Crystal Form Investigation and Morphology Control of Salbutamol Sulfate via Spherulitic Growth
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Antisolvent Crystallization Experiments
2.3. Preparation of Salbutamol Sulfate Solvate
2.4. Powder X-Ray Diffraction (PXRD)
2.5. Optical Polarizing Microscopy and Scanning Electron Microscopy (SEM)
2.6. Thermal Analysis
2.7. Single-Crystal X-Ray Diffraction (SCXRD)
3. Results and Discussion
3.1. Powder X-Ray Diffraction Analysis
3.2. TGA and DSC Analysis
3.3. Crystal Structure of Salbutamol Sulfate Solvate
3.4. Spherical Crystallization
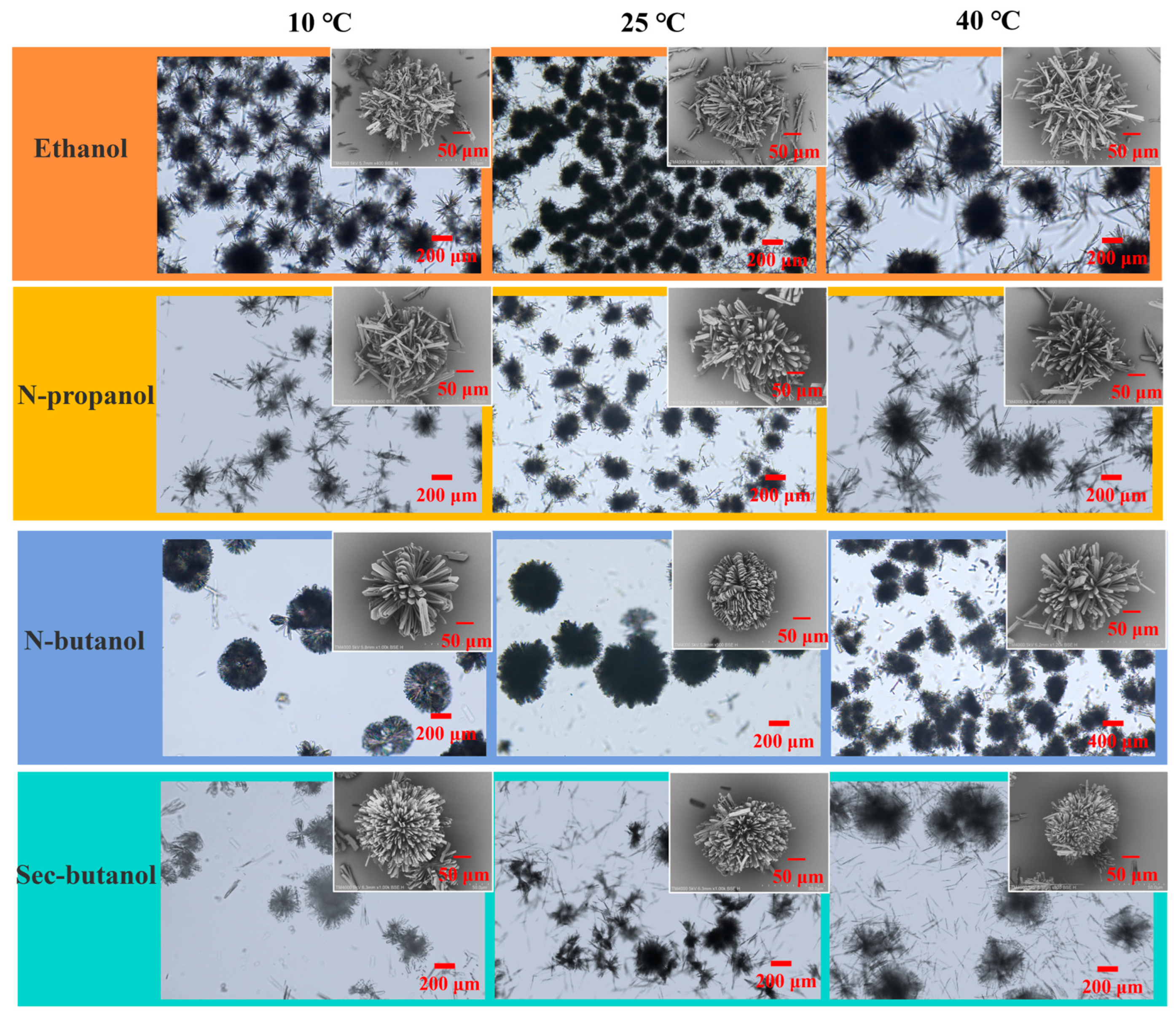
3.4.1. Effect of Antisolvent Type and Temperature
3.4.2. Effect of Volume Ratio of Antisolvent to Solvent
3.4.3. Effect of Solute Concentration
3.4.4. Effect of Feeding Rate and Stirring Speed
3.5. Spherulitic Growth Pattern of Salbutamol Sulfate
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- ter Horst, J.H.; Sefcik, J.; Simone, E. The Future of Industrial Crystallization. Cryst. Growth Des. 2024, 24, 8667–8668. [Google Scholar] [CrossRef]
- Li, B. Structure transition in Cu crystallization. Phys. Scr. 2023, 98, 045916. [Google Scholar] [CrossRef]
- Bhargava, N.; Mor, R.S.; Kumar, K.; Sharanagat, V.S. Advances in application of ultrasound in food processing: A review. Ultrason. Sonochemistry 2021, 70, 105293. [Google Scholar] [CrossRef] [PubMed]
- Thapa, P.; Tripathi, J.; Jeong, S.H. Recent trends and future perspective of pharmaceutical wet granulation for better process understanding and product development. Powder Technol. 2019, 344, 864–882. [Google Scholar] [CrossRef]
- Ma, Y.; Sun, M.; Liu, Y.; Chen, M.; Wu, S.; Wang, M.; Wang, L.; Gao, Z.; Han, D.; Liu, L.; et al. Design of Spherical Crystallization of Active Pharmaceutical Ingredients via a Highly Efficient Strategy: From Screening to Preparation. ACS Sustain. Chem. Eng. 2021, 9, 9018–9032. [Google Scholar] [CrossRef]
- Wang, J.; Cao, W.; Wang, J.; Zhu, L. A Novel Spherical Crystallization Method Using Pickering Emulsions. J. Pharm. Sci. 2022, 111, 1625–1632. [Google Scholar] [CrossRef] [PubMed]
- Shtukenberg, A.G.; Tan, M.; Vogt-Maranto, L.; Chan, E.J.; Xu, W.; Yang, J.; Tuckerman, M.E.; Hu, C.T.; Kahr, B. Melt Crystallization for Paracetamol Polymorphism. Cryst. Growth Des. 2019, 19, 4070–4080. [Google Scholar] [CrossRef]
- Trueman, M.; Akporiaye, D.; Anderson, M.W. Simulating intergrowth formation in zeolite crystals: Impact on habit and functionality. Faraday Discuss. 2022, 235, 343–361. [Google Scholar] [CrossRef] [PubMed]
