Data-Driven Assisted Decision Making for Surgical Procedure of Hepatocellular Carcinoma Resection and Prognostic Prediction: Development and Validation of Machine Learning Models
Abstract
Simple Summary
Abstract
1. Introduction
- A data-driven HCC surgical-assisted decision-making system was developed for the first time, and relatively satisfactory results were obtained from the external test set.
- Three high-performing ensemble learning models were developed, all of which outperformed the mainstream ensemble models. Based on this, the associated web server was deployed.
- After rigorous feature screening, efficient feature expression (radiomics-clinical) was explored.
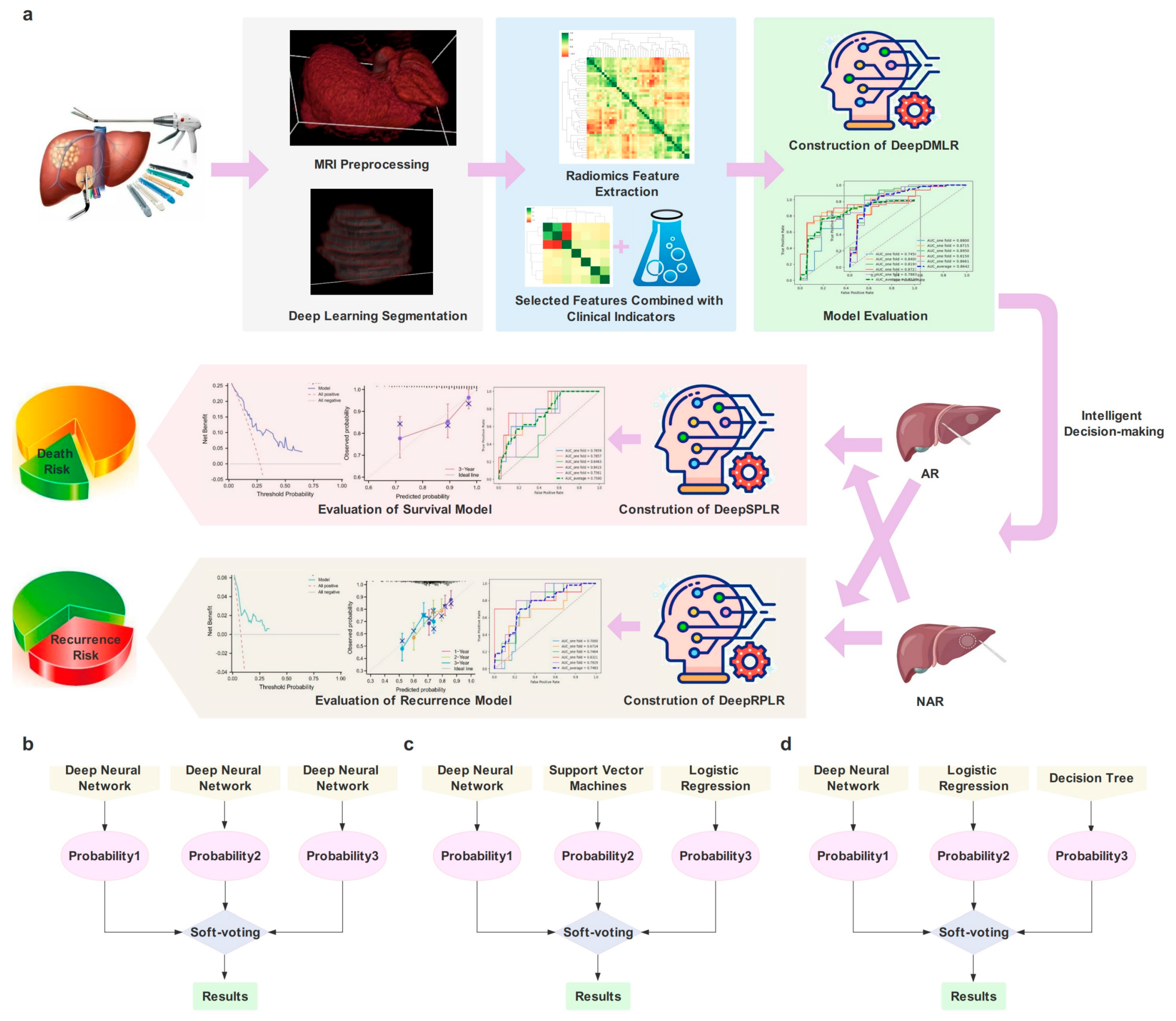
2. Materials and Methods
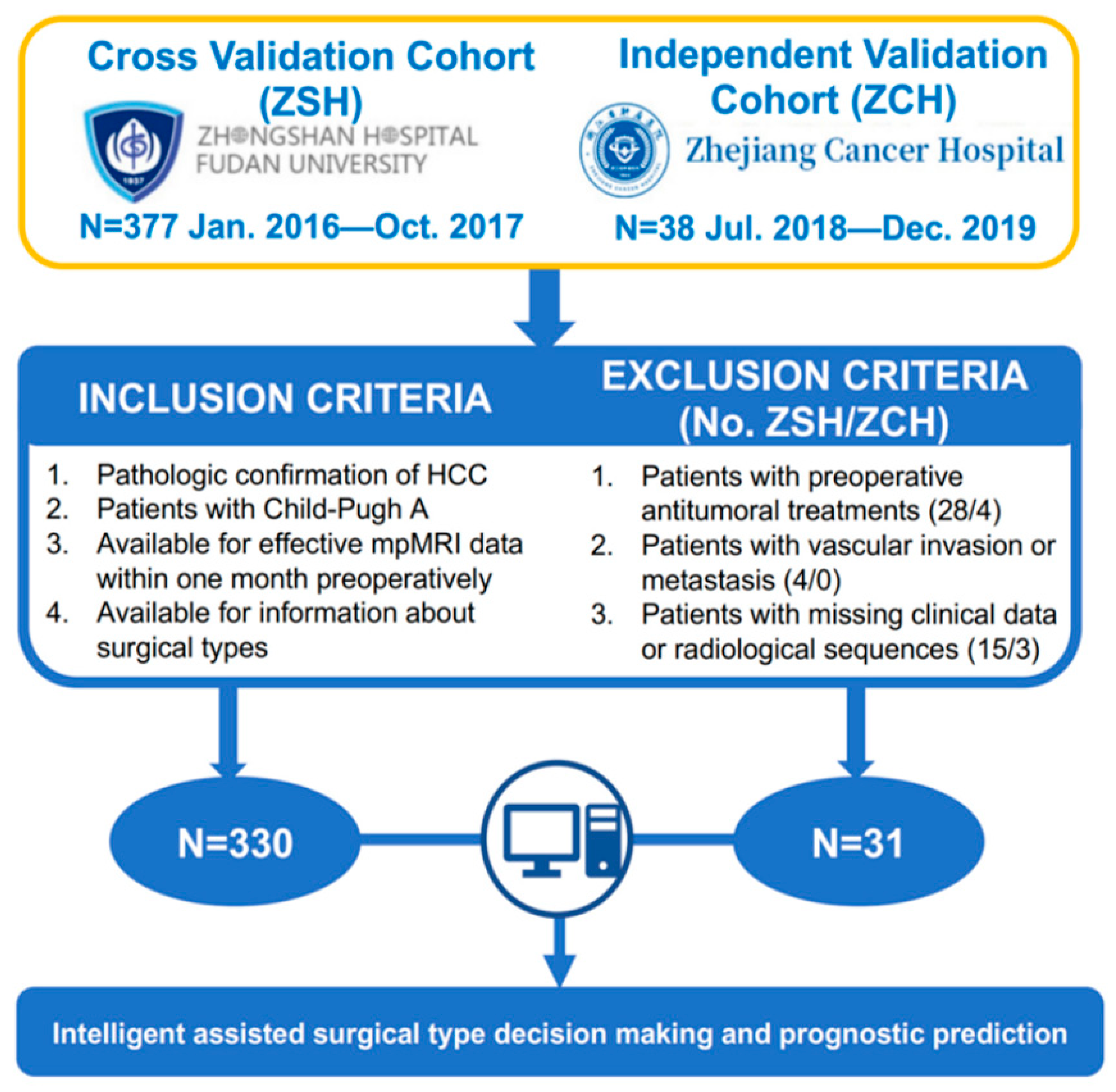
2.1. Patients Enrollment
2.2. Decision-Making of Surgical Procedure by the Experienced Surgeons
2.3. Follow-Up
2.4. Clinical Characteristics Selection
2.5. Image Acquisition, Annotation and Preprocessing
2.6. Automatic Segmentation Models Construction
2.7. Radiomics Features Extraction and Selection
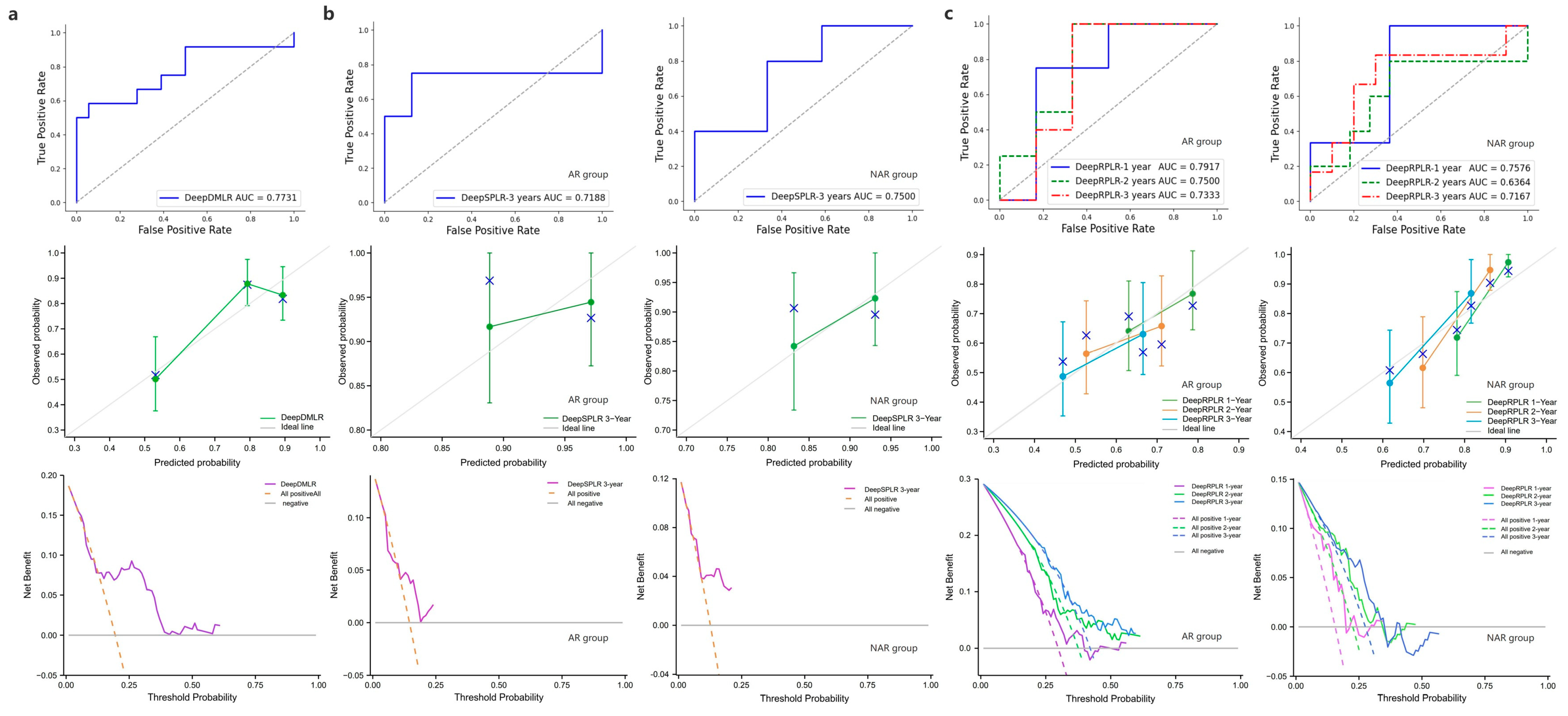
2.8. Decision Making and Prognosis Models Construction
2.8.1. Deep Model of Decision-Making of Liver Resection (DeepDMLR)
2.8.2. Deep Model of Survival Prediction after Liver Resection (DeepSPLR)
2.8.3. Deep Model of Recurrence Prediction after Liver Resection (DeepRPLR)
2.8.4. Model Comparison
2.9. Experimental Setup
2.10. Statistics
3. Results
3.1. Patient’s Demographics and Baseline Indicators
3.2. Segmentation Results
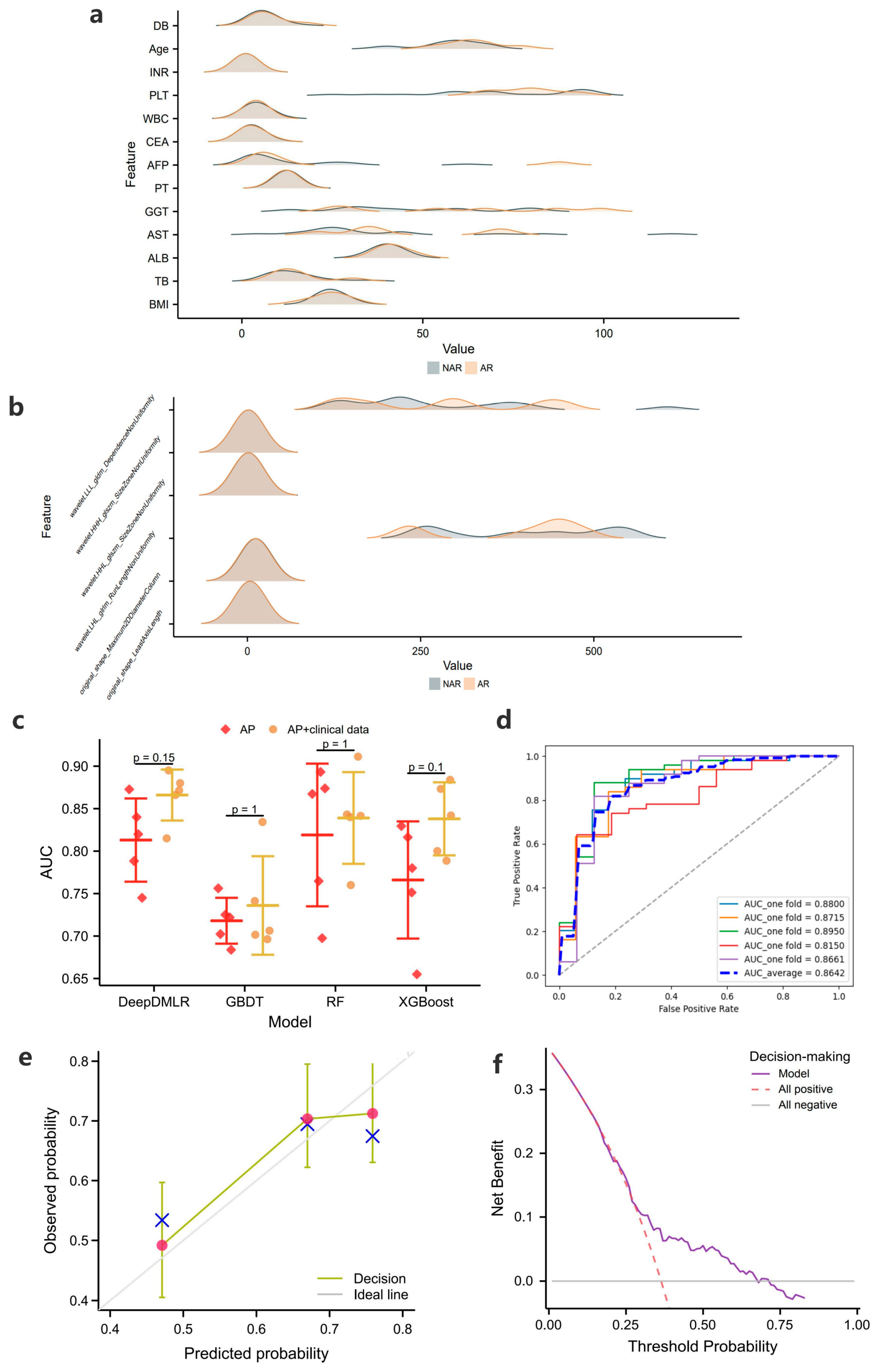
3.3. Radiomics Features Included
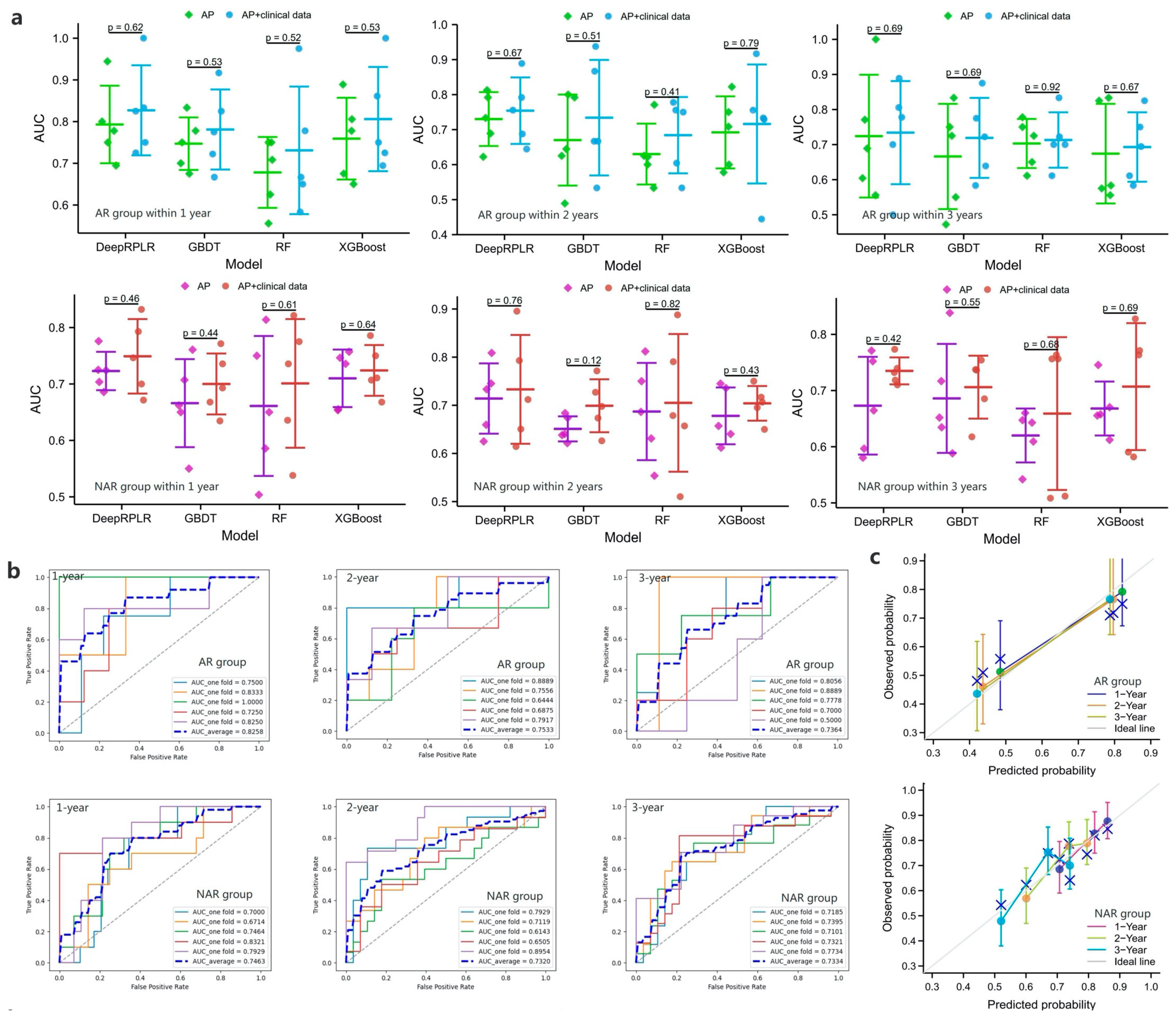
3.4. Results of Decision-Making and Prognosis Prediction Models
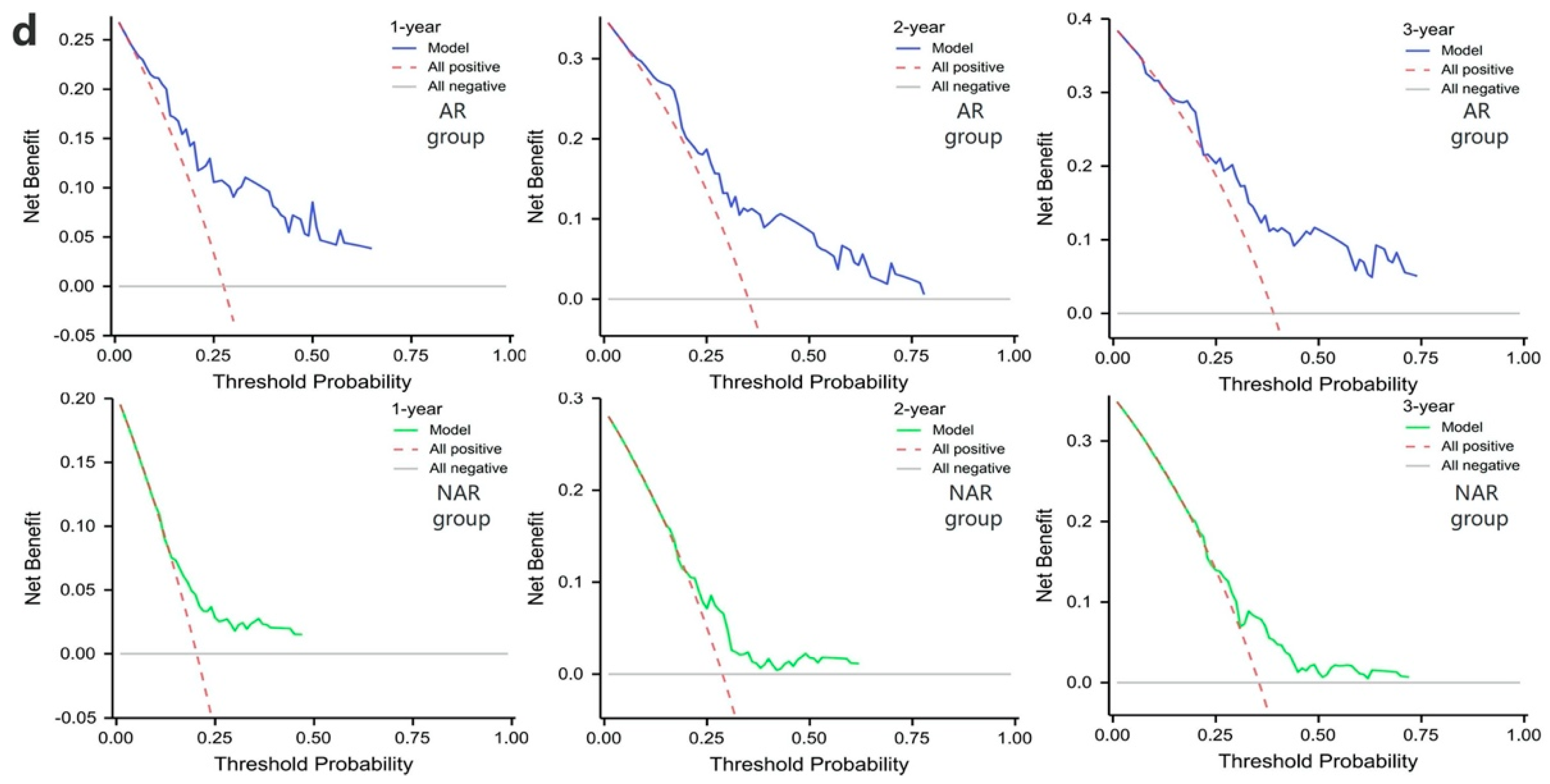
3.4.1. DeepDMLR and Comparison Models
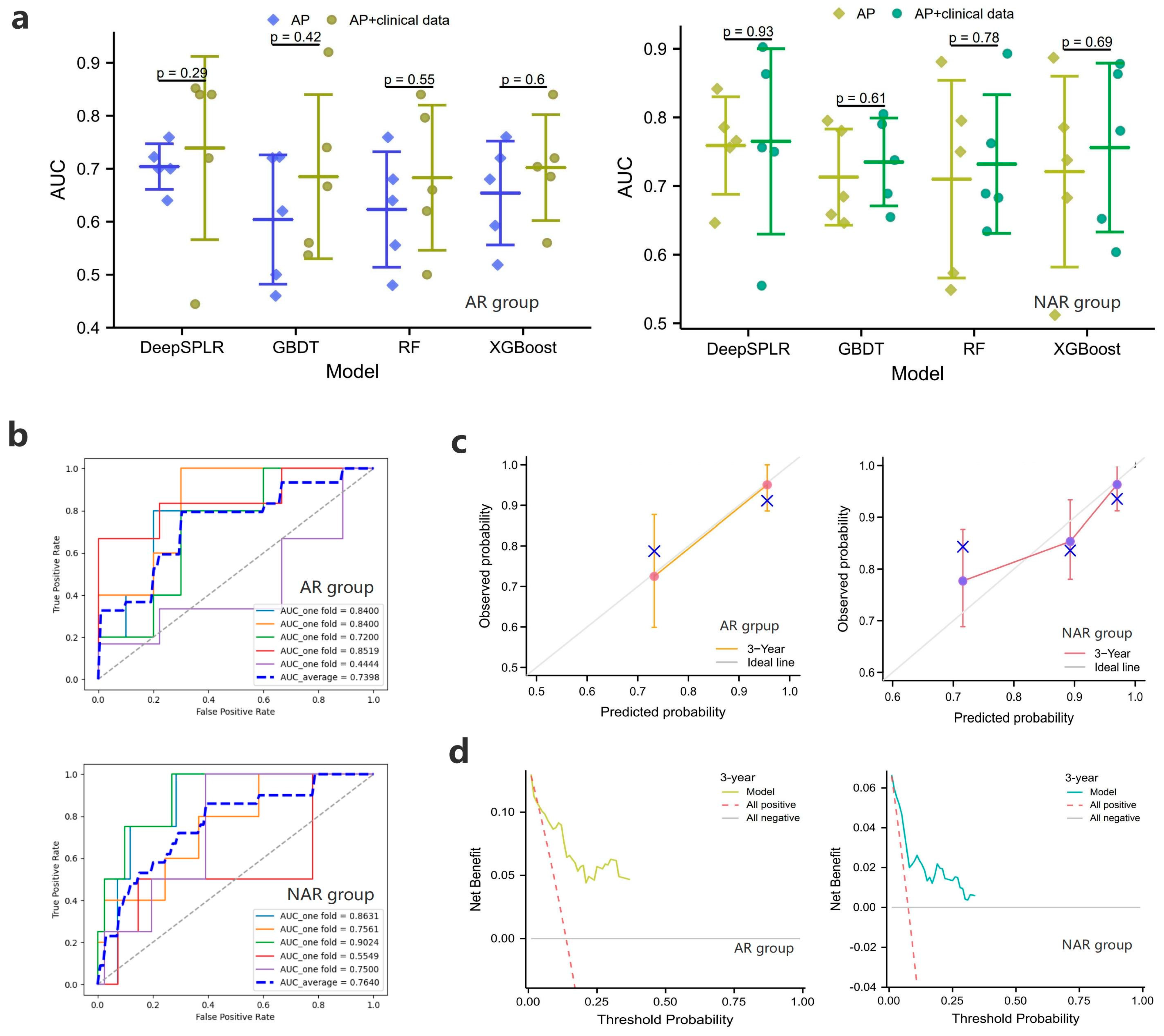
3.4.2. DeepSPLR and Comparison Models
3.4.3. DeepRPLR and Comparison Models
