Qualitative and Semiquantitative Parameters of 18F-FDG-PET/CT as Predictors of Malignancy in Patients with Solitary Pulmonary Nodule
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. 18F-FDG PET/CT Acquisition and Analysis
2.3. Statistical Analysis
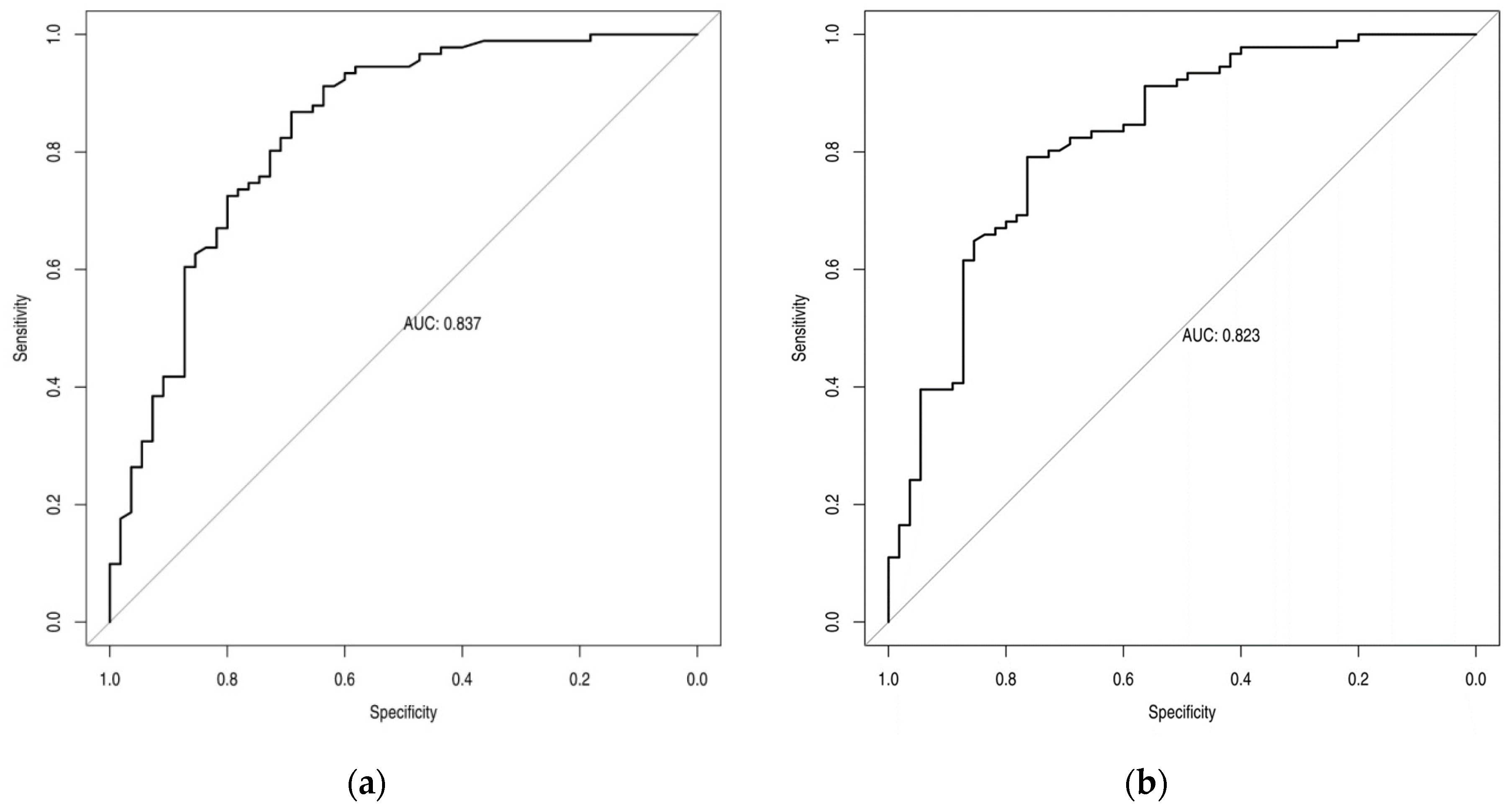
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cruickshank, A.; Stieler, G.; Ameer, F. Evaluation of the solitary pulmonary nodule. Intern. Med. J. 2019, 49, 306–315. [Google Scholar] [CrossRef] [PubMed]
- Sim, Y.T.; Poon, F.W. Imaging of solitary pulmonary nodule-a clinical review. Quant. Imaging Med. Surg. 2013, 3, 316–326. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.K.; Li, X.D.; Quan, J.T.; Ouyang, X.; Zheng, H. Diagnostic value of (18)F-FDG PET/CT for solitary nodular-type bronchoalveolar carcinoma. Nan Fang Yi Ke Da Xue Xue Bao 2015, 35, 114–116. [Google Scholar] [PubMed]
- Ruilong, Z.; Daohai, X.; Li, G.; Xiaohong, W.; Chunjie, W.; Lei, T. Diagnostic value of 18F-FDG-PET/CT for the evaluation of solitary pulmonary nodules: A systematic review and meta-analysis. Nucl. Med. Commun. 2017, 38, 67–75. [Google Scholar] [CrossRef]
- Paśnik, M.; Bestry, I.; Roszkowski-Śliż, K. Solitary pulmonary nodule-the role of imaging in the diagnostic process. Adv. Respir. Med. 2017, 85, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Ziai, P.; Hayeri, M.R.; Salei, A.; Salavati, A.; Houshmand, S.; Alavi, A.; Teytelboym, O.M. Role of Optimal Quantification of FDG PET Imaging in the Clinical Practice of Radiology. Radiographics 2016, 36, 481–496. [Google Scholar] [CrossRef]
- Steiger, S.; Arvanitakis, M.; Sick, B.; Weder, W.; Hillinger, S.; Burger, I.A. Analysis of Prognostic Values of Various PET Metrics in Preoperative (18)F-FDG PET for Early-Stage Bronchial Carcinoma for Progression-Free and Overall Survival: Significantly Increased Glycolysis Is a Predictive Factor. J. Nucl. Med. 2017, 58, 1925–1930. [Google Scholar] [CrossRef]
- Evangelista, L.; Cuocolo, A.; Pace, L.; Mansi, L.; Del Vecchio, S.; Miletto, P.; Sanfilippo, S.; Pellegrino, S.; Guerra, L.; Pepe, G.; et al. Performance of FDG-PET/CT in solitary pulmonary nodule based on pre-test likelihood of malignancy: Results from the ITALIAN retrospective multicenter trial. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 1898–1907. [Google Scholar] [CrossRef]
- McWilliams, A.; Tammemagi, M.C.; Mayo, J.R.; Roberts, H.; Liu, G.; Soghrati, K.; Yasufuku, K.; Martel, S.; Laberge, F.; Gingras, M.; et al. Probability of cancer in pulmonary nodules detected on first screening CT. N. Engl. J. Med. 2013, 369, 910–919. [Google Scholar] [CrossRef]