- Qu, H.; Li, Z.; Zhang, G.; Zhou, Z.; Wu, S. Tuning the physicochemical properties of axitinib by crystallization: Preparation, calculation and Structure-property relationship. J. Ind. Eng. Chem. 2023, 124, 570–578. [Google Scholar] [CrossRef]
- Li, L.; Ji, X.; Cheng, X.; Li, D.; Wang, T.; Huang, X.; Wang, N.; Yin, Q.; Hao, H. Effect of the solvent on the morphology of sulfamerazine crystals and its molecular mechanism. CrystEngComm 2022, 24, 5497–5506. [Google Scholar] [CrossRef]
- Dutt, B.; Choudhary, M.; Budhwar, V. Enhancement of stability profile of aspirin through cocrystallization technique. Res. J. Pharm. Technol. 2022, 15, 768–772. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, S.; Li, J.; Guo, S.; Yan, H.; Li, K.; Tong, L.; Gao, Y.; Li, T.; Chen, M.; et al. Preparation of ethyl vanillin spherical particles with functions of sustained release and anti-caking by an organic solvent-free process. Food Chem. 2023, 402, 134518. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Tan, Z.; Yang, D.; Tu, J.; Wang, Y.; Zhang, Y.; Liu, Y.; Gan, G. Improving the Solubility of Aripiprazole by Multicomponent Crystallization. Crystals 2021, 11, 343. [Google Scholar] [CrossRef]
- Sun, M.; Bi, J.; Zhao, Y.; Gong, J. Particle Design of Drugs via Spherical Crystallization: A Review from Fundamental Aspects to Technology Development. Cryst. Growth Des. 2024, 24, 2266–2287. [Google Scholar] [CrossRef]
- Chen, K.; Hou, B.; Wu, H.; Huang, X.; Li, F.; Xiao, Y.; Li, J.; Bao, Y.; Hao, H. Hollow and Solid Spherical Azithromycin Particles Prepared by Different Spherical Crystallization Technologies for Direct Tableting. Processes 2019, 7, 276. [Google Scholar] [CrossRef]
- Gupta, M.; Chatterjee, A.; Srivastava, B. Spherical crystallization: A technique use to reform solubility and flow property of active pharmaceutical ingredients. Int. J. Pharm. Investig. 2017, 7, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Xue, Z.-H.; Xu, R.; Qin, J.; Wang, Z.; Liu, Y.; Yan, Q.-L. Desensitization of spherical CL-20 composites by embedding insensitive nanosized energetic crystals. CrystEngComm 2024, 26, 5617–5631. [Google Scholar] [CrossRef]
- Xing, X.; Ouyang, J.; Guo, S.; Chen, M.; Gao, Z.; He, F.; Zhou, L.; Xie, Z. Spherical particles design of vanillin via crystallization method: Preparation, characterization and mechanism. Sep. Purif. Technol. 2023, 314, 123622. [Google Scholar] [CrossRef]
- Yan, H.; Liu, Y.; Peng, H.; Li, K.; Li, C.; Jiang, S.; Chen, M.; Han, D.; Gong, J. Improving calcium citrate food functions through spherulitic growth in reactive crystallization and a mechanism study. Food Chem. 2023, 404, 134550. [Google Scholar] [CrossRef] [PubMed]
