Bond Strength of Universal Adhesive/Resin Cement Combinations Relying on Touch-Cure Mechanisms
Abstract
1. Introduction
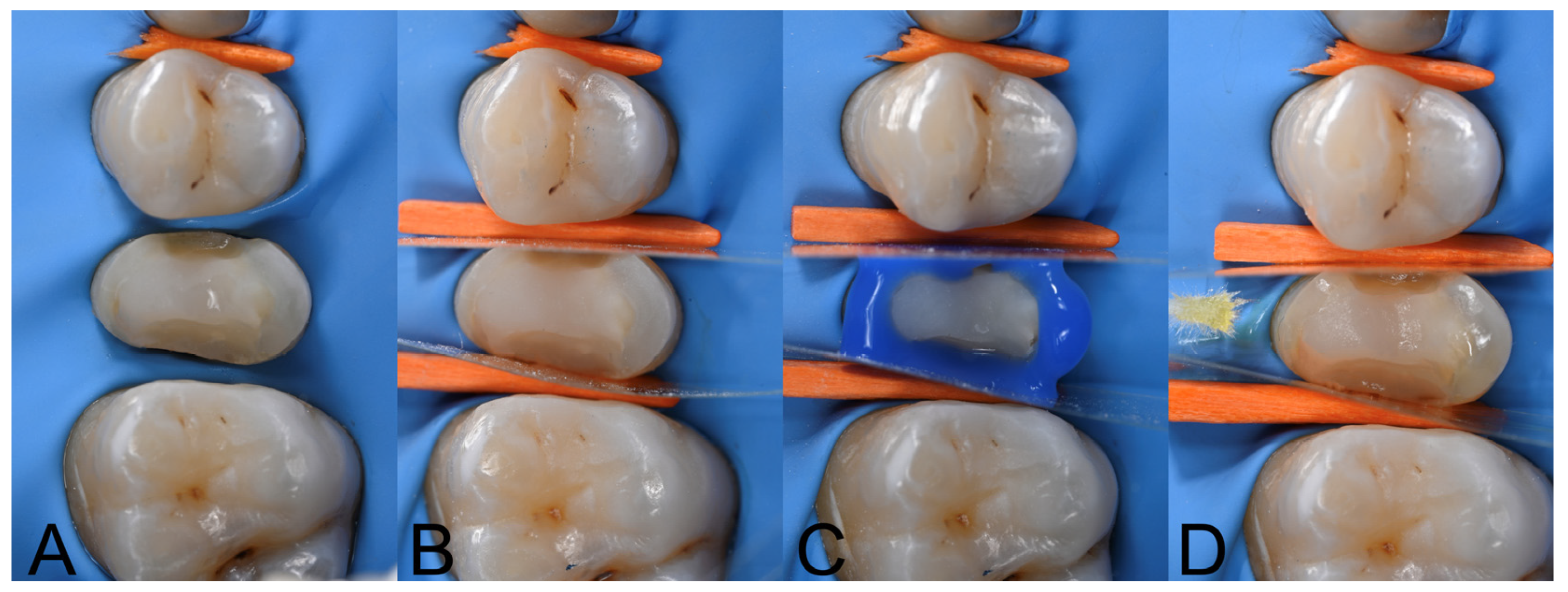
2. Materials and Methods
3. Results
3.1. μShear Bond Strength (μSBS) Testing
3.1.1. μShear Bond Strength to Resin Composite Substrate
3.1.2. μShear Bond Strength to Dentine Substrate
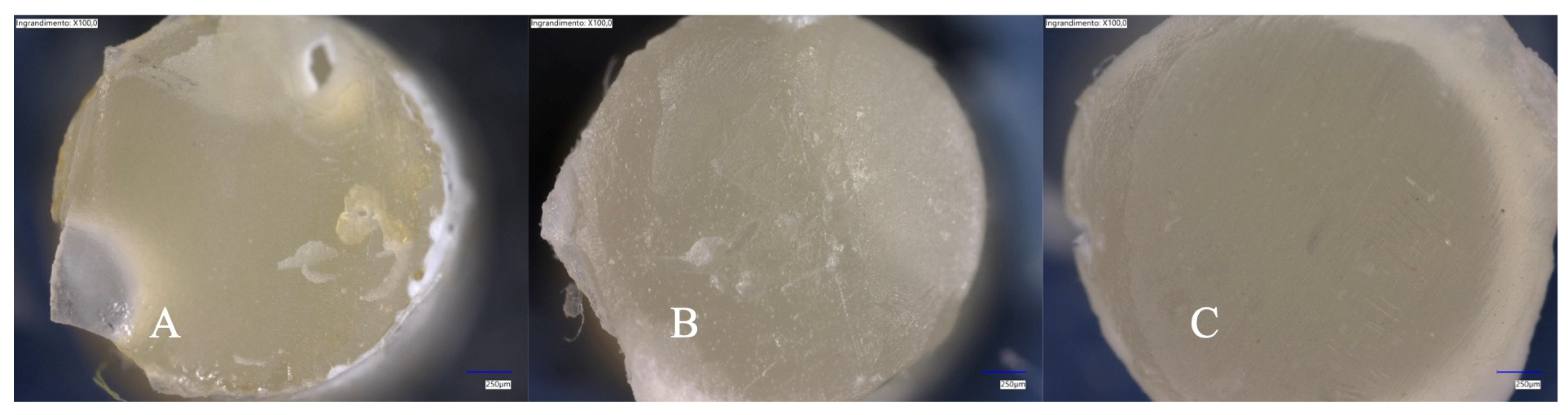
3.2. Failure Mode Analysis and Microscopy
4. Discussion
5. Conclusions
- (1)
- It demonstrated similar bonding performance across different curing modes when bonded to composite resin.
- (2)
- In dentine, light curing increased the initial bond strength.
- (3)
- Self-curing provided stable bond strength after aging.
- (4)
- It benefited from light curing when bonding to the composite resin.
- (5)
- In dentine, the bond strength remained stable with chemical polymerization.
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bresser, R.A.; Hofsteenge, J.W.; Buijs, G.J.; van den Breemer, C.R.G.; Özcan, M.; Cune, M.S.; Gresnigt, M.M.M. Partial Glass-Ceramic Posterior Restorations with Margins beyond or above the Cemento-Enamel Junction: An Observational Retrospective Clinical Study. J. Prosthodont. Res. 2024, 69, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Alberto Jurado, C.; Kaleinikova, Z.; Tsujimoto, A.; Alberto Cortés Treviño, D.; Seghi, R.R.; Lee, D.J. Comparison of Fracture Resistance for Chairside CAD/CAM Lithium Disilicate Crowns and Overlays with Different Designs. J. Prosthodont. 2022, 31, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Opdam, N.J.M.; Frankenberger, R.; Magne, P. From “direct versus Indirect” toward an Integrated Restorative Concept in the Posterior Dentition. Oper. Dent. 2016, 41, S27–S34. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Xu, Y.; Si, L.; Li, X.; Fu, B.; Hannig, M. Long-Term Clinical Performance of Composite Resin or Ceramic Inlays, Onlays, and Overlays: A Systematic Review and Meta-Analysis. Oper. Dent. 2021, 46, 25–44. [Google Scholar] [CrossRef]
- Fathy, H.; Hamama, H.H.; El-Wassefy, N.; Mahmoud, S.H. Clinical Performance of Resin-Matrix Ceramic Partial Coverage Restorations: A Systematic Review. Clin. Oral. Investig. 2022, 26, 3807–3822. [Google Scholar] [CrossRef]
