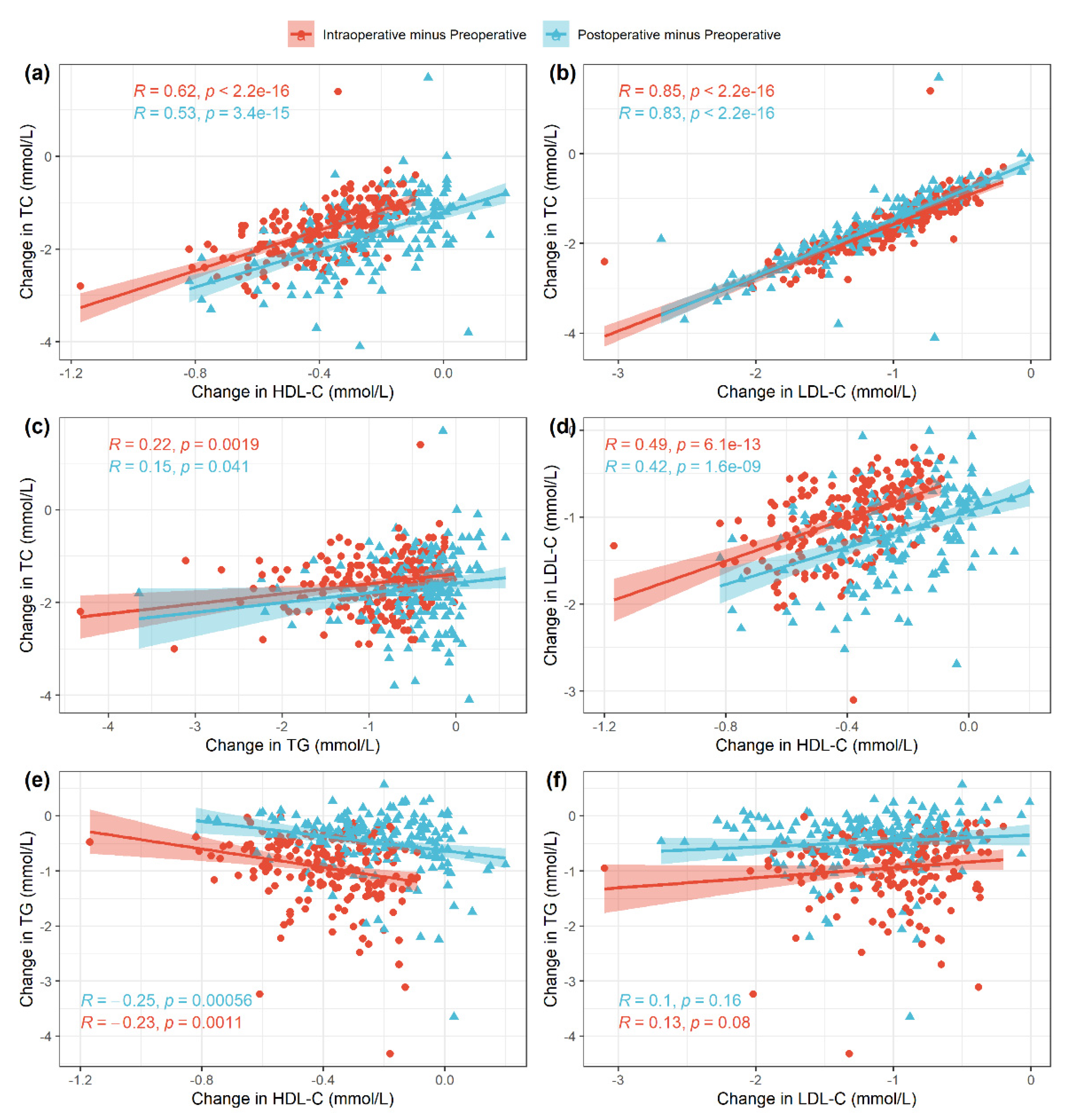
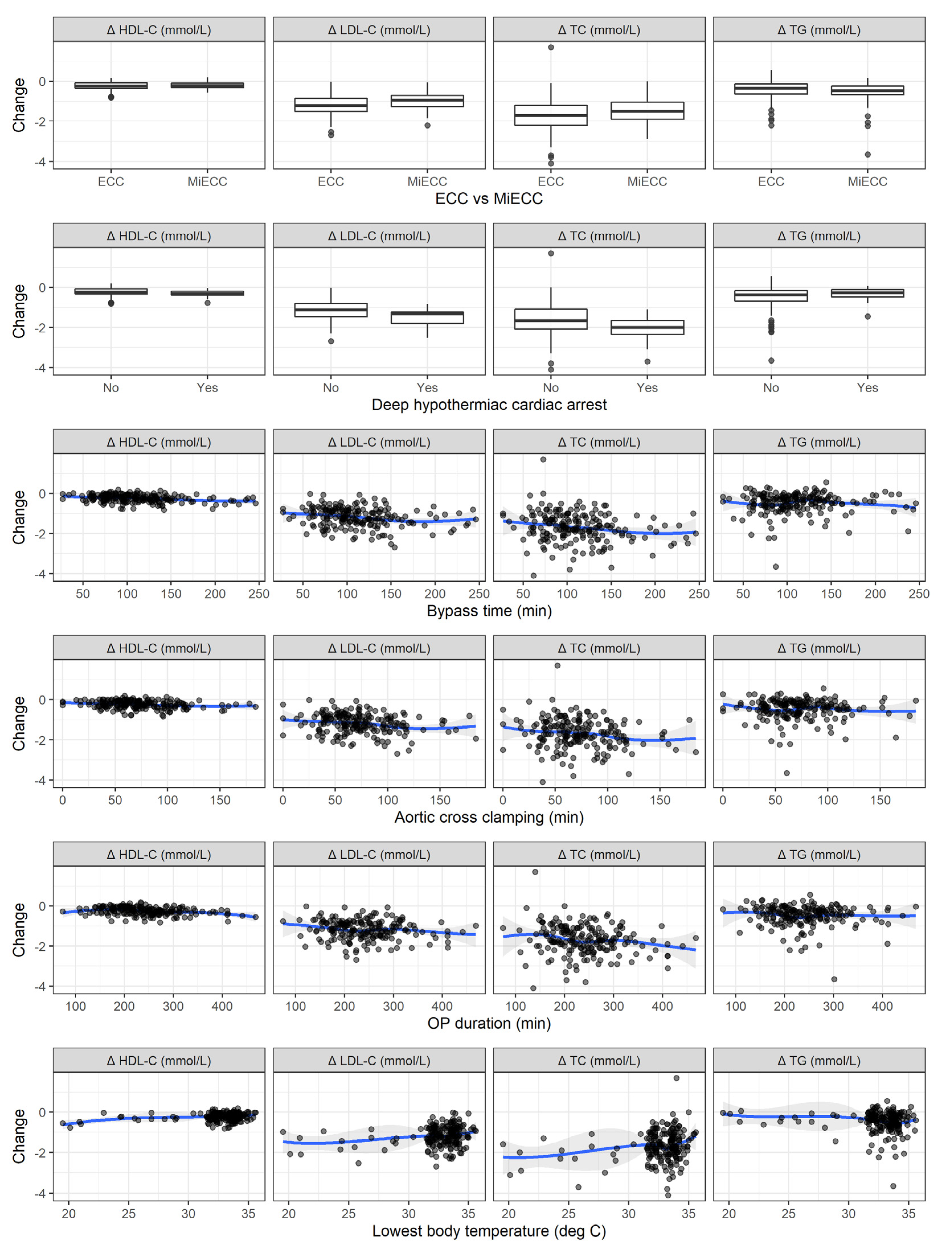
3.2. Perioperative Alterations in Lipid Levels
3.3. Clinical Outcomes
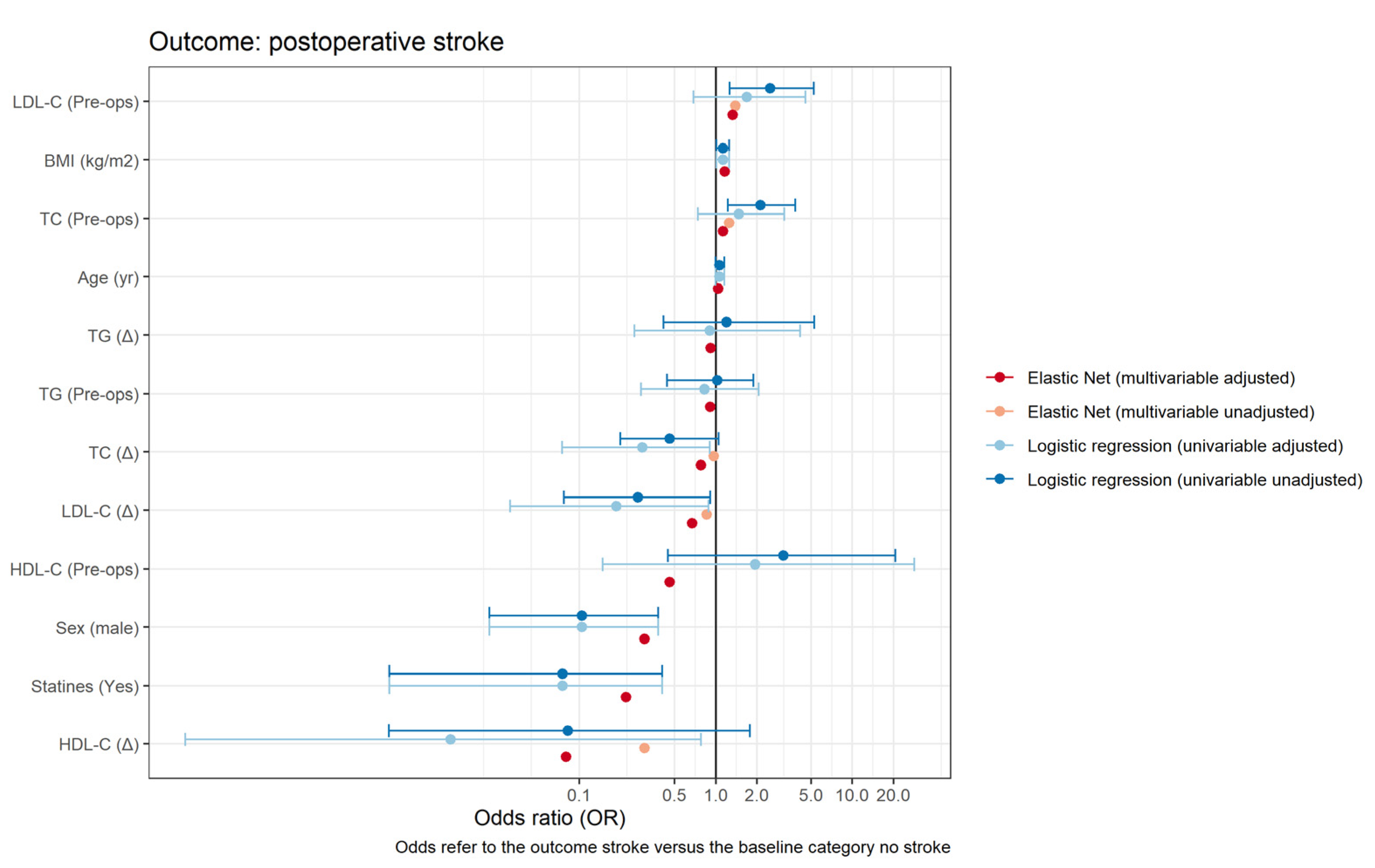
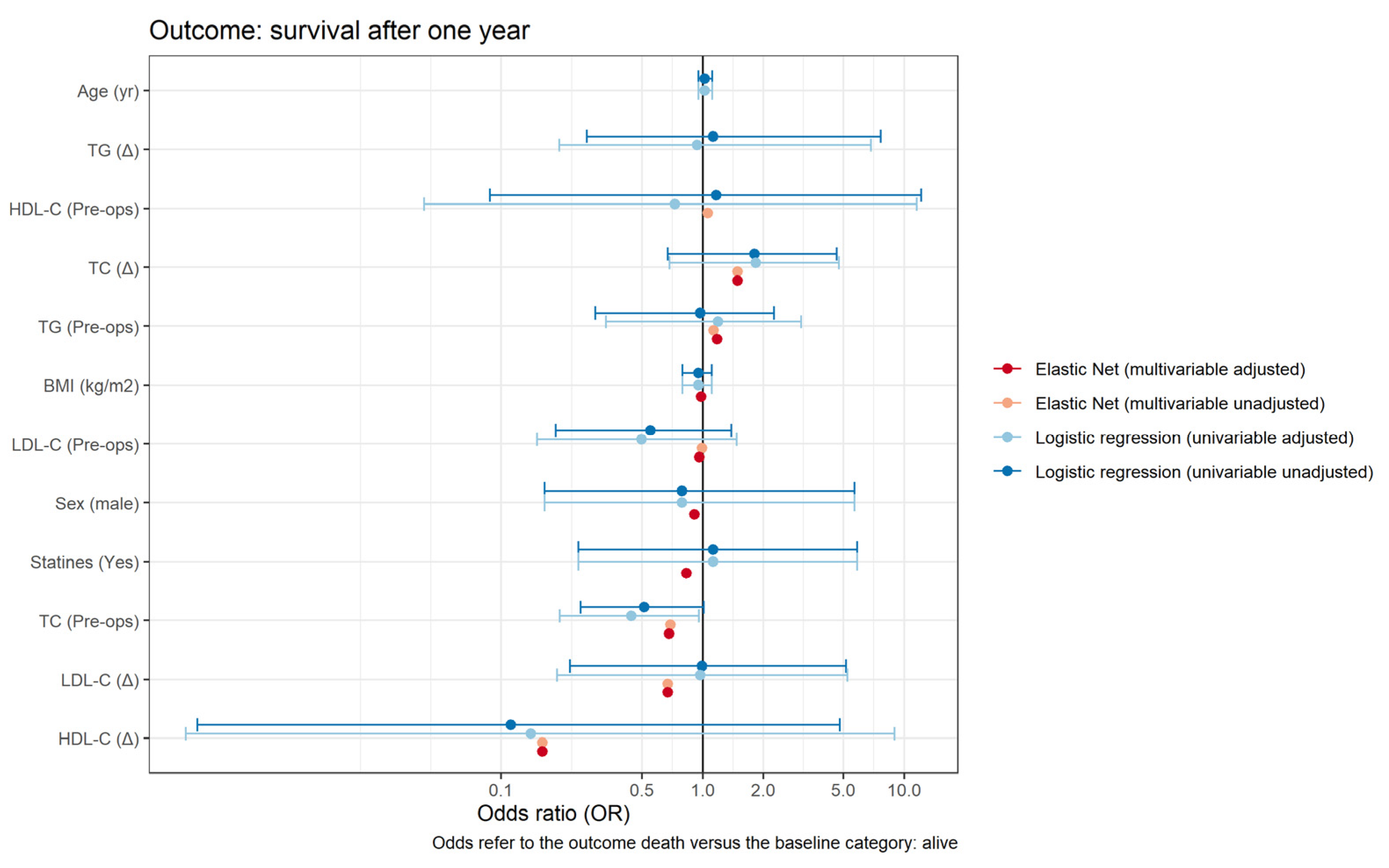
3.4. Association between Lipids and Postoperative Stroke and Overall Survival
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Collet, J.-P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar]
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 2019, 139, e526–e528. [Google Scholar] [CrossRef] [PubMed]
- Claessen, B.E.; Guedeney, P.; Gibson, C.M.; Angiolillo, D.J.; Cao, D.; Lepor, N.; Mehran, R. Lipid Management in Patients Presenting With Acute Coronary Syndromes: A Review. J. Am. Heart Assoc. 2020, 9, e018897. [Google Scholar] [CrossRef] [PubMed]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Z.; Jayaram, R.; Jiang, L.; Emberson, J.; Zhao, Y.; Li, Q.; Du, J.; Guarguagli, S.; Hill, M.; Chen, Z.; et al. Perioperative Rosuvastatin in Cardiac Surgery. N. Engl. J. Med. 2016, 374, 1744–1753. [Google Scholar] [CrossRef] [PubMed]
- Eisen, A.; Cannon, C.P.; Blazing, M.A.; Bohula, E.A.; Park, J.G.; Murphy, S.A.; White, J.A.; Giugliano, R.P.; Braunwald, E. The benefit of adding ezetimibe to statin therapy in patients with prior coronary artery bypass graft surgery and acute coronary syndrome in the IMPROVE-IT trial. Eur. Heart J. 2016, 37, 3576–3584. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019, 73, 3168–3209. [Google Scholar] [CrossRef]
- Sousa-Uva, M.; Head, S.J.; Milojevic, M.; Collet, J.P.; Landoni, G.; Castella, M.; Dunning, J.; Gudbjartsson, T.; Linker, N.J.; Sandoval, E.; et al. 2017 EACTS Guidelines on perioperative medication in adult cardiac surgery. Eur. J. Cardio-Thorac. Surg. 2018, 53, 