Exploring the Genomic Landscape of Hepatobiliary Cancers to Establish a Novel Molecular Classification System
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Selection of a Genomic Database
2.2. Gene Panels Used for Next-Generation Sequencing of Hepatobiliary Cancers
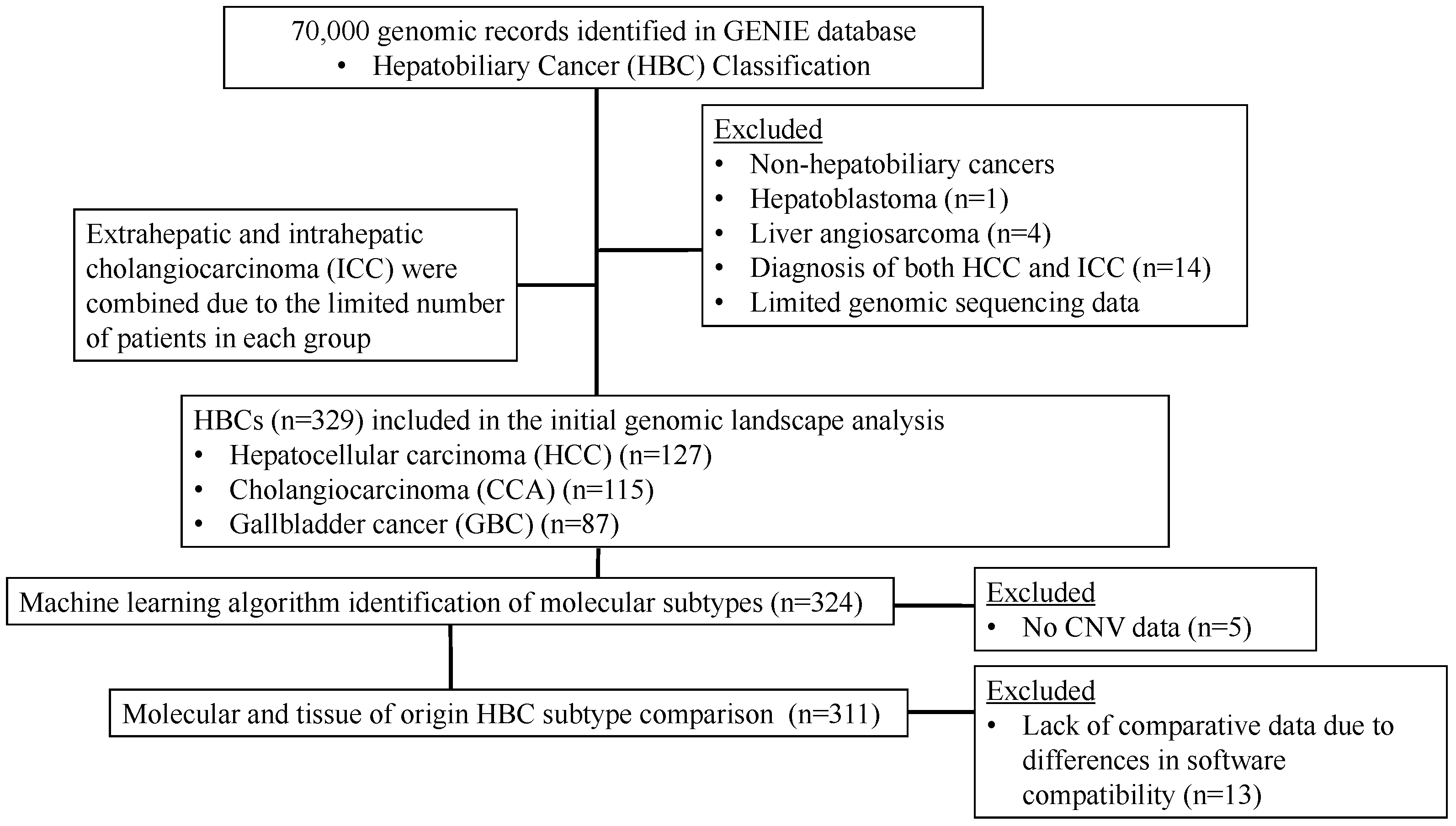
2.3. Patient Selection
2.4. Processing of Genomic Data
2.5. Identification of HBC Molecular Subtypes
2.6. Bioinformatics and Biostatistical Analyses
3. Results
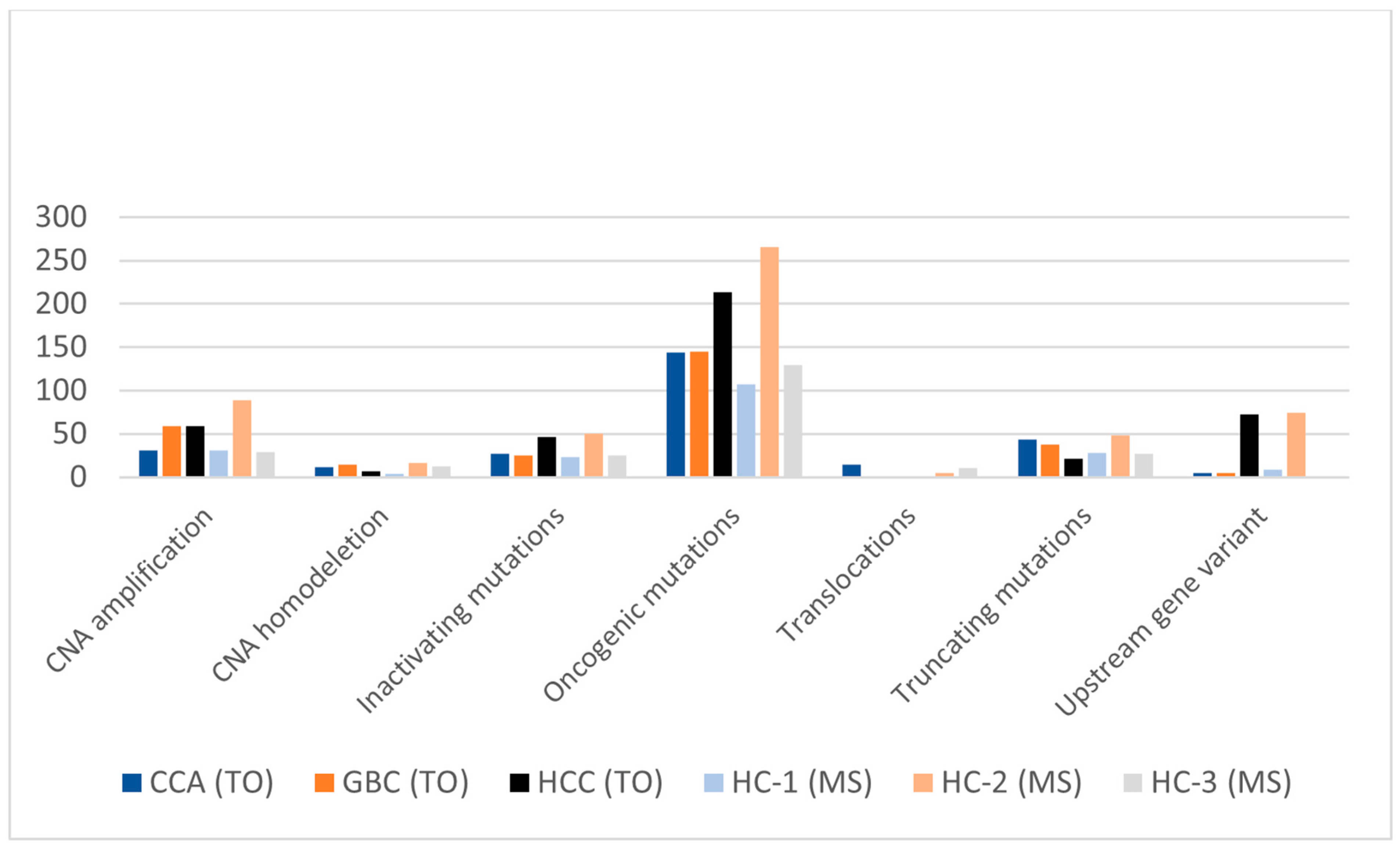
3.1. Genomic Landscape of HBCs Reveals Variation between TO Subtypes
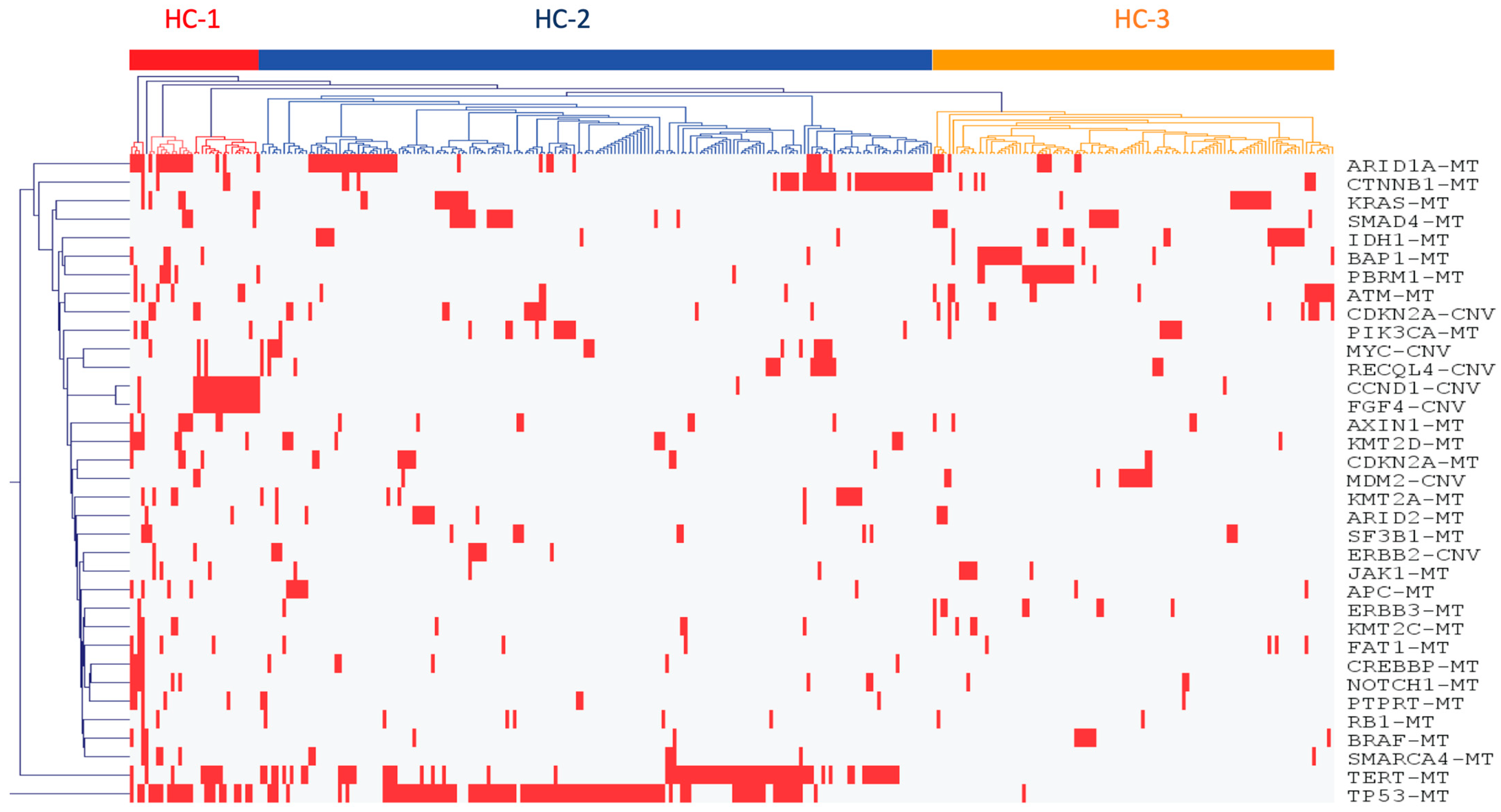
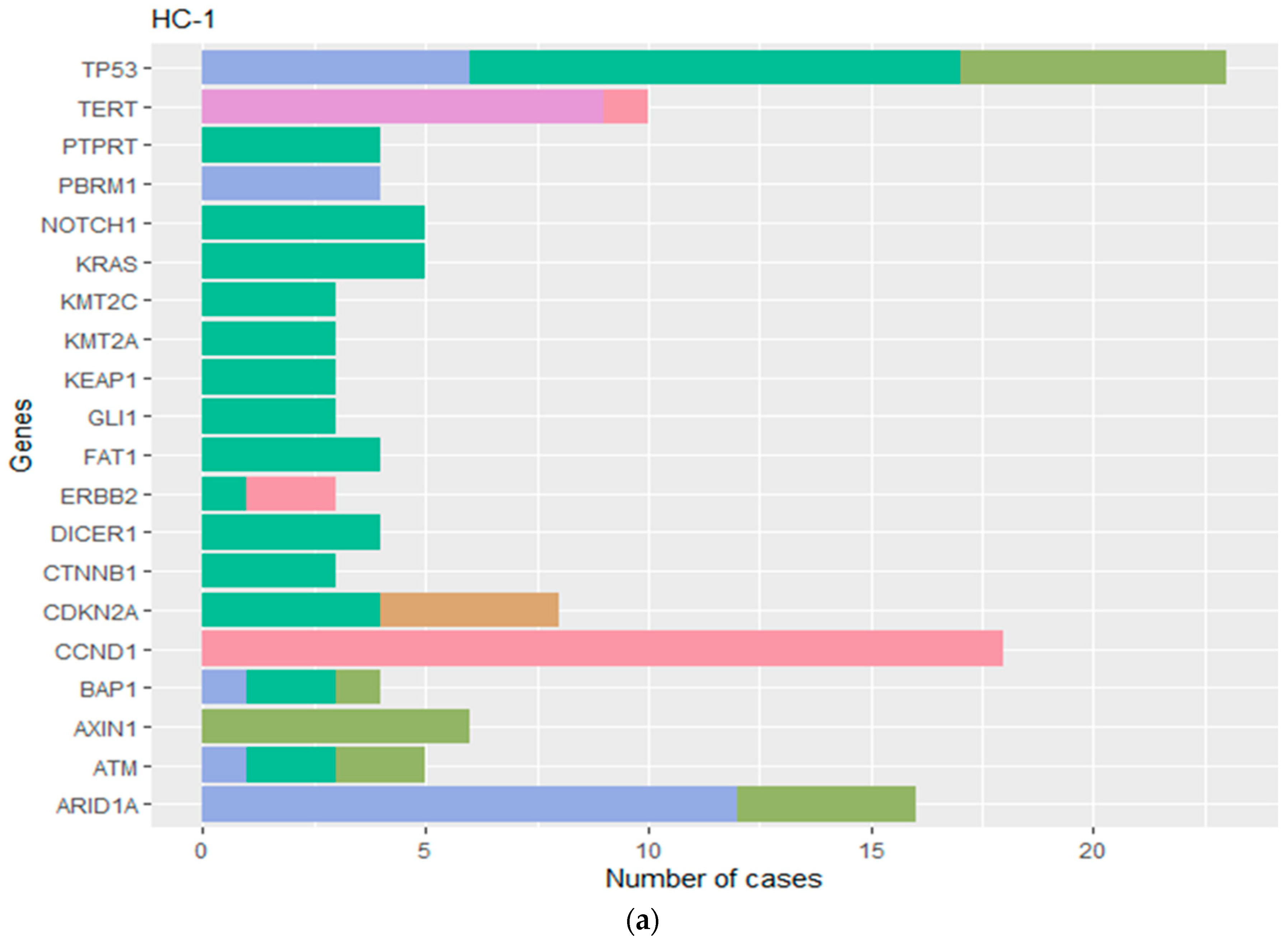
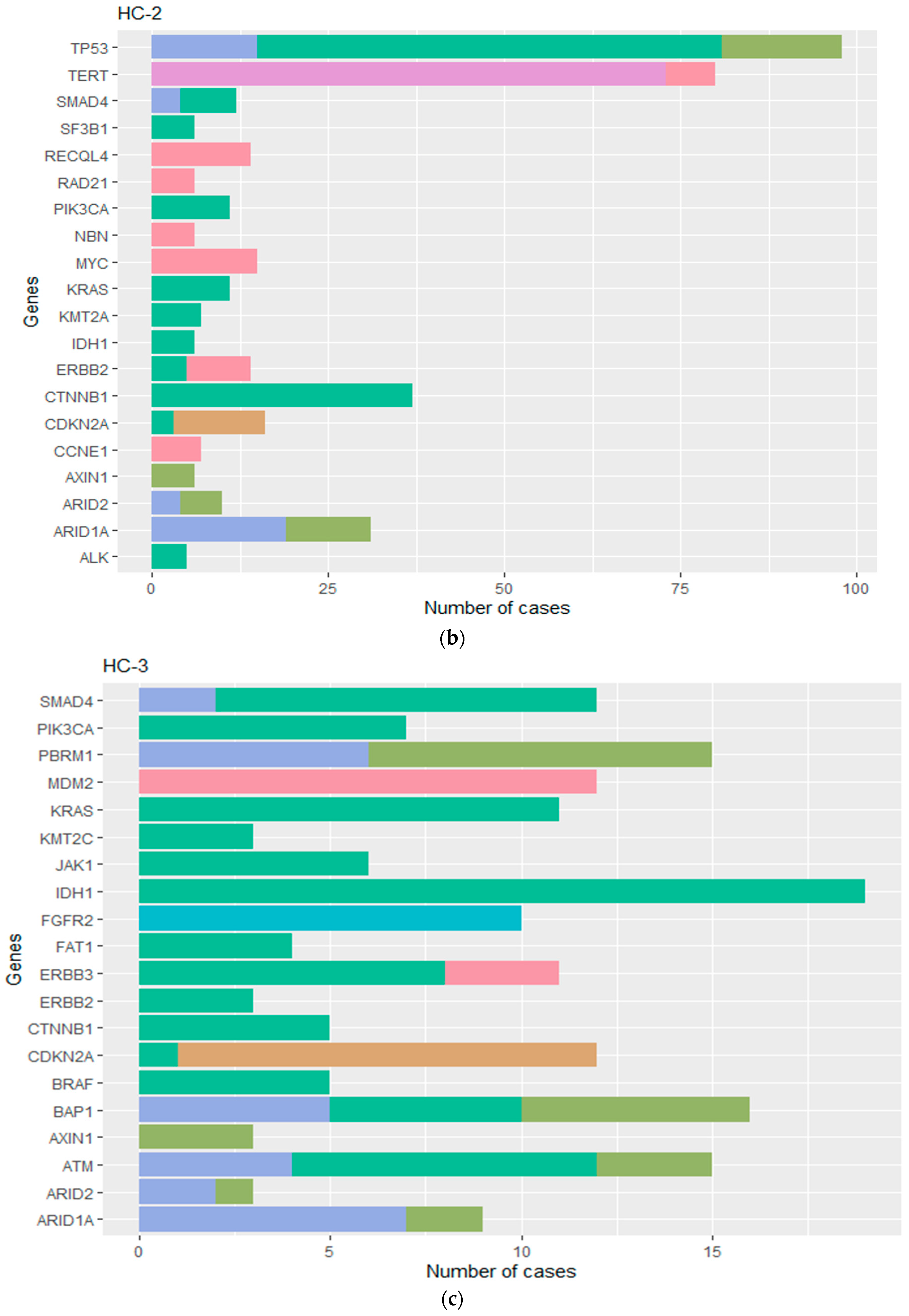
3.2. Machine Learning Distinguishes Three Unique HBC Molecular Subtypes
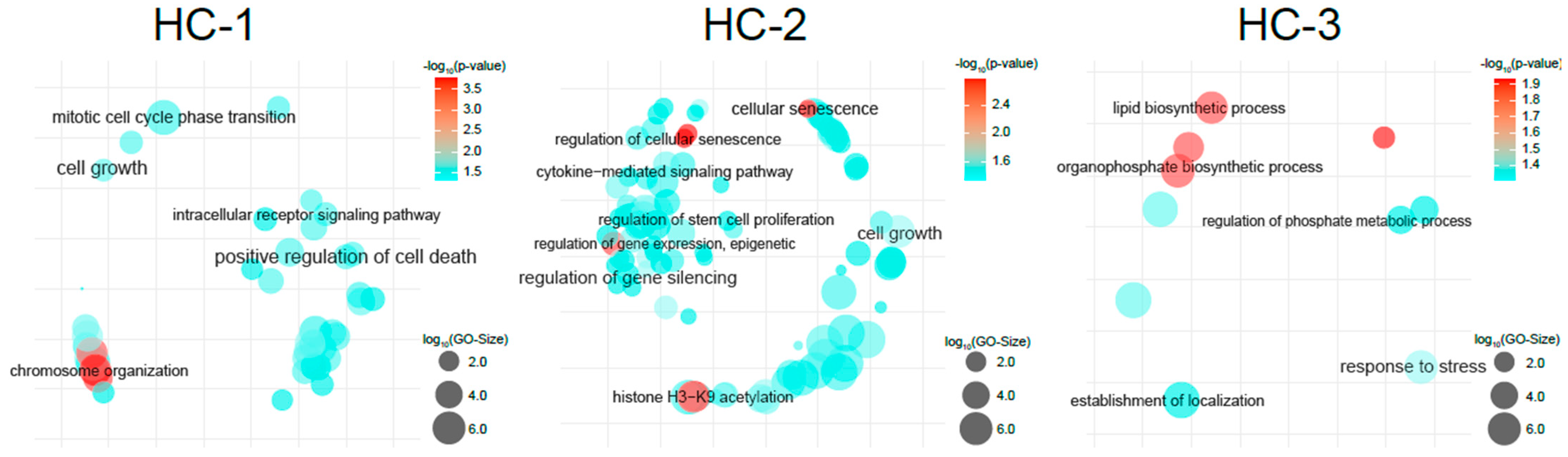
3.3. Gene Enrichment Analyses Elucidates Oncogenomic Pathways
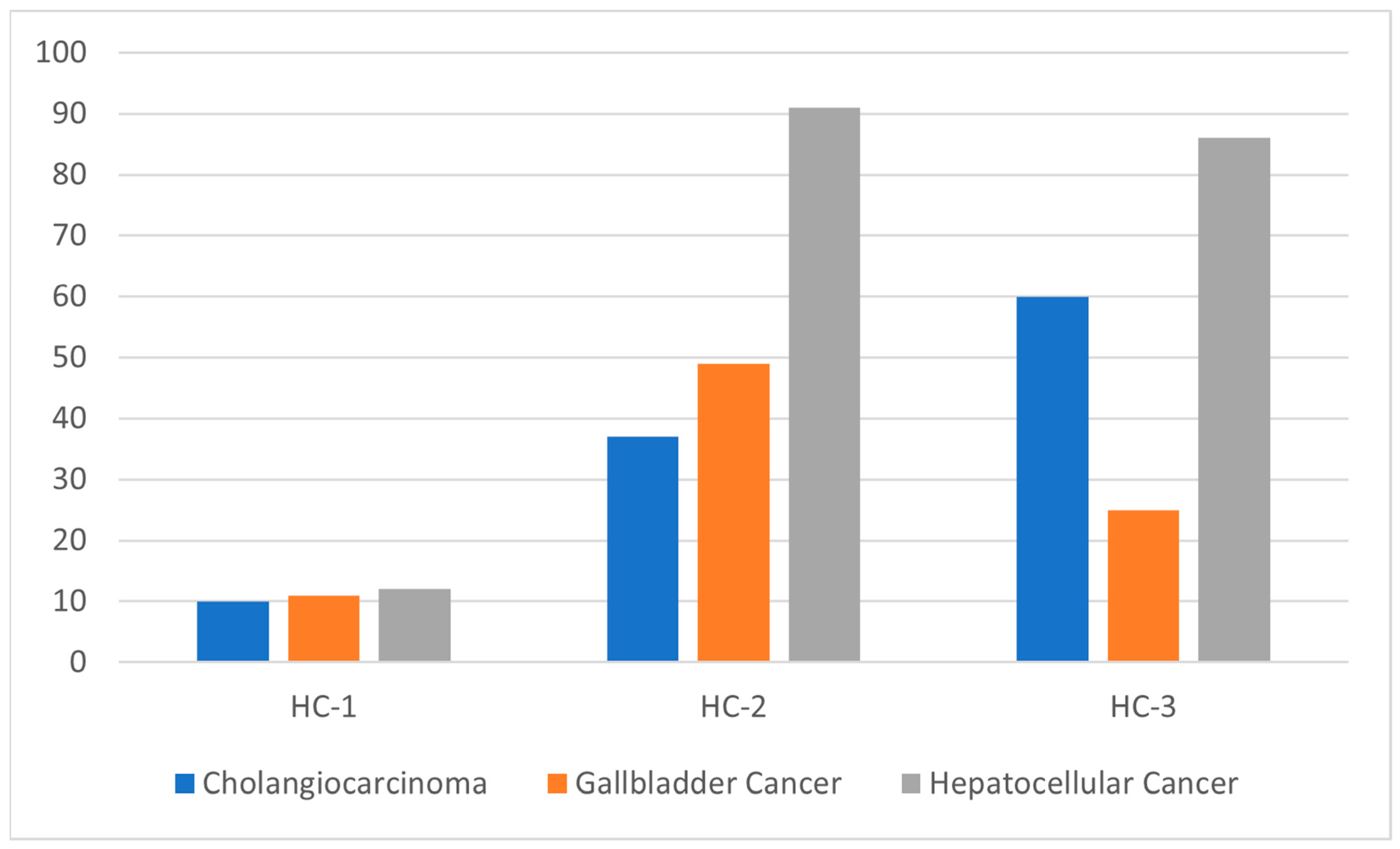
3.4. Comparative Analysis of HBC Molecular and TO Subtypes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Glossary
| HBC | hepatobiliary cancer |
| TO | tissue of origin |
| GA | genomic alterations |
| MS | molecular subtype |
| NGS | next-generation sequencing |
| HC-1 | molecular subtype 1, “hyper-mutated-proliferative state” |
| HC-2 | molecular subtype 2, “adaptive stem cell-cellular senescence” |
| HC-3 | molecular subtype 3, “metabolic-stress pathway” |
| CCA | cholangiocarcinoma |
| HCC | hepatocellular carcinoma |
| GBC | gallbladder cancer |
| PS | prognostic stage |
| ICC | intrahepatic cholangiocarcinoma |
| AJCC | American Joint Committee on Cancer |
| AARC-GENIE | American Association of Cancer Research Genomics Evidence Neoplasia Information Exchange |
| SNPs | single nucleotide polymorphisms |
| CNV | copy number variation |
References
- Islami, F.; Ward, E.M.; Sung, H.; Cronin, K.A.; Tangka, F.K.L.; Sherman, R.L.; Zhao, J.; Anderson, R.N.; Henley, S.J.; Yabroff, K.R.; et al. Annual Report to the Nation on the Status of Cancer, Part 1: National Cancer Statistics. J. Natl. Cancer Inst. 2021, 113, 1648–1669. [Google Scholar] [CrossRef]
- Horgan, A.M.; Amir, E.; Walter, T.; Knox, J.J. Adjuvant therapy in the treatment of biliary tract cancer: A systematic review and meta-analysis. J. Clin. Oncol. 2012, 30, 1934–1940. [Google Scholar] [CrossRef]
- Hundal, R.; Shaffer, E.A. Gallbladder cancer: Epidemiology and outcome. Clin. Epidemiol. 2014, 6, 99–109. [Google Scholar] [CrossRef]
- Mavros, M.N.; Economopoulos, K.P.; Alexiou, V.G.; Pawlik, T.M. Treatment and Prognosis for Patients with Intrahepatic Cholangiocarcinoma: Systematic Review and Meta-analysis. JAMA Surg. 2014, 149, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Lamarca, A.; Hubner, R.A.; David Ryder, W.; Valle, J.W. Second-line chemotherapy in advanced biliary cancer: A systematic review. Ann. Oncol. 2014, 25, 2328–2338. [Google Scholar] [CrossRef] [PubMed]