- Lee, Y.; Kim, J.; Shin, Y. Push-out Bond Strength Evaluation of Fiber-Reinforced Composite Resin Post Cemented with Self-Adhesive Resin Cement Using Different Adhesive Bonding Systems. Materials 2021, 14, 3639. [Google Scholar] [CrossRef]
- Miotti, L.L.; Follak, A.C.; Montagner, A.F.; Pozzobon, R.T.; da Silveira, B.L.; Susin, A.H. Is Conventional Resin Cement Adhesive Performance to Dentin Better than Self-Adhesive? A Systematic Review and Meta-Analysis of Laboratory Studies. Oper. Dent. 2020, 45, 484–495. [Google Scholar] [CrossRef]
- Donmez, M.B.; Çakmak, G.; Yılmaz, D.; Schimmel, M.; Abou-Ayash, S.; Yilmaz, B.; Peutzfeldt, A. Bond Strength of Additively Manufactured Composite Resins to Dentin and Titanium When Bonded with Dual-Polymerizing Resin Cements. J. Prosthet. Dent. 2024, 132, 1067.e1–1067.e8. [Google Scholar] [CrossRef]
- Breschi, L.; Maravic, T.; Mazzitelli, C.; Josic, U.; Mancuso, E.; Cadenaro, M.; Pfeifer, C.S.; Mazzoni, A. The Evolution of Adhesive Dentistry: From Etch-and-Rinse to Universal Bonding Systems. Dent. Mater. 2024, 41, 141–158. [Google Scholar] [CrossRef]
- Fehrenbach, J.; Isolan, C.P.; Münchow, E.A. Is the Presence of 10-MDP Associated to Higher Bonding Performance for Self-Etching Adhesive Systems? A Meta-Analysis of in Vitro Studies. Dent. Mater. 2021, 37, 1463–1485. [Google Scholar] [CrossRef]
- Teshima, I. Degradation of 10-Methacryloyloxydecyl Dihydrogen Phosphate. J. Dent. Res. 2010, 89, 1281–1286. [Google Scholar] [CrossRef] [PubMed]
- Cadenaro, M.; Josic, U.; Maravić, T.; Mazzitelli, C.; Marchesi, G.; Mancuso, E.; Breschi, L.; Mazzoni, A. Progress in Dental Adhesive Materials. J. Dent. Res. 2023, 102, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Breschi, L. Buonocore Memorial Lecture 2023: Changing Operative Mindsets with Universal Adhesives and Cements. Oper. Dent. 2025, 50, 12–32. [Google Scholar] [CrossRef] [PubMed]
- Aoki, R.; Takamizawa, T.; Hayashi, K.; Arai, Y.; Ishii, R.; Shoji, M.; Kamimoto, A.; Miyazaki, M. Influence of Different Curing Modes on the Bonding Effectiveness of Self-Adhesive Resin Luting Cements in Combination with Universal Adhesives. Dent. Mater. 2024, 40, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Yoshihara, K.; Nagaoka, N.; Benino, Y.; Nakamura, A.; Hara, T.; Maruo, Y.; Yoshida, Y.; Van Meerbeek, B. Touch-Cure Polymerization at the Composite Cement-Dentin Interface. J. Dent. Res. 2021, 100, 935–942. [Google Scholar] [CrossRef]