5–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mihalj, M.; Carrel, T.; Urman, R.D.; Stueber, F.; Luedi, M.M. Recommendations for Preoperative Assessment and Shared Decision-Making in Cardiac Surgery. Curr. Anesthesiol. Rep. 2020, 10, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Antonopoulos, A.S.; Odutayo, A.; Oikonomou, E.K.; Trivella, M.; Petrou, M.; Collins, G.S.; Antoniades, C. Development of a risk score for early saphenous vein graft failure: An individual patient data meta-analysis. J. Thorac. Cardiovasc. Surg. 2020, 160, 116–127.e4. [Google Scholar] [CrossRef] [Green Version]
- Gallo, M.; Trivedi, J.R.; Monreal, G.; Ganzel, B.L.; Slaughter, M.S. Risk Factors and Outcomes in Redo Coronary Artery Bypass Grafting. Heart Lung Circ. 2020, 29, 384–389. [Google Scholar] [CrossRef]
- Zhu, Y.Y.; Hayward, P.A.; Hare, D.L.; Reid, C.; Stewart, A.G.; Buxton, B.F. Effect of lipid exposure on graft patency and clinical outcomes: Arteries and veins are different. Eur. J. Cardio-Thorac. Surg. 2014, 45, 323–328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zou, H.; Hastie, T. Regularization and variable selection via the elastic net. J. R. Stat. Soc Ser. B (Stat. Methodol.) 2005, 67, 301–320. [Google Scholar] [CrossRef] [Green Version]
- Park, J.H.; Shim, J.K.; Song, J.W.; Soh, S.; Kwak, Y.L. Effect of atorvastatin on the incidence of acute kidney injury following valvular heart surgery: A randomized, placebo-controlled trial. Intensive Care Med. 2016, 42, 1398–1407. [Google Scholar] [CrossRef] [PubMed]
- Öztekin, I.; Gökdogan, S.; Öztekin, D.S.; Issever, H.; Göksel, O.; Canik, S. Effects of Propofol and Midazolam on Lipids, Glucose, and Plasma Osmolality during and in the Early Postoperative Period Following Coronary Artery Bypass Graft Surgery: A Randomized Trial. Yakugaku Zasshi 2007, 127, 