- Valle, J.; Wasan, H.; Palmer, D.H.; Cunningham, D.; Anthoney, A.; Maraveyas, A.; Madhusudan, S.; Iveson, T.; Hughes, S.; Pereira, S.P.; et al. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N. Engl. J. Med. 2010, 362, 1273–1281. [Google Scholar] [CrossRef]
- Baffy, G.; Brunt, E.M.; Caldwell, S.H. Hepatocellular carcinoma in non-alcoholic fatty liver disease: An emerging menace. J. Hepatol. 2012, 56, 1384–1391. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Rahman, O.; Elsayed, Z.; Elhalawani, H. Gemcitabine-based chemotherapy for advanced biliary tract carcinomas. Cochrane Database Syst. Rev. 2018, 4, CD011746. [Google Scholar] [CrossRef]
- Ma, N.; Cheng, H.; Qin, B.; Zhong, R.; Wang, B. Adjuvant therapy in the treatment of gallbladder cancer: A meta-analysis. BMC Cancer 2015, 15, 615. [Google Scholar] [CrossRef]
- Rizzo, A.; Ricci, A.D.; Cusmai, A.; Acquafredda, S.; De Palma, G.; Brandi, G.; Palmiotti, G. Systemic Treatment for Metastatic Biliary Tract Cancer: State of the Art and a Glimpse to the Future. Curr. Oncol. 2022, 29, 551–564. [Google Scholar] [CrossRef]
- Zhang, L.; Bluth, M.H.; Bhalla, A. Molecular Diagnostics in the Neoplasms of the Pancreas, Liver, Gallbladder, and Extrahepatic Biliary Tract: 2018 Update. Clin. Lab. Med. 2018, 38, 367–384. [Google Scholar] [CrossRef]
- Percy, C.; Fritz, A.; Jack, A.; Shanmugarathan, S.; Sobin, L.; Parkin, D.M.; Whelan, S. International Classification of Diseases for Oncology (ICD-O); AbeBooks: Victoria, BC, USA, 2020; ISBN 9789241545341. [Google Scholar]
- Washington, M.K.; Goldberg, R.M.; Chang, G.J.; Limburg, P.; Lam, A.K.; Salto-Tellez, M.; Arends, M.J.; Nagtegaal, I.D.; Klimstra, D.S.; Rugge, M.; et al. Diagnosis of digestive system tumours. Int. J. Cancer 2021, 148, 1040–1050. [Google Scholar] [CrossRef]
- Cree, I.A.; Indave Ruiz, B.I.; Zavadil, J.; McKay, J.; Olivier, M.; Kozlakidis, Z.; Lazar, A.J.; Hyde, C.; Holdenrieder, S.; Hastings, R.; et al. The International Collaboration for Cancer Classification and Research. Int. J. Cancer 2021, 148, 560–571. [Google Scholar] [CrossRef]
- Uttley, L.; Indave, B.I.; Hyde, C.; White, V.; Lokuhetty, D.; Cree, I. Invited commentary-WHO Classification of Tumours: How should tumors be classified? Expert consensus, systematic reviews or both? Int. J. Cancer 2020, 146, 3516–3521. [Google Scholar] [CrossRef]
- Salto-Tellez, M.; Cree, I.A. Cancer taxonomy: Pathology beyond pathology. Eur. J. Cancer 2019, 115, 57–60. [Google Scholar] [CrossRef] [PubMed]
- Hang, H.; Jeong, S.; Sha, M.; Kong, D.; Xi, Z.; Tong, Y.; Xia, Q. Cholangiocarcinoma: Anatomical location-dependent clinical, prognostic, and genetic disparities. Ann. Transl. Med. 2019, 7, 744. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology, Hepatobiliary Cancers (Version 1.2022); National Comprehensive Cancer Network: Plymouth Meeting, PA, USA, 2022. [Google Scholar]
- Schulze, K.; Nault, J.; Villanueva, A. Genetic profiling of hepatocellular carcinoma using next-generation sequencing. J. Hepatol. 2016, 65, 1031–1042. [Google Scholar] [CrossRef]