- Mazzitelli, C.; Maravic, T.; Josic, U.; Mancuso, E.; Generali, L.; Checchi, V.; Breschi, L.; Mazzoni, A. Effect of Adhesive Strategy on Resin Cement Bonding to Dentin. J. Esthet. Restor. Dent. 2023, 35, 501–507. [Google Scholar] [CrossRef]
- Irie, M.; Okada, M.; Maruo, Y.; Nishigawa, G.; Matsumoto, T. Long-Term Bonding Performance of One-Bottle vs. Two-Bottle Bonding Agents to Lithium Disilicate Ceramics. Polymers 2024, 16, 2266. [Google Scholar] [CrossRef]
- Tang, C.; Mercelis, B.; Ahmed, M.H.; Yoshihara, K.; Peumans, M.; Van Meerbeek, B. Adhesive Performance Assessment of Universal Adhesives and Universal Adhesive/Composite Cement Combinations. J. Adhes. Dent. 2023, 25, 241–256. [Google Scholar] [CrossRef]
- Eggmann, F.; Ayub, J.M.; Conejo, J.; Blatz, M.B. Deep Margin Elevation—Present Status and Future Directions. J. Esthet. Restor. Dent. 2023, 35, 26–47. [Google Scholar] [CrossRef]
- Kadowaki, Y.; Kakuda, S.; Kawano, S.; Katsumata, A.; Ting, S.; Hoshika, S.; Ikeda, T.; Tanaka, T.; Carvalho, R.M.; Sano, H. Bond Performance of “Touch and Cure” Adhesives on Resin Core Systems. Dent. Mater. J. 2016, 35, 386–391. [Google Scholar] [CrossRef]
- Faria-e-Silva, A.L.; Casselli, D.S.M.; Lima, G.S.; Ogliari, F.A.; Piva, E.; Martins, L.R.M. Kinetics of Conversion of Two Dual-Cured Adhesive Systems. J. Endod. 2008, 34, 1115–1118. [Google Scholar] [CrossRef] [PubMed]
- Dimitriadi, M.; Petropoulou, A.; Zinelis, S.; Eliades, G. Degree of Conversion of Dual-Cured Composite Luting Agents: The Effect of Transition Metal-Based Touch-Cure Activators. J. Dent. 2024, 147, 105147. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Shimada, Y.; Sadr, A.; Tabata, T.; Sato, T.; Byun, J.E.; Han, S.H. Degree of Conversion and Interfacial Adaptation of Touch-Cure Resin Cement Polymerized by Self-Curing or Dual-Curing with Reduced Light. Clin. Oral Investig. 2024, 28, 463. [Google Scholar] [CrossRef] [PubMed]
- Aizawa, D.; Hanabusa, M.; Hayakawa, T.; Yamamoto, T. Residual Stresses in Glass Crowns Generated by Polymerization and Water Sorption of Resin Cements. Dent. Mater. J. 2024, 43, 460–468. [Google Scholar] [CrossRef]
- Vrochari, A.D.; Eliades, G.; Hellwig, E.; Wrbas, K.T. Curing Efficiency of Four Self-Etching, Self-Adhesive Resin Cements. Dent. Mater. 2009, 25, 1104–1108. [Google Scholar] [CrossRef]