3.5. External Validation Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fu, X.W.; Song, C.Q. Identification and Validation of Pyroptosis-Related Gene Signature to Predict Prognosis and Reveal Immune Infiltration in Hepatocellular Carcinoma. Front. Cell Dev. Biol. 2021, 9, 748039. [Google Scholar] [CrossRef]
- Donne, R.; Lujambio, A. The liver cancer immune microenvironment: Therapeutic implications for hepatocellular carcinoma. Hepatology 2022. [Google Scholar] [CrossRef]
- Sun, Y.; Zhang, W.; Bi, X.; Yang, Z.; Tang, Y.; Jiang, L.; Bi, F.; Chen, M.; Cheng, S.; Chi, Y.; et al. Systemic Therapy for Hepatocellular Carcinoma: Chinese Consensus-Based Interdisciplinary Expert Statements. Liver Cancer 2022, 11, 192–208. [Google Scholar] [CrossRef] [PubMed]
- Chong, C.C.; Fuks, D.; Lee, K.F.; Zhao, J.J.; Choi, G.H.; Sucandy, I.; Chiow, A.K.H.; Marino, M.V.; Gastaca, M.; Wang, X.; et al. Propensity Score-Matched Analysis Comparing Robotic and Laparoscopic Right and Extended Right Hepatectomy. JAMA Surg. 2022, 157, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Reig, M.; Forner, A.; Rimola, J.; Ferrer-Fàbrega, J.; Burrel, M.; Garcia-Criado, Á.; Kelley, R.K.; Galle, P.R.; Mazzaferro, V.; Salem, R.; et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J. Hepatol. 2022, 76, 681–693. [Google Scholar] [CrossRef]
- Azari, F.; Zhang, K.; Kennedy, G.T.; Chang, A.; Nadeem, B.; Delikatny, E.J.; Singhal, S. Precision Surgery Guided by Intraoperative Molecular Imaging. J. Nucl. Med. 2022, 63, 1620–1627. [Google Scholar] [CrossRef]
- Gotohda, N.; Cherqui, D.; Geller, D.A.; Abu Hilal, M.; Berardi, G.; Ciria, R.; Abe, Y.; Aoki, T.; Asbun, H.J.; Chan, A.C.Y.; et al. Expert Consensus Guidelines: How to safely perform minimally invasive anatomic liver resection. J. Hepatobiliary Pancreat. Sci. 2022, 29, 16–32. [Google Scholar] [CrossRef]
- Dai, X.M.; Xiang, Z.Q.; Wang, Q.; Li, H.J.; Zhu, Z. Oncological outcomes of anatomic versus non-anatomic resections for small hepatocellular carcinoma: Systematic review and meta-analysis of propensity-score matched studies. World J. Surg. Oncol. 2022, 20, 299. [Google Scholar] [CrossRef]
