Estimating the Time Toxicity of Contemporary Systemic Treatment Regimens for Advanced Esophageal and Gastric Cancers
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Overview
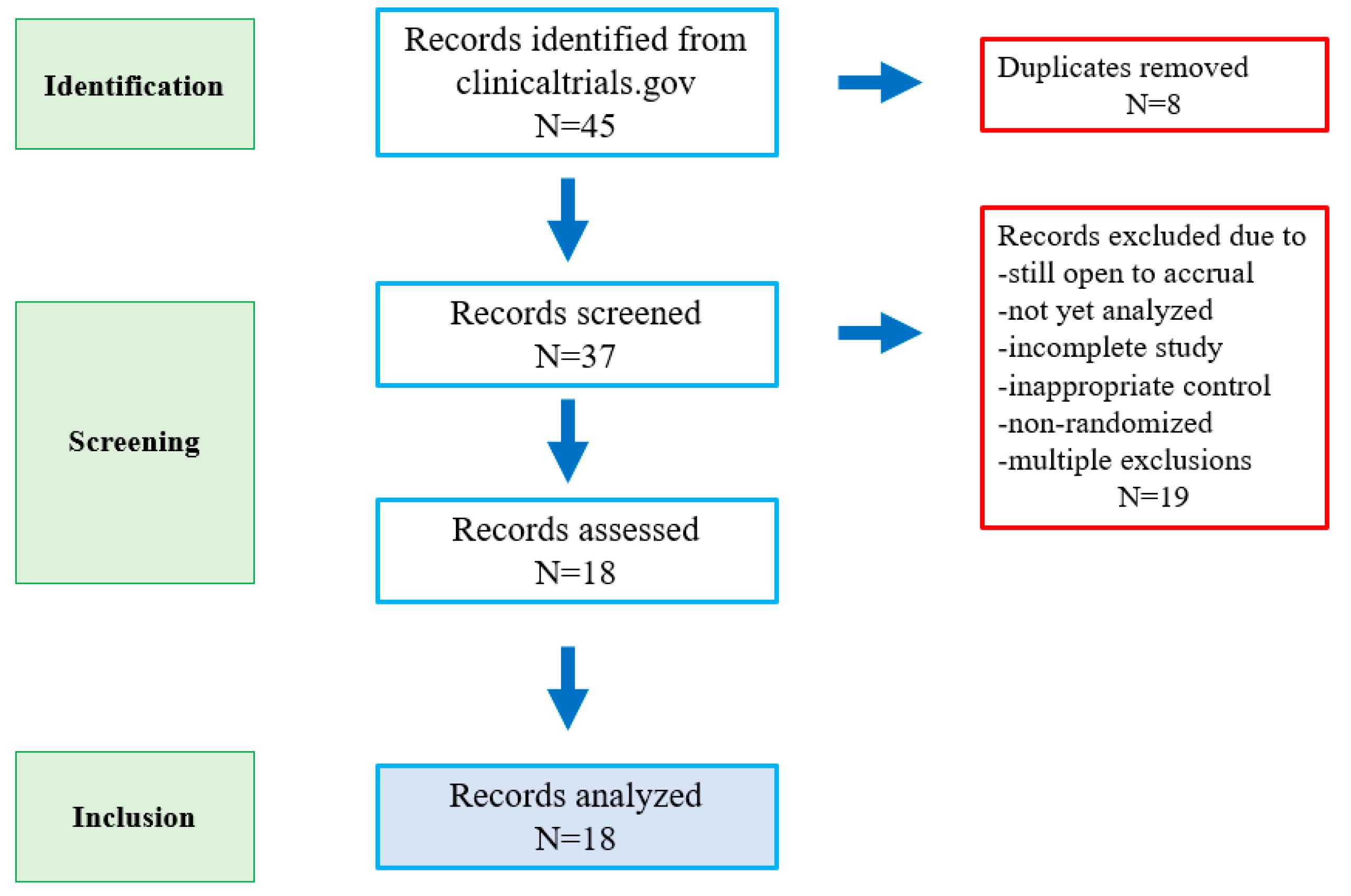
2.2. Literature Search and Selection
2.3. Data Extraction
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wong, M.C.S.; Huang, J.; Chan, P.S.F.; Choi, P.; Lao, X.Q.; Chan, S.M.; Teoh, A.; Liang, P. Global Incidence and Mortality of Gastric Cancer, 1980–2018. JAMA Netw. Open 2021, 4, e2118457. [Google Scholar] [CrossRef]
- Hur, C.; Miller, M.; Kong, C.Y.; Dowling, E.C.; Nattinger, K.J.; Dunn, M.; Feuer, E.J. Trends in esophageal adenocarcinoma incidence and mortality. Cancer 2013, 119, 1149–1158. [Google Scholar] [CrossRef]
- Hogner, A.; Moehler, M. Immunotherapy in Gastric Cancer. Curr. Oncol. 2022, 29, 1559–1574. [Google Scholar] [CrossRef]
- Gupta, A.; Jensen, E.H.; Virnig, B.A.; Beg, M.S. Time-related burdens of cancer care. JCO Oncol. Pract. 2022, 18, 245–246. [Google Scholar] [CrossRef]
- Fundytus, A.; Prasad, V.; Booth, C.M. Has the current oncology value paradigm forgotten patients’ time?: Too little of a good thing. JAMA Oncol. 2021, 7, 1757–1758. [Google Scholar] [CrossRef]
- Johnson, W.V.; Blaes, A.H.; Booth, C.M.; Ganguli, I.; Gupta, A. The unequal burden of time toxicity. Trends Cancer 2023, 9, 373–375. [Google Scholar] [CrossRef]
- Cheng, A.C.; Levy, M.A. Data Driven Approach to Burden of Treatment Measurement: A Study of Patients with Breast Cancer. AMIA Annu Symp Proc. 2016, 10, 1756–1763. [Google Scholar]
- Gupta, A.; Eisenhauer, E.A.; Booth, C.M. The Time Toxicity of Cancer Treatment. J. Clin. Oncol. 2022, 40, 1611–1615. [Google Scholar] [CrossRef]
- Rocque, G.B.; Williams, C.P.; Ingram, S.A.; Azuero, A.; Mennemeyer, S.T.; Pierce, J.Y.; Nipp, R.D.; Reeder-Hayes, K.E.; Kenzik, K.M. Health care-related time costs in patients with metastatic breast cancer. Cancer Med. 2020, 9, 8423–8431. [Google Scholar] [CrossRef]