- Callister, M.E.; Baldwin, D.R.; Akram, A.R.; Barnard, S.; Cane, P.; Draffan, J.; Franks, K.; Gleeson, F.; Graham, R.; Malhotra, P.; et al. British Thoracic Society guidelines for the investigation and management of pulmonary nodules. Thorax 2015, 70 (Suppl. 2), ii1–ii54. [Google Scholar] [CrossRef]
- Erdogdu, E.; Ozkan, B.; Duman, S.; Agkoc, M.; Erturk, S.M.; Kara, M.; Toker, A. Predictors of Malignancy in Patients with Solitary Pulmonary Nodules Undergoing Pulmonary Resection. Clin. Respir. J. 2022, 16, 361–368. [Google Scholar] [CrossRef]
- Weir-McCall, J.R.; Harris, S.; Miles, K.A.; Qureshi, N.R.; Rintoul, R.C.; Dizdarevic, S.; Pike, L.; Cheow, H.K.; Gilbert, F.J.; Banerjee, A.; et al. Impact of solitary pulmonary nodule size on qualitative and quantitative assessment using 18F-fluorodeoxyglucose PET/CT: The SPUTNIK trial. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 1560–1569. [Google Scholar] [CrossRef] [PubMed]
- Hou, S.; Lin, X.; Wang, S.; Shen, Y.; Meng, Z.; Jia, Q.; Tan, J. Combination of Positron Emission Tomography/Computed Tomography and Chest Thin-Layer High-Resolution Computed Tomography for Evaluation of Pulmonary Nodules: Correlation with Imaging Features, Maximum Standardized Uptake Value, and Pathology. Medicine 2018, 97, e11640. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Hernández, G.; de Juan, R.; Samanes, A.; Verea, H.; Peñas, J.M.; Veres, A.; Lapeña, L.; Montz, R.; Carreras, J.L. Positron emission tomography using 18-FDG-PET in radiologically indeterminate pulmonary lesions. An. De Med. Interna 2004, 21, 12–16. [Google Scholar] [CrossRef]
- Soma, T.; Takeda, Y.; Tnabe, M.; Akiyama, Y.; Suzuki, T.; Yano, M.; Inagaki, K.; Morita, T.; Hara, T.; Kudo, K. Diagnostic efficacy of 18F-fluorodeoxy glucose-positron emission tomography in multiple solitary pulmonary nodules. Nihon Kokyuki Gakkai Zasshi 2000, 38, 854–859. [Google Scholar] [PubMed]
- Erdoğan, M.; Evrimler, Ş.; Aydın, H.; Karaibrahimoğlu, A.; Şengül, S.S. Solitary Pulmonary Nodule: Morphological Effects on Metabolic Activity Assessment. Mol. Imaging Radionucl. Ther. 2019, 28, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.Y.; Jeong, J.Y.; Lee, K.S.; Kim, H.J.; Han, J.; Kim, B.T.; Kim, J.; Shim, Y.M.; Kim, J.H.; Song, I. Solitary pulmonary nodular lung adenocarcinoma: Correlation of histopathologic scoring and patient survival with imaging biomarkers. Radiology 2012, 264, 884–893. [Google Scholar] [CrossRef]
- Lee, H.Y.; Han, J.; Lee, K.S.; Koo, J.H.; Jeong, S.Y.; Kim, B.T.; Cho, Y.S.; Shim, Y.M.; Kim, J.; Kim, K.; et al. Lung adenocarcinoma as a solitary pulmonary nodule: Prognostic determinants of CT, PET, and histopathologic findings. Lung Cancer 2009, 66, 379–385. [Google Scholar] [CrossRef]