- Kwon, J.H.; Lee, J.W.; Lee, J.W.; Lee, Y.J. Effects of Anatomical or Non-Anatomical Resection of Hepatocellular Carcinoma on Survival Outcome. J. Clin. Med. 2022, 11, 1369. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.M.; Zhou, C.Y.; Chen, X.P.; Zhang, Z.W. Anatomic resection improved the long-term outcome of hepatocellular carcinoma patients with microvascular invasion: A prospective cohort study. World J. Gastrointest. Oncol. 2021, 13, 2190–2202. [Google Scholar] [CrossRef] [PubMed]
- Kitano, Y.; Hayashi, H.; Matsumoto, T.; Nakao, Y.; Kaida, T.; Mima, K.; Imai, K.; Yamashita, Y.I.; Baba, H. The efficacy of anatomic resection for hepatocellular carcinoma within Milan criteria: A retrospective single-institution case-matched study. Eur. J. Surg. Oncol. 2022, 48, 2008–2013. [Google Scholar] [CrossRef]
- Minagawa, M.; Mise, Y.; Omichi, K.; Ichida, H.; Mizuno, T.; Yoshioka, R.; Imamura, H.; Yanagisawa, N.; Inoue, Y.; Takahashi, Y.; et al. Anatomic Resection for Hepatocellular Carcinoma: Prognostic Impact Assessed from Recurrence Treatment. Ann. Surg. Oncol. 2022, 29, 913–921. [Google Scholar] [CrossRef]
- Meng, X.P.; Tang, T.Y.; Ding, Z.M.; Wang, J.; Lu, C.Q.; Yu, Q.; Xia, C.; Zhang, T.; Long, X.; Xiao, W.; et al. Preoperative Microvascular Invasion Prediction to Assist in Surgical Plan for Single Hepatocellular Carcinoma: Better Together with Radiomics. Ann. Surg. Oncol. 2022, 29, 2960–2970. [Google Scholar] [CrossRef]
- Kim, H.Y.; Lampertico, P.; Nam, J.Y.; Lee, H.C.; Kim, S.U.; Sinn, D.H.; Seo, Y.S.; Lee, H.A.; Park, S.Y.; Lim, Y.S.; et al. An artificial intelligence model to predict hepatocellular carcinoma risk in Korean and Caucasian patients with chronic hepatitis B. J. Hepatol. 2022, 76, 311–318. [Google Scholar] [CrossRef]
