Importance of Diversity, Equity, and Inclusion in the Hepatopancreatobiliary Workforce
Abstract
Simple Summary
Abstract
1. Introduction: Defining the Problem
1.1. Characterizing the Problem—Recruitment and Retention of a Diverse HPB Workforce
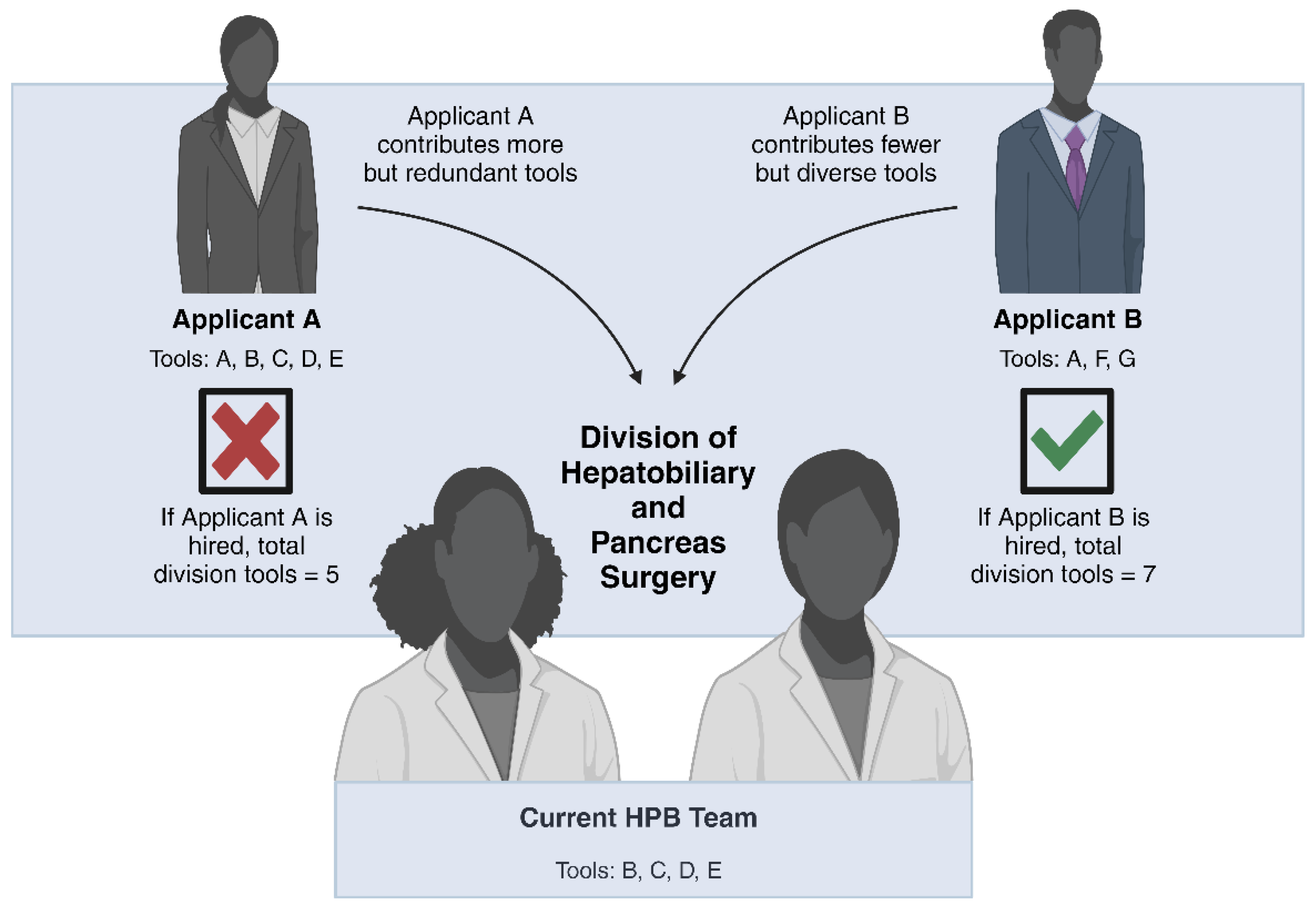
1.2. The Importance of Diversity in the HPB Surgery Workforce
1.3. Surgical Referral Patterns
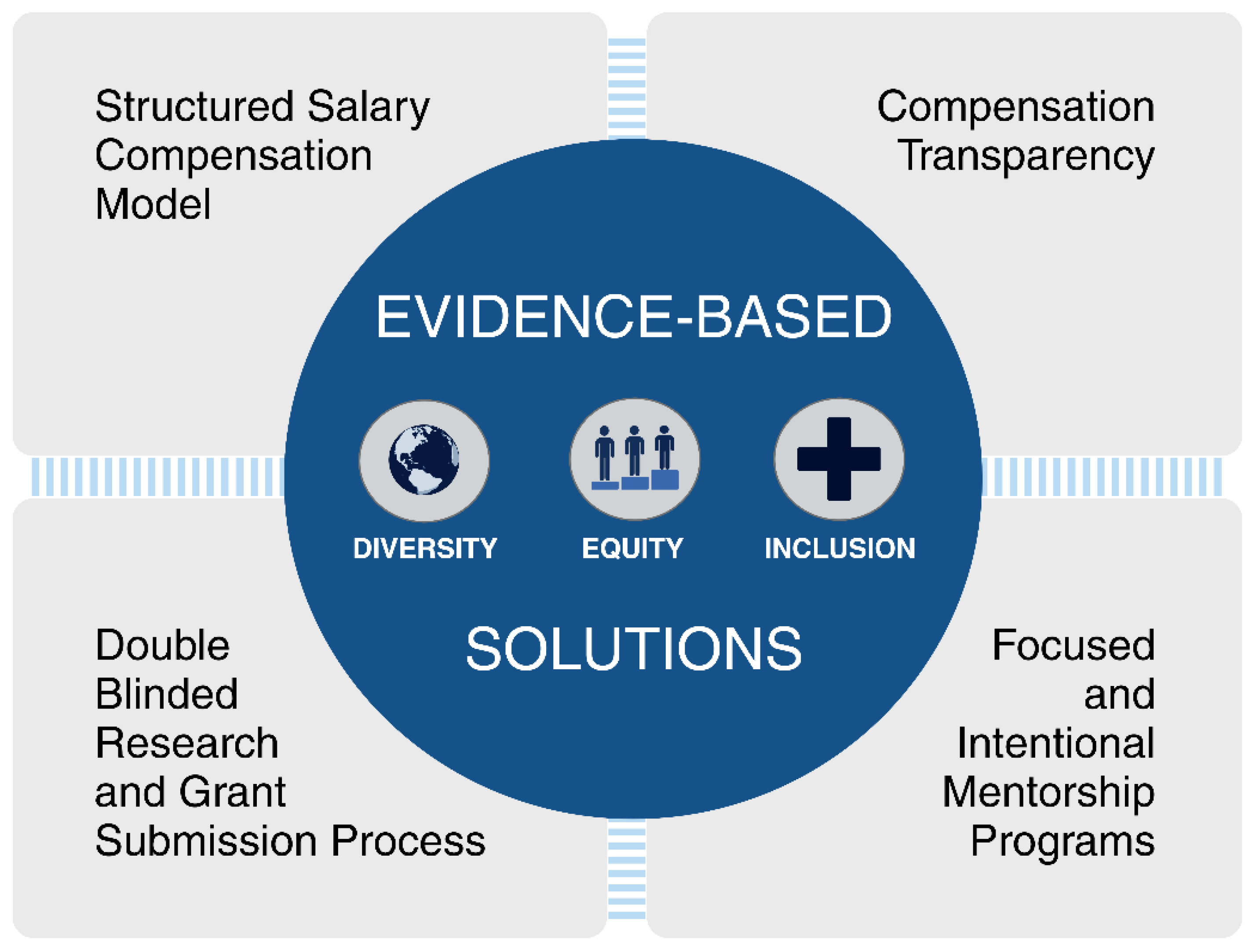
2. Discussion: Identifying Solutions
2.1. Evidence-Based Solutions: Workforce
2.2. Evidence-Based Solutions: Patient Care
3. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health—Final Report of the Commission on Social Determinants of Health. Available online: https://www.who.int/publications-detail-redirect/WHO-IER-CSDH-08.1 (accessed on 9 September 2023).
- Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care; Smedley, B.D., Stith, A.Y., Nelson, A.R., Eds.; National Academies Press (US): Washington, DC, USA, 2003.