- Hall, E.T.; Sridhar, D.; Singhal, S.; Fardeen, T.; Lahijani, S.; Trivedi, R.; Gray, C.; Schapira, L. Perceptions of time spent pursuing cancer care among patients, caregivers, and oncology professionals. Support. Care Cancer 2021, 29, 2493–2500. [Google Scholar] [CrossRef]
- Yabroff, K.R.; Davis, W.W.; Lamont, E.B.; Fahey, A.; Topor, M.; Brown, M.L.; Warren, J.L. Patient Time Costs Associated with Cancer Care. JNCI J. Natl. Cancer Inst. 2007, 99, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Rocque, G.B.; Williams, C.P.; Miller, H.D.; Azuero, A.; Wheeler, S.B.; Pisu, M.; Hull, O.; Rocconi, R.P.; Kenzik, K.M. Impact of Travel Time on Health Care Costs and Resource Use by Phase of Care for Older Patients with Cancer. J. Clin. Oncol. 2019, 37, 1935–1945. [Google Scholar] [CrossRef] [PubMed]
- Patruni, S.; Fayyaz, F.; Bien, J.; Phillip, T.; King, D.A. Immunotherapy in the Management of Esophagogastric Cancer: A Practical Review. JCO Oncol. Pract. 2023, 19, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Thawani, R.; Agrawal, N.; Taflin, N.; Kardosh, A.; Chen, E.Y.-S. Application of value framework to phase III trials of immune checkpoint inhibitors in esophageal and gastric cancer. J. Clin. Oncol. 2022, 40, e18817. [Google Scholar] [CrossRef]
- Garg, S.K.; Sarvepalli, S.S.; Parikh, M.P.; Wadhwa, V.; Jang, S.; Thota, P.N.; Sanaka, M.R. Inpatient burden of esophageal cancer and analysis of factors affecting in-hospital mortality and length of stay. Dis. Esophagus 2018, 31, doy022. [Google Scholar]
- Bange, E.M.; Doucette, A.; Gabriel, P.E.; Porterfield, F.; Harrigan, J.J.; Wang, R.; Wojcieszynski, A.P.; Boursi, B.; Mooney, B.I.; Reiss, K.A.; et al. Opportunity Costs of Receiving Palliative Chemotherapy for Metastatic Pancreatic Ductal Adenocarcinoma. JCO Oncol. Pract. 2020, 16, e678. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.-A.; Hao, S.B.; Boyd, B.A.; Mitsakos, A.; Irish, W.; Burke, A.M.; Parikh, A.A.; Snyder, R.A. Opportunity Costs of Surgical Resection and Perioperative Chemotherapy for Locoregional Pancreatic Adenocarcinoma. JCO Oncol. Pract. 2022, 18, 302–309. [Google Scholar] [CrossRef]