- Baena, E.; Fuentes, M.V.; Garrido, M.A.; Rodríguez, J.; Ceballos, L. Influence of Post-Cure Time on the Microhardness of Self-Adhesive Resin Cements inside the Root Canal. Oper. Dent. 2012, 37, 548–556. [Google Scholar] [CrossRef]
- Ilie, N.; Simon, A. Effect of Curing Mode on the Micro-Mechanical Properties of Dual-Cured Self-Adhesive Resin Cements. Clin. Oral. Investig. 2012, 16, 505–512. [Google Scholar] [CrossRef]
- Aldhafyan, M.; Silikas, N.; Watts, D.C. Influence of Curing Modes on Conversion and Shrinkage of Dual-Cure Resin-Cements. Dent. Mater. 2022, 38, 194–203. [Google Scholar] [CrossRef]
- Aldhafyan, M.; Silikas, N.; Watts, D.C. Influence of Curing Modes on Monomer Elution, Sorption and Solubility of Dual-Cure Resin-Cements. Dent. Mater. 2022, 38, 978–988. [Google Scholar] [CrossRef]
- Perdigão, J. Current Perspectives on Dental Adhesion: (1) Dentin Adhesion—Not There Yet. Jpn. Dent. Sci. Rev. 2020, 56, 190–207. [Google Scholar] [CrossRef]
- Garberoglio, R.; Brännström, M. Scanning Electron Microscopic Investigation of Human Dentinal Tubules. Arch. Oral Biol. 1976, 21, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, M.; Nagano, F.; Endo, K.; Ohno, H. A Review: Biodegradation of Resin–Dentin Bonds. Jpn. Dent. Sci. Rev. 2011, 47, 5–12. [Google Scholar] [CrossRef]
- Balkaya, H.; Demirbuğa, S. Evaluation of Six Different One-Step Universal Adhesive Systems in Terms of Dentin Bond Strength, Adhesive Interface Characterization, Surface Tension, Contact Angle, Degree of Conversion and Solvent Evaporation after Immediate and Delayed Use. J. Esthet. Restor. Dent. 2023, 35, 479–492. [Google Scholar] [CrossRef] [PubMed]
- Carrilho, E.; Cardoso, M.; Marques Ferreira, M.; Marto, C.M.; Paula, A.; Coelho, A.S. 10-MDP Based Dental Adhesives: Adhesive Interface Characterization and Adhesive Stability—A Systematic Review. Materials 2019, 12, 790. [Google Scholar] [CrossRef]
- Sarahneh, O.; Günal-Abduljalil, B. The Effect of Silane and Universal Adhesives on the Micro-Shear Bond Strength of Current Resin-Matrix Ceramics. J. Adv. Prosthodont. 2021, 13, 292–303. [Google Scholar] [CrossRef]
- Yoshihara, K.; Nagaoka, N.; Sonoda, A.; Maruo, Y.; Makita, Y.; Okihara, T.; Irie, M.; Yoshida, Y.; Van Meerbeek, B. Effectiveness and Stability of Silane Coupling Agent Incorporated in ‘Universal’ Adhesives. Dent. Mater. 2016, 32, 1218–1225. [Google Scholar] [CrossRef]