173–182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schouten, O.; Boersma, E.; Hoeks, S.E.; Benner, R.; van Urk, H.; van Sambeek, M.R.; Verhagen, H.J.; Khan, N.A.; Dunkelgrun, M.; Bax, J.J.; et al. Fluvastatin and perioperative events in patients undergoing vascular surgery. N. Engl. J. Med. 2009, 361, 980–989. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakazawa, M.; Arashi, H.; Yamaguchi, J.; Ogawa, H.; Hagiwara, N. Lower levels of high-density lipoprotein cholesterol are associated with increased cardiovascular events in patients with acute coronary syndrome. Atherosclerosis 2020, 303, 21–28. [Google Scholar] [CrossRef]
- Jin, X.; Chen, H.; Shi, H.; Fu, K.; Li, J.; Tian, L.; Teng, W. Lipid levels and the risk of hemorrhagic stroke: A dose-response meta-analysis. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 23–35. [Google Scholar] [CrossRef]
- Miura, T.; Izawa, A.; Motoki, H.; Miyashita, Y.; Kashima, Y.; Ebisawa, S.; Tomita, T.; Koyama, J.; Ikeda, U. Clinical Impact of Rapid Reduction of Low-Density Lipoprotein Cholesterol Level on Long-Term Outcome of Acute Myocardial Infarction in the Statin Era: Subanalysis of the ALPS-AMI Study. PLoS ONE 2015, 10, e0127835. [Google Scholar] [CrossRef] [Green Version]
- Navarese, E.P.; Robinson, J.G.; Kowalewski, M.; Kolodziejczak, M.; Andreotti, F.; Bliden, K.; Tantry, U.; Kubica, J.; Raggi, P.; Gurbel, P.A. Association Between Baseline LDL-C Level and Total and Cardiovascular Mortality After LDL-C Lowering: A Systematic Review and Meta-analysis. JAMA 2018, 319, 1566–1579. [Google Scholar] [CrossRef]
- Kulik, A.; Abreu, A.M.; Boronat, V.; Ruel, M. Impact of lipid levels and high-intensity statins on vein graft patency after CABG: Midterm results of the ACTIVE trial. J. Card. Surg. 2020, 35, 3286–3293. [Google Scholar] [CrossRef]