- Prasad, V.; Olivier, T.; Chen, E.Y.; Haslam, A. Estimation of time cost of anti-cancer drugs approved based on comparisons to best supportive care: A cross sectional analysis. J. Cancer Policy 2022, 34, 100363. [Google Scholar] [CrossRef]
- Banerjee, R.; George, M.; Gupta, A. Maximizing Home time for Persons with Cancer. CO Oncol. Pract. 2021, 17, 513–516. [Google Scholar] [CrossRef]
- Zimmerman, B.S.; Seidman, D.; Berger, N.; Cascetta, K.P.; Nezolosky, M.; Trlica, K.; Tiersten, A. Patient perception of telehealth services for breast and gynecologic oncology care during the COVID-19 pandemic: A single center survey-based study. J. Breast Cancer 2020, 23, 542–552. [Google Scholar] [CrossRef]
- Smrke, A.; Younger, E.; Wilson, R.; Husson, O.; Farag, S.; Merry, E.; Jones, R.L. Telemedicine during the COVID-19 pandemic: Impact on care for rare cancers. JCO Glob. Oncol. 2020, 6, 1046–1051. [Google Scholar] [CrossRef] [PubMed]
- Darcourt, J.G.; Aparicio, K.; Dorsey, P.M.; Ensor, J.E.; Zsigmond, E.M.; Wong, S.T.; Chang, J.C. Analysis of the implementation of telehealth visits for care of patients with cancer in Houston during the COVID-19 pandemic. JCO Oncol. Pract. 2021, 17, e36–e43. [Google Scholar] [CrossRef] [PubMed]
- O’neill, C.B.; Atoria, C.L.; O’reilly, E.M.; Henman, M.C.; Bach, P.B.; Elkin, E.B. ReCAP: Hospitalizations in Older Adults ith Advanced Cancer: The Role of Chemotherapy. J. Oncol. Pract. 2016, 12, 151–152. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; O’Callaghan, C.J.; Zhu, L.; Jonker, D.J.; Wong, R.P.; Colwell, B.; Moore, M.J.; Karapetis, C.S.; Tebbutt, N.C.; Shapiro, J.D.; et al. Evaluating the Time Toxicity of Cancer Treatment in the CCTG CO.17 Trial. JCO Oncol. Pract. 2023, 19, e859–e866. [Google Scholar] [CrossRef]
- Janjigian, Y.Y.; Shitara, K.; Moehler, M.; Garrido, M.; Salman, P.; Shen, L.; Wyrwicz, L.; Yamaguchi, K.; Skoczylas, T.; Bragagnoli, A.C.; et al. First-line nivolumab plus chemotherapy versus chemotherapy alone for advanced gastric, gastro-oesophageal junction, and oesophageal adenocarcinoma (CheckMate 649): A randomised, open-label, phase 3 trial. Lancet 2021, 3, 27–40. [Google Scholar] [CrossRef]