- Wilbur, K.; Snyder, C.; Essary, A.C.; Reddy, S.; Will, K.K. Mary Saxon Developing Workforce Diversity in the Health Professions: A Social Justice Perspective. Health Prof. Educ. 2020, 6, 222–229. [Google Scholar] [CrossRef]
- Rotenstein, L.S.; Reede, J.Y.; Jena, A.B. Addressing Workforce Diversity—A Quality-Improvement Framework. N. Engl. J. Med. 2021, 384, 1083–1086. [Google Scholar] [CrossRef]
- Lett, E.; Murdock, H.M.; Orji, W.U.; Aysola, J.; Sebro, R. Trends in Racial/Ethnic Representation Among US Medical Students. JAMA Netw. Open 2019, 2, e1910490. [Google Scholar] [CrossRef] [PubMed]
- Jarman, B.T.; Borgert, A.J.; Kallies, K.J.; Joshi, A.R.T.; Smink, D.S.; Sarosi, G.A.; Chang, L.; Green, J.M.; Greenberg, J.A.; Melcher, M.L.; et al. Underrepresented Minorities in General Surgery Residency: Analysis of Interviewed Applicants, Residents, and Core Teaching Faculty. J. Am. Coll. Surg. 2020, 231, 54–58. [Google Scholar] [CrossRef] [PubMed]
- NEW! NRMP Publishes Research Brief about Applicant Demographic Data Collection. Available online: https://www.nrmp.org/about/news/2023/02/new-nrmp-publishes-research-brief-about-applicant-demographic-data-collection/ (accessed on 9 September 2023).
- Ruff, S.; Ilyas, S.; Steinberg, S.M.; Tatalovich, Z.; McLaughlin, S.A.; D’Angelica, M.; Raut, C.P.; Delman, K.A.; Hernandez, J.M.; Davis, J.L. Survey of Surgical Oncology Fellowship Graduates 2005–2016: Insight into Initial Practice. Ann. Surg. Oncol. 2019, 26, 1622–1628. [Google Scholar] [CrossRef]
- Yheulon, C.G.; Cole, W.C.; Ernat, J.J.; Davis, S.S. Normalized Competitive Index: Analyzing Trends in Surgical Fellowship Training Over the Past Decade (2009–2018). J. Surg. Educ. 2020, 77, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Collins, R.A.; Sheriff, S.A.; Yoon, C.; Cobb, A.N.; Kothari, A.N.; Newman, L.A.; Dossett, L.A.; Willis, A.I.; Wong, S.L.; Clarke, C.N. Assessing the Complex General Surgical Oncology Pipeline: Trends in Race and Ethnicity among US Medical Students, General Surgery Residents, and Complex General Surgical Oncology Trainees. Ann. Surg. Oncol. 2023, 30, 4579–4586. [Google Scholar] [CrossRef]
- Valbuena, V.S.M.; Obayemi, J.E.; Purnell, T.S.; Scantlebury, V.P.; Olthoff, K.M.; Martins, P.N.; Higgins, R.S.; Blackstock, D.M.; Dick, A.A.S.; Watkins, A.C.; et al. Gender and Racial Disparities in the Transplant Surgery Workforce. Curr. Opin. Organ. Transpl. 2021, 26, 560–566. [Google Scholar] [CrossRef]
- Romero-Hernandez, F.; Miller, P.; Mora, R.V.; Hughes, D.; Warner, S.; Alseidi, A.; Visser, B.; Babicky, M. AHPBA SWOT Taskforce AHPBA Graduated Fellows’ Assessments of Strengths, Weaknesses, Opportunities and Threats Facing Fellowship Training in HPB Surgery: “HPB Training Excellence Means Volume, Knowledge, and Mentorship”. HPB 2022, 24, 2063–2071. [Google Scholar] [CrossRef]
- Jackson, T.; Lim, J.S.; Nagatomo, K.; Darwish, M.; Cho, E.E.; Osman, H.; Jeyarajah, D.R. Investigating Factors at Play in Hepatopancreatobiliary Fellowship Selection: Beliefs versus Reality. World J. Surg. 2021, 45, 2556–2566. [Google Scholar] [CrossRef]
- Susanne, G.; Warner, M.D.; Cristina R Ferrone, M.D.; Rebecca, M.; Minter, M.D. HPB Heroines. In AHPBA: The First 25 Years—Chapter 29; AHPBA: Prairie Village, KS, USA, 2020. [Google Scholar]
- Zhu, K.; Das, P.; Karimuddin, A.; Tiwana, S.; Siddiqi, J.; Khosa, F. Equity, Diversity, and Inclusion in Academic American Surgery Faculty: An Elusive Dream. J. Surg. Res. 2021, 258, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Riner, A.N.; Herremans, K.M.; Neal, D.W.; Johnson-Mann, C.; Hughes, S.J.; McGuire, K.P.; Upchurch, G.R.; Trevino, J.G. Diversification of Academic Surgery, Its Leadership, and the Importance of Intersectionality. JAMA Surg. 2021, 156, 748–756. [Google Scholar] [CrossRef] [PubMed]