- Simbolo, M.; Fassan, M.; Ruzzenente, A.; Mafficini, A.; Wood, L.D.; Corbo, V.; Melisi, D.; Malleo, G.; Vicentini, C.; Malpeli, G.; et al. Multigene mutational profiling of cholangiocarcinomas identifies actionable molecular subgroups. Oncotarget 2014, 5, 2839–2852. [Google Scholar] [CrossRef] [PubMed]
- Cancer Genome Atlas Research Network. Comprehensive and Integrative Genomic Characterization of Hepatocellular Carcinoma. Cell 2017, 169, 1327–1341.e23. [Google Scholar] [CrossRef]
- Jain, A.; Javle, M. Molecular profiling of biliary tract cancer: A target rich disease. J. Gastrointest. Oncol. 2016, 7, 797–803. [Google Scholar] [CrossRef]
- Churi, C.R.; Shroff, R.; Wang, Y.; Rashid, A.; Kang, H.C.; Weatherly, J.; Zuo, M.; Zinner, R.; Hong, D.; Meric-Bernstam, F.; et al. Mutation profiling in cholangiocarcinoma: Prognostic and therapeutic implications. PLoS ONE 2014, 9, e115383. [Google Scholar] [CrossRef] [PubMed]
- Ha, K.; Fujita, M.; Karlić, R.; Yang, S.; Xue, R.; Zhang, C.; Bai, F.; Zhang, N.; Hoshida, Y.; Polak, P.; et al. Somatic mutation landscape reveals differential variability of cell-of-origin for primary liver cancer. Heliyon 2020, 6, e03350. [Google Scholar] [CrossRef]
- Hoadley, K.A.; Yau, C.; Hinoue, T.; Wolf, D.M.; Lazar, A.J.; Drill, E.; Shen, R.; Taylor, A.M.; Cherniack, A.D.; Thorsson, V.; et al. Cell-of-Origin Patterns Dominate the Molecular Classification of 10,000 Tumors from 33 Types of Cancer. Cell 2018, 173, 291–304.e6. [Google Scholar] [CrossRef]
- Hoadley, K.A.; Yau, C.; Wolf, D.M.; Cherniack, A.D.; Tamborero, D.; Ng, S.; Leiserson, M.D.M.; Niu, B.; McLellan, M.D.; Uzunangelov, V.; et al. Multiplatform analysis of 12 cancer types reveals molecular classification within and across tissues of origin. Cell 2014, 158, 929–944. [Google Scholar] [CrossRef]
- Liu, Y.; Sethi, N.S.; Hinoue, T.; Schneider, B.G.; Cherniack, A.D.; Sanchez-Vega, F.; Seoane, J.A.; Farshidfar, F.; Bowlby, R.; Islam, M.; et al. Comparative Molecular Analysis of Gastrointestinal Adenocarcinomas. Cancer Cell 2018, 33, 721–735.e8. [Google Scholar] [CrossRef]
- Tomczak, K.; Czerwińska, P.; Wiznerowicz, M. The Cancer Genome Atlas (TCGA): An immeasurable source of knowledge. Contemp. Oncol. 2015, 19, 68. [Google Scholar] [CrossRef] [PubMed]
- O’Cearbhaill, R.; Gannon, J.M.; Prichard, R.S.; Walshe, J.M.; McDermott, E.; Quinn, C.M. The American Joint Commission Cancer 8th Edition Prognostic Stage Including Oncotype DX® Recurrence Score: Impact on Staging of Early Breast Cancer. Pathobiology 2019, 86, 77–82. [Google Scholar] [CrossRef]
- Gradishar, W.J.; Moran, M.S.; Abraham, J.; Aft, R.; Agnese, D.; Allison, K.H.; Anderson, B.; Burstein, H.J.; Chew, H.; Dang, C.; et al. Breast Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc. Netw. 2022, 20, 691–722. [Google Scholar] [CrossRef]