- Alkhalil, M. Effects of intensive lipid-lowering therapy on mortality after coronary bypass surgery: A meta-analysis of 7 randomised trials. Atherosclerosis 2020, 293, 75–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farkouh, M.E.; Godoy, L.C.; Brooks, M.M.; Mancini, G.B.J.; Vlachos, H.; Bittner, V.A.; Chaitman, B.R.; Siami, F.S.; Hartigan, P.M.; Frye, R.L.; et al. Influence of LDL-Cholesterol Lowering on Cardiovascular Outcomes in Patients with Diabetes Mellitus Undergoing Coronary Revascularization. J. Am. Coll. Cardiol. 2020, 76, 2197–2207. [Google Scholar] [CrossRef] [PubMed]
- Açıkgöz, E.; Açıkgöz, S.K.; Yaman, B.; Kurtul, A. Lower LDL-cholesterol levels associated with increased inflammatory burden in patients with acute ST-segment elevation myocardial infarction. Rev. Assoc. Med. Bras. 2021, 67, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Bismuth, J.; Kofoed, S.C.; Jensen, A.S.; Sethi, A.; Sillesen, H. Serum lipids act as inverse acute phase reactants and are falsely low in patients with critical limb ischemia. J. Vasc. Surg. 2002, 36, 1005–1010. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feingold, K.R.; Grunfeld, C. The acute phase response inhibits reverse cholesterol transport. J. Lipid Res. 2010, 51, 682–684. [Google Scholar] [CrossRef] [Green Version]
- Gupta, S.C.; Kunnumakkara, A.B.; Aggarwal, S.; Aggarwal, B.B. Inflammation, a Double-Edge Sword for Cancer and Other Age-Related Diseases. Front. Immunol. 2018, 9, 2160. [Google Scholar] [CrossRef]
- Chen, Z.; Bozec, A.; Ramming, A.; Schett, G. Anti-inflammatory and immune-regulatory cytokines in rheumatoid arthritis. Nat. Rev. Rheumatol. 2019, 15, 9–17. [Google Scholar] [CrossRef] [PubMed]
| Demographics and Perioperative Characteristics | All Patients (N = 192) |
|---|---|
| Demographics | |
| Age (y) | 67.0 (60.0; 73.0) |
| Height (cm) | 173 (8.71) |