- Rengers, T.; Ubl, D.; Habermann, E.; Cleary, S.P.; Thiels, C.A.; Warner, S.G. Supply and Demand of Hepatopancreatobiliary Surgeons in the United States. HPB 2023. [Google Scholar] [CrossRef]
- Nguyen, M.; Chaudhry, S.I.; Desai, M.M.; Chen, C.; Mason, H.R.C.; McDade, W.A.; Fancher, T.L.; Boatright, D. Association of Sociodemographic Characteristics With US Medical Student Attrition. JAMA Intern. Med. 2022, 182, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.; Chaudhry, S.I.; Desai, M.M.; Hajduk, A.M.; McDade, W.A.; Fancher, T.L.; Boatright, D. Rates of Medical Student Placement Into Graduate Medical Education by Sex, Race and Ethnicity, and Socioeconomic Status, 2018–2021. JAMA Netw. Open 2022, 5, e2229243. [Google Scholar] [CrossRef] [PubMed]
- Haruno, L.S.; Chen, X.; Metzger, M.; Lin, C.A.; Little, M.T.M.; Kanim, L.E.A.; Poon, S.C. Racial and Sex Disparities in Resident Attrition Among Surgical Subspecialties. JAMA Surg. 2023, 158, 368–376. [Google Scholar] [CrossRef] [PubMed]
- Iwai, Y.; Yu, A.Y.L.; Thomas, S.M.; Downs-Canner, S.; Beasley, G.M.; Sudan, R.; Fayanju, O.M. At the Intersection of Intersectionality: Race and Gender Diversity among Surgical Faculty and Trainees. Ann. Surg. 2024, 279, 77–87. [Google Scholar] [CrossRef]
- Lund, S.; MacArthur, T.; Watkins, R.; Alva-Ruiz, R.; Thiels, C.A.; Smoot, R.L.; Cleary, S.P.; Warner, S.G. Checking Our Blind Spots: Examining Characteristics of Interviewees Versus Matriculants to a Hepatopancreatobiliary Surgical Fellowship Program. J. Surg. Educ. 2023, 80, 1582–1591. [Google Scholar] [CrossRef]
- Siotos, C.; Payne, R.M.; Stone, J.P.; Cui, D.; Siotou, K.; Broderick, K.P.; Rosson, G.D.; Cooney, C.M. Evolution of Workforce Diversity in Surgery✰. J. Surg. Educ. 2019, 76, 1015–1021. [Google Scholar] [CrossRef]
- Moy, E.; Bartman, B.A. Physician Race and Care of Minority and Medically Indigent Patients. JAMA 1995, 273, 1515–1520. [Google Scholar] [CrossRef]
- Komaromy, M.; Grumbach, K.; Drake, M.; Vranizan, K.; Lurie, N.; Keane, D.; Bindman, A.B. The Role of Black and Hispanic Physicians in Providing Health Care for Underserved Populations. N. Engl. J. Med. 1996, 334, 1305–1310. [Google Scholar] [CrossRef] [PubMed]
- Butler, P.D.; Longaker, M.T.; Britt, L.D. Major Deficit in the Number of Underrepresented Minority Academic Surgeons Persists. Ann. Surg. 2008, 248, 704–711. [Google Scholar] [CrossRef]
- Corbie-Smith, G.; Thomas, S.B.; Williams, M.V.; Moody-Ayers, S. Attitudes and Beliefs of African Americans Toward Participation in Medical Research. J. Gen. Intern. Med. 1999, 14, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Branson, R.D.; Davis, K.; Butler, K.L. African Americans’ Participation in Clinical Research: Importance, Barriers, and Solutions. Am. J. Surg. 2007, 193, 32–39; discussion 40. [Google Scholar] [CrossRef] [PubMed]
- Wallis, C.J.D.; Jerath, A.; Aminoltejari, K.; Kaneshwaran, K.; Salles, A.; Coburn, N.; Wright, F.C.; Gotlib Conn, L.; Klaassen, Z.; Luckenbaugh, A.N.; et al. Surgeon Sex and Long-Term Postoperative Outcomes Among Patients Undergoing Common Surgeries. JAMA Surg. 2023, 158, 1185–1194. [Google Scholar] [CrossRef] [PubMed]
- Otte, S.V. Improved Patient Experience and Outcomes: Is Patient–Provider Concordance the Key? J. Patient Exp. 2022, 9, 23743735221103033. [Google Scholar] [CrossRef]