- Giuliano, A.E.; Connolly, J.L.; Edge, S.B.; Mittendorf, E.A.; Rugo, H.S.; Solin, L.J.; Weaver, D.L.; Winchester, D.J.; Hortobagyi, G.N. Breast Cancer-Major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J. Clin. 2017, 67, 290–303. [Google Scholar] [CrossRef] [PubMed]
- Yoon, E.C.; Schwartz, C.; Brogi, E.; Ventura, K.; Wen, H.; Darvishian, F. Impact of biomarkers and genetic profiling on breast cancer prognostication: A comparative analysis of the 8th edition of breast cancer staging system. Breast J. 2019, 25, 829–837. [Google Scholar] [CrossRef]
- Ahmed, S.; Pati, S.; Le, D.; Haider, K.; Iqbal, N. The prognostic and predictive role of 21-gene recurrence scores in hormone receptor-positive early-stage breast cancer. J. Surg. Oncol. 2020, 122, 144–154. [Google Scholar] [CrossRef]
- Brufsky, A.M. Predictive and prognostic value of the 21-gene recurrence score in hormone receptor-positive, node-positive breast cancer. Am. J. Clin. Oncol. 2014, 37, 404–410. [Google Scholar] [CrossRef]
- Kantor, O.; Bao, J.; Jaskowiak, N.; Yao, K.; Tseng, J. The Prognostic Value of the AJCC 8th Edition Staging System for Patients Undergoing Neoadjuvant Chemotherapy for Breast Cancer. Ann. Surg. Oncol. 2020, 27, 352–358. [Google Scholar] [CrossRef]
- Sparano, J.A.; Crager, M.R.; Tang, G.; Gray, R.J.; Stemmer, S.M.; Shak, S. Development and Validation of a Tool Integrating the 21-Gene Recurrence Score and Clinical-Pathological Features to Individualize Prognosis and Prediction of Chemotherapy Benefit in Early Breast Cancer. J. Clin. Oncol. 2021, 39, 557–564. [Google Scholar] [CrossRef]
- AACR Project GENIE Consortium. AACR Project GENIE: Powering Precision Medicine through an International Consortium. Cancer Discov. 2017, 7, 818–831. [Google Scholar] [CrossRef]
- European Society for Medical Oncology (ESMO). Catalyzing Integration of Genomic and Clinical Datasets across Multiple Cancer Institutions Worldwide. Available online: https://www.esmo.org/oncology-news/archive/catalyzing-integration-of-genomic-and-clinical-datasets-across-multiple-cancer-institutions-worldwide (accessed on 16 November 2023).
- Argentina Association of Clinical Oncology Research. The Genomics Evidence Neoplasia Information Exchange Database 2020; Argentina Association of Clinical Oncology Research: Buenos Aires, Argentina, 2020. [Google Scholar]
- Sondka, Z.; Bamford, S.; Cole, C.G.; Ward, S.A.; Dunham, I.; Forbes, S.A. The COSMIC Cancer Gene Census: Describing genetic dysfunction across all human cancers. Nat. Rev. Cancer 2018, 18, 696–705. [Google Scholar] [CrossRef] [PubMed]
- Ahn, K.S.; O’Brien, D.; Kang, Y.N.; Mounajjed, T.; Kim, Y.H.; Kim, T.; Kocher, J.A.; Allotey, L.K.; Borad, M.J.; Roberts, L.R.; et al. Prognostic subclass of intrahepatic cholangiocarcinoma by integrative molecular-clinical analysis and potential targeted approach. Hepatol. Int. 2019, 13, 490–500. [Google Scholar] [CrossRef] [PubMed]
- Gendoo, D.M.A. Bioinformatics and computational approaches for analyzing patient-derived disease models in cancer research. Comput. Struct. Biotechnol. J. 2020, 18, 375–380. [Google Scholar] [CrossRef]