- Lee, H.Y.; Lee, K.S.; Han, J.; Kim, B.T.; Cho, Y.S.; Shim, Y.M.; Kim, J. Mucinous versus nonmucinous solitary pulmonary nodular bronchioloalveolar carcinoma: CT and FDG PET findings and pathologic comparisons. Lung Cancer 2009, 65, 170–175. [Google Scholar] [CrossRef]
- Bianconi, F.; Palumbo, I.; Fravolini, M.L.; Rondini, M.; Minestrini, M.; Pascoletti, G.; Nuvoli, S.; Spanu, A.; Scialpi, M.; Aristei, C.; et al. Form Factors as Potential Imaging Biomarkers to Differentiate Benign vs. Malignant Lung Lesions on CT Scans. Sensors 2022, 22, 5044. [Google Scholar] [CrossRef]
- Palumbo, B.; Bianconi, F.; Palumbo, I.; Fravolini, M.L.; Minestrini, M.; Nuvoli, S.; Stazza, M.L.; Rondini, M.; Spanu, A. Value of Shape and Texture Features from (18)F-FDG PET/CT to Discriminate between Benign and Malignant Solitary Pulmonary Nodules: An Experimental Evaluation. Diagnostics 2020, 10, 696. [Google Scholar] [CrossRef]
- Bianconi, F.; Fravolini, M.L.; Palumbo, I.; Pascoletti, G.; Nuvoli, S.; Rondini, M.; Spanu, A.; Palumbo, B. Impact of Lesion Delineation and Intensity Quantisation on the Stability of Texture Features from Lung Nodules on CT: A Reproducible Study. Diagnostics 2021, 11, 1224. [Google Scholar] [CrossRef] [PubMed]
- Bianconi, F.; Fravolini, M.L.; Pizzoli, S.; Palumbo, I.; Minestrini, M.; Rondini, M.; Nuvoli, S.; Spanu, A.; Palumbo, B. Comparative evaluation of conventional and deep learning methods for semi-automated segmentation of pulmonary nodules on CT. Quant. Imaging Med. Surg. 2021, 11, 3286–3305. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Lin, W.; Xie, D.; Yu, Y.; Cao, H.; Liao, G.; Wu, S.; Yao, L.; Wang, Z.; Wang, M.; et al. Development and validation of a preoperative CT-based radiomic nomogram to predict pathology invasiveness in patients with a solitary pulmonary nodule: A machine learning approach, multicenter, diagnostic study. Eur. Radiol. 2022, 32, 1983–1996. [Google Scholar] [CrossRef]
- Chen, S.; Harmon, S.; Perk, T.; Li, X.; Chen, M.; Li, Y.; Jeraj, R. Using Neighborhood Gray Tone Difference Matrix Texture Features on Dual Time Point PET/CT Images to Differentiate Malignant from Benign FDG-Avid Solitary Pulmonary Nodules. Cancer Imaging 2019, 19, 56. [Google Scholar] [CrossRef] [PubMed]


| Characteristics of Patients | Value |
|---|---|
| Age (years) | 68.23 ±8.32 |
| Smoking history | 70 (47.95%) |
| Occupational exposure | 18 (12.33%) |
| Family history | 5 (3.42%) |
| Previous cancer | 22 (15.07%) |
| TBC during childhood | 8 (5.48%) |
| COPD | 25 (17.12%) |
| Pulmonary fibrosis | 8 (5.48%) |
| Emphysema | 11 (7.53%) |
| Nodule Lung Localization and Size | Value |