- Fnais, N.; Soobiah, C.; Chen, M.H.; Lillie, E.; Perrier, L.; Tashkhandi, M.; Straus, S.E.; Mamdani, M.; Al-Omran, M.; Tricco, A.C. Harassment and Discrimination in Medical Training: A Systematic Review and Meta-Analysis. Acad. Med. 2014, 89, 817. [Google Scholar] [CrossRef]
- Alimi, Y.; Bevilacqua, L.A.; Snyder, R.A.; Walsh, D.; Jackson, P.G.; DeMaria, E.J.; Tuttle, J.E.; Altieri, M.S. Microaggressions and Implicit Bias in Surgical Training: An Undocumented but Pervasive Phenomenon. Ann. Surg. 2023, 277, e192–e196. [Google Scholar] [CrossRef]
- Lee, Y.S.; Campany, M.; Fullerton, S.; Malik, R.; Dorsey, C.; Mercado, D.; Allen, A.; Erben, Y. State of Gender-Based Microaggressions Among Surgeons and Development of Simulation Workshops for Addressing Microaggressions for Surgical Trainees and Students. Ann. Vasc. Surg. 2023, 95, 285–290. [Google Scholar] [CrossRef]
- Carino Mason, M.R.; Pandya, S.; Joshi, P.; Cai, N.; Murdock, C.J.; Hui-Chou, H.G. Perceptions of Racial and Gender Microaggressions in an Academic Orthopaedic Department. JB JS Open Access 2023, 8, e22.00150. [Google Scholar] [CrossRef]
- Chisholm, L.P.; Jackson, K.R.; Davidson, H.A.; Churchwell, A.L.; Fleming, A.E.; Drolet, B.C. Evaluation of Racial Microaggressions Experienced During Medical School Training and the Effect on Medical Student Education and Burnout: A Validation Study. J. Natl. Med. Assoc. 2021, 113, 310–314. [Google Scholar] [CrossRef]
- Lawlace, M.; Newcomb, M.E.; Whitton, S.W. Minority Stressors and Suicidal Ideation in Sexual and Gender Minority Youth Assigned Female at Birth: Prospective Associations and Racial Differences. Suicide Life Threat. Behav. 2022, 52, 1168–1177. [Google Scholar] [CrossRef] [PubMed]
- Anderson, N.; Lett, E.; Asabor, E.N.; Hernandez, A.L.; Nguemeni Tiako, M.J.; Johnson, C.; Montenegro, R.E.; Rizzo, T.M.; Latimore, D.; Nunez-Smith, M.; et al. The Association of Microaggressions with Depressive Symptoms and Institutional Satisfaction Among a National Cohort of Medical Students. J. Gen. Intern. Med. 2022, 37, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Meyers, C.; Aumer, K.; Schoniwitz, A.; Janicki, C.; Pauker, K.; Chang, E.C.; Gaither, S.E.; Williams, A. Experiences with Microaggressions and Discrimination in Racially Diverse and Homogeneously White Contexts. Cult. Divers. Ethn. Minor. Psychol. 2020, 26, 250–259. [Google Scholar] [CrossRef]
- Guevara, J.P.; Wade, R.; Aysola, J. Racial and Ethnic Diversity at Medical Schools—Why Aren’t We There Yet? N. Engl. J. Med. 2021, 385, 1732–1734. [Google Scholar] [CrossRef] [PubMed]
- Page, S.E. The Diversity Bonus: How Great Teams Pay off in the Knowledge Economy; Princeton University Press: Princeton, NJ, USA, 2019; ISBN 978-0-691-19153-9. [Google Scholar]
- Baker, E.H.; Dowden, J.E.; Cochran, A.R.; Iannitti, D.A.; Kimchi, E.T.; Staveley-O’Carroll, K.F.; Jeyarajah, D.R. Qualities and Characteristics of Successfully Matched North American HPB Surgery Fellowship Candidates. HPB 2016, 18, 479–484. [Google Scholar] [CrossRef]
- Yekula, A.; Sreeram, S.; Dhawan, S.; Sharma, M.; Sandoval-Garcia, C.; Huling, J.D.; Suri, A.; Belani, K.; Park, M.C.; Carter, B.S.; et al. Neurosurgery Residency Match for International Medical Graduates in the United States. J. Neurosurg. 2023, 2023, 291–298. [Google Scholar] [CrossRef]
- Porras Fimbres, D.C.; Zeng, S.; Phillips, B.T. Prevalence of International Medical Graduates in Integrated Plastic Surgery Programs. Plast. Reconstr. Surg. Glob. Open 2023, 11, e5140. [Google Scholar] [CrossRef]