- Yabroff, K.R.; Kim, Y. Time costs associated with informal caregiving for cancer survivors. Cancer 2009, 115, 4362–4373. [Google Scholar] [CrossRef]
| Characteristics | N (%) |
|---|---|
| Immunotherapy Type | |
| Pembrolizumab | 8 (45%) |
| Nivolumab | 6 (33%) |
| Avelumab | 2 (11%) |
| Tislelizumab | 2 (11%) |
| Cancer Type | |
| Gastric and GE junction | 9 (50%) |
| Esophageal | 8 (44%) |
| Esophageal, GE junction, and gastric | 1 (6%) |
| Line of Therapy | |
| First-line metastatic | 9 (50%) |
| Second-line metastatic | 6 (33%) |
| Third-line metastatic | 2 (11%) |
| Adjuvant | 1 (6%) |
| Sample size (median, range) | 639 (94–1581) |
| Treatment Arms (N = 38) | |
| Chemotherapy only | 16 (42%) |
| Immunotherapy only | 12 (32%) |
| Chemotherapy with immunotherapy | 8 (21%) |
| Best supportive care | 2 (5%) |
| Median overall survival (median, range; N = 34) | 10.2 (4.1–17.5) months |
| Median progression-free survival (median, range; N = 34) | 4.0 (1.4–10.9) months |
| Objective response rate (median, range; N = 36) | 21% (0–74%) |
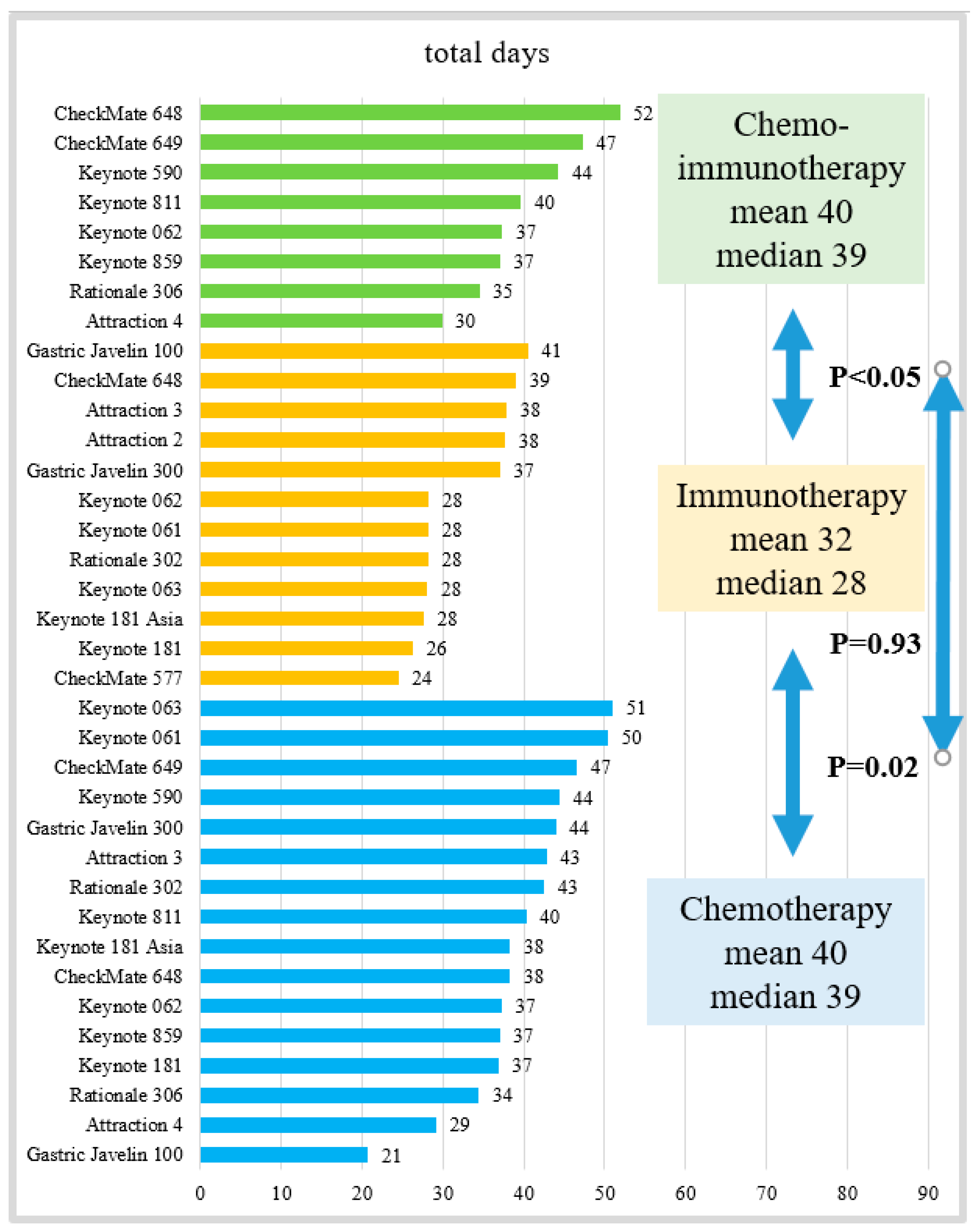
| Time Toxicity (Days) | Median Overall Survival (Months) | Proportion of Survival | |
|---|---|---|---|
| Median (Range) | Median (Range) | % | |
| Chemotherapy only (N = 16) | 39 (21–51) | 8.8 (5.0–17.2) a | 15% |
| Immunotherapy only (N = 12) | 28 (24–41) | 9.1 (4.6–13.7) b | 9% |
| Chemotherapy with immunotherapy (N = 8) | 39 (30–52) | 14.4 (12.5–17.5) c | 9% |
| Best supportive care (N = 2) | 9 (7–11) | 4.1 (4.1–4.1) d | 7% |
| p value | <0.01 | <0.01 |
| Study Name | Registration # (Pub Med PMID) | Cancer Type | Experimental Arm | Control Arm |
|---|---|---|---|---|
| Pembrolizumab | ||||
| KEYNOTE 590 | NCT03189719 (34454674) | Esophageal (all histology), 1st-line advanced/metastatic | 5-Flourouracil (5FU) and cisplatin with pembrolizumab | 5FU and cisplatin with placebo |
| KEYNOTE 181 Asia | NCT03933449 (34973513) | Esophageal (all histology), 2nd-line advanced/metastatic | Pembrolizumab | Docetaxel, paclitaxel, or irinotecan |