- Kawashima, Y.; Okumura, M.; Takenaka, H. Spherical Crystallization: Direct Spherical Agglomeration of Salicylic Acid Crystals During Crystallization. Science 1982, 216, 1127–1128. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Yu, C.; Feng, S.; Wei, J.; Tong, L.; Li, K.; Gao, Y.; Zhao, P.; Li, T.; Chen, M.; et al. Enabling the drug combination of celecoxib through a spherical co-agglomeration strategy with controllable and stable drug content and good powder properties. Int. J. Pharm. 2022, 626, 122180. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Feng, S.; Yu, C.; Liu, Y.; Chen, M.; Gong, J. Sustainable preparation of spherical amphoteric organics:Isoelectric point-spherical agglomeration technology. Powder Technol. 2022, 407, 117645. [Google Scholar] [CrossRef]
- Guo, S.; Feng, S.; Yu, C.; Liu, Y.; Li, K.; Chen, M.; Han, D.; Gong, J. Design of spherical agglomerates via crystallization with a non-toxic bridging liquid: From mechanism to application. Powder Technol. 2022, 408, 117725. [Google Scholar] [CrossRef]
- Chen, H.; Wang, C.; Kang, H.; Zhi, B.; Haynes, C.L.; Aburub, A.; Sun, C.C. Microstructures and pharmaceutical properties of ferulic acid agglomerates prepared by different spherical crystallization methods. Int. J. Pharm. 2020, 574, 118914. [Google Scholar] [CrossRef] [PubMed]
- Jin, S.; Chen, M.; Li, Z.; Wu, S.; Du, S.; Xu, S.; Rohani, S.; Gong, J. Design and mechanism of the formation of spherical KCl particles using cooling crystallization without additives. Powder Technol. 2018, 329, 455–462. [Google Scholar] [CrossRef]
- Wang, X.; Li, Z.; Zhang, C.; Wen, T.; Zhou, Y.; Ouyang, J. Designing Spherical Particles of Arbidol Hydrochloride via Spherical Crystallization: Preparation and Characterization. Ind. Eng. Chem. Res. 2024, 63, 5249–5260. [Google Scholar] [CrossRef]
- Wang, Y.; Du, S.; Wang, X.; Sun, M.; Yang, Y.; Gong, J. Spherulitic growth and morphology control of lithium carbonate: The stepwise evolution of core-shell structures. Powder Technol. 2019, 355, 617–628. [Google Scholar] [CrossRef]
- Cui, P.; Yang, W.; Jia, L.; Zhou, L.; Zhang, M.; Bao, Y.; Xie, C.; Hou, B.; Yin, Q. Spherulitic Growth Strategy for Agitation-Induced Formation of Spherical Amoxicillin Sodium Products. Ind. Eng. Chem. Res. 2022, 61, 9821–9832. [Google Scholar] [CrossRef]
- Cullum, V.A.; Farmer, J.; Jack, D.; Levy, G. Salbutamol: A new, selective β-adrenoceptive receptor stimulant. Br. J. Pharmacol. 1969, 35, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Sawale, A.V.; Muneshwar, S.D.; Honale, V.S. Formulation and Evaluation of Oral Soft Jelly Containing Salbutamol Sulphate for the Treatment of Asthma. J. Drug Deliv. Ther. 2023, 13, 118–124. [Google Scholar] [CrossRef]