- Ramos, A.H.; Lichtenstein, L.; Gupta, M.; Lawrence, M.S.; Pugh, T.J.; Saksena, G.; Meyerson, M.; Getz, G. Oncotator: Cancer variant annotation tool. Hum. Mutat. 2015, 36, 2423. [Google Scholar] [CrossRef]
- Saeed, A.I.; Sharov, V.; White, J.; Li, J.; Liang, W.; Bhagabati, N.; Braisted, J.; Klapa, M.; Currier, T.; Thiagarajan, M.; et al. TM4: A free, open-source system for microarray data management and analysis. Biotechniques 2003, 34, 374–378. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Zhou, B.; Pache, L.; Chang, M.; Khodabakhshi, A.H.; Tanaseichuk, O.; Benner, C.; Chanda, S.K. Metascape provides a biologist-oriented resource for the analysis of systems-level datasets. Nat. Commun. 2019, 10, 1523. [Google Scholar] [CrossRef]
- Valle, J.W.; Lamarca, A.; Goyal, L.; Barriuso, J.; Zhu, A.X. New Horizons for Precision Medicine in Biliary Tract Cancers. Cancer Discov. 2017, 7, 943–962. [Google Scholar] [CrossRef]
- Wardell, C.P.; Fujita, M.; Yamada, T.; Simbolo, M.; Fassan, M.; Karlic, R.; Polak, P.; Kim, J.; Hatanaka, Y.; Maejima, K.; et al. Genomic characterization of biliary tract cancers identifies driver genes and predisposing mutations. J. Hepatol. 2018, 68, 959–969. [Google Scholar] [CrossRef] [PubMed]
- Farshidfar, F.; Zheng, S.; Gingras, M.; Newton, Y.; Shih, J.; Robertson, A.G.; Hinoue, T.; Hoadley, K.A.; Gibb, E.A.; Roszik, J.; et al. Integrative Genomic Analysis of Cholangiocarcinoma Identifies Distinct IDH-Mutant Molecular Profiles. Cell Rep. 2017, 19, 2878–2880. [Google Scholar] [CrossRef] [PubMed]
- Goeppert, B.; Toth, R.; Singer, S.; Albrecht, T.; Lipka, D.B.; Lutsik, P.; Brocks, D.; Baehr, M.; Muecke, O.; Assenov, Y.; et al. Integrative Analysis Defines Distinct Prognostic Subgroups of Intrahepatic Cholangiocarcinoma. Hepatology 2019, 69, 2091–2106. [Google Scholar] [CrossRef] [PubMed]
- Jusakul, A.; Cutcutache, I.; Yong, C.H.; Lim, J.Q.; Huang, M.N.; Padmanabhan, N.; Nellore, V.; Kongpetch, S.; Ng, A.W.T.; Ng, L.M.; et al. Whole-Genome and Epigenomic Landscapes of Etiologically Distinct Subtypes of Cholangiocarcinoma. Cancer Discov. 2017, 7, 1116–1135. [Google Scholar] [CrossRef]
- Torbenson, M.S. Morphologic Subtypes of Hepatocellular Carcinoma. Gastroenterol. Clin. N. Am. 2017, 46, 365–391. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Kwong, L.N.; Javle, M. Genomic Profiling of Biliary Tract Cancers and Implications for Clinical Practice. Curr. Treat. Options Oncol. 2016, 17, 58. [Google Scholar] [CrossRef]
- Javle, M.; Bekaii-Saab, T.; Jain, A.; Wang, Y.; Kelley, R.K.; Wang, K.; Kang, H.C.; Catenacci, D.; Ali, S.; Krishnan, S.; et al. Biliary cancer: Utility of next-generation sequencing for clinical management. Cancer 2016, 122, 3838–3847. [Google Scholar] [CrossRef]