- Shapiro, M.; Chen, Q.; Huang, Q.; Boosalis, V.A.; Yoon, C.H.; Saund, M.S.; Whang, E.E.; Gold, J.S. Associations of Socioeconomic Variables With Resection, Stage, and Survival in Patients With Early-Stage Pancreatic Cancer. JAMA Surg. 2016, 151, 338–345. [Google Scholar] [CrossRef]
- Alawadi, Z.M.; Phatak, U.R.; Kao, L.S.; Ko, T.C.; Wray, C.J. Race Not Rural Residency Is Predictive of Surgical Treatment for Hepatocellular Carcinoma: Analysis of the Texas Cancer Registry. J. Surg. Oncol. 2016, 113, 84–88. [Google Scholar] [CrossRef]
- Munir, M.M.; Woldesenbet, S.; Endo, Y.; Moazzam, Z.; Lima, H.A.; Azap, L.; Katayama, E.; Alaimo, L.; Shaikh, C.; Dillhoff, M.; et al. Disparities in Socioeconomic Factors Mediate the Impact of Racial Segregation Among Patients With Hepatopancreaticobiliary Cancer. Ann. Surg. Oncol. 2023, 2023, 4826–4835. [Google Scholar] [CrossRef] [PubMed]
- Landon, B.E.; Onnela, J.-P.; Meneades, L.; O’Malley, A.J.; Keating, N.L. Assessment of Racial Disparities in Primary Care Physician Specialty Referrals. JAMA Netw. Open 2021, 4, e2029238. [Google Scholar] [CrossRef] [PubMed]
- Yilma, M.; Kim, N.J.; Shui, A.M.; Tana, M.; Landis, C.; Chen, A.; Bangaru, S.; Mehta, N.; Zhou, K. Factors Associated with Liver Transplant Referral Among Patients with Cirrhosis at Multiple Safety-Net Hospitals. JAMA Netw. Open 2023, 6, e2317549. [Google Scholar] [CrossRef] [PubMed]
- Hollingsworth, J.M.; Yu, X.; Yan, P.L.; Yoo, H.; Telem, D.A.; Yankah, E.N.; Zhu, J.; Waljee, A.K.; Nallamothu, B.K. Provider Care Team Segregation and Operative Mortality Following Coronary Artery Bypass Grafting. Circ. Cardiovasc. Qual. Outcomes 2021, 14, e007778. [Google Scholar] [CrossRef] [PubMed]
- Dy, C.J.; Marx, R.G.; Ghomrawi, H.M.K.; Pan, T.J.; Westrich, G.H.; Lyman, S. The Potential Influence of Regionalization Strategies on Delivery of Care for Elective Total Joint Arthroplasty. J. Arthroplast. 2015, 30, 1–6. [Google Scholar] [CrossRef]
- Dossa, F.; Zeltzer, D.; Sutradhar, R.; Simpson, A.N.; Baxter, N.N. Sex Differences in the Pattern of Patient Referrals to Male and Female Surgeons. JAMA Surg. 2022, 157, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Sarsons, H. Interpreting Signals in the Labor Market: Evidence from Medical Referrals; Job Market Paper; Harvard University: Cambridge, MA, USA, 2017. [Google Scholar]
- Teh, C. Women in HPB. HPB 2019, 21, S290. [Google Scholar] [CrossRef]
- Bullock, J.L.; Lai, C.J.; Lockspeiser, T.; O’Sullivan, P.S.; Aronowitz, P.; Dellmore, D.; Fung, C.-C.; Knight, C.; Hauer, K.E. In Pursuit of Honors: A Multi-Institutional Study of Students’ Perceptions of Clerkship Evaluation and Grading. Acad. Med. 2019, 94, S48–S56. [Google Scholar] [CrossRef]
- Hanson, J.L.; Pérez, M.; Mason, H.R.C.; Aagaard, E.M.; Jeffe, D.B.; Teherani, A.; Colson, E.R. Racial/Ethnic Disparities in Clerkship Grading: Perspectives of Students and Teachers. Acad. Med. 2022, 97, S35–S45. [Google Scholar] [CrossRef]
- Cotter, E.J.; Polce, E.M.; Williams, K.L.; Spiker, A.M.; Grogan, B.F.; Lang, G.J. Current State of Research Gap-Years in Orthopedic Surgery Residency Applicants: Program Directors’ Perspectives. Iowa Orthop. J. 2022, 42, 19–30. [Google Scholar]
- Stein, J.S.; Estevez-Ordonez, D.; Laskay, N.M.B.; Atchley, T.J.; Saccomano, B.W.; Hale, A.T.; Patel, O.U.; Burge, K.; Haynes, W.; Yadav, I.; et al. Assessing the Impact of Changes to USMLE Step 1 Grading on Evaluation of Neurosurgery Residency Applicants in the United States: A Program Director Survey. World Neurosurg. 2022, 166, e511–e520. [Google Scholar] [CrossRef] [PubMed]