| Weight (kg) | 80.4 (70.0; 90.1) |
| BMI (kg/m2) | 26.1 (23.7; 30.4) |
| Sex (Male) | 145 (75.5%) |
| Comorbidities | |
| Diabetes (Yes) | 35 (18.2%) |
| Diabetes on insulin | |
| No | 24 (68.6%) |
| Yes | 11 (31.4%) |
| Hypertension† (Yes) | 130 (68.4%) |
| Dyslipidemia† (Yes) | 111 (58.1%) |
| Nicotine† | |
| Former smoker | 49 (26.1%) |
| Non-smoker | 97 (51.6%) |
| Smoker | 42 (22.3%) |
| Obesity (Yes) | 52 (27.1%) |
| Preoperative renal disease (Yes) | 43 (22.4%) |
| Peripheral vascular disease† | |
| No | 167 (93.8%) |
| Stage 1 | 4 (2.25%) |
| Stage 2 | 4 (2.25%) |
| Stage 3 | 1 (0.56%) |
| Stage 4 | 2 (1.12%) |
| Carotid disease† | |
| <50% | 1 (0.58%) |
| >90% | 3 (1.75%) |
| 50–69%, | 9 (5.26%) |
| 70–89% | 2 (1.17%) |
| no | 156 (91.2%) |
| Myocardial infarction† | |
| No MI | 171 (89.5%) |
| MI 0–7 days before operation | 3 (1.57%) |
| MI 8–90 days before operation | 8 (4.19%) |
| MI > 90 days before operation | 9 (4.71%) |
| COPD† (Yes) | 23 (12.1%) |
| NYHA† | |
| 1 | 60 (31.4%) |
| 2 | 90 (47.1%) |
| 3 | 38 (19.9%) |
| 4 | 3 (1.57%) |
| CCS† | |
| 0 | 118 (62.4%) |
| 1 | 34 (18.0%) |
| 2 | 25 (13.2%) |
| 3 | 9 (4.76%) |
| 4 | 3 (1.59%) |
| Ejection fraction† | 60.0 (55.0; 65.0) |
| EuroSCORE2† | 1.73 (0.90; 2.93) |
| Baseline lipid plasma levels | |
| Cholesterol (mmol/L) | 4.42 (1.13) |
| HDL-C (mmol/L) | 1.13 (0.92; 1.35) |
| LDL-C (mmol/L) | 2.68 (2.14; 3.40) |
| Triglycerides (mmol/L) | 1.33 (0.97; 1.88) |
| Perioperative characteristics | |
| Aortic valve surgery (Yes) | 86 (44.8%) |
| Mitral valve surgery (Yes) | 45 (23.4%) |
| Tricuspid valve surgery (Yes) | 17 (8.85%) |
| Coronary artery bypass surgery (Yes) | 77 (40.1%) |
| Ascending aortic surgery (Yes) | 38 (19.8%) |
| Aortic arch surgery (Yes) | 11 (5.73%) |
| ECC or MiECC | |
| ECC | 149 (77.6%) |
| MiECC | 43 (22.4%) |