| Product Name (CODE). Shade. Manufacturer | Composition | Batch Number | Application Mode |
|---|---|---|---|
| ESTECEM II Plus (EP) Universal shade Tokuyama Dental Corp. | Paste A: Bis-GMA 1. TEDGMA 2. Bis-MPEPP 3, peroxide, camphorquinone, silica-zirconia filler (filler load 74% wt) Paste B: Phosphoric acid monomer, Bis-GMA 1, TEGDMA 2, HEMA 4, MTU-6 5, silane coupling agent, peroxide. borate catalysts. acetone. ethanol. purified water. | A055BM | Apply with a mixing tip to the surface restoration. Seat the restoration within 1 min. Remove excess with a brush tip. Light cure for 20 s or more if translucent restorations. Light cure the margins for 20 s or more and allow to set for 8 min. |
| Variolink Esthetic DC (VAR) Neutral shade Ivoclar | UDMA 6, methycrilates, ytterbium trifluoride, spheroid mixed oxide, initiators, stabilizer, pigments and other ingredients | Z02YW3 | Apply with a mixing tip to the surface restoration. Seat the restoration. Remove excess. Cover the margins with glycerine. Photopolimerize (10–20 s x mm ceramic and segment). |
| Tokuyama Universal Bond II (TUB) Tokuyama Dental Corp. | Phosphoric acid monomer (new 3D-SR monomer 7), Bis-GMA 1, TEGDMA 2, HEMA 4, MTU-6 5, silane coupling agent. Peroxide, borate catalyst, acetone, ethanol and purified water. | Bond A: (003M1) Bond B: (502BM1) | Mix one drop of bond A and bond B into mixing well or disposable mixing well until it turns green. Apply within 1 min (mixing well) or 3 min (disposable mixing well). Air dry within 30 s of application. |
| Adhese Universal DC (ADH) single dose (Ivoclar) | Methacrylates, ethanol, water, dispersed silicon dioxide, initiators, stabilizers. Applicator coated with co-initiators. | Z027G5 | Remove the green applicator brush from tis chamber. Mix the adhesive with the co-initiator for 5 s by twisting the applicator until it turns yellow. Scrub the surface for 20 s. Once activated, the adhesive can be used for approx. 120 s. Air dry until glossy, immobile film layer results. Polymerization: light cure for 10 s or self-cured if combines with VAR. |