| KEYNOTE 181 | NCT02564263 (33026938) | Esophageal (all histology), 2nd-line advanced/metastatic | Pembrolizumab | Docetaxel, paclitaxel, or irinotecan |
| KEYNOTE 061 | NCT02370498 (29880231) | Gastric/GE junction adenocarcinoma, 2nd-line advanced/metastatic | Pembrolizumab | Paclitaxel |
| KEYNOTE 063 | NCT03019588 (34878659) | Gastric/GE junction adenocarcinoma (PD-L1 CPS ≥ 1), 2nd-line advanced/metastatic | Pembrolizumab | Paclitaxel |
| KEYNOTE 811 | NCT03615326 (34912120) | Gastric/GE junction adenocarcinoma (HER2+), 1st-line unresectable/metastatic | Chemotherapy with trastuzumab and pembrolizumab | 5FU and cisplatin, or capecitabine and oxaliplatin (CAPOX), with trastuzumab |
| KEYNOTE 062 | NCT02494583 (32880601) | Gastric/GE junction adenocarcinoma (HER2−, PD-L1 CPS ≥ 1), 1st-line advanced/metastatic | Chemotherapy with pembrolizumab (also has pembrolizumab monotherapy arm) | 5FU or capecitabine, and cisplatin, with placebo |
| KEYNOTE 859 | NCT03675737 (37293712) | Gastric/GE junction adenocarcinoma (HER2−) | FP or CAPOX with pembrolizumab | FP or CAPOX with placebo |
| Nivolumab | ||||
| CHECKMATE 648 | NCT03143153 (35108470) | Esophageal, (squamous), 1st-line unresectable, recurrent, or metastatic | 5FU and cisplatin with nivolumab (also has nivolumab with ipilimumab arm) | 5FU and cisplatin |
| CHECKMATE 649 | NCT02872116 (34102137) | Esophageal, GE junction, gastric (HER2− adenocarcinoma), 1st-line unresectable/metastatic | 5FU or capecitabine, and oxaliplatin (FOLFOX or CAPOX), with nivolumab | FOLFOX or CAPOX |
| ATTRACTION 4 | NCT02746796 (35030335) | GE junction, gastric (HER2− adenocarcinoma), 1st-line recurrent/advanced | Capecitabine or S-1 and oxaliplatin (CAPOX or SOX) with nivolumab | CAPOX or SOX |
| ATTRACTION 3 | NCT02569242 (31582355) | Esophageal (squamous), 2nd-line advanced/metastatic | Nivolumab | Docetaxel or paclitaxel |
| ATTRACTION 2 | NCT02267343 (28993052) | Gastric/GE junction adenocarcinoma, 3rd-line recurrent/metastatic | Nivolumab | Placebo |
| CHECKMATE 577 | NCT02743494 (33789008) | Esophageal (all histology), adjuvant after tri-modality therapy for resectable cancer | Nivolumab | Placebo |