| Bypass time (min) | 104 (80.0; 132) |
| Aortic cross clamping (min) | 68.5 (52.0; 91.8) |
| Lowest body temperature (deg C) | 33.2 (32.1; 33.8) |
| Deep hypothermic cardiac arrest† (Yes) | 19 (9.95%) |
| Operation duration (min) | 234 (195; 276) |
| Time Point | Cholesterol (mmol/L) | HDL-C (mmol/L) | LDL-C (mmol/L) | Triglycerides (mmol/L) |
|---|---|---|---|---|
| Baseline | 4.1 (3.5–5.1) | 1.2 (1.01.6) | 2.2 (1.7–2.9) | 1.3 (1.0–2.0) |
| Pre-operative | 4.3 (3.7–5.0) | 1.1 (0.9–1.4) | 2.7 (2.1–3.4) | 1.3 (1.0–1.9) |
| Intra-operative | 2.8 (2.33.4) | 0.7 (0.6–0.9) | 1.7 (1.3–2.2) | 0.5 (0.4–0.7) |
| Post-operative | 2.6 (2.2–3.3) | 0.9 (0.8–1.1) | 1.5 (1.1–2.0) | 1.0 (0.7–1.3) |
| P‡ | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| Post-hoc comparisons (d *) | ||||
| Baseline vs. Pre-operative | −0.08 (−0.20, 0.03) † | 0.24 (0.12, 0.35) † | −0.33 (−0.44, −0.22) † | 0.01 (−0.10, 0.13) † |
| Baseline vs. Intra-operative | 0.73 (0.65, 0.79) † | 0.82 (0.75, 0.87) † | 0.33 (0.22, 0.44) † | 0.86 (0.80, 0.90) |
| Baseline vs. Post-operative | 0.74 (0.66, 0.80) † | 0.63 (0.53, 0.70) † | 0.45 (0.35, 0.55) † | 0.41 (0.30, 0.50) † |
| Intra-operative vs. Post-operative | 0.08 (−0.04, 0.19) | −0.39 (−0.49, −0.28) † | 0.17 (0.05, 0.28) † | −0.66 (−0.74, −0.58) † |
| Pre-operative vs. Intra-operative | 0.75 (0.68, 0.82) † | 0.72 (0.64, 0.79) † | 0.66 (0.57, 0.73) † | 0.86 (0.81, 0.90) † |
| Pre-operative vs. Post-operative | 0.77 (0.69, 0.82) † | 0.46 (0.36, 0.55) † | 0.73 (0.65, 0.79) † | 0.40 (0.29, 0.50) † |
| Clinical Outcomes | All Patients |
|---|---|
| 30-day mortality | |
| Died | 2 (1.04%; 0.13%–3.71%) |
| Survived | 190 (98.96%; 96.29%–99.87%) |
| 1-year follow-up | |
| Alive | 179 (96.24%; 92.40%–98.47%) |
| Deceased | 7 (3.76%; 1.53%–7.60%) |
| Hospital length of stay postoperative (days) | 7.00 (6.00; 9.00) |