- Lowery, M.A.; Ptashkin, R.; Jordan, E.; Berger, M.F.; Zehir, A.; Capanu, M.; Kemeny, N.E.; O’Reilly, E.M.; El-Dika, I.; Jarnagin, W.R.; et al. Comprehensive Molecular Profiling of Intrahepatic and Extrahepatic Cholangiocarcinomas: Potential Targets for Intervention. Clin. Cancer Res. 2018, 24, 4154–4161. [Google Scholar] [CrossRef]
- Marks, E.I.; Yee, N.S. Molecular genetics and targeted therapeutics in biliary tract carcinoma. World J. Gastroenterol. 2016, 22, 1335–1347. [Google Scholar] [CrossRef] [PubMed]
- Offin, M.; Liu, D.; Drilon, A. Tumor-Agnostic Drug Development. Am. Soc. Clin. Oncol. Educ. Book 2018, 38, 184–187. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Kim, J.; Byeon, S.; Jang, K.; Hong, J.Y.; Lee, J.; Park, S.H.; Park, J.O.; Park, Y.S.; Lim, H.Y.; et al. Programmed Death Ligand 1 Expression as a Prognostic Marker in Patients with Advanced Biliary Tract Cancer. Oncology 2021, 99, 365–372. [Google Scholar] [CrossRef]
- Yoon, J.G.; Kim, M.H.; Jang, M.; Kim, H.; Hwang, H.K.; Kang, C.M.; Lee, W.J.; Kang, B.; Lee, C.; Lee, M.G.; et al. Molecular Characterization of Biliary Tract Cancer Predicts Chemotherapy and Programmed Death 1/Programmed Death-Ligand 1 Blockade Responses. Hepatology 2021, 74, 1914–1931. [Google Scholar] [CrossRef]
- Gao, Z.; Chen, J.; Li, X.; Shi, Y.; Tang, Z.; Liu, W.; Zhang, X.; Huang, A.; Luo, X.; Gao, Q.; et al. KRAS acting through ERK signaling stabilizes PD-L1 via inhibiting autophagy pathway in intrahepatic cholangiocarcinoma. Cancer Cell Int. 2022, 22, 128. [Google Scholar] [CrossRef] [PubMed]
- Nussinov, R.; Tsai, C.; Jang, H. Anticancer drug resistance: An update and perspective. Drug Resist. Updat. 2021, 59, 100796. [Google Scholar] [CrossRef]
- Hariharan, D.; Saied, A.; Kocher, H.M. Analysis of mortality rates for gallbladder cancer across the world. HPB 2008, 10, 327–331. [Google Scholar] [CrossRef]
- Bertuccio, P.; Malvezzi, M.; Carioli, G.; Hashim, D.; Boffetta, P.; El-Serag, H.B.; La Vecchia, C.; Negri, E. Global trends in mortality from intrahepatic and extrahepatic cholangiocarcinoma. J. Hepatol. 2019, 71, 104–114. [Google Scholar] [CrossRef]
- Grgurevic, I.; Bozin, T.; Mikus, M.; Kukla, M.; O’Beirne, J. Hepatocellular Carcinoma in Non-Alcoholic Fatty Liver Disease: From Epidemiology to Diagnostic Approach. Cancers 2021, 13, 5844. [Google Scholar] [CrossRef] [PubMed]
- Marinelli, I.; Guido, A.; Fuccio, L.; Farioli, A.; Panni, V.; Giaccherini, L.; Arcelli, A.; Ercolani, G.; Brandi, G.; Cammelli, S.; et al. Clinical Target Volume in Biliary Carcinoma: A Systematic Review of Pathological Studies. Anticancer Res. 2017, 37, 955–961. [Google Scholar] [CrossRef]
- Clevers, H.; Nusse, R. Wnt/β-catenin signaling and disease. Cell 2012, 149, 1192–1205. [Google Scholar] [CrossRef] [PubMed]
- Clevers, H. The Paneth cell, caloric restriction, and intestinal integrity. N. Engl. J. Med. 2012, 367, 1560–1561. [Google Scholar] [CrossRef]
- Yang, X.; Liu, Q.; Zou, J.; Li, Y.; Xie, X. Identification of a Prognostic Index Based on a Metabolic-Genomic Landscape Analysis of Hepatocellular Carcinoma (HCC). Cancer Manag. Res. 2021, 13, 5683–5698. [Google Scholar] [CrossRef] [PubMed]