- Turco, S.; Tiyarattanachai, T.; Ebrahimkheil, K.; Eisenbrey, J.; Kamaya, A.; Mischi, M.; Lyshchik, A.; Kaffas, A.E. Interpretable Machine Learning for Characterization of Focal Liver Lesions by Contrast-Enhanced Ultrasound. IEEE Trans. Ultrason. Ferroelectr. Freq. Control. 2022, 69, 1670–1681. [Google Scholar] [CrossRef]
- Fu, S.; Lai, H.; Huang, M.; Li, Q.; Liu, Y.; Zhang, J.; Huang, J.; Chen, X.; Duan, C.; Li, X.; et al. Multi-task deep learning network to predict future macrovascular invasion in hepatocellular carcinoma. EClinicalMedicine 2021, 42, 101201. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Liu, Y.; Xu, N.; Sun, Y.; Fu, S.; Wu, Y.; Liu, C.; Cui, L.; Liu, Z.; Chang, Z.; et al. Development and validation of a deep learning model for survival prognosis of transcatheter arterial chemoembolization in patients with intermediate-stage hepatocellular carcinoma. Eur. J. Radiol. 2022, 156, 110527. [Google Scholar] [CrossRef] [PubMed]
- Zeng, J.; Zeng, J.; Lin, K.; Lin, H.; Wu, Q.; Guo, P.; Zhou, W.; Liu, J. Development of a machine learning model to predict early recurrence for hepatocellular carcinoma after curative resection. Hepatobiliary Surg. Nutr. 2022, 11, 176–187. [Google Scholar] [CrossRef]
- Gao, W.; Wang, W.; Song, D.; Yang, C.; Zhu, K.; Zeng, M.; Rao, S.X.; Wang, M. A predictive model integrating deep and radiomics features based on gadobenate dimeglumine-enhanced MRI for postoperative early recurrence of hepatocellular carcinoma. Radiol. Med. 2022, 127, 259–271. [Google Scholar] [CrossRef]
- Xie, E.; Wang, W.; Yu, Z.; Anandkumar, A.; Alvarez, J.M.; Luo, P. SegFormer: Simple and Efficient Design for Semantic Segmentation with Transformers. Adv. Neural Inf. Process. Syst. 2021, 34, 12077–12090. [Google Scholar]
- Wang, L.; Wu, M.; Li, R.; Xu, X.; Zhu, C.; Feng, X. MVI-Mind: A Novel Deep-Learning Strategy Using Computed Tomography (CT)-Based Radiomics for End-to-End High Efficiency Prediction of Microvascular Invasion in Hepatocellular Carcinoma. Cancers 2022, 14, 2956. [Google Scholar] [CrossRef]