- Abdalla, M.; Abdalla, S.; Maurer, L.R.; Ortega, G.; Abdalla, M. American Black Authorship Has Decreased Across All Clinical Specialties Despite an Increasing Number of Black Physicians Between 1990 and 2020 in the USA. J. Racial. Ethn. Health Disparities 2023, 2023, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ginther, D.K.; Schaffer, W.T.; Schnell, J.; Masimore, B.; Liu, F.; Haak, L.L.; Kington, R. Race, Ethnicity, and NIH Research Awards. Science 2011, 333, 1015–1019. [Google Scholar] [CrossRef] [PubMed]
- Chloros, G.D.; Konstantinidis, C.I.; Vasilopoulou, A.; Giannoudis, P.V. Peer Review Practices in Academic Medicine: How the Example of Orthopaedic Surgery May Help Shift the Paradigm? Int. Orthop. 2023, 47, 1137–1145. [Google Scholar] [CrossRef] [PubMed]
- Farooq, A.; Sahara, K.; Muneeb, A.; Farooq, K.; Tsilimigras, D.I.; Merath, K.; Mehta, R.; Paredes, A.; Wu, L.; Hyer, J.M.; et al. Analysis of Authorship in Hepatopancreaticobiliary Surgery: Women Remain Underrepresented. J. Gastrointest. Surg. 2020, 24, 2070–2076. [Google Scholar] [CrossRef] [PubMed]
- AHPBA. Underrepresented Minority Travel Grant. Available online: https://www.ahpba.org/awards-grants/underrepresented-minority-travel-grant/ (accessed on 18 July 2023).
- AAS/AASF. Student Diversity Travel Award. Available online: https://www.aasurg.org/awards/travel-grants-visiting-professorships/student-diversity-travel-grant/ (accessed on 23 November 2023).
- Daley, S.P.; Broyles, S.L.; Rivera, L.M.; Brennan, J.J.; Lu, E.R.; Reznik, V. A Conceptual Model for Faculty Development in Academic Medicine: The Underrepresented Minority Faculty Experience. J. Natl. Med. Assoc. 2011, 103, 816–821. [Google Scholar] [CrossRef]
- Larson, A.R.; Englander, M.J.; Youmans, Q.R.; Verduzco-Gutierrez, M.; Stanford, F.C.; Strong, S.A.; Liu, H.Y.; Silver, J.K. Analysis of Physician Compensation Studies by Gender, Race, and Ethnicity. Health Equity 2022, 6, 59–71. [Google Scholar] [CrossRef] [PubMed]
- Medscape Physician Compensation Report 2023: Your Income vs. Your Peers’. Available online: https://www.medscape.com/slideshow/2023-compensation-overview-6016341 (accessed on 24 September 2023).
- Greenwood, S. The Enduring Grip of the Gender Pay Gap. In Pew Research Center’s Social & Demographic Trends Project; Pew Research Center: Washington, DC, USA, 2023. [Google Scholar]
- Morris, M.; Chen, H.; Heslin, M.J.; Krontiras, H. A Structured Compensation Plan Improves but Does Not Erase the Sex Pay Gap in Surgery. Ann. Surg. 2018, 268, 442–448. [Google Scholar] [CrossRef]
- Hayes, S.N.; Noseworthy, J.H.; Farrugia, G. A Structured Compensation Plan Results in Equitable Physician Compensation: A Single-Center Analysis. Mayo Clin. Proc. 2020, 95, 35–43. [Google Scholar] [CrossRef]
- Fang, D.; Moy, E.; Colburn, L.; Hurley, J. Racial and Ethnic Disparities in Faculty Promotion in Academic Medicine. JAMA 2000, 284, 1085–1092. [Google Scholar] [CrossRef]
- Roland, K.B.; Milliken, E.L.; Rohan, E.A.; DeGroff, A.; White, S.; Melillo, S.; Rorie, W.E.; Signes, C.-A.C.; Young, P.A. Use of Community Health Workers and Patient Navigators to Improve Cancer Outcomes Among Patients Served by Federally Qualified Health Centers: A Systematic Literature Review. Health Equity 2017, 1, 61–76. [Google Scholar] [CrossRef] [PubMed]
- Ko, N.Y.; Darnell, J.S.; Calhoun, E.; Freund, K.M.; Wells, K.J.; Shapiro, C.L.; Dudley, D.J.; Patierno, S.R.; Fiscella, K.; Raich, P.; et al. Can Patient Navigation Improve Receipt of Recommended Breast Cancer Care? Evidence from the National Patient Navigation Research Program. J. Clin. Oncol. 2014, 32, 2758–2764. [Google Scholar] [CrossRef] [PubMed]