- Sheinson, D.M.; Wong, W.B.; Flores, C.; Ogale, S.; Gross, C.P. Association between Medicare’s National Coverage Determination and Utilization of Next-Generation Sequencing. JCO Oncol. Pract. 2021, 17, e1774–e1784. [Google Scholar] [CrossRef] [PubMed]
| Genes | Alteration Types | CCA | GBC | HCC | Total | X2 | p Value |
|---|---|---|---|---|---|---|---|
| TERT | Upstream gene variant | 8 | 5 | 90 | 103 | 135.51 | <0.001 |
| CTNNB1 | Oncogenic mutations | 3 | 7 | 71 | 81 | 107.85 | <0.001 |
| KRAS | Oncogenic mutations | 50 | 12 | 1 | 63 | 62.95 | <0.001 |
| IDH1 | Oncogenic mutations | 46 | 1 | 2 | 49 | 80.86 | <0.001 |
| FGFR2 | Translocations | 13 | 1 | 0 | 14 | 22.43 | <0.001 |
| PBRM1 | Truncating mutations | 11 | 2 | 0 | 13 | 15.85 | <0.001 |
| BAP1 | Truncating mutations | 10 | 1 | 1 | 12 | 13.5 | 0.001 |
| MDM2 | CNA amplifications | 8 | 13 | 0 | 21 | 12.29 | 0.002 |
| CCNE1 | CNA amplifications | 3 | 12 | 1 | 16 | 12.88 | 0.002 |
| NFE2L2 | Oncogenic mutations | 1 | 0 | 8 | 9 | 12.67 | 0.002 |
| SMAD4 | Inactivating mutations | 5 | 11 | 0 | 16 | 11.38 | 0.003 |
| AXIN1 | Inactivating mutations | 0 | 5 | 11 | 16 | 11.38 | 0.003 |
| CDKN2A | CNA homo deletion | 24 | 23 | 7 | 54 | 10.11 | 0.006 |
| ATM | Inactivating mutations | 8 | 0 | 2 | 10 | 10.4 | 0.006 |
| JAK1 | Oncogenic mutations | 1 | 1 | 8 | 10 | 9.8 | 0.007 |
| PBRM1 | Inactivating mutations | 10 | 3 | 1 | 14 | 9.57 | 0.008 |
| KDR | Oncogenic mutations | 4 | 0 | 9 | 13 | 9.38 | 0.009 |
| NRAS | Oncogenic mutations | 9 | 2 | 1 | 12 | 9.5 | 0.009 |
| ERBB2 | CNA amplifications | 7 | 10 | 0 | 17 | 9.29 | 0.01 |
| MYC | CNA amplifications | 6 | 7 | 18 | 31 | 8.58 | 0.014 |
| BRAF | Oncogenic mutations | 11 | 1 | 6 | 18 | 8.33 | 0.016 |
| SF3B1 | Oncogenic mutations | 11 | 1 | 7 | 19 | 8 | 0.018 |
| ERBB2 | Oncogenic mutations | 8 | 8 | 0 | 16 | 8 | 0.018 |
| SMAD4 | Oncogenic mutations | 11 | 13 | 2 | 26 | 7.92 | 0.019 |
| SMAD4 | Truncating mutations | 3 | 7 | 0 | 10 | 7.4 | 0.025 |
| RAD21 | CNA amplifications | 0 | 3 | 7 | 10 | 7.4 | 0.025 |
| IDH2 | Oncogenic mutations | 6 | 0 | 2 | 8 | 7 | 0.03 |
| CDK12 | CNA amplifications | 2 | 6 | 0 | 8 | 7 | 0.03 |
| ERBB3 | CNA amplifications | 2 | 6 | 0 | 8 | 7 | 0.03 |
| KRAS | CNA amplifications | 2 | 6 | 0 | 8 | 7 | 0.03 |
| FGFR2 | Oncogenic mutations | 5 | 0 | 1 | 6 | 7 | 0.03 |
| TET1 | Oncogenic mutations | 5 | 1 | 0 | 6 | 7 | 0.03 |
| TSC1 | Oncogenic mutations | 5 | 0 | 1 | 6 | 7 | 0.03 |
| CDK6 | CNA amplifications | 1 | 5 | 0 | 6 | 7 | 0.03 |
| SUZ12 | Oncogenic mutations | 0 | 1 | 5 | 6 | 7 | 0.03 |
| FAT1 | Oncogenic mutations | 13 | 4 | 5 | 22 | 6.64 | 0.036 |
| PIK3CA | Oncogenic mutations | 16 | 16 | 5 | 37 | 6.54 | 0.038 |
| TP53 | Truncating mutations | 7 | 17 | 7 | 31 | 6.45 | 0.04 |
| NTRK1 | CNA amplifications | 2 | 1 | 7 | 10 | 6.2 | 0.045 |