- Montuschi, P.; Ciabattoni, G. Bronchodilating Drugs for Chronic Obstructive Pulmonary Disease: Current Status and Future Trends. J. Med. Chem. 2015, 58, 4131–4164. [Google Scholar] [CrossRef] [PubMed]
- Vorobei, A.M.; Pokrovskiy, O.I.; Ustinovich, K.B.; Parenago, O.O.; Lunin, V.V.; Miroshnichenko, A.G. Micronization of Salbutamol Sulfate by Supercritical Antisolvent Precipitation: The Effect of Process Parameters on the Size and Morphology of Particles. Russ. J. Phys. Chem. B 2018, 12, 1240–1248. [Google Scholar] [CrossRef]
- Tahara, K.; O’Mahony, M.; Myerson, A.S. Continuous Spherical Crystallization of Albuterol Sulfate with Solvent Recycle System. Cryst. Growth Des. 2015, 15, 5149–5156. [Google Scholar] [CrossRef]
- Nocent, M.; Bertocchi, L.; Espitalier, F.; Baron, M.; Couarraze, G. Definition of a solvent system for spherical crystallization of salbutamol sulfate by quasi-emulsion solvent diffusion (QESD) method. J. Pharm. Sci. 2001, 90, 1620–1627. [Google Scholar] [CrossRef] [PubMed]
- Leger, J.M.; Goursolle, M.; Gadret, M.; Carpy, A. Structure cristalline du sulfate de salbutamol [tert-butylamino-2 (hydroxy-4 hydroxymethyl-3 phenyl)-1 ethanol.0.5H2SO4]. Acta Crystallogr. Sect. B 1978, 34, 1203–1208. [Google Scholar] [CrossRef]
- Shaikh, T.R.; Shelke, N.; Tothadi, S. Multicomponent Solvate Crystals of 3, 5-Dinitrobenzoic Acid and Acetamide and CSD Analysis of Solvates. ACS Omega 2023, 8, 24644–24653. [Google Scholar] [CrossRef] [PubMed]
- Sheldrick, G.M. Crystal structure refinement with SHELXL. Cryst. Struct. Commun. 2015, 71, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Dolomanov, O.V.; Bourhis, L.J.; Gildea, R.J.; Howard, J.A.K.; Puschmann, H. OLEX2: A complete structure solution, refinement and analysis program. J. Appl. Crystallogr. 2009, 42, 339–341. [Google Scholar] [CrossRef]
- Varun, N.; Ghoroi, C. Engineered inhalable micro-balloon shaped drug particles for carrier-free dry powder inhalation (DPI) application. Powder Technol. 2022, 408, 117705. [Google Scholar] [CrossRef]
- Sonvico, F.; Coleman, V.; Traini, D.; Young, P.M. Evolved gas analysis during thermal degradation of salbutamol sulphate. J. Therm. Anal. Calorim. 2015, 120, 789–794. [Google Scholar] [CrossRef]
- Felix, F.S.; Cides da Silva, L.C.; Angnes, L.; Matos, J.R. Thermal behavior study and decomposition kinetics of salbutamol under isothermal and non-isothermal conditions. J. Therm. Anal. Calorim. 2009, 95, 877–880. [Google Scholar] [CrossRef]