- Yin, X.X.; Sun, L.; Fu, Y.; Lu, R.; Zhang, Y. U-Net-Based Medical Image Segmentation. J. Healthc. Eng. 2022, 2022, 4189781. [Google Scholar] [CrossRef]
- Zhou, Z.; Siddiquee, M.M.R.; Tajbakhsh, N.; Liang, J. UNet++: A Nested U-Net Architecture for Medical Image Segmentation. In Deep Learning in Medical Image Analysis and Multimodal Learning for Clinical Decision Support; Springer: Berlin/Heidelberg, Germany, 2018; Volume 11045, pp. 3–11. [Google Scholar] [CrossRef]
- Chen, D.; Liu, J.; Zang, L.; Xiao, T.; Zhang, X.; Li, Z.; Zhu, H.; Gao, W.; Yu, X. Integrated Machine Learning and Bioinformatic Analyses Constructed a Novel Stemness-Related Classifier to Predict Prognosis and Immunotherapy Responses for Hepatocellular Carcinoma Patients. Int. J. Biol. Sci. 2022, 18, 360–373. [Google Scholar] [CrossRef]
- An, C.; Yang, H.; Yu, X.; Han, Z.Y.; Cheng, Z.; Liu, F.; Dou, J.; Li, B.; Li, Y.; Li, Y.; et al. A Machine Learning Model Based on Health Records for Predicting Recurrence After Microwave Ablation of Hepatocellular Carcinoma. J. Hepatocell. Carcinoma 2022, 9, 671–684. [Google Scholar] [CrossRef]
- Dong, Z.; Lin, Y.; Lin, F.; Luo, X.; Lin, Z.; Zhang, Y.; Li, L.; Li, Z.P.; Feng, S.T.; Cai, H.; et al. Prediction of Early Treatment Response to Initial Conventional Transarterial Chemoembolization Therapy for Hepatocellular Carcinoma by Machine-Learning Model Based on Computed Tomography. J. Hepatocell. Carcinoma 2021, 8, 1473–1484. [Google Scholar] [CrossRef] [PubMed]
- Ivanics, T.; Nelson, W.; Patel, M.S.; Claasen, M.; Lau, L.; Gorgen, A.; Abreu, P.; Goldenberg, A.; Erdman, L.; Sapisochin, G. The Toronto Postliver Transplantation Hepatocellular Carcinoma Recurrence Calculator: A Machine Learning Approach. Liver Transplant. 2022, 28, 593–602. [Google Scholar] [CrossRef] [PubMed]
- Qadri, S.F.; Shen, L.; Ahmad, M.; Qadri, S.; Zareen, S.S.; Khan, S. OP-convNet: A Patch Classification-Based Framework for CT Vertebrae Segmentation. IEEE Access 2021, 9, 158227–158240. [Google Scholar] [CrossRef]