- DeGroff, A.; Schroy, P.C.; Morrissey, K.G.; Slotman, B.; Rohan, E.A.; Bethel, J.; Murillo, J.; Ren, W.; Niwa, S.; Leadbetter, S.; et al. Patient Navigation for Colonoscopy Completion: Results of an RCT. Am. J. Prev. Med. 2017, 53, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Wells, K.J.; Meade, C.D.; Calcano, E.; Lee, J.-H.; Rivers, D.; Roetzheim, R.G. Innovative Approaches to Reducing Cancer Health Disparities: The Moffitt Cancer Center Patient Navigator Research Program. J. Cancer Educ. 2011, 26, 649–657. [Google Scholar] [CrossRef]
- Wells, K.J.; Luque, J.S.; Miladinovic, B.; Vargas, N.; Asvat, Y.; Roetzheim, R.G.; Kumar, A. Do Community Health Worker Interventions Improve Rates of Screening Mammography in the United States? A Systematic Review. Cancer Epidemiol. Biomark. Prev. 2011, 20, 1580–1598. [Google Scholar] [CrossRef]
- Lee, R.M.; Darby, R.; Medin, C.R.; Haser, G.C.; Mason, M.C.; Miller, L.S.; Staley, C.A.; Maithel, S.K.; Russell, M.C. Implementation of a Hepatocellular Carcinoma Screening Program for At-Risk Patients Safety-Net Hospital: A Model for National Dissemination. Ann. Surg. 2022, 276, 545–553. [Google Scholar] [CrossRef]
- Griesemer, I.; Birken, S.A.; Rini, C.; Maman, S.; John, R.; Thatcher, K.; Dixon, C.; Yongue, C.; Baker, S.; Bosire, C.; et al. Mechanisms to Enhance Racial Equity in Health Care: Developing a Model to Facilitate Translation of the ACCURE Intervention. SSM—Qual. Res. Health 2023, 3, 100204. [Google Scholar] [CrossRef]
- Black, K.Z.; Baker, S.L.; Robertson, L.B.; Lightfoot, A.F.; Alexander-Bratcher, K.M.; Befus, D.; Cothern, C.; Dixon, C.E.; Ellis, K.R.; Guerrab, F.; et al. 14. Health Care: Antiracism Organizing for Culture and Institutional Change in Cancer Care. In Racism: Science & Tools for the Public Health Professional; American Public Health Association: Washington, DC, USA, 2019; ISBN 978-0-87553-303-2. [Google Scholar]
- A Multi-Faceted Intervention Aimed at Black-White Disparities in the Treatment of Early Stage Cancers: The ACCURE Pragmatic Quality Improvement Trial—ClinicalKey. Available online: https://www.clinicalkey.com/#!/content/playContent/1-s2.0-S0027968418301913?returnurl=https:%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS0027968418301913%3Fshowall%3Dtrue&referrer= (accessed on 9 October 2023).
- Griesemer, I.; Lightfoot, A.F.; Eng, E.; Bosire, C.; Guerrab, F.; Kotey, A.; Alexander, K.M.; Baker, S.; Black, K.Z.; Dixon, C.; et al. Examining ACCURE’s Nurse Navigation through an Antiracist Lens: Transparency and Accountability in Cancer Care. 2023. Available online: https://journals.sagepub.com/doi/full/10.1177/15248399221136534 (accessed on 9 October 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rengers, T.A.; Warner, S.G. Importance of Diversity, Equity, and Inclusion in the Hepatopancreatobiliary Workforce. Cancers 2024, 16, 326. https://doi.org/10.3390/cancers16020326
Rengers TA, Warner SG. Importance of Diversity, Equity, and Inclusion in the Hepatopancreatobiliary Workforce. Cancers. 2024; 16(2):326. https://doi.org/10.3390/cancers16020326
Chicago/Turabian StyleRengers, Timothy A., and Susanne G. Warner. 2024. "Importance of Diversity, Equity, and Inclusion in the Hepatopancreatobiliary Workforce" Cancers 16, no. 2: 326. https://doi.org/10.3390/cancers16020326
APA StyleRengers, T. A., & Warner, S. G. (2024). Importance of Diversity, Equity, and Inclusion in the Hepatopancreatobiliary Workforce. Cancers, 16(2), 326. https://doi.org/10.3390/cancers16020326