- Widauer, A.; Petrick, T.L.; Braun, D.E. Comprehensive Insights into Sulfaguanidine in the Solid State: An Experimental and Computational Study. Cryst. Growth Des. 2024, 24, 1438–1457. [Google Scholar] [CrossRef] [PubMed]
- Trimdale-Deksne, A.; Grante, I.; Mishnev, A.; Orola, L.; Bērziṇš, A. Similarity and Differences of Dasatinib Solvates: A Crystallographic Perspective. Cryst. Growth Des. 2024, 24, 5014–5026. [Google Scholar] [CrossRef]
- Li, J.; Yang, R.; Zeng, T.; Hu, J.; Tang, W.; Liu, Z.; Gong, L. Preparation and growth mechanism of micro spherical ammonium dinitramide crystal based on ultrasound-assisted solvent-antisolvent method. Ultrason. Sonochemistry 2021, 78, 105716. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Yan, Q.; Liu, Y.; Hu, C. Study on the regulation mechanism of effective glass transition temperature on the crystallization of crystalline solid dispersion. Drug Deliv. Transl. Res. 2023, 13, 2677–2689. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.R.; Ramkrishna, D. Dispersions in crystal nucleation and growth rates: Implications of fluctuation in supersaturation. Chem. Eng. Sci. 2014, 107, 102–113. [Google Scholar] [CrossRef]








| SS [35] | S-SBA | |
|---|---|---|
| formula | C13H23NO7S | 2(C13H22NO3)·2(C4H10O)·O4S |
| formula wt | 337.39 | 724.93 |
| cryst system | monoclinic | monoclinic |
| space group | Cc | C2 |
| a (Å) | 28.069 (5) | 28.0008 (14) |
| b (Å) | 6.183 (1) | 6.1365 (3) |
| c (Å) | 16.914 (2) | 11.4303 (6) |
| α (°) | 90 | 90 |
| β (°) | 81.19 (1) | 100.381 (3) |
| γ (°) | 90 | 90 |
| V (Å3) | 2900.8 | 1931.88 (17) |
| Z | 8 | 2 |
| Temp (K) | 295 | 193 |
| R1 | 0.0670 | 0.0413 (3934) |
| wR2 | 0.0670 | 0.1090 (3999) |
| CCDC no. | 1254453 | 2449793 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qiu, X.; Li, H.; Du, Y.; Chen, X.; Du, S.; Wang, Y.; Xue, F. Crystal Form Investigation and Morphology Control of Salbutamol Sulfate via Spherulitic Growth. Crystals 2025, 15, 651. https://doi.org/10.3390/cryst15070651
Qiu X, Li H, Du Y, Chen X, Du S, Wang Y, Xue F. Crystal Form Investigation and Morphology Control of Salbutamol Sulfate via Spherulitic Growth. Crystals. 2025; 15(7):651. https://doi.org/10.3390/cryst15070651
Chicago/Turabian StyleQiu, Xinyue, Hongcheng Li, Yanni Du, Xuan Chen, Shichao Du, Yan Wang, and Fumin Xue. 2025. "Crystal Form Investigation and Morphology Control of Salbutamol Sulfate via Spherulitic Growth" Crystals 15, no. 7: 651. https://doi.org/10.3390/cryst15070651
APA StyleQiu, X., Li, H., Du, Y., Chen, X., Du, S., Wang, Y., & Xue, F. (2025). Crystal Form Investigation and Morphology Control of Salbutamol Sulfate via Spherulitic Growth. Crystals, 15(7), 651. https://doi.org/10.3390/cryst15070651