- Bi, L.; Fulham, M.; Li, N.; Liu, Q.; Song, S.; Dagan Feng, D.; Kim, J. Recurrent feature fusion learning for multi-modality pet-ct tumor segmentation. Comput. Methods Programs Biomed. 2021, 203, 106043. [Google Scholar] [CrossRef] [PubMed]
- Anagnostou, V.; Niknafs, N.; Marrone, K.; Bruhm, D.C.; White, J.R.; Naidoo, J.; Hummelink, K.; Monkhorst, K.; Lalezari, F.; Lanis, M.; et al. Multimodal genomic features predict outcome of immune checkpoint blockade in non-small-cell lung cancer. Nat. Cancer 2020, 1, 99–111. [Google Scholar] [CrossRef]
- Gao, R.; Zhao, S.; Aishanjiang, K.; Cai, H.; Wei, T.; Zhang, Y.; Liu, Z.; Zhou, J.; Han, B.; Wang, J.; et al. Deep learning for differential diagnosis of malignant hepatic tumors based on multi-phase contrast-enhanced CT and clinical data. J. Hematol. Oncol. 2021, 14, 154. [Google Scholar] [CrossRef]
- Ali, S.; Hussain, A.; Aich, S.; Park, M.S.; Chung, M.P.; Jeong, S.H.; Song, J.W.; Lee, J.H.; Kim, H.C. A Soft Voting Ensemble-Based Model for the Early Prediction of Idiopathic Pulmonary Fibrosis (IPF) Disease Severity in Lungs Disease Patients. Life 2021, 11, 1092. [Google Scholar] [CrossRef] [PubMed]
- Jones, I.A.; Van Oyen, M.P.; Lavieri, M.S.; Andrews, C.A.; Stein, J.D. Predicting rapid progression phases in glaucoma using a soft voting ensemble classifier exploiting Kalman filtering. Health Care Manag. Sci. 2021, 24, 686–701. [Google Scholar] [CrossRef] [PubMed]
- Tasci, E.; Uluturk, C.; Ugur, A. A voting-based ensemble deep learning method focusing on image augmentation and preprocessing variations for tuberculosis detection. Neural Comput. Appl. 2021, 33, 15541–15555. [Google Scholar] [CrossRef] [PubMed]
- Yüzkat, M.; Ilhan, H.O.; Aydin, N. Multi-model CNN fusion for sperm morphology analysis. Comput. Biol. Med. 2021, 137, 104790. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.W.; Eom, J.; Kim, S.; Kim, H.; Ahn, S.S.; Ku, C.R.; Kim, E.H.; Lee, E.J.; Kim, S.H.; Lee, S.K. Radiomics with Ensemble Machine Learning Predicts Dopamine Agonist Response in Patients with Prolactinoma. J. Clin. Endocrinol. Metab. 2021, 106, e3069–e3077. [Google Scholar] [CrossRef]