| Avelumab | ||||
| Javelin Gastric 100 | NCT02625610 (33197226) | Gastric/GE junction adenocarcinoma, maintenance after induction 1st-line chemotherapy | Avelumab | Continuation of FOLFOX or CAPOX |
| Javelin Gastric 300 | NCT02625623 (30052729) | Gastric/GE junction adenocarcinoma, 2nd-line unresectable, recurrent or metastatic | Avelumab | Irinotecan or paclitaxel |
| Tislelizumab | ||||
| Rationale 302 | NCT03430843 (35442766) | Esophageal squamous cell carcinoma, 2nd-line unresectable or metastatic | Tislelizumab | Paclitaxel, docetaxel, or irinotecan |
| Rationale 306 | NCT03783442 (37080222) | Esophageal squamous cell carcinoma, 1st-line unresectable or metastatic | Cisplatin or oxaliplatin plus fluorouracil (5-FU); cisplatin or oxaliplatin plus capecitabine; cisplatin or oxaliplatin plus paclitaxel, with tislelizumab | Cisplatin or oxaliplatin plus fluorouracil (5-FU); cisplatin or oxaliplatin plus capecitabine; cisplatin or oxaliplatin plus paclitaxel, with placebo |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agrawal, N.Y.; Thawani, R.; Edmondson, C.P.; Chen, E.Y. Estimating the Time Toxicity of Contemporary Systemic Treatment Regimens for Advanced Esophageal and Gastric Cancers. Cancers 2023, 15, 5677. https://doi.org/10.3390/cancers15235677
Agrawal NY, Thawani R, Edmondson CP, Chen EY. Estimating the Time Toxicity of Contemporary Systemic Treatment Regimens for Advanced Esophageal and Gastric Cancers. Cancers. 2023; 15(23):5677. https://doi.org/10.3390/cancers15235677
Chicago/Turabian StyleAgrawal, Neha Y., Rajat Thawani, Corbin P. Edmondson, and Emerson Y. Chen. 2023. "Estimating the Time Toxicity of Contemporary Systemic Treatment Regimens for Advanced Esophageal and Gastric Cancers" Cancers 15, no. 23: 5677. https://doi.org/10.3390/cancers15235677
APA StyleAgrawal, N. Y., Thawani, R., Edmondson, C. P., & Chen, E. Y. (2023). Estimating the Time Toxicity of Contemporary Systemic Treatment Regimens for Advanced Esophageal and Gastric Cancers. Cancers, 15(23), 5677. https://doi.org/10.3390/cancers15235677