| Estelite posterior PA3 shade (Tokuyama Dental Corp.) | Bis-GMA 1, TEGDMA 2, Bis-MPEPP 3, 84% wt silica-zirconia filler (mean particle size: 2 μm, particle size range: 0.1 to 10 μm). Radical-Amplified Photopolymerization initiator technology (RAP) | W3723 | Place on increments 1.8–2 mm. Photopolymerize 5–10 s if using a LED unit |
| Experimental Group | Composite | Dentine | ||
|---|---|---|---|---|
| T0 (SD) | TC (SD) | T0 (SD) | TC (SD) | |
| TUB/EP LC | 29.3 (5.8) AB,a | 17.0 (5.7) C,b | 31.2 (12.6) A,a | 8.8 (4.4) B,b |
| TUB/EP SC | 33.2 (7.5) A,a | 32.7 (7.5) A,a | 20.5 (6.7) B,a | 13.3 (6.9) AB,a |
| ADH/VAR LC | 27.4 (6.9) AB,a | 25.9 (5.9) B,a | 23.3 (8.6) AB,a | 12.5 (4.6) AB,b |
| ADH/VAR SC | 26.3 (7.7) B,a | 17.4 (7.8) C,b | 19.5 (7.4) B,a | 19.1 (4.7) A,a |
| Composite | Dentine | ||
|---|---|---|---|
| Experimental Group | Aging | A/C/M | A/C/M |
| TUB/EP LC | T0 | 0/0/100 | 50/0/50 |
| TC | 15/0/85 | 69/0/31 | |
| TUB/EP SC | T0 | 0/0/100 | 67/0/33 |
| TC | 7/0/93 | 27/0/73 | |
| ADH/VAR LC | T0 | 0/0/100 | 47/0/53 |
| TC | 0/0/100 | 80/0/20 | |
| ADH/VAR SC | T0 | 0/0/100 | 73/0/27 |
| TC | 47/0/53 | 53/0/47 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Forte, A.; Baena, E.; Mazzitelli, C.; Mancuso, E.; D’Urso, D.; Pellegrino, G.; Ceballos, L.; Breschi, L.; Mazzoni, A.; Maravic, T. Bond Strength of Universal Adhesive/Resin Cement Combinations Relying on Touch-Cure Mechanisms. Polymers 2025, 17, 1224. https://doi.org/10.3390/polym17091224
Forte A, Baena E, Mazzitelli C, Mancuso E, D’Urso D, Pellegrino G, Ceballos L, Breschi L, Mazzoni A, Maravic T. Bond Strength of Universal Adhesive/Resin Cement Combinations Relying on Touch-Cure Mechanisms. Polymers. 2025; 17(9):1224. https://doi.org/10.3390/polym17091224
Chicago/Turabian StyleForte, Annamaria, Eugenia Baena, Claudia Mazzitelli, Edoardo Mancuso, Diego D’Urso, Gerardo Pellegrino, Laura Ceballos, Lorenzo Breschi, Annalisa Mazzoni, and Tatjana Maravic. 2025. "Bond Strength of Universal Adhesive/Resin Cement Combinations Relying on Touch-Cure Mechanisms" Polymers 17, no. 9: 1224. https://doi.org/10.3390/polym17091224
APA StyleForte, A., Baena, E., Mazzitelli, C., Mancuso, E., D’Urso, D., Pellegrino, G., Ceballos, L., Breschi, L., Mazzoni, A., & Maravic, T. (2025). Bond Strength of Universal Adhesive/Resin Cement Combinations Relying on Touch-Cure Mechanisms. Polymers, 17(9), 1224. https://doi.org/10.3390/polym17091224