| Superior lobe | 74 (50.68%) |
| Medium lobe | 14 (9.59%) |
| Inferior lobe | 58 (39.73%) |
| Nodule size | 18.28 ± 8.32 mm |
| Histology | Value |
|---|---|
| Primary lung carcinomas | 91 (62.33%) |
| Adenocarcinoma | 63 (69.23%) |
| Spinocellular carcinoma | 11 (12.09%) |
| Squamous carcinoma | 6 (6.59%) |
| Neuroendocrine tumor | 8 (8.79%) |
| Rare histotypes | 3 (3.30%) |
| Benign lesions | 55 (37.67%) |
| Overall Population (n = 146) | Malignant SPNs (n = 91) | Non Malignant SPNs (n = 55) | |
|---|---|---|---|
| Absent/faint uptake | 20 | 4 | 16 |
| Moderate uptake | 44 | 13 | 31 |
| Intense uptake | 82 | 74 | 8 |
| Overall Population (n = 146) | Malignant SPNs (n = 91) | Non Malignant SPNs (n = 55) | Optimal Cut-Offs Values | |
|---|---|---|---|---|
| SUVmax | 5.82 (±5.18) | 7.89 (±2.24) | 2.24 (±1.73) | 3.625 |
| SUVmean | 3 (±2.12) | 3.76 (±2.59) | 1.67 (±1.15) | 2.51 |
| MTV | 2.90 (±2.72) | 3.39 (±2.86) | 1.20 (±1.20) | 2.55 |
| TLG | 10.70 (±13.48) | 16.36 (±15.87) | 1.63 (±2.33) | 11.8 |
| Sensitivity | Specificity | |
|---|---|---|
| SUVmax | 86.6% | 69.1% |
| SUVmean | 79.1% | 76.3% |
| MTV | 74.7% | 70.9% |
| TLG | 66% | 83.6% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Corica, F.; De Feo, M.S.; Stazza, M.L.; Rondini, M.; Marongiu, A.; Frantellizzi, V.; Nuvoli, S.; Farcomeni, A.; De Vincentis, G.; Spanu, A. Qualitative and Semiquantitative Parameters of 18F-FDG-PET/CT as Predictors of Malignancy in Patients with Solitary Pulmonary Nodule. Cancers 2023, 15, 1000. https://doi.org/10.3390/cancers15041000
Corica F, De Feo MS, Stazza ML, Rondini M, Marongiu A, Frantellizzi V, Nuvoli S, Farcomeni A, De Vincentis G, Spanu A. Qualitative and Semiquantitative Parameters of 18F-FDG-PET/CT as Predictors of Malignancy in Patients with Solitary Pulmonary Nodule. Cancers. 2023; 15(4):1000. https://doi.org/10.3390/cancers15041000
Chicago/Turabian StyleCorica, Ferdinando, Maria Silvia De Feo, Maria Lina Stazza, Maria Rondini, Andrea Marongiu, Viviana Frantellizzi, Susanna Nuvoli, Alessio Farcomeni, Giuseppe De Vincentis, and Angela Spanu. 2023. "Qualitative and Semiquantitative Parameters of 18F-FDG-PET/CT as Predictors of Malignancy in Patients with Solitary Pulmonary Nodule" Cancers 15, no. 4: 1000. https://doi.org/10.3390/cancers15041000
APA StyleCorica, F., De Feo, M. S., Stazza, M. L., Rondini, M., Marongiu, A., Frantellizzi, V., Nuvoli, S., Farcomeni, A., De Vincentis, G., & Spanu, A. (2023). Qualitative and Semiquantitative Parameters of 18F-FDG-PET/CT as Predictors of Malignancy in Patients with Solitary Pulmonary Nodule. Cancers, 15(4), 1000. https://doi.org/10.3390/cancers15041000