| RB1 | Inactivating mutations | 1 | 2 | 7 | 10 | 6.2 | 0.045 |
| Overall (n = 311) | Molecular Subtypes (n = 311) | Tissue of Origin Subtypes (n = 311) | ||||||
|---|---|---|---|---|---|---|---|---|
| HC-1 33 (10.6) | HC-2 177 (56.9) | HC-3 101 (32.5) | p-Value | CCA 107 (34.4) | GBC 85 (27.3) | HCC 119 (38.3) | p-Value | |
| Characteristic | ||||||||
| Sex | 0.05 | <0.001 | ||||||
| Male | 18 (10.0) | 112 (62.6) | 49 (27.4) | 61 (34.1) | 26 (14.5) | 92 (51.4) | ||
| Female | 15 (11.4) | 65 (49.2) | 52 (39.4) | 46 (34.8) | 59 (44.7) | 27 (20.5) | ||
| Age Group | 0.22 | 0.4 | ||||||
| <55 years old | 7 (9.8) | 35 (49.4) | 29 (40.8) | 30 (42.3) | 20 (28.2) | 21 (29.5) | ||
| 55–69 years old | 17 (10.6) | 90 (55.9) | 54 (33.5) | 53 (32.9) | 45 (28.0) | 63 (39.1) | ||
| >69 years old | 9 (11.4) | 52 (65.8) | 18 (22.8) | 24 (30.4) | 20 (25.3) | 35 (44.3) | ||
| Race | 0.77 | 0.01 | ||||||
| White | 22 (9.4) | 132 (56.7) | 79 (33.9) | 92 (39.5) | 60 (25.8) | 81 (34.8) | ||
| Asian | 4 (13.3) | 15 (50.0) | 11 (36.7) | 5 (16.7) | 10 (33.3) | 15 (50.0) | ||
| Black | 3 (14.3) | 12 (57.1) | 6 (28.6) | 4 (19.1) | 10 (47.6) | 7 (33.3) | ||
| Other | 4 (14.8) | 18 (66.7) | 5 (18.5) | 6 (22.2) | 5 (18.5) | 16 (59.2) | ||
| Ethnicity | 0.57 | 0.77 | ||||||
| Non-Hispanic | 30 (10.4) | 167 (57.8) | 92 (31.8) | 98 (33.9) | 79 (27.3) | 112 (38.8) | ||
| Hispanic | 2 (11.8) | 9 (52.9) | 6 (35.3) | 8 (47.1) | 4 (23.5) | 5 (29.4) | ||
| Unknown | 1 (20.0) | 1 (20.0) | 3 (60.0) | 1 (20.0) | 2 (40.0) | 2 (40.0) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scholer, A.J.; Marcus, R.K.; Garland-Kledzik, M.; Ghosh, D.; Ensenyat-Mendez, M.; Germany, J.; Santamaria-Barria, J.A.; Khader, A.; Orozco, J.I.J.; Goldfarb, M. Exploring the Genomic Landscape of Hepatobiliary Cancers to Establish a Novel Molecular Classification System. Cancers 2024, 16, 325. https://doi.org/10.3390/cancers16020325
Scholer AJ, Marcus RK, Garland-Kledzik M, Ghosh D, Ensenyat-Mendez M, Germany J, Santamaria-Barria JA, Khader A, Orozco JIJ, Goldfarb M. Exploring the Genomic Landscape of Hepatobiliary Cancers to Establish a Novel Molecular Classification System. Cancers. 2024; 16(2):325. https://doi.org/10.3390/cancers16020325
Chicago/Turabian StyleScholer, Anthony J., Rebecca K. Marcus, Mary Garland-Kledzik, Debopriya Ghosh, Miquel Ensenyat-Mendez, Joshua Germany, Juan A. Santamaria-Barria, Adam Khader, Javier I. J. Orozco, and Melanie Goldfarb. 2024. "Exploring the Genomic Landscape of Hepatobiliary Cancers to Establish a Novel Molecular Classification System" Cancers 16, no. 2: 325. https://doi.org/10.3390/cancers16020325
APA StyleScholer, A. J., Marcus, R. K., Garland-Kledzik, M., Ghosh, D., Ensenyat-Mendez, M., Germany, J., Santamaria-Barria, J. A., Khader, A., Orozco, J. I. J., & Goldfarb, M. (2024). Exploring the Genomic Landscape of Hepatobiliary Cancers to Establish a Novel Molecular Classification System. Cancers, 16(2), 325. https://doi.org/10.3390/cancers16020325