| Characteristic | Training Cohort | External Validation Cohort | ||||
|---|---|---|---|---|---|---|
| AR (n = 82) | NAR (n = 248) | p | AR (n = 13) | NAR (n = 18) | p | |
| Cirrhosis (%) | 0.021 * | 0.275 | ||||
| No | 53 (64.6%) | 122 (49.2%) | 3 (23.1%) | 8 (44.4%) | ||
| Yes | 29 (35.4%) | 126 (50.8%) | 10 (76.9%) | 10 (55.5%) | ||
| BCLC grade (%) | 0.115 | 0.208 | ||||
| 0 | 11 (13.4%) | 55 (22.2%) | 0 (0%) | 0 (0%) | ||
| A | 66 (80.5%) | 170 (68.5%) | 9 (69.2%) | 16 (88.9%) | ||
| B | 5 (6.1%) | 23 (9.3%) | 4 (30.8%) | 2 (11.1%) | ||
| Hepatitis C (%) | 0.460 | 0.419 | ||||
| No | 81 (98.8%) | 240 (96.8%) | 12 (92.3%) | 18 (100.0%) | ||
| Yes | 1 (1.2%) | 8 (3.2%) | 1 (7.7%) | 0 (0%) | ||
| BMI, median (IQR) | 23.88 (21.99, 25.91) | 23.88 (21.96, 26.12) | 0.770 | 21.97 (20.4, 24.24) | 21.5 (19.64, 26.46) | 0.650 |
| TB, median (IQR) or mean ± SD | 11.85 (9.62, 15.78) | 11.6 (8.57, 15.3) | 0.516 | 12.6 ± 3.55 | 14.12 ± 5.96 | 0.419 |
| ALB, median (IQR) | 41 (38.25, 44) | 42 (39, 44) | 0.441 | 43 (41.2, 45.8) | 43.2 (31.02, 46.77) | 0.575 |
| AST, median (IQR) | 29 (23.25, 43.75) | 26.5 (21, 34) | 0.010 * | 35 (32, 42) | 28 (23, 36.5) | 0.123 |
| GGT, median (IQR) | 52.5 (36, 96.5) | 44 (28, 78.25) | 0.019 * | 68 (35, 117) | 33.5 (21, 44.5) | 0.041 * |
| PT, median (IQR) | 11.5 (11.03, 12) | 11.6 (11.07, 12.2) | 0.487 | 12.4 (11.6, 12.8) | 12.2 (11.6, 13) | 0.733 |
| AFP, median (IQR) | 16.4 (5.4, 536.43) | 32.7 (4.4, 395.55) | 0.793 | 10.2 (2.8, 156) | 42.4 (2.77, 315.1) | 0.603 |
| CEA, median (IQR) | 2.2 (1.42, 3.1) | 2.3 (1.6, 3.3) | 0.482 | 1.36 (1.11, 2.42) | 1.73 (1.01, 2.51) | 0.423 |
| WBC, median (IQR) | 5.59 (4.57, 6.83) | 5.11 (4.04, 6.24) | 0.018 * | 6.4 (4.5, 8.5) | 6.25 (4.5, 7.57) | 0.645 |