| Postoperative stroke | |
| No | 179 (94.21%; 89.88%–97.07%) |
| Yes | 11 (5.79%; 2.93%–10.12%) |
| Myocardial infarction | |
| No | 186 (96.88%: 93.32%–98.84%) |
| Yes | 6 (3.12%; 1.16%–6.68%) |
| Logistic Regression (Univariable) | Elastic Net (Multivariable) | |||||
|---|---|---|---|---|---|---|
| Covariate | OR | P | OR (Adjusted) | P | OR | OR (Adjusted) |
| Cholesterol (preop) | 2.12 (1.23−3.82) | 0.008 | 1.48 (0.74−3.17) | 0.284 | 1.25 | 1.13 |
| Cholesterol (∆) | 0.46 (0.20−1.05) | 0.062 | 0.29 (0.07−0.90) | 0.047 | 0.97 | 0.78 |
| HDL-C (preops) | 3.12 (0.45−20.64) | 0.239 | 1.95 (0.15−28.40) | 0.612 | 0.46 | |
| HDL-C (∆) | 0.08 (0.00−1.78) | 0.104 | 0.01 (0.00−0.78) | 0.039 | 0.30 | 0.08 |
| LDL-C (preop) | 2.51 (1.27−5.21) | 0.010 | 1.68 (0.69−4.53) | 0.272 | 1.39 | 1.33 |
| LDL-C-(∆) | 0.27 (0.08−0.91) | 0.035 | 0.19 (0.03−0.88) | 0.045 | 0.86 | 0.67 |
| Triglycerides (preop) | 1.03 (0.44−1.89) | 0.937 | 0.82 (0.28−2.07) | 0.699 | 0.91 | |
| Triglycerides (∆) | 1.2 (0.41−5.28) | 0.777 | 0.91 (0.25−4.14) | 0.890 | 0.92 | |
| Age (y) | 1.07 (1.00−1.16) | 0.102 | 1.04 | |||
| Sex (male) | 1.13 (1.01−1.25) | 0.029 | 0.30 | |||
| BMI (kg/m2) | 0.1 (0.02−0.38) | 0.001 | 1.16 | |||
| Statin (Yes) | 0.08 (0.00−0.41) | 0.015 | 0.22 | |||
| Logistic Regression (Univariable) | Elastic Net | |||||
|---|---|---|---|---|---|---|
| Covariate | OR | P | OR (Adjusted) | P | OR | OR (Adjusted) |
| Cholesterol (preop.) | 0.51 (0.25, 1.01) | 0.058 | 0.45 (0.20, 0.98) | 0.046 | 0.35 | 0.68 |
| Cholesterol (∆) | 1.81 (0.67, 4.64) | 0.220 | 1.8 (0.67, 4.61) | 0.217 | 4.57 | 1.49 |
| HDL-C (preop.) | 1.17 (0.09, 12.14) | 0.900 | 0.8 (0.05, 10.46) | 0.869 | 3.00 | |
| HDL-C (∆) | 0.11 (0.00, 4.79) | 0.233 | 0.15 (0.00, 8.22) | 0.334 | 0.01 | 0.16 |