| PLT, median (IQR) or mean ± SD | 164.5 (130.5, 220) | 148.5 (113, 184.25) | 0.013 * | 170.92 ± 75.84 | 146.11 ± 52.38 | 0.289 |
| INR, median (IQR) | 1 (0.96, 1.07) | 1.02 (0.97, 1.08) | 0.273 | 1.03 (0.97, 1.07) | 1.04 (0.98, 1.09) | 0.269 |
| Age, median (IQR) | 56.5 (47, 63.75) | 59 (51, 65) | 0.104 | 63 (57, 68) | 63.5 (56.5, 68.5) | 0.588 |
| DB, median (IQR) or mean ± SD | 4.9 (3.92, 6.27) | 4.7 (3.7, 6.5) | 0.391 | 5.1 ± 1.71 | 5.61 ± 2.34 | 0.514 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, L.; Song, D.; Wang, W.; Li, C.; Zhou, Y.; Zheng, J.; Rao, S.; Wang, X.; Shao, G.; Cai, J.; et al. Data-Driven Assisted Decision Making for Surgical Procedure of Hepatocellular Carcinoma Resection and Prognostic Prediction: Development and Validation of Machine Learning Models. Cancers 2023, 15, 1784. https://doi.org/10.3390/cancers15061784
Wang L, Song D, Wang W, Li C, Zhou Y, Zheng J, Rao S, Wang X, Shao G, Cai J, et al. Data-Driven Assisted Decision Making for Surgical Procedure of Hepatocellular Carcinoma Resection and Prognostic Prediction: Development and Validation of Machine Learning Models. Cancers. 2023; 15(6):1784. https://doi.org/10.3390/cancers15061784
Chicago/Turabian StyleWang, Liyang, Danjun Song, Wentao Wang, Chengquan Li, Yiming Zhou, Jiaping Zheng, Shengxiang Rao, Xiaoying Wang, Guoliang Shao, Jiabin Cai, and et al. 2023. "Data-Driven Assisted Decision Making for Surgical Procedure of Hepatocellular Carcinoma Resection and Prognostic Prediction: Development and Validation of Machine Learning Models" Cancers 15, no. 6: 1784. https://doi.org/10.3390/cancers15061784
APA StyleWang, L., Song, D., Wang, W., Li, C., Zhou, Y., Zheng, J., Rao, S., Wang, X., Shao, G., Cai, J., Yang, S., & Dong, J. (2023). Data-Driven Assisted Decision Making for Surgical Procedure of Hepatocellular Carcinoma Resection and Prognostic Prediction: Development and Validation of Machine Learning Models. Cancers, 15(6), 1784. https://doi.org/10.3390/cancers15061784