| LDL-C (preop.) | 0.55 (0.19, 1.39) | 0.239 | 0.5 (0.15, 1.48) | 0.230 | 0.96 | |
| LDL-C (∆) | 0.99 (0.22, 5.14) | 0.992 | 0.96 (0.19, 5.21) | 0.965 | 0.07 | 0.67 |
| Triglycerides (preop.) | 0.97 (0.29, 2.26) | 0.952 | 1.19 (0.33, 3.08) | 0.750 | 3.59 | 1.18 |
| Triglycerides (∆) | 1.13 (0.27, 7.66) | 0.888 | 0.94 (0.19, 6.88) | 0.948 | 2.06 | |
| Age (y) | 1.02 (0.95, 1.12) | 0.585 | ||||
| Sex (Male) | 0.95 (0.79, 1.11) | 0.563 | 0.91 | |||
| BMI (kg/m2) | 0.79 (0.16, 5.66) | 0.783 | 0.98 | |||
| Statin (Yes) | 1.13 (0.24, 5.86) | 0.878 | 0.83 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mihalj, M.; Heinisch, P.P.; Huber, M.; Schefold, J.C.; Hartmann, A.; Walter, M.; Steinhagen-Thiessen, E.; Schmidli, J.; Stüber, F.; Räber, L.; et al. Effect of Perioperative Lipid Status on Clinical Outcomes after Cardiac Surgery. Cells 2021, 10, 2717. https://doi.org/10.3390/cells10102717
Mihalj M, Heinisch PP, Huber M, Schefold JC, Hartmann A, Walter M, Steinhagen-Thiessen E, Schmidli J, Stüber F, Räber L, et al. Effect of Perioperative Lipid Status on Clinical Outcomes after Cardiac Surgery. Cells. 2021; 10(10):2717. https://doi.org/10.3390/cells10102717
Chicago/Turabian StyleMihalj, Maks, Paul Philipp Heinisch, Markus Huber, Joerg C. Schefold, Alexander Hartmann, Michael Walter, Elisabeth Steinhagen-Thiessen, Juerg Schmidli, Frank Stüber, Lorenz Räber, and et al. 2021. "Effect of Perioperative Lipid Status on Clinical Outcomes after Cardiac Surgery" Cells 10, no. 10: 2717. https://doi.org/10.3390/cells10102717
APA StyleMihalj, M., Heinisch, P. P., Huber, M., Schefold, J. C., Hartmann, A., Walter, M., Steinhagen-Thiessen, E., Schmidli, J., Stüber, F., Räber, L., & Luedi, M. M. (2021). Effect of Perioperative Lipid Status on Clinical Outcomes after Cardiac Surgery. Cells, 10(10), 2717. https://doi.org/10.3390/cells10102717







